Causes of subcutaneous paraproctitis
The main reason for the formation of purulent formations in the pararectal area is harmful microorganisms that colonize the rectum.
Most often these are anaerobic bacteria, enterococci, staphylococci and E. coli. They penetrate into the subcutaneous layers, which leads to a pronounced inflammatory process. Such microorganisms are capable of infecting any cellular space located close to the rectum, and in rare cases, several different areas at the same time. Why is subcutaneous paraproctitis dangerous? The main causative agents of acute subcutaneous paraproctitis are able to penetrate into the subcutaneous layers through wounds and ulcers, Morgagni crypts and anal sinuses. Moreover, they can infect almost any cellular space located near the rectum: submucosal layer, fat layer, pelvic area, etc.
There are factors whose presence contributes to the occurrence of pathology. These include:
- the presence of cracks and wounds near the anus;
- digestive system disorders causing diarrhea and constipation;
- haemorrhoids;
- sexual intercourse performed rectally;
- diabetes;
- weakened immunity.
What is paraproctitis?
The cause of inflammation is infections, most often such as Escherichia coli (Escherichia coli), Proteus, streptococci, staphylococci.
In the immediate environment of the rectum, three fascial-cellular spaces are distinguished: subcutaneous, ischiorectal and pelvic-rectal.
Depending on which of the spaces is affected by inflammation, paraproctitis can be of three types:
- subcutaneous paraproctitis,
- ischiorectal paraproctitis,
- pelvic-rectal paraproctitis.
According to the nature of the course, acute and chronic paraproctitis are distinguished.
Symptoms of subcutaneous paraproctitis
In medicine, there are several groups of signs that characterize this type of disease:
- Severe sharp pain in the anus: tugging, shooting, which appears almost from the first days of the onset of the disease and gradually increases. Most often, during defecation there is an increase in pain.
- A rise in body temperature to 39° C, with chills, pain in muscles, joints, bones, and loss of appetite.
- Diffuse, severe redness of the skin in the painful area near the anus. Palpation of this area is painful. The skin is swollen, somewhat thickened, and feels elevated to the touch.
If you have such symptoms, you should immediately consult a specialist.
Symptoms of manifestation
Subcutaneous paraproctitis in acute form is accompanied by pronounced manifestations. It is characterized by the following symptoms:
- Severe pain in the anal area. It is sharp, pulsating, very sharp. It can appear constantly, even while sitting. But it becomes more intense with intense physical activity.
- Hyperemia in the affected area, swelling of the skin.
- Problematic defecation. The inability to empty the bowels is associated with severe pain in the rectum. This may cause the patient to experience constipation. But in some cases, on the contrary, diarrhea is observed, which is also considered characteristic of subcutaneous paraproctitis.
- General deterioration in health. The patient suffers from chills, weakness, and insomnia.
Severe pain in the anal area is a symptom of subcutaneous paraproctitis.
Also, with acute paraproctitis, a fistula can form - a large hole through which pus is released. Requires immediate treatment.
If the disease is not treated, a chronic form of pathology develops. Accompanied by acute phases and periods of remission. It is characterized by the following symptoms:
- Bloody discharge from fistula openings. May contain purulent impurities.
- There is practically no pain, only occasionally the affected area may ache.
- Bloody discharge irritates the skin in the perineum. This patient may experience constant itching.
When the fistula becomes clogged with dead cells or pus, the acute phase begins with characteristic symptoms. Even if the fistula hardly bothers you, you need to see a doctor urgently, since it does not go away on its own, so sooner or later new manifestations will appear.
Diagnosis of the disease
If painful symptoms appear in the area of the rectum or anal sphincter, you should seek help from a competent specialist who will prescribe a diagnostic examination, make a diagnosis and prescribe treatment.
In addition to interviewing the patient and external examination of the painful area, the doctor performs the following procedures:
- Digital examination of the rectum. At this time, swelling of the intestinal wall, swelling and the location of a painful abscess are determined.
- Fistulography is a diagnostic that allows you to clarify the size of the abscess and the boundaries of the lesion. For subcutaneous process it is prescribed in some cases.
- General blood analysis. This analysis allows you to determine leukocytosis and ESR.
- Ultrasound. Helps to accurately determine the location of the purulent tract, leaks of pus, the location of the abscess and the presence of cavities.
- Bacteriological culture. Laboratory research to determine the flora that caused the process.
Causes of the disease
The causes of paraproctitis that trigger pathological processes are:
- anal area injuries;
- violation of defecation - constipation, diarrhea;
- colitis, nonspecific ulcerative colitis;
- Crohn's disease;
- hemorrhoids, anal fissure;
- inflammatory diseases of female organs;
- prostatitis;
- decreased immunity due to viral diseases;
- poor nutrition;
- inadequate physical activity;
- alcohol, smoking.
The phenomenon of “dormant infection” is known, when after surgical removal of an abscess, a small focus of inflammation remains in the rectum. Under unfavorable conditions, repeated paraproctitis occurs. This happens from a poorly cleaned abscess. The infection can penetrate for a second time through rectal fissures.
Treatment of subcutaneous paraproctitis
If purulent paraproctitis develops, you should not try to cure yourself, as this can only aggravate the situation and lead to complications of the disease. As a treatment for subcutaneous paraproctitis, surgical intervention and non-surgical methods - drug therapy and effective folk remedies - are used to open the abscess. Dietary nutrition is also recommended for patients.
Acute paraproctitis
Acute paraproctitis is a purulent inflammation of the tissue surrounding the rectum.
The infection penetrates the tissue from the rectum. This can occur when its mucous membrane is damaged and a defect forms in it, through which the infection easily penetrates into the tissues surrounding the rectum.
