October 20, 2019
- What is lupus erythematosus
- Causes of the disease
- Lupus symptoms
- Development mechanism
- Symptoms of the disease at different stages
- How do doctors diagnose lupus?
- Features of treatment and prognosis
Hello, dear readers of the KtoNaNovenkogo.ru blog. “Lupus erythematosus” is an unusual name for a disease that affects several million people in the world.
The coverage is not small - I tell you. It’s worth “dig deeper” and find out what lupus is, what kind of “beast” it is, how to identify the disease and fight it back. Let's start with the concept.
What it is
Before talking about why systemic lupus erythematosus (SLE) develops, it is necessary to first understand what it is and whether the disease is contagious to others or not? SLE is an autoimmune disease in which the body begins to produce antibodies to its own cells, gradually destroying them.
It appears mainly on the skin. The etiology of its development is still not fully understood. However, if previously the diagnosis of “lupus erythematosus” was made as a death sentence, today modern medicine offers many ways to combat it, which can reduce symptoms, improve the patient’s condition and prolong his life.
Most often, SLE is diagnosed in women of reproductive age, mainly several years after childbirth. In men, this disease is detected much less frequently. The incidence of this pathology on the planet is low - 2-3 cases per 1000 people.
Regarding the question of whether SLE is transmitted or not, it must be said that it is impossible to become infected with this disease through contact, household, sexual or airborne transmission. This is an autoimmune disease and it develops due to malfunctions of the immune system.
Lupus in pregnant women and children
The development of lupus erythematosus is possible during pregnancy at any stage . Often, expectant mothers mistake the initial symptoms of the disease for changes in the body during pregnancy.
If a pregnant woman begins to develop SLE, she may:
- blood pressure rise;
- kidney problems will appear;
- in 25% of cases there will be a miscarriage;
- labor begins prematurely;
- the fetus will stop developing , due to which the baby is born with anomalies;
- blood clots form in the placenta , which is why nutrients are poorly supplied to the fetus.
When a pregnant woman is diagnosed with lupus erythematosus, she must be under medical supervision in a hospital setting for the remaining time before giving birth. Such patients should take medications following two main rules:
- The action and dose of medications taken should suppress the intensity of the pathology and ensure successful pregnancy, childbirth and the postpartum period .
- The influence of funds on the future baby and the formation of its organs and systems should be minimal.
As for children, the disease manifests itself in them in the form of multiple symptoms. The disease gradually affects different organs in the baby’s body, and doctors are not able to predict in which system the next failure will occur. It initially appears as an allergy or dermatitis , which makes lupus difficult to diagnose.
In childhood, SLE is characterized by the development of the following symptoms:
- dystrophy;
- thinning of the skin, photosensitivity;
- fever , which causes profuse sweating and chills ;
- allergic rash;
- dermatitis , initially localized in the area of the cheeks and bridge of the nose ;
- pain in the joints;
- brittle nail plates;
- tissue necrosis in the area of the fingertips and palms;
- hair loss;
- seizures;
- mental disorders (irritability, moodiness, etc.);
- stomatitis , which cannot be treated.
Each patient who has pronounced symptoms of lupus erythematosus is treated in a hospital . The most effective drugs for this disease are from the group of corticosteroids , the active ingredient of which is Prednisolone . These medications help weaken the pathological process and prolong the life of a person with this pathology.
We recommend reading: everything about the ointment for nail fungus “Terbinafine” - instructions for use, analogues, contraindications, reviews.
"Loceryl" for nail fungus: price, instructions for use, composition, release forms, reviews. See information here.
Antifungal medicine "Irunin":
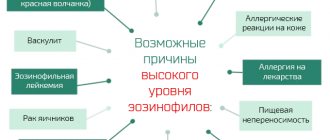
Reasons for development
What kind of disease is lupus in women has already been said above. What are the reasons for its development? It was previously noted that the etiology of SLE is not fully understood. However, in the majority of patients with this disease, antibodies to the Epstein-Barr virus were found in the blood, which confirms the possible viral nature of the pathology. In this case, malfunctions in the functioning of the immune system are noted - it begins to synthesize autoantibodies, which were also detected in all patients.
The causes of lupus erythematosus are also hidden in hormonal disorders. This is not an officially confirmed fact, but the presence of hormonal system disorders was found in 30% of patients. And, despite the fact that they cannot provoke the development of the disease, they significantly worsen its course. Therefore, women who have been diagnosed with SLE are not recommended to take oral contraceptives.
