Allergic dermatitis - symptoms and treatment in adults are very different. An inadequate skin reaction can be caused not only by direct exposure to its surface, but also by ingestion of an allergen.
Sometimes this is a skin response to a stressful situation (neurodermatitis). Manifestations of a pathological reaction can be immediate, or can develop as a cumulative effect over several months.
How to recognize an allergen? How to treat contact dermatitis with the latest generation of drugs? Is it worth using folk remedies or not?
Causes and risk factors
Allergic dermatitis refers to delayed-type allergic reactions, in which the main role is played not by antibodies, but by cells of the immune system and, above all, lymphocytes.
The following chemicals may cause symptoms of allergic dermatitis:
- paint and varnish products;
- washing powders;
- cosmetic and perfumery products;
- synthetic fabrics;
- latex.
Some medications (antibiotics, vitamins, syntomycin emulsion), and nickel jewelry can also act as allergens. Very often, the cause of allergic dermatitis on the hands is contact with plants (white ash, primrose, hogweed). This form of the disease is called phytodermatitis.
Allergic dermatitis may be a reaction to household chemicals
A special role in the development of an allergic reaction upon direct contact of the irritant and the skin is played by the phagocyte cells located in it. They absorb and digest allergens and immune complexes that enter the skin. After applying a specific irritant to the skin of a sensitized person, the number of phagocyte cells increases several times in a short period of time.
Phagocyte cells not only digest allergens, but also promote their contact with specific cells of the immune system, which causes a full-blown immune response, i.e., the development of an allergic reaction.
You can reduce the risk of developing allergic dermatitis by limiting contact with household chemicals. When working with them, you should use personal protective equipment (respirator, rubber gloves).
When the skin comes into contact with the allergen again, the allergic reaction occurs more vividly and violently than the first time. This is explained by the fact that the patient’s body already has antibodies and immune cells to this allergen.
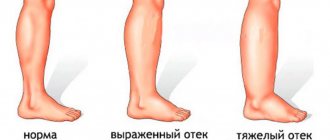
Phagocytes and lymphocytes at the site of inflammation also contribute to redness and swelling of the skin, dilation of blood vessels, and increased itching.
Predisposing factors to the development of allergic dermatitis are:
- thinning of the stratum corneum of the skin;
- increased sweating (hyperhidrosis);
- chronic inflammatory diseases accompanied by impaired immune response;
- predisposition to the development of allergic reactions.
Reasons for development and classification
Allergic dermatitis has various causes. A distinctive feature of this disease is its contact nature. Under the influence of provoking substances on the surface of the skin, sensitization of the body can occur. Due to the absence of antibodies, the skin reaction can be very strong. Symptoms appear at the moment when a certain amount of irritant has accumulated, which is enough to cause a reaction.
Skin dermatitis can appear under the influence of various allergens. This irritating effect is caused by:
- medications;
- cosmetic and perfumery products;
- polymeric substances;
- fruits and vegetables;
- chemical and industrial compounds.
Depending on the nature of the irritating influence, various types of disease may appear. Allergic dermatitis is divided into 4 types.
- With contact dermatitis, irritation appears after direct exposure to the allergen on the surface of the skin. An insect bite can also be a source of the reaction.
- During a toxic-allergic reaction, the allergen affects the respiratory tract, gastrointestinal tract, and skin. Symptoms appear very quickly.
- With atopic dermatitis, signs of rhinitis and eczema may appear. What distinguishes this disease from non-allergic skin diseases is that they are eliminated after therapy.
- Fixed erythema is preceded by long-term use of medications.
Depending on the nature of the course, the disease can be expressed in several stages:
- acute;
- protracted;
- subacute;
- chronic.
After contacting a medical facility, the doctor assesses the symptoms and tells you how to treat allergic dermatitis of one type or another.
Symptoms of allergic dermatitis
Skin lesions in allergic dermatitis are always localized at the site of contact with the irritating factor. For example, if the allergen is washing powder, then you should expect the development of allergic dermatitis on your hands. At the same time, the symptoms of allergic dermatitis on the face are most often caused by individual intolerance to cosmetics (powder, mascara, foundation, lipstick, blush).
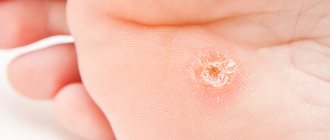
In allergic dermatitis, the lesion always has clearly defined boundaries. Initially, swelling of the skin and its redness are observed. Then papules (dense nodules) appear, which quickly turn into blisters filled with clear liquid. After some time, the bubbles open, and erosion appears in their place. All these skin changes are accompanied by severe itching.
