Instrumental studies carried out to diagnose diseases of the abdominal organs cause a lot of discomfort. This leads to patients postponing a visit to the doctor for an indefinite period, which contributes to the development of serious complications. Currently, CT or MRI have begun to be used to examine the stomach, small and large intestines. What is better to use to make a more accurate diagnosis?
Research methods - colonoscopy and MRI
Which is better when diagnosing gastrointestinal diseases - MRI of the intestines or colonoscopy - depends entirely on the symptoms, with the development of which a preliminary diagnosis will be established. Each method has its own advantages and disadvantages, which should be taken into account when prescribing such a research method. It is up to the doctor to finally decide which method will be most effective in diagnosing a particular disease.
In addition, doctors’ arsenal includes other, no less effective methods for examining patients with gastrointestinal diseases. Among them:
- X-ray examination - irriography is usually prescribed, where X-rays can determine intestinal pathology. The group of X-ray examinations also includes MRI, despite the fact that X-rays are not involved in this examination.
- Laboratory diagnostics - in which blood is donated from a vein for the presence of tumor markers in it when diagnosing intestinal cancer, refers to non-instrumental diagnostic methods.
- Endoscopic examinations - a group of which includes colonoscopy - a special device equipped with optics is inserted by a doctor into the intestines to examine and study the structure of the organ or the presence of pathologies in it.
MRI of the intestine and colonoscopy are fundamentally different research methods in purpose and essence. But for many patients who are prescribed this or that examination, the main question remains of choice.
Preparing for MRI
In order to be examined effectively, when preparing for an MRI of the intestine, all cleansing methods are used:
- diet;
- medicines;
- cleansing enemas.
Food restrictions are aimed primarily at reducing flatulence.
To reduce gas formation and fermentation, 2 days before the diagnostic test, the following are excluded:
- legumes;
- black bread;
- fermented milk drinks;
- whole milk;
- fresh fruits and vegetables containing coarse fiber that settles on the intestinal walls;
- pickled vegetables;
- sweet drinks with gas.
It is necessary to remove heavy foods that fill the intestines from the diet:
- fresh white bread;
- fatty, fried, spicy foods that irritate the walls or take a long time to digest.
Fruit juices with pulp, coffee, and energy drinks should also be excluded from drinks. There are no other restrictions on drinking.
If the diet is ineffective and constipation and flatulence persist, the doctor will give a recommendation for therapy that will help cleanse the intestines. For 2-3 days you need to take:
- enterosorbents, defoamers, carminatives in adequate dosages (Polysorb, Espumisan, Simethicone);
- antispasmodics for increased intestinal tone (No-spa, Drotaverine).
For prolonged constipation, cleansing enemas are given on the eve of the examination and on the day of the procedure. At home, it is preferable to use an Esmarch mug - it is more convenient than a regular enema bulb in that it holds up to 2 liters of water. The enema is done twice with an hour break. Use warm boiled or purified water at a comfortable temperature. A cold enema will cause muscle spasms, while a hot one can cause a burn. In the morning, enemas are repeated 3 hours before the examination.
If a cleansing enema using an Esmarch mug is contraindicated, you can use ready-made pharmaceuticals (Mikrolax, Salofalk). They are easy to use, act quickly, and do not cause tenesmus or discomfort.
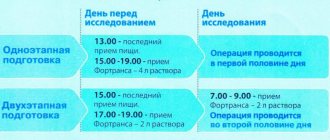
There are special effective laxatives in powder form - Fortrans. It is available in packages, the dose is calculated based on the patient's weight. The powder is dissolved in 1 liter of water, drunk within an hour: 1 glass every 15 minutes. The drug is taken in the evening and early in the morning on the day of the diagnostic procedure.
If the diagnosis is done in a private clinic, it is paid. To obtain a free MRI under the compulsory medical insurance policy, you must go to a medical institution at your place of residence and take a referral in the prescribed form from your attending physician. You must also bring your outpatient card and the results of previous studies to your appointment.
On the appointed day, an hour before the tomography, you need to urinate, take an antispasmodic 30 minutes in case of pain in the intestines. Before scanning, you must remove jewelry, watches, hair clips, mobile phone and bank card with a magnetic stripe. This is done because metal objects in the MRI machine become heated and magnetized, and the operation of electronic devices is disrupted by the magnetic field.