Injuries to the rectum are usually the result of mechanical force. This may be a small, literally pinpoint, tear of the mucous membrane caused by
- injury,
- small rupture of the internal hemorrhoid,
- anal fissure,
- accidentally swallowed fish bone,
- a sharp fruit pit,
- poorly chewed and overcooked peels from fruits and vegetables.
The cause of paraproctitis is persistent constipation, which is accompanied by hard “sheep” feces. Its passage through the rectum can injure the mucous membrane.
Frequent loose stools with undigested food debris irritate the rectal mucosa and can also lead to microtrauma.
If the infection penetrates the anal glands and a blockage occurs, then in this case acute purulent paraproctitis develops.
Paraproctitis: symptoms
All types of acute paraproctitis are characterized by common symptoms:
- sharp throbbing pains,
- high body temperature,
- chills,
- a significant shift to the left in the blood test: ESR increases, leukocytosis appears.
Each type of paraproctitis has its own characteristic symptoms.
Subcutaneous paraproctitis
A purulent abscess forms in the subcutaneous fatty tissue. If the abscess is located closer to the anus, then compaction and pain appear near the anus. When light pressure is applied to the abscess, it moves.
With a deeper location, there is no redness or thickening.
Body temperature rises to 37.5-38 ºС. When an abscess is formed, the temperature may be higher.
Ishiorectal paraproctitis
With this type of proctitis, a dull pain appears, the body temperature rises to 38 ºС, and a general feeling of malaise is felt.
Redness of the skin is usually absent. A digital examination of the rectum reveals a compaction that bulges into the lumen of the rectum. The examination causes sharp pain.
Pelvic-rectal paraproctitis
This form of paraproctitis is the most severe.
The abscess is located high, under the pelvic peritoneum. Its symptoms are similar to another type of paraproctitis - retrorectal paraproctitis. In this case, the abscess is located behind the rectum.
The condition of patients in these cases is severe, general intoxication of the body is observed, body temperature rises to 40 ºС. However, local signs (changes in the anus) are very mild.
Such forms of paraproctitis are often not immediately recognized and are mistaken for pneumonia or some kind of infectious disease.
Diagnostics
The main research method is digital examination of the rectum.
In the presence of an abscess located high in the pelvic-rectal tissue, there may be no protrusion into the intestinal lumen, but upon digital examination, acute pain is sure to occur, radiating to the pelvis.
To determine the position of the internal fistula, methylene blue is injected into the abscess cavity. When a sterile probe-tampon (tumper) is inserted, the position of the fistula is determined by the location of the blue spot.
Paraproctitis can be detected by colonoscopy.
Treatment of acute paraproctitis
If an abscess has formed, urgent surgery is necessary. It involves opening the abscess and draining it.
If the compaction is small and the temperature is not high, then you can try to cure paraproctitis without surgery.
As a treatment, it is necessary to take hot (37-38 ºС) baths with potassium permanganate for 15-20 minutes. After the bath, a suppository is inserted into the rectum.
For the treatment of paraproctitis, a suppository is recommended consisting of belladonna extract 0.015 g, novocaine 0.12 g, xeroform 0.1 g, white streptocide 0.08 g, 4 drops of 0.1% adrenaline solution, cocoa butter 1.5-2 g. A compress of Vishnevsky ointment is applied to the anus. Before insertion, the candle must be generously lubricated with the same ointment.
Due to pain during defecation, bowel movements are incomplete, so it is recommended to do cleansing enemas.
If such treatment does not help, then the infiltrate grows and the body temperature rises. In this case, surgery is necessary.
How to do cleansing enemas is described in the article “Proctitis”.
If such treatment does not help, then the infiltrate grows and the body temperature rises. In this case, surgery is necessary.
Forecast
Timely and correct treatment results in complete recovery.
Prevention of paraproctitis
The main preventive measure is the prevention and treatment of constipation and diarrhea. Attentive attention to the digestive process, eating slowly, and thoroughly chewing food also reduce the likelihood of developing paraproctitis.
Surgical treatment
To treat subcutaneous and other types of paraproctitis, the surgical method is most often used. In most cases, doctors perform one-stage operations, since the boundaries and location of the abscess are known, and the surrounding tissues are not affected.
The manipulation is performed under general anesthesia. The doctor performs an autopsy of the source of inflammation and drains the abscess. Tissues affected by the purulent process are also removed. To minimize pain, the patient is prescribed special painkillers.
In the postoperative period, the patient is recommended:
- dressing the wound using regenerating drugs and antiseptics;
- physiotherapy;
- painkillers.
There are contraindications to performing a one-stage operation, these include:
- severe general condition of the patient;
- unknown location of the crypt, abscess and purulent tract.
In such a situation, specialists urgently open the abscess, clean it, and postpone the second stage of intervention for several days (usually no more than a week). The second stage of the operation involves removal of the affected gland and crypt.
After the operation, physiotherapeutic treatment with ultra-high frequencies, ultraviolet irradiation, and microwave therapy is recommended. The physiotherapist chooses the technique. Most often, 5-10 sessions are prescribed.
During the postoperative period, the patient requires additional care. The patient must perform dressings independently or with someone else's help. Monitoring by a surgeon or attending physician is also required once a week.
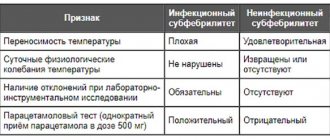
Signs of paraproctitis
(based on the results of laboratory and instrumental research methods)
A subcutaneous abscess has quite pronounced symptoms, but to complete the clinical picture and determine the severity of the disease, the patient must undergo additional examinations.
These tests will confirm the diagnosis and make it possible to determine the necessary treatment tactics.