Repeated skin contact with an allergen can lead to the formation of chronic allergic dermatitis. In this case, the lesion acquires blurred boundaries, and the inflammatory process can spread to distant areas of the skin, including those not in contact with the irritant. Symptoms of the chronic form of allergic dermatitis are:
- thickening of the skin;
- dryness;
- peeling;
- formation of papules;
- lichenization (increased severity of skin pattern).
Due to severe itching, patients constantly scratch the lesions, which is accompanied by trauma to the skin and can lead to the addition of secondary purulent-inflammatory lesions.
Allergic dermatitis is characterized by severe itching
Causes of occurrence in adults
The disease appears as a result of skin interaction with allergens and irritants. There are several main types of irritants that provoke the appearance and development of the disease:
- metals - chromium and nickel;
- certain chemicals - rubber, plastic, cement and pest control agents;
- adhesives;
- cosmetics and perfumes;
- some medicines, especially antibiotics and injectable medicines;
- food colors and products that contain them;
- some plants (oak, poison ivy and sumac, houseplant sap and pollen), berries and citrus fruits;
- household chemicals;
- toothpastes, rinses and other oral hygiene products;
- insects and their poison;
- tattoo ink;
- dental instruments;
- weather conditions - frostbite, chapping, direct sunlight;
Dermatitis is a consequence of increased sensitivity to a particular irritant. Many substances and products that are used in everyday life can cause an allergic reaction.
The disease can only be effectively cured if this source is clearly identified. Doing this, especially at home, is extremely difficult. The fact is that the disease, as a rule, is provoked by a very low concentration of the irritant. Therefore, at the first symptoms you should consult a specialist. In rare cases, the source of the allergic reaction cannot be identified.
You need to pay attention to where inflammation appears. For example, if those areas of the skin that are systematically treated with hygienic or cosmetic substances are affected, the body is likely to react to them.
Features of allergic dermatitis in children
Allergic dermatitis is a fairly commonly observed pathology in childhood. The disease has a chronic course, characterized by alternating periods of remissions and exacerbations. After puberty, in most adolescents, the signs of allergic dermatitis completely disappear.
The main role in the development of the disease in children belongs to genetic factors. If one of the parents suffers from allergies, then the probability of the child developing the disease is 50%, if both - 80%. If both father and mother are healthy, then the risk of allergic dermatitis in their offspring does not exceed 20%. However, the disease develops in children only when exposure to a specific irritant, i.e., an allergen, is added to the hereditary factor. Allergy factors may include:
- respiratory factor (inhalation of dust, aerosols, pollen);
- food factor (certain foods that are perceived by the child’s immune system as harmful irritants);
- contact factor (aggressive substance, for example soap, shampoo or baby cream).
Allergic dermatitis in infants initially manifests itself as a variant of food allergy that occurs as a result of non-compliance by a nursing mother with a hypoallergenic diet or the early introduction of complementary foods (eggs, cow's milk, cereals) into the child's diet. In the future, exacerbations of the disease are provoked not only by food allergens, but also by other irritants (house dust, fungal spores, animal epidermis, plant pollen). In many children in the first years of life, the cause of the development of allergic dermatitis is infection with certain types of staphylococcus, which cause chronic inflammation of the skin.
In children, allergic dermatitis initially manifests itself as a variant of food allergy
The main symptoms of allergic dermatitis in children are:
- local or generalized redness of the skin (hyperemia);
- areas of skin irritation and/or peeling;
- itching or burning;
- tearfulness;
- sleep disorders;
- dysfunction of the digestive system.
During allergic dermatitis in children, there are several age stages:
- Infantile dermatitis. It occurs from the first months of a baby’s life and lasts until the age of two. The disease is manifested by the appearance of characteristic rashes on the flexor surface of the child’s arms and legs, in natural skin folds. Often, in children with allergic dermatitis, an abundant small rash appears on the face in the cheek area, causing the cheeks to look painfully crimson. The lesions often become wet and covered with crusts.
- Children's dermatitis. It is observed in children from 2 to 12 years old. It is characterized by the appearance of areas of skin redness, with plaques, cracks, scratches, erosions and crusts. These lesions are in most cases localized in the area of the elbows and neck.