Resonance imaging of the intestine
A clear advantage of this method is its high efficiency in examining patients in the early stages of gastrointestinal diseases. Essentially, the device itself is a tube in which a person is placed, and the radio waves and magnetic fields that are in it allow one to obtain detailed images of the intestine scanned layer by layer. Indications for MRI:
- When the preliminary diagnosis is malignant and benign neoplasms.
- Detection of the number and location of metastases.
- When, besides MRI, any other methods of examining the gastrointestinal tract are contraindicated.
- To study intestinal vessels and their filling.
- To study the peritoneal lymph nodes and their ducts.
- Determining the origin of abdominal pain.
- Diagnosis of diseases of the liver, pancreas, bile ducts.
How is the examination done?
The preparatory stage for the study includes filling the intestines with water so that its loops “swell.” Eating is not allowed for 10 hours before an MRI of the intestine, and eating before the study is also prohibited. Before entering the office, you should remove any metal objects from yourself - piercings, halter, dentures, and for women - a bra. When the MRI machine is in operation, the use of mobile phones is prohibited, so it is better to leave it outside the MRI room. The doctor who conducts the examination must explain to the patient that for the diagnosis to be effective, he must lie level and motionless the entire time the device is working, and only report a sharp deterioration in his condition.
Video about bowel examination methods
A selection of videos about how to check the intestines. They are full of useful and essential information. Thanks to the first video, you will have the opportunity to see how an intestinal examination takes place. A professor of proctology will tell you all the nuances of the process and clarify whether it is painful to do a colonoscopy. You will find out if there are alternatives to this procedure. In the second video, the doctor will talk about what is better, colonoscopy or MRI of the intestine. Watch the video to the end and learn how to properly prepare for an intra-abdominal examination.
Colonoscopy
Colonoscopy of the intestine
Magnetic resonance imaging
What is MRI? Simple and clear!
What does an MRI of the intestine reveal?
The accuracy of this method is extremely high, which makes it possible to determine both organic disorders in the intestines and its smallest structures and formations - duct stones, neoplasms, metastases, polyps. As a result of such a study, not only the topographic location of the pathology will be visible, but also its size and structure. In addition, MRI allows layer-by-layer examination of nearby organs and tissues of the peritoneum to exclude concomitant diseases of the abdominal cavity, as well as stomach diseases, in contrast to colonoscopic examination. The method is considered painless and does not cause discomfort or pain to the patient.
Reasons for prescribing MRI
The digestive system is a multifunctional mechanism based on converting food into easily digestible elements and removing waste byproducts. Well-organized activity of all links in this chain affects the degree of saturation of the body with useful elements.
Malfunctions of the digestive organs manifest themselves through the following signs:
- periodic pain in the abdominal cavity;
- a sharp decrease in body weight;
- loss of appetite;
- bowel disorders.
If such symptoms appear, you should make an appointment with a gastroenterologist and proctologist.
This research method is relevant if there is a risk of the following diseases:
- internal bleeding;
- inflammation of the mucous membranes;
- intestinal obstruction;
- tumor;
- ulcer;
- gastritis.
An MRI can also help identify a foreign body in the digestive tract.
This type of tomography is not informative enough in the following situations:
- minor inflammatory processes of the mucous membranes;
- overly “mobile” peristalsis.
This method is not used in emergency situations. Computed tomography is a faster way to examine the body. For making urgent diagnostic decisions, it is unrivaled. In routine diagnostics of the digestive system, the importance of CT and MRI is equal.
Contraindications to MRI diagnostics of the intestine:
- Early pregnancy – up to 12 weeks.
- Aneurysms of cranial vessels.
- Individual intolerance to the contrast agent used.
- Pain syndrome requiring constant administration of analgesics.
- Foreign bodies in the body - for example, replaced joints or intrauterine devices.
- Tattoos whose ink contains metal-containing compounds.
- Fear of closed spaces – claustrophobia. To prevent a panic attack in patients with this disease, they are given narcotic or strong sedatives.
- Childhood.