- To obtain additional information about subcutaneous paraproctitis, the patient must undergo a general blood test. An increase in the erythrocyte sedimentation rate, an increase in the level of leukocytes and a shift in the formula to the left are the main signs of the presence of a strong inflammatory process in the human body.
- To clarify the boundaries of the pathological focus and its size, it is advisable to use fistulography. Using this research method, it is possible to determine the presence of fistulas, their direction and extent. Diagnosis is carried out using a radiopaque contrast agent. The resulting picture allows us to determine the degree of damage to the subcutaneous fat and decide on further treatment.
- In case of acute paraproctitis, the doctor may recommend an ultrasound examination of the abscess using a rectal sensor. This method will allow us to determine the location, its size and the presence or absence of fistulas with millimeter accuracy. Data on subcutaneous paraproctitis obtained using ultrasound will help confirm the diagnosis.
If the first signs of an abscess in the anus occur, you should consult a doctor as soon as possible to decide on immediate treatment. There is no need to wait for your health to worsen and try to cope with the problem on your own.
Timely measures should be taken to help achieve a quick recovery.
Folk remedies
Treatment of paraproctitis at home is used quite often in the form of complex therapy. If an illness occurs, it is recommended to use proven effective remedies:
- Sea salt baths. Dilute 2 tbsp in five liters of water. spoons of salt. Take cool baths (sitting) with the resulting solution.
- Infusion of plantain, yarrow and marshmallow root. Take 100 g of plantain and marshmallow, 80 g of yarrow, mix everything. Pour the mixture with 600 ml of hot water and leave overnight. In the morning, filter the prepared solution and take 150 ml 4 times a day.
- Rowan decoction. Pour 2 teaspoons of rowan fruit into 400 ml of hot water and leave for an hour. If desired, you can add sugar. Take 3 times a day before meals.
Medical therapy
Surgical and conservative methods are used to treat paraproctitis. An integrated approach is often used, which involves simultaneously performing surgery and prescribing medications. How and with what to treat the disease depends on its form, location of the lesion and the general condition of the patient.
Medicines
Drug treatment of acute paraproctitis involves the use of the following groups of drugs:
- Antibiotics. They are the main component of drug therapy. Broad-spectrum antibacterial agents are prescribed: Amikacin, Gentamicin, Ceftriaxone. The choice of antibiotic depends on the nature of the inflammation (purulent or putrefactive).
- Anti-inflammatory drugs. Nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed in a short course. The use of this group of drugs allows you to stop the inflammatory reaction, reduce pain, swelling, and redness of the skin.
- Saline solutions. Used for severe intoxication syndrome. Infusion of saline solutions can reduce signs of intoxication. Infusions of saline and Ringer are prescribed.
To treat the chronic form, systemic and local drugs are used. Systemic agents include antibiotics and anti-inflammatory drugs. The following local remedies are used:
- Antiseptic solutions for washing. For example, "Chlorhexidine", "Hydrogen Peroxide".
- Ointments and gels that have a wound healing effect. Such drugs have reparative properties and accelerate the healing of the mucous membrane. The most commonly used is Methyluracil Ointment.
- Rectal suppositories. Prescribed outside of an acute process. For example, “Proctosan”, “Relief”.
All medications must be prescribed by your doctor. Self-administration of medications can provoke the development of adverse reactions.
ethnoscience
It is impossible to completely cure paraproctitis at home. Folk remedies that are used for treatment have anti-inflammatory, antiseptic or wound-healing effects. For chronic paraproctitis the following are used:
- Sitz baths with herbs. Used during remission in chronic paraproctitis. Chamomile flowers, calendula, and mint leaves are used to prepare the bath.
- Compress with sea buckthorn oil. Apply to the affected area to speed up healing. You must first clean the area using antiseptic solutions.
- Microclysters. Used for cases of constipation. You can use a decoction of oak bark, an infusion of calendula and chamomile flowers as a basis.
In case of acute inflammatory process, it is not recommended to use traditional recipes. This can accelerate the generalization of infection and the spread of inflammation.
Radical techniques
The main method of treating paraproctitis is surgery. The surgical tactics depend on the form of the disease.
In the acute form of the disease, open surgery is performed, which consists of the following:
- opening of an abscess;
- washing the affected area;
- installation of drainage;
- search and removal of the source of infection (inflamed crypt).
The course of the operation depends on the location of the lesion.
In the chronic form of the disease, surgical intervention is also indicated. The operation consists of excision of the fistula. During the period of exacerbation, the purulent process is also opened, washed and drained.
Since the operation is performed under general anesthesia, there is a risk of death for the patient. Therefore, before performing surgery, you need to undergo a series of laboratory and instrumental studies and consult with an anesthesiologist.
Diet
For paraproctitis, it is important to follow a therapeutic diet. Proper nutrition can reduce the load on the intestines and speed up recovery. Nutrition during illness is based on the following recommendations:
- Eat more fiber. It is found in large quantities in fresh vegetables and fruits: apples, cucumbers, cabbage, zucchini. This allows you to form softer stools and prevent injury to the intestinal mucosa.
- Drink more fluids. This can be plain water, green and fruit tea, freshly squeezed juices, kefir.
- Add more cereals to your diet: buckwheat, oatmeal. This will also prevent the development of constipation.
- Avoid consuming fatty foods, flavorings and preservatives.
- Do not refuse first courses; eating them softens the stool.
Diet is an important component of treatment, without which recovery is impossible. You need to adhere to the diet not only during the period of therapy, but also after the end of treatment, to prevent relapses.
Diet food
After surgery, each patient is recommended to eat a diet, since diet is one of the important components in this disease.
In the postoperative period, the patient must:
- eat small meals 4 times a day;
- The diet must include first courses - low-fat broth or soup;
- You need to cook food steamed or boiled;
- eat fish and lean meat;
- drink enough fluids;
- exclude smoked and spicy foods from the diet, and also limit flour;
- stop smoking and drinking alcohol.