- Teenage dermatitis. Diagnosed in adolescents from 12 to 18 years of age. At this age, in most cases, the manifestations of allergic dermatitis disappear on their own, but in some adolescents, the symptoms of the disease, on the contrary, increase their severity. In these cases, contact with the allergen leads to the appearance of rashes on the face, neck, elbow pits, hands, feet, fingers and natural folds of the skin.
Sensitization is the stage before the onset of symptoms
The basis of dermatological diseases of an allergic nature is considered to be altered reactivity of the immune and nervous systems. Moreover, what matters is not structural disorders of the brain or spinal cord, but functional disorders involving the autonomic nervous system. They contribute to increased severity of allergic reactions and are often a provoking factor for relapse of the disease.
Sensitization of the body can occur through several mechanisms:
- absorption of incoming antigens by macrophages with subsequent activation and antigen-dependent proliferation of T-lymphocytes, it is these cells that serve as carriers of immune “memory”;
- the production of specific antibodies, of particular importance in this case is circulating Ig E, the increased production of which is often determined genetically and indicates atopy.
After initial contact with an allergen, the abnormally functioning immune system will retain information about it for an indefinite period. This condition is called sensitization. It puts the body on high alert for a quick response to repeated exposure to the same antigen. This is not accompanied by any symptoms, the person still feels healthy. But new contact with an allergen leads to a hyperergic reaction on the part of the immune system and its subordinate cells, and in allergic dermatoses, the dermis is predominantly the target.
Diagnostics
The diagnosis is made by identifying a combination of three major and at least three minor criteria in the patient. Major diagnostic criteria for allergic dermatitis include:
- recurrent nature of the disease;
- family or personal history of allergies;
- typical localization of rashes (under the earlobes, scalp, groin area, popliteal and elbow fossae, armpits, neck and face);
- severe itching of the skin, even with a small amount of elements of the rash.
Allergic dermatitis refers to delayed-type allergic reactions, in which the main role is played not by antibodies, but by cells of the immune system and, above all, lymphocytes.
Additional or minor diagnostic criteria include:
- onset of the disease in the first years of life;
- increased level of IgE antibodies;
- follicular hyperkeratosis, affecting the skin of the elbows, forearms and lateral surfaces of the shoulders);
- whitish spots on the skin of the shoulder girdle and face (Pityriasis alba);
- folding of the soles and palms (hyperlinearity);
- folding of the anterior surface of the neck;
- white dermographism;
- frequent infectious skin lesions of herpetic, fungal or staphylococcal etiology;
- nonspecific dermatitis of the legs and arms;
- ichthyosis, xerosis, peeling;
- redness and itching of the skin after taking a bath (this sign is detected in children in the first two years of life);
- symptom of “allergic glow” (dark circles around the eyes);
- increased sweating (hyperhidrosis), accompanied by itching.
Allergy skin tests help determine the cause of allergic dermatitis
To identify the allergen that caused the development of the disease, special skin tests are performed. To perform them, test strips impregnated with various allergens are used. These strips are fixed to an area of well-cleaned skin. After a certain time, they are removed and the presence or absence of an allergic reaction is assessed by swelling and redness of the skin.
Additional diagnostic tests may be required to identify concomitant pathologies:
- general blood analysis;
- blood biochemistry;
- blood sugar;
- general urine analysis;
- general stool analysis;
- microbiological examination of stool.
If necessary, the patient is consulted by a gastroenterologist or endocrinologist.
Causes of morbidity
The reason for the development of the skin dermatitis disease shown in the photo is the incorrect perception by the immune system of substances that somehow interact with the body. This process is directly called allergy.
Treatment of allergic dermatitis
Under the influence of allergens, many complex biochemical processes are launched in the patient’s body, so treatment of allergic dermatitis should be long-term and comprehensive, including the following areas:
- identifying and eliminating contact with the allergen;
- diet therapy;
- systemic pharmacotherapy (membrane-stabilizing and antihistamines, corticosteroids, antibiotics, immunomodulators, vitamins, drugs that regulate the functions of the gastrointestinal tract and central nervous system);
- external therapy (talkers, ointments, lotions);
- rehabilitation.