The mechanism of development of the disease is hidden in a violation of immunoregulation - the body begins to produce autoantigens, which begin to destroy healthy cells
Scientists also noted that in individuals with a genetic predisposition to the pathology and in identical twins, the risks of developing systemic lupus erythematosus are much higher than in other people.
What is lupus erythematosus
Lupus is a chronic autoimmune disease that affects the kidneys, vascular, connective tissue, and other organs and systems.
The body of a healthy person produces antibodies that are able to resist “uninvited guests” - foreign organisms from the outside.
When lupus develops, the number of antibodies directed to healthy cells and their components increases sharply - an immune complex inflammatory process is observed, leading to dysfunction of various elements of the body.
Attention! Women are more likely to suffer from lupus . This is explained by the structural features of the body.
At risk are also girls going through puberty, pregnant and lactating women, patients with a hereditary predisposition to pathology (what is it?).
Congenital lupus erythematosus develops in a child’s body in the first years of life.
Symptoms
Symptoms of systemic lupus erythematosus vary. As a rule, connective tissue, skin and epithelium are damaged. The main symptom of the disease is simultaneous and symmetrical damage to large joints with subsequent deformation. But if in other articular pathologies (arthritis, arthrosis, etc.) erosive tissue changes are observed, then in SLE pathological changes occur due to the involvement of ligaments and tendons.
The disease also manifests itself:
- pneumonitis;
- pleurisy;
- myalgia.
However, the most pronounced signs of pathology are observed on the skin, mainly on the face. A multiple rash appears, which merges to form large lesions. It is this symptom that most often identifies SLE.
At the very beginning of its development, the disease manifests itself as a continuous course with periodic transitions to the remission stage, after which it acquires a systemic form. Patients have symptoms of butterfly-type erythematous dermatitis on the face. Almost all areas are affected - nose, forehead, cheeks, forehead. At the same time, sensitivity to solar radiation increases, resulting in photodermatosis. It is multiple in nature and usually round in shape.
In SLE, photodermatoses have one feature - the presence of a hyperemic corolla. In the central part of the lesions, atrophied tissues are observed, depigmentation predominates. Pityriasis scales begin to form on top. They do not separate from the skin and all attempts to remove them cause severe pain in a person. And when the atrophy phase begins, in place of the erythema, smooth and delicate white skin is formed, gradually displacing the affected areas.
The main symptom of SLE is a butterfly rash on the face.
Not all patients experience the disease only on the face. There are cases when the symptoms of lupus erythematosus spread to the scalp, causing severe hair loss and the appearance of patches of baldness.
The most unpleasant sign of SLE is the appearance of erythema on the red border of the lips and mucous membranes of the mouth. They often bleed and are prone to ulceration, which causes severe pain to the person while eating or drinking. In this case, the erythema lesions acquire a bluish tint, they are dense and covered with scales, and their contours do not have clear boundaries.
Talking about what lupus erythematosus is and how it manifests itself, it should be noted that this disease has a seasonal course. The condition of the skin deteriorates significantly when exposed to ultraviolet rays. And since they are strongest in the summer-autumn period, it is at this time that exacerbations most often occur.
IMPORTANT! The first symptoms of the disease do not appear immediately. Many people do not even suspect that they have SLE, since in its clinical picture it can mimic or repeat the symptoms of other pathologies, for example, arthritis, fibromyalgia and other disorders affecting internal organs and systems. And in order to make a correct diagnosis and prescribe appropriate treatment, the patient needs to undergo special tests.
But when lupus erythematosus begins to actively develop and enters the subacute phase, then in this case its symptoms are very difficult not to recognize. In a person, psoriasis-like lesions appear throughout the body, telangiectasia is pronounced, and a tree-like pattern becomes clearly visible on the legs.
In almost all patients, the pathology is accompanied by:
- skin itching;
- baldness (partial or complete);
- allergic rashes such as urticaria.
In this case, all organs that contain connective tissue are affected:
- lining of the heart;
- renal pelvis;
- Gastrointestinal tract.
IMPORTANT! In addition to dermatological manifestations, systemic lupus erythematosus provokes headaches and joint pain in patients (most often due to changing weather conditions), disorders of the heart and urinary system, and frequent mood swings.
In older patients, skin lesions are less pronounced. However, against the background of SLE, they begin to develop Sjögren's syndrome, which is also an autoimmune condition that affects the salivary glands, dry eyes, and photophobia.
And if we summarize, talking about the main manifestations of lupus erythematosus, we should highlight the following:
Osteitis deformans
- a rash on the face that looks like a butterfly;
- deterioration of the condition of the skin, increased sensitivity to ultraviolet radiation;
- periodically occurring causeless fever;
- pain in joints and muscles;
- active hair loss;
- changes in the color of the fingers, which become lighter in cold ambient temperatures;
- anemia;
- swelling of the upper and lower extremities;
- weakness, fatigue;
- inflammation of the mucous membranes in the mouth and nose.