Forecast
The prognosis will depend on the stage of development of paraproctitis and the location of the abscess in the anal canal. With timely and correct treatment of the early stage, the result is positive.
Chronic, complicated acute purulent paraproctitis can reappear, especially when treating fistulas formed after an illness. A severe illness requires enormous efforts for the recovery to be final. Such therapy can last for several years and result in a cure.
We recommend: Symptoms and treatment of malabsorption syndrome in children
Complications of paraproctitis
If the first symptoms of this disease occur, you should immediately consult a specialist, since there is a possibility of dangerous complications:
- Formation of purulent fistulas between the vagina and rectum;
- Melting of the rectal wall. In this case, the contents may enter the perirectal tissue, which is fraught with serious consequences.
- Breakthrough of pus into the retroperitoneal tissue and abdominal cavity with retroperitoneal phlegmon and the development of peritonitis. These symptoms lead to sepsis and, as a result, death.
- Purulent melting of the urethra and the transition of the purulent process to the scrotum area, followed by gangrene.
- Skin necrosis in the area where the lesion spreads.
Classification of paraproctitis
The rectum is quite complex.
According to the nature of the inflammation, paraproctitis can be acute or chronic. In chronic paraproctitis, fistulous tracts are formed from the area of purulent inflammation, through which pus is constantly released onto the surface of the skin or into the lumen of the anal canal.
According to the localization of purulent leakage, paraproctitis is divided into:
- subcutaneous;
- submucosal;
- intermuscular;
- ischiorectal (ischiorectal);
- pelvic-rectal:
- pelviorectal,
- retrorectal,
- horseshoe-shaped.
According to the location of the purulent fistula:
- intrasphincteric;
- transsphincteric;
- extrasphincteric.
The surgical tactics and the likelihood of complications depend on the location of the lesion and the nature of the purulent tract.
According to the nature of the pathogen:
- aerobic;
- anaerobic:
- clostridial,
- non-clostridial.
This division is necessary for choosing a treatment method. Anaerobes - bacteria that exist without oxygen - cause more severe damage. Particularly dangerous are pathogenic anaerobes of the genus Clostridia, different types of which cause diseases such as tetanus, gangrene, botulism, and necrotic enteritis.
Prevention
To avoid the occurrence of subcutaneous paraproctitis, it is recommended to adhere to the following rules:
- maintaining normal body weight;
- do not lift heavy objects;
- prevention of constipation. It is necessary to achieve soft stools;
- The daily diet should contain foods rich in fiber (fresh fruits, vegetables) as well as fermented milk products (cottage cheese, kefir, yogurt). Limit the consumption of butter dough;
- If you have diabetes, you should maintain normal blood sugar levels;
- treatment of anal fissure and chronic hemorrhoids;
- compliance with personal hygiene rules.
To increase the effectiveness of treatment, it is necessary to lead an active lifestyle, exercise regularly, and support the immune system with the help of vitamin and mineral complexes.
Diagnostics
Paraproctitis can be suspected based on clinical data and physical examination. The doctor examines the perirectal area to identify swelling, redness, and pain. These signs indicate paraproctitis.
To diagnose the acute form of the disease, the following diagnostic methods are used:
- General blood analysis. Allows you to identify signs of bacterial infection and inflammation: an increase in the number of leukocytes, neutrophils, erythrocyte sedimentation rate (ESR).
- Finger examination. Allows you to identify the location of the abscess.
- Ultrasonography. Used in cases where inflammation is localized in the pelviorectal space.
To diagnose chronic paraproctitis, the following studies are used:
- Finger examination. Prescribed for exacerbation of the inflammatory process to identify the location of the lesion.
- Vaginal examination. Used for the discharge of pus from the vagina. This may indicate the presence of a rectovaginal fistula.
- Fistulography. The method involves injecting a contrast agent into the fistula. This allows you to visualize the fistula and its direction.
- Sigmoidoscopy. An additional research method that is used to assess the condition of the rectum.
- Sphincterometry. A method that allows you to assess sphincter tone.
Causes of paraproctitis
The causes of the development of the inflammatory process in the peri-rectal tissues may be:
- Haemorrhoids;
- anal fissures (anal fissures);
- inflammation of the anal glands.
In fact, paraproctitis is one of the complications of the listed diseases - it can only develop as a consequence of incorrectly performed/independently interrupted treatment.
First signs
Paraproctitis can be acute or chronic. The clinical picture and symptoms of both forms of manifestation of the disease differ.
Spicy
The disease during its acute manifestation can be characterized by symptoms of a common inflammatory phenomenon in the body. As a rule, body temperature rises (sometimes up to 390), weakness, muscle, joint and headache appear, and appetite disappears. The passage of feces and urine is disrupted: unnatural desires to defecate appear, constipation occurs, urination becomes more frequent and becomes painful.
Symptoms of paraproctitis directly depend on where the inflammation is localized. The subcutaneous form of paraproctitis is distinguished by the fact that the affected area is visible to the naked eye: the skin turns red, swells, the tissue is compacted, there is a tumor near the anus, in the anus. The patient cannot sit due to pain and therefore immediately seeks help from a doctor. The disease most often manifests itself in the subcutaneous form. When pressing and palpating, severe pain is felt. This is how the disease manifests itself in children.
Submucosal paraproctitis symptoms are similar to the subcutaneous type. The differences are that the body temperature does not rise much and the pain is not so pronounced. The abscess is located near the intestines and breaks into the rectum.