- People with diseases of the central nervous system - cerebral palsy, epilepsy.
- Intestinal bleeding.
- Hernias.
- Metal fragments.
- Heart valve prostheses.
- Weight more than 100 kg.
Advantages and disadvantages
This method is used using a contrast agent, which is absolutely safe for patients and is easily and quickly eliminated by the body. If a contrast agent was not used, intestinal MRI would have low informativeness and diagnostic efficiency. The examination itself lasts about an hour. During this time, patients are advised to remain in a relaxed state, but not to sleep, since in their sleep they may move, which will disrupt the entire study as a whole. To securely fix it, special belts are used to fasten it to the table surface.
Despite the high percentage of positive qualities, intestinal MRI is not a leader in the diagnosis of diseases of the large and small intestine. Flaws in pathology visualization, the high cost of the study, the length of stay in the camera of the device, and, compared with colonoscopy, the inability to carry out local intestinal therapy or take pathological material (biopsy) for further research.
https://youtu.be/9lWctu151ms
Diagnosed pathologies
Using this diagnostic technique, medical specialists also have the opportunity to identify the following pathological changes:
- single and multiple polyps;
- diverticula;
- foreign bodies;
- pathologies of the development of intestinal loops;
- intestinal obstruction;
- benign and malignant neoplasms;
- presence and localization of foci of metastasis;
- Crohn's disease;
- erosive and ulcerative changes in the intestinal wall;
- acute and chronic pathologies of the colon (nonspecific ulcerative colitis).
Magnetic resonance imaging of the stomach and intestines is effective not only in diagnosing malignant neoplasms, but also in determining the degree of development of a malignant tumor.
Using MRI diagnostics, it is possible to monitor the effectiveness of drug therapy. If there are individual indications, patients undergo a repeat magnetic resonance examination.
Diverticulosis is a disease in which pouch-like protrusions up to 1-2 cm in size form in the intestinal walls
During the magnetic resonance imaging procedure, it is possible to detect structural changes in the area of the walls of the large and small intestine, as well as the presence of benign and malignant neoplasms.
The most reliable and common sign of Crohn's disease is uneven thickening of the intestinal wall. In addition, signs such as dissection of the intestinal wall, segmental lesions and longitudinal deep ulcers are revealed. Thanks to this diagnostic technique, it is possible to detect inflammatory changes in the mesentery and circulatory disorders.
Each form of Crohn's disease is characterized by an increase in the size of the lymph nodes along the entire length of the mesentery of the small intestine. In addition, MRI images clearly show the edematous tissue that surrounds the intestines. The walls of the inflamed intestine tend to accumulate contrast agent.
When malignant neoplasms are detected in the intestinal area, their location, size and structure will be displayed with maximum information.
Increased accumulation of contrast agent, an increase in the number of blood vessels and blood supply indicate the active phase of a particular disease. If the pathological process is chronic, then MRI images will show areas of fibrosis.
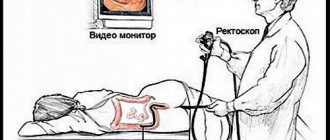
Features of rectal colonoscopy
Devices that are used for diagnostic purposes in diseases of the large intestine are called colonoscopes. The length of their working, flexible tube varies depending on the anatomical region of the intestine that needs to be examined, hence the name:
- 65-85 cm – sigmoidoscopes.
- 105-110 cm – short devices.
- 135-145 cm – average dimensions of the device.
- 165-175 cm – long devices.
At the end of such a tube there is a mini-video camera and a light source.
Painful sensations
An endoscope is inserted into the anus, then air is introduced into the patient's intestines. The disadvantage of this method is that patients often have a negative attitude towards colonoscopy and are afraid of the procedure, since all medical procedures, despite the administered anesthetics, are accompanied by unpleasant sensations, and in some cases very severe pain attacks. But for specialists, colonoscopy is a higher priority examination than the others. Its diagnostic value, which allows not only to conduct a detailed examination of the lumen of the large intestine, but also to take tissue for research, puts colonoscopy at the head of all methods of intestinal examination.
Features of preparation
Preparation for bowel examination is the same for both MRI and colonoscopy. Its main purpose is to cleanse the intestines so that the organ is better visualized in the pictures. A few days before the test, a short-term diet is prescribed, which is aimed at unloading the intestines.
