5695
1
Adhesions in the pelvis are a common female gynecological disease. Why is infertility so common in women today? The answer is simple: because patients do not consult a gynecologist on time, do not undergo examinations every 6 months, do not have an ultrasound of the pelvic organs, and generally know little about their health in general. What are the symptoms of adhesions in the pelvis? How does a woman understand that she needs to seek medical help?
Adhesive disease often manifests itself with atypical symptoms in the form of pathological miscarriage, pelvic pain, and digestive disorders. In the absence of surgical intervention, patients develop acute intestinal obstruction. Most often, such a diagnosis is made to women with a history of inflammatory process of the pelvic organs or as a consequence of surgery. In the latter, adhesions are formed in 96% of cases.
What causes adhesions in the pelvis in women?
Adhesions often form against the background of such changes:
- Gynecological diseases: colpitis, adnexitis, parametritis, endometritis;
- Consequences of surgical interventions after cesarean section, removal or excision of appendages, amputation of the uterus above the vagina;
- After ovarian apoplexy or pathological rupture of the tube;
- Mechanical injuries of the pelvic organs;
- Promiscuous intimate relationships with partners;
- Lack of regular examinations and checks of women's health.
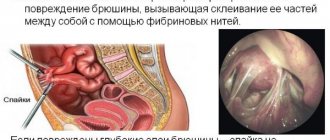
With all the processes described above, the structure of the connective tissue is disrupted, and fibrin production is activated. As a result, partial or complete gluing of the internal genital organs with fibrin fibers occurs. Such a reaction is considered protective and is aimed at neutralizing the source of inflammation or protecting damaged areas of the ovaries, fallopian tubes, etc.
With extensive damage to the pelvic organs of a woman, the adhesions grow and thicken so much that this limits the physiological mobility of the uterus. The displacement of organs relative to their normal position provokes irritation of the nerve endings, followed by severe pain.
Why do adhesions form?
A variety of mechanical and inflammatory factors provoke adhesions in the pelvis. Let's consider the main reasons for the development of this pathology:
- Surgical intervention. Postoperative adhesions appear due to prolonged contact of internal tissues with air and instruments, and drying out of the peritoneum. Therefore, the number of cords formed depends on the volume of the operation, the type of access chosen, the introduction of drains to remove inflammatory fluid and blood, the installation of meshes to strengthen the peritoneal tissue, etc. With repeated surgical interventions, pelvic adhesions appear with a probability of 95%.
- Diseases accompanied by inflammation of the pelvic peritoneum (pelvioperitonitis), uterus and appendages (parametritis, endometritis, salpingoophoritis). The impetus for their development is sexually transmitted infections (chlamydia, ureaplasmosis, gonorrhea, etc.), surgical procedures (abortion, hysteroscopy, etc.), installation of an intrauterine device, absence or improper treatment of pelvic diseases.
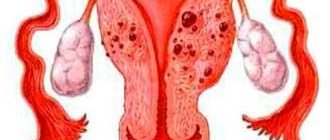
- Endometriosis is hyperplasia of the inner layer of the uterus that extends beyond its boundaries. During menstruation, the endometrium secretes blood into the pelvic cavity, which provokes a protective reaction of the peritoneum, triggering the formation of cords.
- Difficult pregnancy and childbirth. During these periods, adhesive disease of the pelvis can occur after complications (cesarean section, infection of the uterus during childbirth, etc.).
- Hemorrhage inside the peritoneum and pelvic cavity, which occurs with ovarian apoplexy, mechanical damage, ectopic pregnancy, retrograde reflux of menstrual blood through the fallopian tubes.
- Inflammatory processes in the abdominal organs that are indirect in nature (appendicitis).
The above reasons do not always lead to the formation of adhesions in women. The risk of their occurrence is reduced to zero if inflammatory processes are treated on time, adequately and all doctor’s recommendations are followed.
https://youtu.be/nnWcrAyqOtM
Classification of adhesive disease
Depending on the symptoms of adhesions in the pelvic organs, pathologies are distinguished as:
- An acute process in which a woman’s body temperature rises against the background of an inflammatory process, her blood pressure decreases, her health worsens, she feels nauseous and vomits. These manifestations indicate increasing intoxication in the body, followed by intestinal obstruction. The patient's life and health are at risk.