Difficulties in making the correct diagnosis arise with the pelvic-rectal form of the disease. They are due to the same symptoms for all forms of infectious diseases. The patient seeks help from various specialists; there are often cases when patients independently begin to treat what they consider to be a common respiratory disease. The focus of this form of paraproctitis is located deep, at the border of the abdominal cavity and the pelvic floor muscles.
This inflammation can last up to two weeks. During this time, the patient notes a noticeable deterioration in the condition of his own body. During defecation, in addition to feces, blood and pus are observed. At the same time, the temperature decreases and the severity of the pain syndrome decreases. This is how an abscess that opens directly into the rectum manifests itself. Representatives of the fairer sex often feel an abscess bursting into the vagina, and pus mixed with blood appears from the perineum.
Danger arises if a purulent abscess breaks into the abdominal cavity, causing peritonitis. Or into the intestines, which will lead to a more favorable outcome.
The ileo-rectal type of paraproctitis is characterized by the appearance of specific symptoms only on the seventh day. The course of the disease is characterized by difficulty in making a diagnosis in the first days. Only after a week has passed, the skin near the epicenter of inflammation turns red and swollen, and the buttocks become different sizes.
The most dangerous for the patient is necrotizing paraproctitis. This type is characterized by instant intoxication, severe pain covering the entire perineum. In this case, low blood pressure, an increase in heart rate and cyanosis of the skin are observed. The soft tissue dies. The process is not accompanied by redness and the appearance of pus; instead, necrosis and strong gas formation are observed - rotting with the release of “swamp” gas.
Necrotizing paraproctitis develops due to damage by putrefactive microbes, clostridia, fusobacteria, and anaerobic microorganisms.
If the abscess is opened by the patient himself or the course of treatment is chosen incorrectly, acute paraproctitis easily turns into chronic.
Doctor speaking! Under no circumstances should you self-medicate! This will only accelerate the transition of an acute purulent process into a chronic form, aggravate the condition, and will also contribute to the appearance of complications and tumors in the body.
Chronic
A condition in which there is a fistula in the anus and a constant inflammatory process is called chronic paraproctitis. For the most part, chronic paraproctitis is painless.
The most common reason why clinical paraproctitis occurs is improper treatment of its acute form or delay in seeing a doctor. The main complications that distinguish chronic paraproctitis are:
- fistula on the skin in the anus and buttocks;
- pus and feces are released from the fistula tracts;
- irritation and itching of the skin in the area of the fistula;
- pain during bowel movements.
The clinical picture of chronic paraproctitis can be characterized by alternating remissions and exacerbations of the disease. If the disease is not treated, consequences such as fecal incontinence and inflammation of the rectum are possible. If pus breaks through into the pelvic tissue, the sick person may die.
At the stage of remission of the disease, the patient only notices the discharge of pus mixed with blood and feces from the fistula canal in the anus. If the fistula cavity is not clogged, then the pain does not bother you. When the canal becomes clogged, an abscess appears in the perineal area, during the development of which new fistulas are formed. If the disease is severely advanced, branched fistula canals arise with a common epicenter in which the infection nests.
When the fistula channel is poorly drained, symptoms of acute paraproctitis are observed. During the acute period of the disease, a new fistula forms.
Doctor speaking! Chronic paraproctitis cannot be cured on its own. Each relapse worsens the disease and leads to tissue necrosis and the appearance of malignant tumors.
Paraproctitis is a dangerous disease that should not be neglected under any circumstances. The chronic form of paraproctitis is difficult to treat. For this reason, it is important not to transfer the disease to the chronic stage.
Types and their symptoms
Types of purulent paraproctitis and their main symptoms are presented in the table:
| View | Placement of purulent focus | Main symptoms |
| Subcutaneous | Deep under the skin around the anus | The appearance of a red swelling in the anus |
| Feeling of sharp or throbbing pain in the area of inflammation | ||
| Increase in body temperature | ||
| Violation of the process of defecation | ||
| Pelviorectal | At the border of the intestine and abdominal cavity | Weakness, aches |
| Signs of body intoxication | ||
| Urinary retention | ||
| Swelling of the mucous membrane | ||
| Strengthening the vascular pattern | ||
| Retrorectal | Posterior part of the rectum | Pain along the sciatic nerve |
| Fever | ||
| Submucosal | Under the intestinal mucosa | Abscess formation |
| Pain during bowel movements, indicating that an abscess has ruptured into the intestinal lumen | ||
| ischiorectal | Ischiorectal fossa | Severe pain radiating to the pelvis and intensifying with straining |
| Swelling in the hip area of the body | ||
| High body temperature | ||
| Smoothing anal folds |
In most cases of the disease, subcutaneous paraproctitis is diagnosed. A rare, but very serious type of disease is putrefactive paraproctitis (necrotizing). This pathology is characterized by a very rapid spread of the infectious process and is accompanied by multiple necrosis of the soft tissues of the intestine. If the abscess opens on its own during putrefactive paraproctitis, the following appears:
When the abscess is opened, systemic fever appears.
- systemic fever;
- severe weakness;
- intoxication;
- pain in areas of necrosis;
- discomfort during bowel movements.
Treatment of paraproctitis, operation and features
As mentioned above, conservative therapy for acute paraproctitis is impossible - it’s the same as trying to cure acute appendicitis - the outcome will be the same. If a diagnosis of “acute paraproctitis” is made, only charlatans can offer treatment without surgery.
- Moreover, you need to try to ensure that the operation is performed in a special proctology department, and by certified surgeons - proctologists.
And that's why:
In principle, this operation can be quickly performed in any purulent surgery department. But there is one small subtlety here: in the department of purulent surgery they will do what they are usually used to doing, namely: they will open the abscess, empty it, and drain the cavity.