The mechanism of development of lupus
To understand what systemic lupus erythematosus is, it is worth following the process of development of the disease. Third-party factors affect the body’s immune system, stimulating failure and the production of antibodies to “native” cells.
The human body perceives its tissues and organs as foreign objects and begins a “ self-destruction program ”.
This body response is classified as a pathogenic phenomenon and stimulates the progression of inflammation and inhibition of healthy cells .
Typically, connective and vascular tissue cells are the scapegoat. When the disease actively progresses, damage to internal organs and systems cannot be avoided.
Symptoms of lupus depending on the stage of the disease
Lupus erythematosus has 3 stages and progressions, each of which differs in clinical manifestations:
- Spicy . The disease progresses rapidly, the patient experiences fatigue and complains of muscle pain. Body temperature “jumps” to 39-40 degrees. Within 30 days, the disease spreads to all human organs and systems.
- Subacute . “Clinic” is not as obvious as in the first case. More than 12 months may pass from the moment of infection to the appearance of the first symptoms. The pathology is replaced by periods of exacerbations and stable remission.
- Chronic . The course of the disease is sluggish, signs are few, organs and systems are not affected.
Classification
Lupus erythematosus - what kind of disease is it, is it contagious? These questions have already been answered above. Now it is necessary to consider in more detail the varieties of this disease. After all, each of them has its own characteristics.
Cutaneous form
It primarily affects the skin, which is constantly exposed to ultraviolet rays. Has 3 subspecies:
- acute;
- subacute;
- chronic.
Mainly manifests itself:
- butterfly rash;
- round spots covered with scales that are raised above the skin (in appearance, such rashes are similar to the lesions that occur with psoriasis);
- a rash on the head and ears that has a red-violet tint.
IMPORTANT! Exposure of the affected areas of the skin to sunlight only worsens the course of the disease. And when it takes a chronic form, internal organs begin to be involved in the pathological process.
The disease affects almost all tissues and organs, causing disruption of their functionality and the appearance of various, at first glance, unrelated symptoms.
Neonatal form
Diagnosed in newborns. Neonatal lupus erythematosus begins to develop in a child during the period of intrauterine development, when maternal antibodies attack the fetus. However, women themselves may not have the disease at all during pregnancy. It may develop much later.
The neonatal form of the disease manifests itself with the following symptoms:
- anemia;
- butterfly-type rash on the face;
- liver dysfunction.
With timely detection and adequate treatment, the neonatal form of lupus erythematosus disappears in infants after 5-6 months.
Is prevention possible?
There are no preventive measures for this disease, but following certain rules will help reduce the severity of its symptoms and increase the duration of periods of remission, and people with a predisposition will help avoid the onset of SLE.
Recommendations:
- strengthen the immune system with a healthy lifestyle, a balanced diet, and periodic courses of vitamin supplements;
- promptly and completely treat identified pathologies, especially infectious ones;
- Avoid self-medication, and coordinate any drug therapy with your doctor.
In sunny weather, it is not recommended to stay outside for a long time and/or often. When necessary, use sunscreen.
Diagnostics
Diagnosis of systemic lupus erythematosus primarily involves a visual examination of the patient and a history. If the doctor suspects this particular disease, the patient is prescribed a consultation with specialists of a narrower profile - a rheumatologist and a dermatologist.
The final diagnosis is made based on the presence of manifestations in each symptomatic group:
- from the skin: erythemic lesions of the butterfly type, discoid rash, dermatitis are detected;
- from the joints: arthralgia, “pearl bracelets” syndrome is observed, which occurs against the background of deformation of the articular tissues;
- from the internal organs: serositis, cylinduria, proteinuria are detected;
- from the central nervous system: frequent mood swings, psychosis, convulsions;
- on the part of hematopoiesis: thrombocytopenia, lymphopenia, leukopenia are detected.
Additionally, blood tests are performed to rule out other medical conditions and identify symptoms of systemic inflammation, and an antinuclear antibody test is performed to diagnose autoimmune disorders.
A negative antinuclear antibody test result does not exclude the presence of an autoimmune disease
To exclude the presence of complications from the heart and respiratory system, the following must be carried out:
- X-ray examination of the lungs;
- echocardiography.