- Intermittent stage, characterized by acute attacks and remissions. The patient may complain of unbearable pain in the abdominal area or may not experience any discomfort at all. That is why the disease is considered dangerous.
- The chronic stage, in which inflammation is practically asymptomatic. Sometimes the patient complains of indigestion, constipation, nausea, and pain in the lower abdomen. A woman, as a rule, does not see a doctor for a long time. And she does this only when attempts to get pregnant are unsuccessful.
Based on the type of adhesions, several stages are distinguished:
- At the first stage, the tissues of the ovary and fallopian tubes become infected, but no physiological disturbances in the functioning of the genital organs are observed. A woman can become pregnant and carry a child to term.
- In the second stage, adhesions affect the outer lining of the ovary and fallopian tubes. As a result, the fertilization process is disrupted: the egg cannot pass through the fibrin fibers.
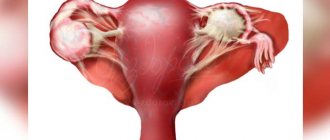
- At the third stage, most of the ovary is affected by adhesions. In this case, the fallopian tubes are deformed, and their lumen is closed by multiple adhesions.
PELVIC ADHESIONS SYMPTOMS AND TREATMENT
Adhesive disease (morbus adhaesivus) is a condition characterized by the formation of adhesions in the abdominal cavity and pelvic organs - connective tissue cords.
Recently, the prevalence of adhesive disease in gynecology has increased greatly. This is due to many provoking factors in the modern world.
Causes and mechanism of adhesions in the pelvis
The most common reasons contributing to the occurrence of adhesions in the pelvis are the following:
1) inflammatory diseases of the pelvic organs. These include infections of the uterus, appendages and pelvic peritoneum: endometritis (inflammation of the uterine cavity), metroendometritis (inflammation of the mucous and muscular lining of the uterus), parametritis (spread of infection to the space outside the uterus), salpingo-oophoritis (inflammation of the uterine appendages), pelvioperitonitis (inflammation of the pelvic peritoneum).
Predisposing factors for the development of the listed infectious diseases are: long-term wearing of an intrauterine device; curettage of the uterine cavity, in particular abortions; sexually transmitted infections (chlamydia, ureaplasmosis, trichomoniasis, mycoplasmosis, gonorrhea).
The mechanism of occurrence of adhesive disease is as follows: when an inflammatory process occurs in the pelvis, the inflamed tissues become swollen, and a fibrin coating appears on the peritoneum. Fibrin seems to glue adjacent tissues together. As a result, there is an obstacle to the further spread of the inflammatory process. After suffering an inflammatory disease, the glued surfaces of the tissues form adhesions with each other. Adhesions are adhesions, they perform a protective function - they limit the inflammatory process.
When an infection enters the fallopian tubes, inflammatory exudate does not always form. Abortion of acute inflammation of the mucous membrane of the tubes may occur before it enters the exudation stage. In many patients, the exudate formed in the acute stage of the disease resolves. Only in a small proportion of patients, an acute inflammatory process in the fallopian tubes leads to the spread of inflammatory serous or purulent exudate throughout the tube. Exudate flowing through the abdominal opening of the tube into the abdominal cavity can cause a response - loss of fibrin, sealing the abdominal opening, which is hermetically obliterated over time. The fallopian tube turns into a closed cavity. With the development of a purulent process, a pyosalpinx forms in it. If the uterine opening of the tube remains open, exudate may leak into the uterine cavity and then through the vagina to the outside. From the fallopian tubes with exudate and hematogenously, bacteria can penetrate the ovary and cause its purulent melting (pyovar).
Both the fallopian tube and the ovary increase in size as the inflammatory exudate accumulates, while the tube acquires a retort-shaped shape, and the ovary acquires a spherical shape. In the mucous membrane of the tube, areas of desquamation of the epithelium and gluing of opposite surfaces with the formation of partitions are observed. As a result, a multi-chamber saccular formation is formed, filled in some cases with serous exudate - hydrosalpinx, in others - with purulent exudate - pyosalpinx. When gluing and then fusion of the pyosalpinx and pyovar at the fusion sites, melting of the capsules may occur.
