What is calcification
Calcifications in the ovaries in themselves are not a pathology. The radiological sign is detected using ultrasound or MRI in completely healthy ovaries. Pathological calcifications are associated with tumor formations: mature teratoma or dermoid cyst, mucinous cystadenoma (a type of ovarian cyst) or serous neoplasia.
Ovarian calcification detected for the first time is not an indication for a biopsy or other intervention. Pathological evaluation is only required if tumors or cysts are present.
Calcifications detected using gynecological ultrasound are of two types:
- psammous - spherical layer-by-layer formations of protein-lipid substances on which calcium salts are deposited;
- non-psammotic - they are integral accumulations that appear during diagnosis as a zone of increased echogenicity.
It is the identification of psammous deposits that indicates the risk of a serous neoplasm and the need for further examination.
https://youtu.be/4eiF8-dOaIk
Description of the pathology
Calcifications are not considered a full-fledged disease. Most often these are the consequences of childbirth with complications, chronic inflammatory processes in the woman’s reproductive organs. Calcium salts themselves are always present in the human body; they participate in mineral metabolism.
Calcification can be found in the ovaries, appendages, uterus, placenta, mammary gland, etc. Calcifications significantly increase in size and interfere with normal metabolism in tissues.
Reasons for education
Calcium is a conductor of nerve impulses, and therefore plays an important role in the body. In tissues, salts are deposited where cell death occurs as a result of inflammatory processes.
On this topic
- Female reproductive system
Differences between cytology and colposcopy
- Natalya Gennadievna Butsyk
- December 6, 2020
Calcifications in the ovaries are detected as a result of past pathologies:
- adnexitis;
- difficult labor with compression of the ovaries;
- polycystic disease;
- follicular cysts.
Sometimes they occur when the venous outflow from the pelvic organs is disrupted, which occurs during prolonged sitting. Without oxygen, cells begin to die. The influence of hormonal changes on the deposition of calcium salts has been proven.
Every month, a woman’s ovaries produce a corpus luteum, a source of sex hormone production after ovulation. It consists of luteal cells interspersed with fat and reaches up to 1.5 cm in diameter.
7-8 days after ovulation, the corpus luteum involutes, loses the amount of fat in the membrane, and its body becomes white. It is at this moment that, using ultrasound, you can see a focus of connective tissue with calcifications - the result of natural cell death. The corpus luteum is completely reabsorbed within a few months.
On this topic
- Female reproductive system
Echosigns of adenomyosis
- Olga Vladimirovna Khazova
- December 4, 2020
Calcifications can be signs of pathology, but their detection does not indicate ovarian cancer. Salt deposition occurs in only 8% of tumors, predominantly serous cancer. The formations have the shape of concentric circles.
Calcifications detected against the background of malignant tumors are divided into two types:
- metastatic, which are associated with hypercalcemia;
- dystrophic - formed against the background of destruction of epithelial cells and the formation of areas of necrosis.
This process is called ectopic calcification - outside the bone tissue. The deposit is caused by a disturbance in the metabolism of calcium and phosphorus.
Ovarian cancer cells produce specific substances that lead to destruction and changes in surrounding tissue. Calcification is also one of the criteria for tumor destruction during ultrasound examination.
Methods: how to do an ultrasound of the ovaries
For preventive purposes, every healthy woman should undergo an ultrasound procedure twice a year. This is necessary to monitor the condition of the patient’s reproductive system, identify possible pathologies and timely take adequate measures.
- various menstrual irregularities or absence of menstruation;
- starting to take hormonal contraception or inserting an intrauterine device;
- pregnancy planning;
- infertility;
- suspicion of gynecological diseases;
- vaginal discharge containing blood in the middle of the cycle;
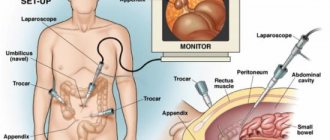
- before and after the “lapara”;
- evaluation of treatment results;
- pulling, cutting pain in the lower abdomen, in the right or left side.
- Most often, sonologists use the transabdominal method of performing ultrasound of the uterus and ovaries. The study of organs occurs using an ultrasound sensor. A special gel is applied to the skin of the lower abdomen to help the device glide over the body. During the examination, the patient does not feel pain or discomfort.
- The transvaginal research method is more informative, as it allows you to get as close to the organ as possible and get a clear picture. A special sensor is inserted directly into the vagina, thanks to which the ovary is perfectly visualized on the computer monitor screen.
- Hysterography makes it possible to obtain a high-quality image of the pelvic organs. A contrast agent is injected into the patient’s vagina, with the help of which a specialist can recognize malignant formations, their size and area of distribution.
- Dopplerography allows you to assess the intensity and direction of blood flow in the vessels and organs of the genitourinary system. It is carried out in case of suspicion of the presence of neoplasms.
- Recently, three-dimensional ultrasound has become widely used. This technology opens up new possibilities in diagnostics. A three-dimensional image (photo) can reveal not only anomalies in the structure of an organ, but also defects in its membranes. The price of such a procedure will be higher than the cost of a conventional study, but the results will be the most reliable.
There are several methods for performing ultrasound examination of the ovaries. The choice of one or another technique directly depends on the purpose of the study and the patient’s medical history.