Treatment of SLE in Moscow
Systemic lupus erythematosus requires timely diagnosis and correct treatment with the selection of ongoing therapy. You can undergo a full examination to identify systemic lupus erythematosus in Moscow in the Yusupov Hospital. The clinic is equipped with modern equipment that allows for a full range of diagnostic measures necessary to make an accurate diagnosis. Based on the data obtained, highly qualified staff of rheumatologists selects individual treatment in accordance with the stage of development of the disease. You can make an appointment with a doctor, as well as find out more about prices by phone or on the official website of the Yusupov Hospital.
Author
Dmitry Nikolaevich Staroverov
Head of the department of anesthesiology and resuscitation with intensive care and intensive care wards - anesthesiologist-resuscitator
Treatment
Systemic lupus erythematosus is a chronic disease. Unfortunately, it is impossible to get rid of it completely. However, there are still some therapeutic strategies that help effectively combat the manifestations of the disease and prevent the development of complications.
Treatment in each case is selected individually. Moreover, the chosen treatment approach may change over time, it all depends on the rate of progression of the pathology and the general condition of the patient. Replacing the selected treatment may also occur due to the fact that medications that previously helped began to provoke adverse reactions or began to act less effectively. It is for this reason that patients with SLE are recommended to regularly visit their doctor in order to adjust the therapeutic plan if necessary.
As a rule, drug therapy is prescribed for lupus erythematosus. It includes various drugs:
- Immunosuppressants. The action of drugs from this pharmacological group is aimed at suppressing the activity of the immune system, reducing its ability to attack the body. Such properties make it possible to slow down the development of SLE, but they negatively affect human health, because the body’s resistance to infections is reduced and the risks of other serious diseases increase several times.
- Painkillers. Most often, patients are prescribed non-steroidal anti-inflammatory drugs. They help relieve inflammation and relieve muscle and joint pain.
- Corticosteroids. These drugs help relieve swelling and pain. Such medications are prescribed both in the form of tablets and injections, and in the form of ointments. The latter cope well with skin manifestations of the disease.
- Antimalarials. They help fight pneumonia, pain and rashes on the body.
- BLyS-specific inhibitors. Taking these medications helps prevent people from developing abnormal B cells that create autoantibodies.
- Symptomatic remedies. They are selected individually, depending on what other symptoms of lupus erythematosus the patient has. For example, these could be drugs for high blood pressure or osteoporosis.
Living with lupus erythematosus becomes a real challenge for many patients. They are deeply concerned that they have no control over their body and life. Constant fatigue and weakness interfere with the performance of usual duties at work, which creates financial difficulties due to which the patient cannot provide the necessary treatment for himself. Against this background, depressive states and psychoses arise. And to improve their mental health, many people suffering from lupus are advised to see a therapist.
Treatment methods
The disease SLE is incurable, however, it is possible to stop the immune and inflammatory processes for a long time with the help of drug therapy, which will reduce the symptoms that arise and allow the patient to live quite fully.
Treatment is prescribed purely individually, it depends on the severity of the disease and the characteristics of the patient’s body, and can change during the course of the disease.
The following drugs are used for maintenance therapy for SLE:
- drugs aimed at combating inflammatory processes - glucocorticosteroids (prednisolone, hydrocortisone, etc.);
- medications that suppress the immune system - cytostatics (cyclophosphamide, azathioprine, etc.);
- antimalarials - Immard, Plaquenil, hydroxychloroquil;
- non-steroidal anti-inflammatory drugs - diclofenac, ibuprofen, etc.;
- medications to relieve symptoms.
The main treatment for SLE are glucocorticoid hormonal drugs, which are prescribed in huge doses, but they save the lives of thousands of sick people, however, such therapy is fraught with many side effects - heart disease, osteoporosis, increased blood sugar and cholesterol levels in patients, as well as the occurrence of infectious diseases of moderate severity.
Treatment for discoid lupus erythematosus differs from that for SLE. It is mainly aimed at eliminating the symptoms of skin manifestations, that is, local use of drugs, however, some drugs are prescribed orally - it all depends on the severity of the disease.
I would like to talk about the principles of treating SLE using oriental medicine methods. There, first of all, therapy is aimed at harmonizing the patient’s emotional state. Next, a personal diet is developed for each patient, which plays an important role in the course of the disease.
Eastern healers have a rule - no hormonal treatment - recovery occurs through special procedures:
- Tibetan massage of the patient's body using biologically active points;
- treating affected areas of the skin with herbal infusions;
- acupressure, acupuncture, which relieve swelling, inflammation, relieve itching and remove redness;
- moxotherapy - exposure to bioactive points with the tip of a wormwood or charcoal cigar - has a warming effect and removes toxins;
- Horme oil compress - soothes and relaxes;
- cupping massage and much more.