The tunica albuginea and the walls of the fallopian tube, as hyaluronic acid is deposited in them and fibrous tissue grows, turn into dense, impenetrable capsules. These inflammatory formations (hydrosalpinx, pyosalpinx, pyovar, purulent tubo-ovarian tumors) are usually fused with the walls of the pelvis, with the uterus, fallopian tube, ovary of the opposite side, with the omentum, bladder and intestines. The formation of capsules impenetrable to microbes and extensive adhesions in the acute stage plays a protective role, preventing the spread of infection. Subsequently, after the death of the causative agents of the inflammatory process, these impenetrable capsules delay the resorption of the accumulated serous or purulent exudate.
See also: I'm embarrassed by my body. Season 4. Issue 14 from 05/04/17 Watch online
The location of the pelvic organs with inflammatory saccular formations changes significantly, and the function of neighboring organs (rectum, bladder) and, of course, reproductive function are often disrupted.
2) inflammatory diseases of the abdominal organs, for example, appendicitis;
3) mechanical damage to the pelvic and abdominal organs (trauma, surgical interventions). Adhesions develop when there is hemorrhage in the abdominal cavity, especially when the escaping blood becomes infected. In gynecology, the formation of adhesions is often caused by bleeding during ectopic pregnancy and ovarian apoplexy. The importance of peritoneal trauma, cooling or overheating in the development of adhesive disease has been experimentally proven.
The presence of foreign bodies (wipes, drains) in the abdominal cavity during surgery is also accompanied by the formation of adhesions. ;
4) hemorrhages in the abdominal cavity (ectopic pregnancy, ovarian apoplexy, etc.);
5) endometriosis is a disease characterized by the growth of endometrioid tissue outside the endometrium - the inner layer of the uterus.
The inflammatory process in the abdominal cavity and pelvis does not always lead to the formation of adhesions. If treatment is started on time and carried out correctly, the likelihood of formation of adhesions is reduced. Adhesions form when an acute process becomes chronic and the healing process extends over time.
The most common cause of adhesive disease is inflammation of the appendix and appendectomy (about 43%), in second place are diseases and operations on the pelvic organs and operations for intestinal obstruction (about 30%).
Symptoms of the presence of adhesions in the pelvis
The severity of symptoms in adhesive disease depends entirely on the degree of spread of adhesions in the pelvic space. Options range from asymptomatic to pronounced clinical picture. There are three main clinical forms of the disease:
1) spicy. Patients with this form of the disease have quite pronounced complaints - the pain syndrome gradually increases, vomiting, nausea bothers them, the temperature rises, and the heart rate increases. Examination of the abdomen (pressure) causes sharp pain. Intestinal obstruction occurs. After which the patient’s condition sharply worsens: the pressure drops sharply, the amount of urine excreted decreases, weakness and drowsiness occur. Water-salt and protein metabolism in the body is disrupted. The condition of patients with an acute form of adhesive disease is assessed as extremely serious;
2) intermittent form: pain occurs periodically, intestinal disorders - constipation, diarrhea - may be disturbing.
3) chronic form - characterized by a hidden clinical picture: the clinic is absent, or aching pain in the lower abdomen and constipation occur from time to time. It is the chronic form of adhesive disease that is most often encountered in gynecological practice. Quite often it is a manifestation of endometriosis and hidden infections, which neither the patient nor the gynecologist is aware of. The adhesive process causes obstruction of the fallopian tubes, which leads to infertility. It is with this complaint - the inability to get pregnant within a year - that patients turn to a gynecologist in the asymptomatic course of a chronic form of adhesive disease.
If a painful attack occurs and signs of intoxication (vomiting, nausea and fever), the patient should immediately consult a gynecologist. If the complaints are severe, you need to call an ambulance. Based on the symptoms, adhesive disease can be confused with many diseases, ranging from acute surgical pathology (appendicitis, intestinal obstruction, ectopic pregnancy), and ending with banal poisoning.