The main goals of the treatment of allergic dermatitis are:
- restoration of the functions and structure of the skin (normalization of humidity, improvement of metabolism and reduction of the permeability of the walls of blood vessels in the lesion);
- elimination of skin itching and manifestations of the inflammatory reaction;
- prevention of progression of the disease to a severe form, which can cause patients to lose their ability to work;
- therapy of concomitant pathology.
Considering that the pathological mechanism of development of allergic dermatitis is based on allergic inflammation, basic therapy is carried out with antihistamines and anti-inflammatory drugs.
In the chronic course of the disease, it is important to observe the stages and duration of treatment.
The general treatment regimen for allergic dermatitis in the acute phase includes the administration of the following medicinal groups of drugs:
- antihistamines with additional membrane-stabilizing and anti-mediator effects (second generation) for 4-6 weeks;
- first generation antihistamines (with sedative effect) at night;
- lotions with a 1% tannin solution or a decoction of oak bark in the presence of exudation;
- creams and ointments with corticosteroids (prescribed in a short course lasting no more than 7-10 days);
- systemic corticosteroid therapy (only if there is no effect from the therapy described above).
In the treatment of allergic dermatitis, ointments and creams with corticosteroids are prescribed
Treatment for chronic allergic dermatitis includes:
- second generation antihistamines for a long course (3-4 months);
- polyunsaturated fatty acids;
- immunosuppressive drugs (drugs that suppress excessive activity of the immune system);
- externally ointments with corticosteroids and antibiotics.
After achieving remission, it is necessary to carry out treatment of allergic dermatitis, aimed at preventing exacerbations of the disease. In this case, the following scheme is usually used:
- third generation antihistamines (active metabolites) for a course of 6 months or more;
- immunomodulators;
- specific immunotherapy with allergens;
- preparations containing polyunsaturated fatty acids.
Experimental treatment for allergic dermatitis
Clinical trials of the drug nemolizumab in the treatment of allergic dermatitis are currently underway. It is a member of a group of humanized monoclonal antibodies specific for interleukin-31.
The results of the second phase were published in 2019 in The New England Journal of Medicine. The drug was prescribed for three months to 264 adult patients suffering from severe forms of allergic dermatitis, in whom traditional treatment did not lead to a lasting positive effect. The patients were divided into two groups, one of them received nemolizumab, the other (control) received placebo. The effectiveness of therapy was assessed based on measuring the area of the affected area and the severity of the intensity of itching (assessed using a special visual analogue scale).
During treatment with nemolizumab, the intensity of itching decreased in 60% of patients, in the control group in 21%. A reduction in the area of lesions in the main group was recorded in 42% of patients, and in the control group in 27%. These results gave grounds to consider nemolizumab a promising drug in the treatment of allergic dermatitis.
Why does allergic dermatosis develop?
The cause of the development of allergic dermatosis is human contact with an allergen. It can be one-time or regularly repeated. The development of an abnormal reaction with skin damage is possible only if a person has previous sensitization to this allergen. That is, contact with this substance must be repeated, and the duration of its initial intake in most cases does not matter. Antigens of plants, animals and fungi, microbial agents, drugs and various chemical compounds can act as a sensitizer.
Predisposing factors for the formation of allergic dermatosis are hereditary predisposition, the presence of other diseases of an allergic nature (which may indicate atopy), chronic pathology of the gastrointestinal tract and intestinal dysbiosis. A certain role is assigned to regular contact with animals whose tissues have fairly strong antigenic properties. There is evidence that employees of zoo farms, poultry farms, fish farming and fish processing enterprises have an increased risk of developing allergic skin reactions.
The high level of environmental pollution at the place of permanent work or residence of a person is also important. This explains the prevalence of allergic dermatoses among urban residents and workers in the heavy and oil refining industries. Approximately 1/3 of people employed in chemical production have various forms of skin lesions of an allergic nature.
Allergic dermatoses in children often occur against the background of early unsystematic introduction of complementary foods and irrational artificial feeding. Their development is also facilitated by maternal allergy during pregnancy and breastfeeding, and previous use of antibacterial agents.
Eating foods saturated with artificial additives, the widespread use of various drugs during the raising of poultry and livestock, the use of pesticides in agriculture - all this also increases the general background of allergization of the population and contributes to an increase in the risk of developing allergic dermatoses.
1. Toxidermia 2. Papular urticaria
Nutrition for allergic dermatitis
Diet therapy plays an important role in the complex treatment of allergic dermatitis. It allows you to reduce treatment time and helps achieve stable remission. Products that increase sensitization of the body are excluded from the diet. These include:
- coffee;
- cocoa;
- chocolate;
- nuts;
- citrus;
- pickles and marinades;
- legumes;
- strawberry;
- seafood.