And of course, herbal medicine, which is the basis of oriental medicine. It helps strengthen the immune system, improve regeneration processes and activate blood flow, and most importantly, establish balance in the body.
Nutrition
Diet plays an important role in systemic lupus erythematosus. It helps not only the body cope with the disease, but also improve the condition of dermatological manifestations. Patients are recommended to include in the menu:
- vegetarian soups;
- meat and fish soups cooked in recycled broth;
- dietary varieties of poultry and rabbit meat (allowed only in boiled or baked form);
- lean fish;
- cereals prepared in the form of porridges or side dishes;
- chicken egg white;
- crackers, brown bread;
- low-fat cottage cheese;
- vegetable oil, unsalted butter;
- cheese, but only mild and unsalted;
- dairy products;
- vegetables and fruits (raw, boiled, stewed, baked);
- marshmallows, marshmallows, marmalade;
- green tea;
- vegetable and fruit juices;
- chicory;
- still alkaline mineral waters;
- rosehip decoction.
With SLE, dietary nutrition must be followed constantly
Persons who have been diagnosed with lupus erythematosus are strictly prohibited from eating the following foods:
- concentrated meat and fish broths;
- fatty meats, offal;
- sausages;
- canned food;
- smoked meats;
- pickles, marinades;
- cooking and animal fats;
- sauces (mayonnaise, ketchup, etc.);
- products containing starch, yeast;
- cocoa;
- coffee;
- chocolate;
- Black tea;
- fatty varieties of fermented milk products;
- confectionery;
- legumes;
- vinegar;
- honey, jam, preserves;
- whole milk;
- seafood;
- alcoholic and carbonated drinks.
Your doctor should tell you more about what you can eat if you have lupus erythematosus and what you can’t. Only by following all his recommendations can the patient learn to cope with the manifestations of the disease.
Systemic lupus erythematosus is a serious disease that is fraught with dire consequences. But thanks to new modern methods of its treatment, they occur extremely rarely. As for the prognosis, it is individual. On average, life expectancy after diagnosis is 25-30 years, but only if all doctor’s recommendations are followed.
Causes
Today, dermatologists continue to study the probable causes that can cause the development of discoid lupus erythematosus. The most common reasons for its occurrence include the following factors:
- mechanical damage to the skin - most often, it is with rough influence on the skin of the face that (mainly) the initial manifestations of the disease are noted, its functioning worsens, and signs of atopic processes are also noted, followed by atrophy of the upper layer of the epidermis;
- frostbite of the skin - even small areas of frostbite become the main foci of inflammatory and atrophic processes, where the skin loses most of its elasticity, becomes thinner and more susceptible to mechanical stress;
- infectious diseases that undermine the protective functions of the skin;
- taking a number of medications.
A general decrease in immunity, the presence of a number of hidden ongoing diseases also become the reasons for the development of this type of lupus. The skin also loses its protective qualities when exposed to ultraviolet (artificial and solar) rays for a long time, or when exposed to excessively high and low temperatures.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 5.1 | 3.2 | 3.2 | 2.4 | 0.7 | 0 | 0 | 5.1 | 14.4 | 14.4 | 10 | 4 |
Diagnosis of the disease
At the very beginning, DLE can easily be confused with diseases such as:
- psoriasis;
- pink acne;
- allergy;
- eczema;
- seborrheic dermatitis;
- ringworm;
- lymphoplasia;
- sarcoidosis, which begins with skin lesions.
To make a correct diagnosis, you need to contact your attending physician, who will prescribe the necessary measures, which include a blood test, and in order to also exclude other types of diseases, the following is carried out:
- histological examination (a piece of affected skin is checked in the laboratory);
- microscopic examination of scales and hair to identify the causative agent of the disease;
- immunofluorescence study - they look at how antigens interact with antibodies.
After conducting such tests, as well as a visual examination of the condition of the skin, the doctor will make a diagnosis with 100% accuracy.
Symptoms and first signs
The first signs of this skin lesion include the following manifestations:
- the appearance of red spots on the skin, which stand out on the skin due to their swelling and discoloration;
- the surface of these stains gradually dries out and becomes covered with dry particles that can be removed independently;
- spots constantly increase in size, their middle part becomes thinner and subject to mechanical stress;
- the spots gradually merge into one large affected area.
There is also infiltration of the skin in the affected areas, swelling becomes more and more pronounced, the skin in areas of greater manifestation of the disease is covered with scales, under which there are keratinized skin plugs in the form of sharp spikes.
Lifestyle
Treating an illness does not guarantee good health. People with lupus erythematosus are forced to adhere to a certain lifestyle in order to maintain a normal condition, eliminating the development of complications. This applies to many factors and is a prerequisite for therapy.