Self-medication in this case is unacceptable - only competent consultation with a specialist will help protect yourself from unpleasant consequences.
Diagnosis of adhesive disease
Diagnosis of adhesions in the pelvis is not so simple; a gynecologist can suspect its presence at the first examination if there are characteristic complaints and anamnesis (surgical interventions in the past). During a vaginal examination, the pelvic organs are motionless or slightly mobile during examination. With a pronounced adhesive process, examination on a chair causes pain. However, a reliable diagnosis can only be made after a series of tests and studies:
See also: HERPES KERATITIS EYE TREATMENT
— Vaginal flora smear;
- PCR - diagnostics - examination for urogenital infections;
— Ultrasound of the pelvic organs;
- MRI - magnetic resonance imaging of the pelvic organs - is carried out after a preliminary ultrasound of the pelvic organs. Non-invasive instrumental research method with high information content;
— Diagnostic laparoscopy is an operative, but the most reliable diagnostic method. Two small incisions are made on the abdominal wall. Air is pumped into the abdominal cavity. A laparoscope (a thin tube with a video camera unit at the end, through which the image is transmitted to the monitor screen) is inserted into one incision. A manipulator is inserted into another incision; with its help, the doctor examines the organs, displaces them, and examines them in detail. This allows you to make an accurate diagnosis with complete confidence.
Depending on the laparoscopic picture, there are 3 stages of the spread of adhesive disease: 1st stage - adhesions are located only near the fallopian tube, ovary or other area, but do not prevent the capture of the egg; Stage 2 - adhesions are located between the fallopian tube and the ovary or between these organs and prevent the capture of the egg; Stage 3 - torsion of the fallopian tube, blockage of the fallopian tube by adhesions, which makes it absolutely impossible to capture the egg.
Obstruction of the fallopian tubes according to hysterosalpingography (a contrast agent is injected into the uterus, X-ray images are taken), gynecological examination and ultrasound examination with a high degree of certainty indicate the presence of adhesions, but the patency of the fallopian tubes does not exclude the presence of adhesions that seriously impede pregnancy. Conventional ultrasound does not reliably detect the presence of pelvic adhesions .
Thus, it is the determination of the stage of spread of the adhesive process that is fundamental for determining treatment tactics. In many cases, patients can be observed and examined by a gynecologist for years with an unclear diagnosis, but laparoscopy allows not only an accurate diagnosis, but also effective treatment of adhesive disease.
Treatment of adhesive disease
Treatment of adhesive disease depends entirely on the severity of the disease; it can be either conservative or surgical. Let me say right away that in acute and intermittent forms of the disease, surgical treatment - laparoscopy - is the only treatment method due to its high efficiency and rapid effect. Very often, surgical treatment is combined with conservative treatment for greater effect.
In the chronic form of adhesive disease, only conservative treatment can be used. It is necessary to identify the cause of the development of adhesive disease. If any urogenital infection is detected (say, chlamydia), then first of all, treatment should be aimed at eliminating the underlying disease in order to prevent further spread of the adhesive process. For this purpose, the drugs of choice are antibiotics and anti-inflammatory drugs (NSAIDs, corticosteroids). If the cause of adhesive disease is endometriosis, then hormonal treatment, anti-inflammatory drugs, desensitizing and symptomatic therapy are prescribed.
Nonspecific therapy is widely popular - enzyme therapy - fibrinolytic drugs that dissolve fibrin (longidase, trypsin, chymotrypsin), these are quite effective drugs that resolve small adhesions. In the absence of an acute infectious process, physiotherapy is used - internal laser therapy and external magnetic laser therapy.
This treatment is not a panacea for the chronic form of adhesive disease. Conservative treatment is most effective in stage 1 of the disease.
See also: TREATMENT WITH LEVOMEKOL IN GYNECOLOGY
If all of the above methods are ineffective and if adhesions continue to spread, therapeutic and diagnostic laparoscopy is indicated. As a rule, a gynecological surgeon diagnoses adhesive disease already on the operating table and at the same time performs an operation - dissects and removes adhesions. There are 3 options for laparoscopy: - adhesions are cut using a laser - laser therapy; - adhesions are cut using water under pressure - aquadissection; - adhesions are cut using an electric knife - electrosurgery.