You should not eat foods that contain dyes, emulsifiers, or preservatives, as all these substances are strong allergens.
If you have allergic dermatitis, you need to exclude all allergenic foods from your diet.
Also, fried foods and rich, strong broths are not recommended for patients suffering from allergic dermatitis. This is explained by the fact that they enhance the absorption of irritating substances by the mucous membrane of the gastrointestinal tract.
Very often, the cause of allergic dermatitis on the hands is contact with plants (white ash, primrose, hogweed). This form of the disease is called phytodermatitis.
It is recommended to reduce the consumption of salt and sugar by 2-3 times, and even better, if possible, completely abandon their use during therapy. Before use, cereals must be washed in several waters and soaked for several hours.
For allergic dermatitis, nutritionists recommend eating:
- stewed or steamed lean meat;
- black bread;
- natural fermented milk products (without preservatives, sweeteners and dyes);
- freshly squeezed apple juice;
- greens (dill, parsley);
- cereals (rice, oatmeal, buckwheat);
- olive oil (no more than 25-30 grams per day).
Basic treatment methods
An important factor in successful treatment is the complete exclusion of the patient’s contact with the source of irritation. This is followed by therapy using special ointments, medications and procedures. The main tools for eliminating the disease are antihistamines and skin ointments. Late stages of the disease also require medications that would remove the effects of scratching and help fight ulcers and ulcers.
Antihistamines
Anti-allergy medications for illness are usually ointments that are applied to problem areas of the skin. There are several proven remedies that are most often used in therapy.
- Boromenthol . A menthol-based ointment helps relieve inflammation and significantly alleviates itching. The product is applied directly to the inflammation, usually before bed, to relieve the symptoms of the disease, which tend to worsen at night. The dosage, number of applications and duration of use are determined by the attending physician.
- Zodak . Available in tablet form. Unlike many similar drugs, it does not cause drowsiness. The dosage of the drug does not exceed one tablet per day, regardless of the condition.
- Psilo-balm. Used for the rapid relief of symptoms, mainly itching. The product is available in the form of an ointment and has dosage restrictions. It can be used only four times a day; if this limit is exceeded, the ointment can cause irritation. Psilo-balm can be used during pregnancy.
- Popular antihistamines that are used to relieve symptoms of most types of allergies are Cetrin, Telfast, Lortadin, Fenistil, Zyrtec, Erius and Claretin. It is advisable to use them as first aid at the initial stage of the disease.
It should be remembered that all drugs, especially if they are antibiotics, have contraindications and restrictions. They are not recommended to be used without first consulting a doctor. Only a doctor can most accurately determine the dosage, frequency of use and duration of therapy, taking into account the individual characteristics of the patient and the stage of the disease.
Some antihistamines, especially the first and second generation, can cause pronounced side effects such as drowsiness and distraction, tachycardia, gastrointestinal problems, and visual disturbances. In addition, if taken frequently, these drugs cease to be effective and require replacement with analogues.
Hormonal ointments
In some cases, when non-hormonal drugs cannot provide adequate treatment effectiveness, hormonal ointments are prescribed.
There is a fairly large list of drugs that are used to combat the disease:
- Prednisolone . The use of the drug occurs under the supervision of a physician. This is the most common remedy for treating the disease. The ointment is rubbed into the affected areas of the skin for one to two weeks, three times a day. It is recommended to rub in at regular intervals. The drug relieves inflammation and relieves itching.
- Advantan . The most modern hormonal ointment that has minimal side effects. Use no more than once a day. Duration of therapy is up to three months.
- Sinaflan . Apply four times a day. The peculiarity of this ointment is that rubbing can only be done if the skin area has been cleansed with an antiseptic. This allows the medicine to penetrate deeper. The duration of treatment is one to two weeks.
Hormonal medications are effective, but you should be aware of the side effects that can occur if used incorrectly. In this case, consultation with a doctor is mandatory, since the dosage of a particular ointment varies depending on individual indicators. These drugs may cause withdrawal symptoms.
Preparations for the treatment of scratches and pustules
The disease is characterized by severe itching. Prolonged and intense scratching of problem areas can cause skin damage, in particular ulcers and ulcers.