Effect of UV rays
You should be exposed to ultraviolet rays as little as possible. It is advisable to avoid sun exposure to the skin altogether. The same goes for UV lights, which are often used in dance clubs. If you do not follow these recommendations, your lupus may worsen, and the disease will be accompanied by even more dangerous symptoms.
If you need to go outside for a long time in sunny weather, you should use a special ointment.
Support from loved ones
Even for an adult patient, the support of loved ones is of great importance. Many people believe that there is nothing terrible about illness and do not attach any importance to it. Some, on the contrary, treat it with excessive caution. All this can negatively affect a person’s psychological state, which will negatively affect lupus itself. It is very important that loved ones always support the patient, reassure him, and say pleasant things. Especially if a girl has lupus, because... often the appearance changes for the worse.
Sport
There are no restrictions on sports activities. The patient is advised to regularly do exercises, do gymnastics, walk a lot, and be in the fresh air. However, when engaging in active sports that require you to be outdoors, you must use sunscreen and appropriate clothing. It is advisable to avoid sports during periods of strong solar activity.
Diet
Patients should follow a simple diet. It is enough to eat a healthy, balanced diet, excluding overeating and hunger strikes. If treatment involves taking corticosteroids, you need to devote more space in your diet to foods containing reduced amounts of salt and sugar. This will avoid an increase in blood pressure, as well as the development of diabetes with weight gain. Additionally, it is recommended to consume foods that are rich in vitamin D and calcium.
Cloth
As already mentioned, it is important to avoid exposure to sunlight. To do this, you must always wear long sleeves and apply cream to your skin. It is recommended to wear a wide-brimmed hat to reduce sun exposure to the scalp and face. You should dress properly even on cloudy days, because... Ultraviolet light penetrates clouds and hits the skin.
Vaccinations
Children with lupus are at increased risk of infection. For this reason, vaccination against all kinds of infections is very important, therefore the vaccination schedule should be followed as strictly as possible. It should be noted that their need is determined by the severity of the disease, as well as the prescribed treatment.
The patient can attend school, except during periods of exacerbation and the occurrence of severe complications.
Sexual life, pregnancy
There are no restrictions on sex life. However, caution should be exercised and contraception should be used if the disease is in an active phase. It is recommended to use condoms, because... Some birth control pills that contain estrogen cause flare-ups of lupus.
Pregnancy must be carefully planned. It is important that it occurs during remission. Otherwise, there is a high risk of miscarriage. Throughout pregnancy, the patient should be under special medical supervision. Most women can give birth without problems despite the disease. However, some medications used against lupus can adversely affect the fetus. Even with the right lifestyle and high-quality medical supervision, there is a risk of premature birth.
The incidence among newborns is 3%. In the first weeks of a child's life, he may be diagnosed with neonatal lupus, which can be transmitted from the mother. This type of disease, as a rule, goes away on its own in the first six months of life.
Some children whose mother had lupus develop heart problems.
Visit doctor
Patients should visit their doctor regularly. He must be informed of the occurrence of any unpleasant symptoms, because this may be a signal of an exacerbation of the disease. If necessary, you should consult a dermatologist, cardiologist and other specialists. Children require special attention, because... For them, lupus is more dangerous. The frequency of tests and examinations is determined by the doctor, based on the medical history.
How is SLE traditionally treated?
It is necessary to begin treatment for systemic lupus immediately as soon as such a diagnosis is made. But in most cases, this disease is detected late, since false diagnoses associated with seborrhea, eczema and photodermatosis are first made.
It is important not only on time, but also to choose the right therapy for SLE. Then it will be possible to avoid complications leading to human disability. Typically treatment consists of the following steps:
- drug therapy;
- healthy lifestyle;
- skin surface treatment;
- immunosuppressive therapy.
Medicines
To eliminate pain, the doctor prescribes non-steroidal anti-inflammatory drugs. In addition to this, the following is written:
- glucocorticosteroids, which protect internal organs from subsequent damage;
- cytostatic drugs;
- inhibitors that stop the progression of inflammatory processes;
- hormonal drugs that eliminate unpleasant symptoms of the disease.
During drug therapy, the doctor monitors the patient's condition. He may reduce the dosage of prescribed medications or make certain adjustments.
Complex therapy
In addition to taking medications, the patient is advised to follow the following recommendations:
- lead a healthy lifestyle;
- stop smoking and drinking alcohol;
- Do regular moderate exercise;
- balance your diet;
- maintain a comfortable internal state;
- avoid stressful situations.