The choice in favor of one or another treatment method is determined by the doctor during laparoscopy, depending on the location of the adhesions and the extent of the process. During the operation, the surgeon also carries out conservative treatment in order to prevent adhesions: barrier fluids are introduced - dextran, povilin, etc.), polymer absorbable films are applied to the fallopian tubes and ovaries.
Factors influencing the treatment of adhesive disease
Once a diagnosis of “Adhesive Disease” has been established, it is necessary to adhere to certain canons and rules in order to avoid repeated relapses of the disease:
- visiting a gynecologist once every six months; - rational diet - eat small portions with short breaks between meals - about 5 times a day; avoid foods that cause increased gas formation; - physiotherapeutic procedures are very useful for a speedy recovery, so it is recommended to regularly visit a physiotherapist - you can carry out electrophoresis with medications, therapeutic massage and physical exercise); - if a painful attack occurs, you can use antispasmodics (no-spa, papaverine). If the attacks do not go away, you should consult a gynecologist and not self-medicate.
After treatment - after surgery or conservative treatment - patients are given physical rest for 3-6 months, dynamic observation by a gynecologist. In the first 2-3 months, you must adhere to the rational diet described above. Physical therapy and physiotherapeutic procedures also contribute to rapid recovery. If all rehabilitation measures are completed, the prognosis is favorable.
Folk remedies for adhesions in the pelvis
Traditional medicine is also used for adhesive disease as a symptomatic treatment. However, it should be borne in mind that all folk remedies are effective only if we are talking about single adhesions, otherwise herbal tinctures are not helpful and prolonged “leaning” on herbs can only worsen the condition. It is very useful to use herbal tinctures during the rehabilitation period and as an additional remedy to the main treatment. For this purpose, St. John's wort is used in dried and crushed form. A tablespoon of St. John's wort herb is poured into a glass of boiling water, boiled for 15 minutes, filtered and the decoction taken 1/4 cup 3 times a day.
Complications of adhesive disease
Adhesive disease is a very formidable disease to turn a blind eye to. There are cases when the disease proceeds rather favorably without making itself felt, but under unfavorable circumstances the adhesive process rapidly spreads and in the absence of a competent approach and treatment, very serious complications are possible, such as: infertility, menstrual irregularities, bending (displacement) of the uterus, intestinal obstruction, obstruction of the fallopian tubes, ectopic pregnancy, not to mention the acute form of the disease, which can lead to very life-threatening consequences.
Prevention of adhesive disease
Prevention of adhesive disease includes: regular observation by a gynecologist, gynecological massage, timely treatment of urogenital infections, natural family planning: protection against unwanted pregnancy, refusal of abortion, vaginal birth, regular sex life.
Symptoms of adhesive disease
If adhesive disease in women proceeds without complications, then the woman does not feel anything other than pain in the ovarian area above the pubic area. In the complicated stage of the disease, the patient complains of constant aching pain not only in the pelvic organs, but also in the lumbar area and even in the rectum.
How do the genitals hurt, how exactly is it expressed? The pain becomes stronger with every movement of the woman, while lifting minor weights.
The provoking factor for pain can be stress, hormonal changes in the body (menopause, menstruation). Pain below the abdomen worries during defecation, during sexual intercourse, when urinating is delayed, or immediately after the process.
If adhesions in the pelvis grow to nearby internal organs, then the woman suffers additional attacks of pain. When the digestive organs are compressed, the patient complains of vomiting, flatulence, diarrhea or frequent constipation, and loss of appetite.
When the adhesive process moves to the ovaries, fallopian tubes, and uterus, reproductive function is disrupted. The adhesive process is a dangerous disease. She is considered “invisible”; the woman does not understand and has no idea that irreversible changes are taking place in her body. And only at the stage of pregnancy planning the patient is faced with a diagnosis of primary infertility.
Diagnostics
The examination includes laboratory, hardware, and instrumental methods. But they are preceded by a bimanual examination on a gynecological chair. The procedure causes significant pain to the woman, especially during palpation of the uterus. The reproductive organ is limited in mobility.