Intestinal diagnostics
Its basic rules are:
- foods that cause increased flatulence are excluded: fresh vegetables and fruits, legumes, cabbage, carbonated drinks;
- the consumption of heavy foods is limited, it is recommended to consume soups with water, baked vegetables and fruits;
- You can’t overeat, you need to eat in small portions;
- the day before the test, you need to give up food completely, you can only drink water and weak tea.
Advantages and disadvantages of the method
The obvious advantages of this method are that it allows specialists to examine the large intestine in detail, affecting almost all of its sections. Also, using this method, it is possible to carry out a biopsy from detected tumors, remove polyps or a foreign body. Colonoscopy is recommended for:
- Rapid weight loss.
- Inflammation of various etiologies in the large intestine.
- Hemorrhoids in the acute phase.
- Long-term constipation.
- Internal bleeding.
- Ischemic colitis.
- Chronic peritonitis.
- Diabetes.
- Pregnancy.
- Abnormalities of intestinal development.
- Intestinal ulcers.
- Intestinal tumors.
https://youtu.be/g2dSvyFSc7k
The disadvantages of colonoscopy include the inability to examine other areas of the peritoneum and pelvic area, and the pain syndrome that accompanies the examination. Also, the method allows you to examine only the large intestine.
- Rupture of the intestine at the point of communication with the abdominal region.
- Aneurysm of the aorta, its abdominal section.
- Myocardial infarction.
- Pulmonary embolism.
- Postoperative period.
- Unstable hemodynamic parameters.
- The patient's categorical refusal to undergo the procedure.
- Pulmonary failure.
- Colds and ARVI.
- Disorders of the patient's blood clotting system.
- Shock of any etiology.
After the procedure, it is recommended to remain under the supervision of a doctor for some time. The diet can no longer be followed; in case of severe and prolonged bloating, it is recommended to take enterosorbents, after taking which the patient’s condition usually returns to normal.
Why is a colonoscopy preferable to an MRI?
Colonoscopy is considered a more informative and detailed method only in cases where the study needs to be carried out on the large intestine. In other cases, an MRI examination is performed. There are gastrointestinal pathologies when both of these methods are required. The attending physician will help the patient make the final decision based on the medical history, clinical picture and his condition. Whether a colonoscopy of the large intestine replaces an MRI examination when examining the peritoneal organs depends entirely on the location of the pathology - if we are talking only about the large intestine, then the methods are interchangeable.
Alternative research methods
In addition to those described above, there are also alternative methods for studying gastrointestinal diseases.
Endorectal ultrasound
Ultrasound, which is done using special equipment. The method is especially effective in diagnosing cancer of the distal intestine - colon.
Irrigoscopy, hydrotomography and colonoscopy - an alternative to MRI
An irrigocopy is performed after the administration of a barium mixture in the form of an enema, after which several x-rays are taken. The method allows you to detect scars, ulcers and polyps of the small intestine, and is especially convenient because it does not have “blind areas”. When using it, the radiation dose is less than when using CT methods.
Computed tomography of the intestine or virtual colonography
A CT scan is carried out as follows: the patient, as with an MRI, lies down on a table to which he is fixed with belts, a tube is inserted into the anus and the intestines are filled with air. The table is directed into a chamber where the patient will have to hold his breath when the doctor tells him to do so. The examination is not accompanied by severe pain; its duration is about 15-20 minutes. Preparation for the study includes the same points that must be completed for colonoscopy and MRI.
Hydro-MRI
The method is relatively new and is effective in detecting tumors at the earliest stages of the disease. This examination uses a contrast agent.
Non-instrumental research methods
They include laboratory methods for testing blood from a patient’s vein, stool analysis for occult blood to diagnose intestinal cancer.
How is the CT procedure performed?
Computed tomography is performed over 15-30 minutes. The patient is also advised to lie still, but in this case this does not make much difference.
When examining the abdominal cavity using contrast, the patient is injected with a special solution in order to better visualize the formations. This makes it possible to detect even small tumors, hematomas and blood clots. Contrast-enhanced CT is used only if additional imaging is needed.