People with systemic lupus erythematosus should avoid direct sunlight.
You need to wear clothing that covers the affected areas of the body. The skin surface will need to be treated with external preparations:
- non-hormonal ointments;
- corticosteroid drugs.
Why is the disease dangerous?
The danger of chronic lupus does not lie in the rash itself, which covers the skin of the face and body. The problem is much more complicated, because during the course of the disease, the internal organs of a person are destroyed and their functional ability is reduced. Also, with DLE, joints and connective tissue suffer, alopecia appears, but the most dangerous are damage to the kidneys and central nervous system.
Autoimmune kidney damage leads to chronic renal failure, the need for regular hemodialysis and even a kidney transplant.
When the central nervous system is damaged, mental disorders occur; patients often suffer from obsessions and delusions. But such changes in the functioning of the central nervous system are characteristic of late stages of the disease if treatment is not started in a timely manner.
ethnoscience
Treatment with medications will be much more effective if they are supplemented with traditional methods.
Here are the most effective:
- Boil a couple of teaspoons of mistletoe leaves (a parasitic plant that lives on birch trees), prepared in cold weather, in one and a half glasses of water and cover to infuse properly. Take the decoction three times a day, half a glass with meals. Be extremely careful - the mistletoe plant is poisonous!;
- An ointment made from birch buds, which are ground in the amount of one glass and mixed with half a kilogram of lard, will greatly help you in the fight against DKV. Apply this ointment to lupus spots three times a day or leave overnight. You can take this mixture orally with milk, one teaspoon per day;
- and here bee products will help you - collect a tablespoon of dead fruit and pour a glass of medical alcohol into it. This medicine is infused for three weeks. This infusion, diluted 1:1 with water, is used to make lotions that help relieve inflammation. After the procedure, the skin pathology is lubricated with an ointment based on birch buds.
Prevention of the disease
Now you know what symptoms accompany lupus, what kind of disease it is. Photos of the symptoms of this disease are also presented in the materials of this article. Is it possible to prevent its development?
According to experts, high-quality methods for preventing this disease have not yet been developed. However, it is possible to prevent the occurrence of relapses and maintain the condition of patients in stable remission. First of all, it is necessary to undergo regular examination by a rheumatologist and take prescribed medications in the recommended dosage. If side effects occur, you should consult your doctor again. It is extremely important to maintain a work-rest schedule and sleep at least eight hours a day. Eating a balanced diet is another step towards preventing relapses.
When a diagnosis of lupus erythematosus is made, the cause of the disease must be explained by a doctor. The patient should remember that this pathology is “afraid” of surgical interventions, hypothermia and does not accept a “chocolate tan.” Patients with lupus should forget about vacationing in southern latitudes for the rest of their lives.
What tests need to be taken
At your appointment, your doctor will suggest doing the following tests, which will help identify certain components contained in the blood, the amount of which increases with DLE:
- a detailed blood test that will help assess the number of leukocytes, red blood cells, platelets, red blood cells, as well as check hemoglobin, any change in which likely indicates the presence of the disease;
- Analysis of urine. Since lupus can lead to kidney damage, it will show whether there is protein, squamous epithelial cell particles, blood cells, as well as sugar and nitrates in the urine. High protein levels may indicate that kidney dysfunction is occurring;
- biochemistry analysis, which will give a picture of the presence of proteins in the blood that attack their own cells, which will finally confirm the diagnosis of DLE;
- a study on ESR will show whether there is an inflammatory process in the body;
- blood test for antibodies to nuclear antigens. If they are detected, the diagnosis will not be in doubt.
All these studies will help assess the patient’s condition and prescribe the necessary treatment.
How to live with lupus?
If you have been diagnosed with this disease, it does not mean that you can give up on yourself. Many people live with a diagnosis of lupus. Photos of such patients clearly prove that it is simply necessary to fight the disease. You will probably have to make some changes to your usual lifestyle. Doctors recommend resting as needed. It is better to lie down several times a day than to work too hard.
Study the main symptoms indicating the transition of the disease to the acute stage. It is usually preceded by severe stress, prolonged exposure to the sun, and a cold. If you avoid these triggers, life can become much easier.
Don't forget about regular physical activity, but you shouldn't overwork your body either. You can choose Pilates or yoga as your main sport. On the other hand, it is necessary to give up all bad habits. Smoking and drinking alcoholic beverages do not improve your health. Such people get sick more often and overload their heart and kidneys. You shouldn't risk your own life for a moment's pleasure.
Accept your diagnosis and consult your doctor if necessary. The specialist should tell you how lupus develops and what kind of disease it is. Photos of patients living with this disease can motivate you to continue to actively fight it.