Retrorectal paraproctitis
This case is also complex because the source of infection occurs behind the rectum. It does not manifest itself for a long time. There may only be symptoms of intoxication. Some patients complain of pain along the sciatic nerve. In such cases, the clinical picture has neurological symptoms.
Among the specific signs, it can be noted that with this disease, pain radiates to the perineum and thigh area. Sometimes there is also slight bleeding of the mucous membrane in the area of the ampulla and hyperemia.
It should be noted that only 1.5-2.5% of patients suffering from acute purulent paraproctitis have a retrorectal form indicated in their medical history. This is indeed a very rare case. But it is quite curable. After a digital examination and sigmoidoscopy, the doctor prescribes therapy that will help you heal quickly.
Forms and symptoms
Acute type of disease
Symptoms of acute paraproctitis are pronounced and fully manifested. In acute cases, rectal fistulas form, causing discomfort. The deviation begins with the following manifestations:
A symptom of the disease may be lack of normal sleep.
- painful sensations in the butt, aggravated by excretion of feces;
- a febrile state in which the body temperature rises;
- impaired bowel movement, in which constipation alternates with diarrhea;
- frequent urge to go to the toilet, which is most often false;
- signs of intoxication:
- general malaise;
- constant desire to drink;
- lack of normal sleep;
- painful sensations in the head.
As the abscess develops, it often ruptures, which can result in bleeding from the anus. Pus is often excreted along with feces, and when the abscess breaks through to the skin, a noticeable fistulous tract is observed. In this case, the symptoms subside a little, but the treatment of paraproctitis becomes more complicated.
Chronic
If treatment for an acute disease is not started in time, then chronic paraproctitis cannot be avoided. In a chronic course, the pathology recurs several times even after drug treatment. In this case, the same signs are noted as in the acute course, but they may not be expressed so clearly or may not manifest themselves fully. The patient experiences a constant increase in temperature, which is difficult to control with antipyretics. Without surgery, it will not be possible to eliminate this form of deviation.
Disease prognosis
If, during the acute course of the inflammatory process in question, contacting a doctor was timely, then you can safely count on a complete recovery without possible relapses.
And even if the patient decides to undergo surgical treatment already at the stage of a formed fistula with chronic paraproctitis, then its excision and removal of purulent tracts also leads to a favorable prognosis.
It is impossible to give a favorable prognosis only when diagnosing chronic paraproctitis with fistula in patients who ignore prescribed treatment.
Tsygankova Yana Aleksandrovna, medical observer, therapist of the highest qualification category.
26, total, today
( 170 votes, average: 4.56 out of 5)
Hemorrhoidal bleeding: how to stop bleeding from hemorrhoids
Colon polyps
Related Posts
Prevention of exacerbations
To avoid illness, it is important to organize a balanced diet.
To speed up the healing process and prevent relapses of the disease, it is recommended:
- avoid bowel retention;
- balance nutrition;
- maintain normal weight;
- carefully monitor the hygiene of the anal area;
- treat diseases of the rectal area in a timely manner.
A timely operation completely eliminates the purulent process, which contributes to a person’s rapid recovery. To prevent the development of such a disease, you must consult a doctor if any pathological manifestations appear in the rectal area and do not self-medicate.
Treatment
Treatment of such a disease, like any of the paraproctitis, is carried out only by surgery. After the abscess has matured, the abscess is opened, cleaned, and drainage is installed. At the same time, the affected crypt and glands are excised. If the patient’s condition does not allow both stages of the operation to be performed at once, then the second stage is carried out after a few days. In the case of subcutaneous-submucosal paraproctitis, the course of the operation, the shape of the incisions, and the sequence of removal of the affected tissue are slightly changed.
The next stage of treatment is physiotherapeutic procedures using ultraviolet rays and ultrasound. Bandages with antiseptic and antibacterial ointments are applied to the perineum in the anus area. A gas tube is sometimes inserted into the intestinal lumen after surgery. If the body temperature does not decrease for a long time, the doctor will prescribe a course of antibiotics.
An auxiliary treatment method is the use of traditional medicine recipes. In the postoperative period, sitz baths with a decoction of calendula, chamomile, microenemas, compresses from medicinal decoctions, and tampons with badger fat are prescribed.
In the first weeks after surgery, a diet is recommended that makes bowel movements easier. You need to eat small portions, pureed food, drink more fluids, and eliminate foods that irritate the intestines.
Drug treatment of subcutaneous paraproctitis can be prescribed only at the very beginning of the disease, but is often ineffective. The doctor usually prescribes antibiotics, anti-inflammatories and painkillers. But, in order to avoid the disease becoming chronic, relapses, and serious complications, it is recommended to treat paraproctitis radically - surgically. If relapses recur, immunomodulator drugs are prescribed.
In the future, the patient may be prescribed special physical exercises to increase blood flow in the pelvis and lower extremities.
Classification
There are several different classifications of acute paraproctitis. Let's look at each of them.
The first classification is based on the etiology of this pathology:
- Common acute paraproctitis, resulting from constipation and subsequent infection;
- The acute form of anaerobic paraproctitis is diagnosed in the case of an anaerobic infection;
- A specific form of acute paraproctitis;
- Acute paraproctitis of traumatic nature. Occurs as a result of chemical or mechanical damage to tissue.
The following classification is based on the localization of the resulting fistulas or infiltrates:
- Subcutaneous acute paraproctitis. The purulent infiltrate is localized under the skin in the anal area.
- Ishiorectal acute paraproctitis. Occurs in 38-40% of cases.
- Retrorectal acute paraproctitis is called an abscess and occurs in 1.5, less often 2% of patients who apply.
- Submucosal acute paraproctitis. The inflammatory process is localized directly under the mucous layer of the rectum.
- Pelviorectal acute paraproctitis. The lesion is localized in the fatty tissue located above the pelvic diaphragm.