In order to eliminate them, special drugs are prescribed:
- Actovegin . Accelerates metabolism in skin tissues, which promotes their regeneration. Methods of application depend on the patient’s condition - during periods of exacerbation, rubbing is done twice a day, in other cases - no more than once. Therapy lasts up to two weeks. The ointment is used until the effects of dermatin completely disappear.
- Arkalen . The drug is similar to Actovegin, with the difference that it can cause allergies or swelling in some cases. The medicine does not belong to the class of antibiotics, but is considered extremely effective, but it should only be used under the supervision of a physician.
- Baneocin . Use with caution, since exceeding the standard dosage of 200 grams of the substance is fraught with side effects. If used incorrectly, problems with internal organs may occur. Not recommended for patients who have kidney problems. The drug is placed under the bandage. Duration of therapy is a week. Use no more than once a day.
- Levomekol . This ointment is well suited for removing pus from the affected areas of the skin. Usually used with a compress - a small amount of the substance is applied to gauze and applied to the wound. The compress should be changed once a day. As a preventive measure, the affected area is treated with an antiseptic.
The dosage of many medications is selected individually, since improper use of the above ointments can provoke inflammation and aggravate the disease.
Many drugs are used not only during periods of exacerbation, but also after recovery as means of prevention. Maintenance therapy can last up to several months. It is not recommended to adjust the timing of treatment on your own - symptoms may return at any time.
Traditional treatment of allergic dermatitis
In consultation with the attending physician, some traditional medicine methods can be used in the complex therapy of allergic dermatitis, for example:
- lotions with decoctions of medicinal herbs (chamomile, viburnum or oak bark, black currant bark, string);
- compresses with decoctions of felt burdock, calendula, lemon balm, elecampane roots;
- lubricating the affected areas with an ointment made from a mixture of baby cream or melted goose fat and sea buckthorn oil;
- aromatherapy with sandalwood, geranium or lavender oil;
- medicinal baths with decoctions of wild rosemary leaves, medicinal valerian roots, blue cornflower or chamomile flowers, nettle leaves and common oregano.
Folk remedies can be used as part of complex treatment of allergic dermatitis
Allergens - who are they?
Dust, poplar fluff, grass pollen, household chemicals, pet hair - these are just some of the factors that the body may not like. Often the allergic dermatitis shown in the photo causes problems for women. Treatment for allergic rashes is required on the face due to the use of inappropriate makeup, ointments and creams.
Forecast
If it is possible to identify and eliminate contact with the allergen, then the prognosis for allergic dermatitis is favorable, the disease ends in complete recovery.
In cases where it is not possible to eliminate contact with the allergen, allergic dermatitis becomes chronic and periodically worsens. The sensitization of the patient's body gradually increases, which ultimately becomes the reason for the generalization of the process and the development of systemic allergic reactions, even life-threatening ones.
First dots over i
There is no skin disease more common in the world than allergic dermatitis. The disease is in some ways so indiscriminate that it does not divide its victims by gender or age. However, allergic dermatitis, the photo of symptoms of which is discussed in today’s publication, is an exclusively adult disease. If an allergy manifests itself on a child’s skin, it is customary to talk about atopic dermatitis.
Prevention
There is no primary prevention aimed at preventing the disease of allergic dermatitis. The risk of its development can be reduced by limiting contact with household chemicals. When working with them, you should use personal protective equipment (respirator, rubber gloves).
When purchasing clothes and jewelry, you should give preference to quality products from reliable manufacturers. This will reduce the likelihood of skin contact with toxic metals and dyes, which often become allergens.
If the disease has already occurred, it is necessary to carry out active treatment aimed at achieving a state of remission. To do this, first of all, the allergen should be identified and further contact of the patient with it should be excluded.
Video from YouTube on the topic of the article:
More about the disease
Dermatosis of this type is included in the so-called heterogeneous group of skin diseases - allergic dermatoses. From the name it is clear that the appearance of characteristic redness on the skin is the body’s response to certain irritants. A separate type of disease is toxic-allergic dermatitis. A photo with its description is given above.
Stages of dermatosis
At the initial stage of dermatosis, symptoms appear on unchanged skin. Primary elements develop, which include:
- Stains.
- Vascular spots (hemorrhagic, ischemic, hyperemic).
- Blisters.
- Bubbles.
- Pustules (cavities filled with purulent contents).
- Vesicles (watery cavities raised above the skin level).