Particular attention must be paid to the diet. It is recommended to abandon all harmful products, because they negatively affect the functioning of the main systems of internal organs. Caffeine and products containing it are also prohibited. This substance makes the heart beat faster, does not allow it to rest, thereby overloading the central nervous system. The diet should consist of lean meat, fish in large quantities, as well as vegetables and fresh fruits. Don't forget about dairy products. They contain healthy amounts of calcium and vitamin D, which helps prevent osteoporosis.
Symptoms of the disease
Depending on the intensity of the disease, symptoms may manifest in different ways. The main ones:
- the appearance of pink-red spots of different sizes, covered with scales. If you tear it off, pain occurs, and a crust appears in place, similar to the surface of a lemon;
- the occurrence of skin atrophy (thinning) with pronounced scars;
- accumulation of fluid in the lesions;
- thickening of the stratum corneum of the epidermis;
- itching and burning;
- in 15% of cases the oral cavity is affected - ulcers appear on the mucous membrane;
- Sometimes there is hair loss and joint pain.
The appearance of areas with pronounced pigmentation may also occur. Spider veins may appear on the spots. The rashes have different sizes, ranging from 3 mm. They can be either single or multiple. Lesions occur most often on the face (cheeks, nose, scalp and neck). Less commonly, in severe cases, spots appear on the arms, back, stomach, shoulders, and eyes.
Forms of the disease
There are three forms of the disease.
The acute form is characterized by:
- an abrupt onset, when the patient can name a specific day;
- high temperature, chills;
- polyarthritis;
- rash and the appearance of a “lupus butterfly” on the face;
- cyanosis (blueish skin color) on the nose and cheeks.
Within six months, signs of acute serositis (inflammation of the serous membranes of the pericardium, pleura, peritoneum), pneumonitis (inflammation of the lungs with damage to the alveolar walls), neurological and mental disorders, seizures similar to epileptic ones develop.
The course of the disease in its acute form is severe. Life expectancy without active therapy is no more than a year or two.
The subacute form begins with manifestations such as:
- general symptoms of lupus erythematosus;
- pain and swelling of small joints;
- arthritis with relapses;
- skin lesions such as discoid lupus (ulcerations on the skin, flaky, covered with scales);
- photodermatoses appearing in the neck, chest, forehead, lips, ears.
The undulation of the course of the subacute form is manifested quite clearly. Over a period of 2–3 years, a complete clinical picture is formed.
Noted:
- Persistent paroxysmal headaches, high degree of fatigue.
- Severe heart damage in the form of Libman-Sachs endocarditis and inflammation of the valves - mitral, aortic, tricuspid.
- Myalgia (muscle pain, even at rest).
- Inflammation of muscles and skeletal muscles with their atrophy - myositis.
- Raynaud's syndrome (blue or whitening of the skin of the tips of the fingers or feet during cold, stress), often leading to necrosis of the tips of the fingers.
- Lymphadenopathy is a pathological enlargement of lymph nodes.
- Lupus pneumonitis (inflammation of the lungs in SLE, developing in the form of vasculitis or atypical pneumonia).
- Inflammation of the kidneys, which does not become as severe as in the acute form;
- Anemia, leukopenia (severe reduction in the number of white blood cells), thrombocytopenia or Wellhoff syndrome (a sharp decrease in platelets in the blood, which is accompanied by bruises, hematomas on the skin, mucous membranes, bleeding and difficulty stopping bleeding even after minor injuries).
- Increased concentration of immunoglobulins in the blood.
Chronic form
The disease lupus erythematosus, which occurs in a chronic form, is expressed for a long time in frequent polyarthritis, manifestations of discoid lupus, lesions of small arteries, and Wellhoff syndrome.
During 6–9 years of the disease, other organic pathologies (nephritis, pneumonitis) occur.
Treatment: discoid lupus
Only a specialist can prescribe effective treatment. First of all, the skin must be protected from injury and excess heat using special creams.
When diagnosed with lupus erythematosus, the following medications are prescribed::
- Photoprotective creams and ointments;
- Antibiotics of the penicillin group;
- Antimalarial drugs – Plaquenil, Hingamin;
- Complex drugs.
For effective treatment of discoid lupus, a comprehensive medication regimen is required, combining drugs from different groups. It is necessary to remember about individual intolerance to some components of medications, so the course of treatment should be selected only after a thorough examination and consultation with the attending physician, taking into account all the characteristics of the patient. During treatment, it is advisable to change the diet - include foods containing nicotinic acid (vitamin PP): cod, beef liver, beans, nuts, buckwheat and oatmeal.