- Necrotizing paraproctitis.
There is a classification of chronic paraproctitis based on the anatomical features of the fistulas formed as a result of the pathological process:
- Complete fistula. The formed formation has both one and several different passages, merging into one with a common hole on the surface of the skin.
- Incomplete fistula. There is no fistula opening on the surface of the skin. The passage opens onto the intestinal mucosa.
- External fistula. The lesion has access to the surface of the skin.
- Internal fistula. Both exits open into the pelvic cavity or intestinal space.
The following classification is based on the direction of the opening of the fistula:
- Side;
- Front;
- Rear.
Depending on the nature of the location of the fistula opening relative to the anal sphincter, several different types of paraproctitis are distinguished:
- Intrasphincteric, i.e. the fistula is localized to the sphincter on the intestinal side and is diagnosed in 30-35% of cases. It is characterized by the presence of a focus of inflammation without branching fistula tracts.
- Extrasphincteric. The opening of the fistula is located outside the sphincter on the outside.
- Transsphincteric. Doctors find fistula fibers directly in the sphincter area. A characteristic feature is the presence of several purulent tracts, complicating treatment. Gradually, scarring of purulent pockets and the formation of new fistula tracts occurs.
Operation
After surgery, complete recovery occurs in 90% of cases. Most often, the operation is carried out quickly and easily - initially you need to open and clean the inflammation, then remove the connection to the rectum.
In some cases, it is not possible to perform the operation at once. This can happen for various reasons. In such cases, the purulent focus is first cleaned, and after some time it is removed.
The operation does not require any special preparation; moreover, it is most often carried out according to indications and in the serious condition of the patient, in emergency conditions. Surgical intervention requires precision and compliance with all rules; it must be carried out by an experienced proctologist.
The operation requires complete muscle relaxation, so it is performed under anesthesia. The simplest operation for subcutaneous paraproctitis - in this case, an incision is made, pus is released, all connecting bridges are removed, the wound is drained or tamponed. Usually an experienced proctologist carries out both stages at once. If the doctor doubts his abilities, he can postpone the second stage of the intervention for several days or weeks.
Clinic
The clinical picture of the disease is caused by manifestations of suppuration of the soft tissues of the perineum. They are not diverse, but the degree of severity directly depends on the localization of the inflammatory process, the characteristics of the microbes and the state of the immune system.
When patients with acute paraproctitis seek radical help late, fistulas form as a manifestation of the chronic form of the disease.
The presence of a purulent tract, inflammatory and cicatricial changes in the rectum, as well as the soft tissues of the perineum has an unfavorable prognosis.
Acute course
In some cases, the general symptoms of intoxication predominate, displacing local signs of the disease into the background. But most often the opposite happens. Paraproctitis, as a rule, begins acutely. There may be a short prodromal period (up to 3 days), after which more typical manifestations develop.
It happens that inflammation spreads throughout the fatty tissue of the pelvis in the form of phlegmon, but a localized purulent focus does not form, which is why the clinical picture becomes uncertain.
Period of prevalence of general symptoms
Depending on where the purulent process and the primary focus are localized, the period of general manifestations can last 2-10 days. After this, if adequate surgical treatment has not been carried out, the inflammation spreads to other soft tissues of the pelvis.
In the classic course, the following general symptoms of paraproctitis appear:
- Increasing, initially non-localized, pain in the perineal area;
- Increased body temperature;
- Symptoms of intoxication - weakness, malaise,
loss of appetite, insomnia, chills in the evening, and increased sweating at night;
- Tenesmus - the appearance of a painful urge to defecate;
- Constipation;
- Dysuric phenomena (impaired urination).
Symptoms of localized forms
When the inflammatory process takes on a localized form, the clinical picture may have its own characteristics, which also determines the prognosis. The following symptoms of paraproctitis are identified, presented in the table:
| Form | Peculiarities | Symptoms |
| 1. Subcutaneous paraproctitis | The most common form, which is characterized by the rapid appearance and increase in clinical symptoms. The most favorable in prognostic terms. |
|
| 2. Ishiorectal paraproctitis | This form occurs in more than a quarter of patients. The purulent focus is located near the ischium. |
|
| 3. Submucosal paraproctitis | Found in less than 10% of cases. Due to the characteristics of the rectal wall, the lesion usually protrudes into its lumen. |
|
| 4. Pelviorectal paraproctitis | It is also a fairly rare form of the disease, but the most severe. The purulent focus is located in the deep parts of the small pelvis. |
|
| 5. Retrorectal paraproctitis | The rarest form of the disease, the frequency of which, according to the literature, does not exceed 2%. |
|
Ulcer breakthrough
If the patient does not consult a doctor in time, a purulent focus breaks into the rectum, onto the skin of the perineum, or into one of the adjacent cellular spaces. This is accompanied by a short period of pain reduction and stabilization of the patient’s condition, but this is followed by a sharp deterioration, and the symptoms become even more pronounced.
Spontaneous opening of the abscess does not provide proper outflow (drainage), and recovery is slow, increasing the risk of chronicity of the inflammatory process.
Simultaneous damage to several spaces of the pelvis aggravates the inflammatory process, darkening the prognosis for the patient. With purulent melting of the walls of the rectum, widespread infection occurs when it is impossible to prevent feces from getting into the affected soft tissues.
Outcomes
After spontaneous opening of the abscess, the following outcomes of the disease are possible:
- The formation of fistulas is a chronic form of paraproctitis;
- Development of a recurrent form of the disease with frequent periods of exacerbation of the purulent-inflammatory process;
- Recovery.
Complete recovery occurs in less than half of the cases. This is only possible when the gate of infection is destroyed and the abscess cavity is adequately drained until the period of numbness.