- Papules (nodule).
As a result of evolutionary changes and damage to primary elements on the skin, the following are formed:
- Erosion.
- Scales.
- Excoriation.
- Ulcers.
- Cracks.
- Scarring.
- Lichenization.
- Vegetation.
Key Features
Let's figure out what allergic dermatitis is and what it looks like. The basis of this pathology is an allergic reaction. Those. immune response to a stimulus. The patient himself can assume this disease if a characteristic picture occurs.
Visual skin manifestations:
- red spots of irregular, blurry outlines and sizes;
- clusters of bubbles filled with clear liquid;
- vesicular accumulations (numerous red tubercles).
The duration of the disease depends on:
- on the type of disease;
- from an irritant;
- level of sensitization;
- degree of impact;
- state and characteristics of the immune system.
The disease itself is not contagious, as it is caused by individual immune processes. But if the cause of dermatitis was some kind of infection, then it’s a different matter.
The acute symptomatic picture also varies in time. Symptoms may subside in a few days with mild sensitization, or they may plague the patient for months.
According to the medical classification (ICD-10), allergic contact dermatitis is coded L23.
Types of dermatitis on the hands
1. for reasons of appearance:
Contact dermatitis occurs after the action of an external irritant. As a result, this pathology is localized exactly where the contact occurred. Atopic dermatitis is characterized by the occurrence of inflammation on the skin, which is genetically determined. Solar dermatitis is an inflammatory reaction of the dermis that appears after exposure to sunlight, and occurs like an allergic reaction (see sun allergy: symptoms, treatment). Actinic dermatitis - radiation exposure, ultraviolet radiation, sun rays, sources of ionizing radiation. The clinical picture of dermatitis depends on the intensity and time of exposure to radiation on the skin. It affects welders, farmers, foundry workers, and radiologists. Allergic dermatitis on the hands is the body's reaction to exposure to various allergens. It manifests itself as a rash, itching, and burning sensation on the skin. May be recurrent.
| Actinic dermatitis | Allergic dermatitis | Atopic dermatitis |
| Solar dermatitis | Contact dermatitis |
2. according to the course of the disease
Acute form, which is characterized by the severity of symptoms (redness, swelling, itching, burning, blistering); A chronic form, which is characterized by the presence of prolonged swelling in the area of inflammation. As a result, the skin color changes to a bluish tint, and the skin in the affected area thickens.
What do the symptoms of dermatitis on the hands look like?
In the acute form of the disease, the following symptoms are observed:
the skin on the hands becomes red or pink, and when exposed to cold, turns bluish-red; severe itching appears in places of redness; the disease is accompanied by pain; tissue swelling may occur; bubbles filled with cloudy liquid may appear, which, after bursting, leave weeping erosions, which are subsequently covered with scales or crusts; in severe cases, tissue necrosis is possible; if the cause is mechanical damage, abrasions and blisters appear on the skin, on the palms, it looks like calluses.
In the absence of treatment, the disease becomes chronic, for which the characteristic symptoms are:
the skin on the hands takes on a bluish tint; the upper layer of the skin thickens, and areas of keratinization appear; the skin of the hands becomes dry, peels and cracks; If the disease is not treated, atrophy of the epidermis may occur.
Complications
Dermatitis of the hands and fingers causes significant discomfort to the patient. It can lead to the development of serious diseases:
Sepsis or blood poisoning Eczema, which develops as a result of infection by bacteria, viruses and fungi in the area affected by dermatitis. Dermatitis can also lead to psycho-emotional disorders that are associated with incessant itching and burning in the affected area
However, with adequate and effective treatment, dermatitis does not cause serious complications.
Treatment of dermatoses
Depending on the cause of the disease, its development and possible complications, medications from the following pharmacological groups are used to treat dermatoses:
- Corticosteroids.
- Antibiotics.
- Antiviral.
- Antifungal.
- Antimicrobial.
- Antiparasitic.
- Antihistamines.
- Angioprotectors.
- Immunostimulants.
- Detoxification.
- Nonsteroidal anti-inflammatory drugs.
The name of the drugs, their dosage and treatment regimen are determined individually after identifying the cause of the disease, the severity of the process and the degree of its severity.
Why should dermatitis be treated?
Contrary to popular belief, mild dermatitis will not go away on its own. Even if the rash has a small area of spread, the disease cannot be eliminated at home.