Transabdominal ultrasound method
During the examination, the doctor moves the sensor with slow, smooth movements, changing the angle of inclination if necessary. This technique allows you to better study the structure, determine the size and structure of the organ, and show it from different sides. For a more detailed study of the ovaries, hysterography and Dopplerography are additionally performed.
All data obtained during the procedure are compared with normal values and recorded in the study protocol. Based on the results of the ultrasound, the gynecologist identifies existing abnormalities, signs of disease, or diagnoses pathology.
Diagnostics
Calcifications are usually detected using x-rays or ultrasound. The sensor detects pinpoint hyperechoic foci ranging in size from 1-3 mm.
If non-psammotic formations without signs of tumors are detected, the diagnostician does not recommend further examination. If psammous calcifications are detected, a repeat ultrasound examination may be prescribed.
Lesions are detected by CT in 34.1% and by histological examination in 56% of ovarian cysts. Sometimes they are detected in the epithelial cells of malignant tumors - serous carcinomas.
In this case, the doctor refers the patient to a biopsy to study a tissue sample. In the absence of cancer cells, calcifications are considered benign.
Treatment
Calcifications are a sign of other pathologies. In normal ovaries they indicate a local metabolic disorder.
In tissues, the pH - acid-base balance - increases, which leads to the accumulation of calcium salts inside the cells. This pathology does not require drug or surgical intervention.
If calcifications are associated with ovarian cysts, then most often they indicate a certain type of formation. Serous and mucinous cystodenomas are subject to surgical removal.
If a malignant process is suspected, a more detailed diagnosis is carried out to identify the stage of the tumor and the presence of metastases.
Calcium salts in the ovaries without concomitant pathologies cannot be treated. There is an opinion that it is necessary to create a calcium deficiency in the body in order to resolve deposits. But this approach may increase the risk of osteoporosis.
Surgical intervention
Although uterine fibroids themselves cannot grow in a calcium capsule, the tissue around it can grow. That is, theoretically, the growth of a neoplasm is possible. In this case, if it is large, surgery is required.
Also, when a large nodule calcifies, it begins to put more pressure on neighboring organs. Possible frequent urination and intestinal dysfunction. More severe pain in the lower abdomen and lower back may also occur. In this case, surgery is also indicated.
However, the tumor is treated quite successfully conservatively. You can learn about this from the article “Treatment of uterine fibroids.” The features of surgical removal are described in the material “Surgery to remove uterine fibroids.”
By clicking the “Submit” button, you accept the terms of the privacy policy and consent to the processing of personal data under the conditions and for the purposes specified in it.
In medical practice, calcifications are defined as deposits of calcium salts. Moreover, this can happen in the cavities of various organs. Calcifications are often found in the uterus.
The uterus is an unpaired hollow organ that consists of three layers. The inner layer is the endometrial, represented by powerful muscles. The widest middle layer is the myometrium. The outer part of the uterine structure is the peritoneum.
Complications
Malignant tumors cannot be called a complication of pathology; rather, the deposition of calcium salts is a sign of a past or existing pathological process. They do not affect ovulation, ovarian function or the possibility of conception.
The study showed that calcifications up to 5 mm are normal. Scientists observed women with calcium salts in their ovaries for 30 months.
None of them developed malignant tumors. Histological examination (biopsy) confirmed that calcium appeared as a result of degeneration of the white corpus luteum.
Spleen: structural features and functions
The spleen is an organ of the hematopoietic and immune system, bean-shaped and located in the abdominal cavity in the left hypochondrium. The normal dimensions of the organ in an adult are:
- length 6–8 cm;
- width 9–12 cm;
- thickness up to 4 cm.
On the outside, the spleen is covered with a connective tissue capsule, which, in the form of partitions, penetrates into the parenchyma and divides it into lobules (compartments).
The internal part is represented by red and white pulp. Pulp is a type of connective tissue containing large quantities of reticular fibers. Thanks to the fibrous structure, a kind of network is formed that holds the formed elements of blood. Areas rich in white blood cells (leukocytes and lymphocytes) are the white pulp. Areas rich in red blood cells, macrophages, plasma cells and dendritic cells are the red pulp.
The main functions of the spleen:
- Formation and maintenance of immunity. The organ synthesizes specific antibodies that activate the immune system and protect the body from infections of a viral and bacterial nature. In addition, the spleen is the main source of lymphocytes - cells of the immune system that provide protection to the body.
- Blood filtration. The parenchyma of the organ contains a large number of macrophages and reticulocytes that are capable of capturing bacteria, damaged red blood cells and other cells circulating in the blood. It filters the blood from toxins and insoluble components that appear in the plasma during pathological conditions such as injuries and burns.
- Participation in the life cycle of erythrocytes and iron transport. Pulp cells capture damaged and old red blood cells, recycling them. In this case, iron, which is part of hemoglobin, is included in other proteins. Transferrin synthesized in the spleen enters the bone marrow, bringing iron necessary for the formation of red blood cells.
- Blood cell depot. The organ is able to accumulate red blood cells, platelets and leukocytes. If necessary - injury, shock, physical activity, it contracts, releasing formed elements into the blood.
The spleen is not considered a vital organ. When removed, its functions are taken over by other organs of the body’s immune and hematopoietic systems. It has been noted that in people with a removed spleen, resistance to bacterial infections decreases, and changes in the blood count also occur.