In most cases, this occurs with subcutaneous and submucosal forms of paraproctitis, or when receiving surgical treatment.
Chronic course
Almost always, the chronic form of paraproctitis is characterized by a wave-like course. Periods of exacerbation are followed by remission, but the wound surface does not disappear. It is covered with loose granulation deposits, which forms an external opening for the outflow of pus.
The characteristics and amount of inflammatory discharge are determined by the activity of the process, as well as the presence of fistulous branches.
Clinical manifestations
Typically, the general condition of patients with a chronic form of paraproctitis does not suffer, and pain is not typical until periods of exacerbation of the process. With the constant presence of an inflammatory focus, neuropsychiatric symptoms begin to predominate, and the quality of life of patients worsens.
During an exacerbation, the following symptoms appear:
Increased pain, especially during bowel movements, heavy straining or physical activity;
- The patient's body temperature rises;
- Pus is released from the fistula tract in varying quantities (depending on the flora);
- Suppression of the general background, rapid fatigue, deterioration in performance;
- Presence of headaches, insomnia, irritability;
- Inability to retain intestinal gases (due to damage to the sphincter);
- With a large diameter of the fistula tract, gases and feces are released through it.
Complications
In patients with chronic paraproctitis, the following complications develop over the course of several years:
- Asthenization (constant increased fatigue, irritability, headaches) up to neurotic reactions;
- Public self-isolation. Often associated with the presence of an unpleasant odor that accompanies the release of contents from fistulas;
- Skin maceration;
- Chronic proctitis;
- Chronic proctosigmoiditis;
- Amyloidosis of internal organs;
- Pectenosis is a process in which the muscle structures of the submucosal layer are replaced by scar tissue;
- Malignancy of fistulas (leads to cancer).
Treatment of the disease
Purulent paraproctitis of acute and chronic forms can only be treated surgically. If surgery is not performed and the person is treated at home, the infection will spread to surrounding tissues.
The most serious complication is infection entering the bloodstream and general blood poisoning, which can cause death.
Prices for removal depend on the clinic, but on average range from 7,500 to 25,000 rubles.
The disease is treated with antibiotics after surgery to eliminate the risk of re-infection. Self-medication can only do harm, since a person cannot independently determine the type of bacteria that caused the inflammation.
If a person refuses surgery, the disease becomes chronic. Nowadays, surgery is more developed, so removal of ulcers usually does not cause complications.
During surgery, the paraproctitis or abscess is opened, followed by pumping out the contents. After this, the source of infection is determined, and the scar with purulent contents is excised. This will help prevent relapses of this pathology in the future. If you leave the formed fistula, then the development of new abscesses is possible in the future.
Depending on how the surgical wound is healing, antibiotics may be prescribed. If a person has a high temperature for more than 3 days, swelling and inflammation of tissues is observed, then antibiotic therapy cannot be avoided.
On average, the postoperative period takes 3 weeks, but it can be longer. At this time, the patient should be observed by a surgeon and proctologist.
Treatment and prognosis
If it was possible to catch paraproctitis at the initial stage, then conservative (non-surgical) treatment can be used. For this, broad-spectrum antibiotics, potassium permanganate baths, and UHF therapy are used. If there is an already formed abscess or fistulous tract, then therapy involves surgical intervention. In case of acute paraproctitis or exacerbation of chronic paraproctitis, the main task of the operation is to open and empty the abscess, followed by washing its cavity with antiseptics.
But sometimes leaving the abscess cavity, even washed out, can lead to relapse, that is, re-occurrence of inflammation. Therefore, complete excision of damaged tissue is often used, including fistulas that form during the transition from acute to chronic form. Usually the operation is performed under general anesthesia. Surgical treatment is always combined with antibiotic therapy: this avoids the recurrence of a purulent lesion and the spread of infection.
With timely treatment of purulent paraproctitis, the prognosis is favorable: complete recovery occurs.
Chronic paraproctitis
This form of the disease is a consequence of a poorly treated acute process, when the disease becomes protracted.
In the chronic course of the inflammatory process, very often a fistula tract , which opens into the perineum.
Such a fistula, as a rule, is not accompanied by pain, since the purulent contents come out.
If the patient experiences and intensifies pain during defecation, this indicates that an internal fistula has formed and there are problems with the outflow of pus. If the abscess does open on its own, this significantly improves the patient’s condition.
Patients with a fistula usually complain of discharge of pus, blood and/or feces from the external opening onto the skin around the anus.
Causes of pathology
The main reason for the development of acute paraproctitis is the penetration of microorganisms into the pararectal area. There are also other causes of the disease:
The cause of the disease may be diabetes mellitus.
- damage to the integrity of the skin near the anus;
- anal intercourse;
- intestinal diseases;
- decreased immunity;
- development of hemorrhoids;
- diabetes;
- constipation or diarrhea;
- infection from organs located near the rectum;
- infection through the bloodstream.
Causes
As a rule, acute purulent paraproctitis occurs due to human infection with microorganisms of pathogenic origin.
Most often it is E. coli. It penetrates almost unhindered into the fatty tissue either from the rectal area or through ulcers and wounds. The disease can also occur due to infection with clostridia, enterococci, anaerobic bacteria and staphylococci.
It should be noted that microorganisms can penetrate almost any part of the subcutaneous fatty tissue. But as a rule, they affect the layer or pelvic-rectal area.
In rare cases, the cause of acute purulent paraproctitis is inflammation of the prostate gland of a bacterial nature.
If we talk about risk groups, those most susceptible to this disease are men suffering from diabetes mellitus, hemorrhoids or atherosclerotic vascular disease. In addition, predisposing factors include anal sex, cracks resulting from it, as well as weak immunity.