The disease has dangerous complications. In addition to the fact that inflammation will cover the entire large surface of the skin, lack of treatment threatens the appearance of abscesses, phlegmon (damage to the subcutaneous tissue), ulcers, ulcers, general weakness and a runny nose. In some cases, fever, vomiting, nausea, chills and other unpleasant symptoms may occur.
Diagnosis
In the diagnosis of this form of dermatitis, special tests are used, which involve applying suspected allergens to the patient’s skin to identify a specific one based on the concomitant reaction. This option for diagnosing the disease is extremely important in the matter of subsequent treatment. In frequent cases, patients themselves notice which substance provoked the development of an allergic reaction in them.
Allergic dermatitis in children, as well as in adults, requires the identification of specific allergens and their prompt exclusion, because exposure to them can provoke larger and more serious manifestations characteristic of allergic reactions (for example, asthma, Quincke's edema or anaphylactic shock).
Causes
Internal causes of the disease:
diseases of the endocrine system, which result in hormonal imbalance; diseases of the digestive system; neuroses; depressive states;
External factors:
| Physical stimuli | Friction, exposure to high or low temperatures, exposure to ultraviolet radiation. |
| Biological reasons | Exposure of the skin to pollen or plant juice (nettle, wormwood, milkweed.) |
| Cosmetical tools | Use of creams, scrubs, lotions, perfumes. |
| Chemical irritants | Skin contact with washing powders or detergents. |
| Medicines | Taking medications (antibiotics, nonsteroidal anti-inflammatory drugs, vitamin supplements, medications that contain nickel or chromium). |
| Food products | Food products with a large amount of dyes, preservatives, honey, nuts, chocolate, coffee, alcoholic drinks. |
Diagnosis of dermatitis
To diagnose, the doctor will need to establish the nature of the irritant, the rate of development of the reaction after contact with it, and the affected area. In addition, the patient will need to submit:
General detailed analysis of blood and urine Undergo serological and immunological tests Biopsy followed by histology (if indicated) Contact an allergist and take blood tests for various allergens
The rate of development of the disease, the type of dermatitis and the main cause of its occurrence will determine the doctor’s decision on how to treat dermatitis on the hands.
Causes of dermatitis
There are external irritants that cause dermatitis of the skin of the hands from the hand to the elbow. About 90% of patients suffering from dermatitis are women.
Physical agents. This group includes the effects of pressure, friction, high or low temperature conditions, and radiation. For example, the causes of cold dermatitis can be spasm of peripheral capillaries and the development of inflammation caused by low temperature (see cold allergy: symptoms, treatment). Biological stimuli. This group includes the juice or pollen of plants, for example, nettle, buttercup, garlic, aloe, snowdrop, milkweed and others. Group of chemical agents. These are chemicals that can damage the skin (acid, alkali, washing powder, varnishes, paints, etc.). Quite a lot of people complain about flaking of the skin of their hands and recurrence of dermatitis after using washing powders or detergents at home.
Allergens that cause dermatitis:
Products that cause an individual allergic reaction or food intolerance - cow's milk, citrus fruits, nuts, red fruits, honey, confectionery, any products with artificial additives, preservatives, flavors, etc. Polluted air containing a lot of toxic substances, industrial emissions, exhaust gases from vehicles, as well as plant pollen during the flowering period. Taking medications, absolutely any medication can cause allergies, be it an antibacterial drug, an analgesic, NSAIDs, or even herbs and dietary supplements. Cosmetics and perfumes are a separate category of external irritants; every year the number of women who develop allergies to various hand creams, balms, as well as deodorants, perfumes, eau de toilette, mascara, powder or eye shadow increases.
The causes of atopic dermatitis on the hands in adults are considered to be a hereditary predisposition of the human body to the occurrence of atopy, autoimmune conditions, chronic pathologies of internal organs, especially the gastrointestinal tract and endocrine glands (see treatment of atopic dermatitis in children).
Research by Italian scientists proves that having a dog in the house reduces the risk of dermatitis in a child by 25%, provided that the dog is in the house from birth (see Dogs reduce the risk of atopic dermatitis in children).
It is important to remember that dermatitis on the hands can be caused by neuroses, depressive disorders, stressful situations and hormonal imbalance.
If the patient has a history of allergic diseases in combination with certain disorders in the functioning of the immune system, then the action of external factors can lead to a significantly more intense reaction of the body compared to healthy people.