Basic diagnostics:
- Urine and blood analysis (for biochemical, bacteriological, clinical testing, PCR).
- Ultrasound of the pelvis. Allows you to preliminarily establish that the cause of deterioration in health is the adhesive process.
- Laparoscopy. It involves performing 2-3 punctures near the pelvis and then introducing a special thin instrument. It is tube-shaped and equipped with a camera. Through this, the condition of the pelvis and the presence of adhesions in its cavity are clearly visible.
- Hysterosalpingography. Thanks to this method, it is possible to determine how much the fallopian tubes are involved in the pathological process.
- MRI of the pelvis. Refers to a complex radiation imaging method. A three-dimensional image allows you to detect the presence of synechiae of varying degrees of severity.
To identify adhesions in the pelvis, it is necessary to exclude the development of tumors, acute or chronic inflammation. If the gynecologist considers this appropriate, an additional visit to a urologist or surgeon will be required.
Symptoms at the initial stage of the disease
At the initial stage of adhesive disease of the pelvic organs, tissue scarring occurs. That is, the patient does not feel any characteristic pain signs. When fibrin fibers begin to grow and grow into nearby organs, pain occurs and tends to intensify. A woman needs to pay attention to the following symptoms of adhesions in the pelvis at the initial stage:
- Sharp acute pain in the lower abdomen;
- Recurrent dull pain in the abdomen, which intensifies over time due to the growth of adhesions;
- Increased pain during menstruation;
- Pain that is difficult to relieve with painkillers and antispasmodics in the form of No-Shpa.
Additional manifestations of adhesive disease of the female genital organs are:
- Primary infertility is a condition in which the patient cannot become pregnant within a year;
- Indigestion;
- Intestinal obstruction;
- Acute pain during menstruation (until recently, menstrual periods passed painlessly);
- Pain during intimate relationships;
- Unpleasant sensations in the lumbar region, abdomen;
- Spasms in the lower abdomen and pubic area;
- Bloody discharge (depending on the stage of adhesive disease, the discharge may be spotty or copious).
In some patients, with adhesions of the genital organs, the menstrual cycle is disrupted due to impaired functioning of the ovaries. You should consult a gynecologist whenever your period is delayed by several days. If menstruation does not occur after several weeks or even months, then it is necessary to conduct a comprehensive examination: ultrasound, blood test for hormones, etc.
With inflammatory processes in the ovaries, a woman may experience greenish vaginal discharge.
Signs and symptoms
Symptoms of this disease include nagging pain in the lower abdomen, frequent constipation, bowel dysfunction, constant fatigue, and depression. Failure to see a doctor in a timely manner can lead to adhesions entangling a woman’s reproductive organs like a spider’s web, and practically reducing a woman’s chances of becoming a mother to zero.
When the disease becomes acute, a woman begins to suffer from ever-increasing pain in the lower abdomen, attacks of nausea and vomiting, rapid heartbeat, fever and other unpleasant symptoms. In this case, the patient needs emergency medical care.
Symptoms of adhesions in gynecological diseases
Adhesions in the pelvis begin with gynecological diseases. During inflammatory processes, a woman complains of:
- Vaginal discharge with an unpleasant odor;
- Burning during urination;
- Itching of the genitals;
- Hyperemia, swelling of the external genitalia;
- Weakness, fatigue.
With inflammation of the uterine appendages - salpingo-oophoritis, the patient is worried about: pain in the lower abdomen, increased body temperature, bloody discharge from the vagina that is not associated with menstruation. Following the inflammatory process of the uterus, the destruction of connective tissue and stimulation of fibrin production begins. The genital organ is covered with multiple adhesions, which perform a protective function - stopping the further spread of the inflammatory process. At the same time, pain in the abdomen, in the ovarian area and above the pubis intensifies.
The fallopian tubes and ovaries, as purulent or non-purulent exudate accumulates in them (under the influence of the inflammatory process), pathologically increase in size. The epithelium of the genital organs sticks together, which leads to the formation of septa. The woman feels severe pain during adhesions, which intensify as the connective tissue grows. Patients experience impaired reproductive function.
Adhesive disease also occurs as a result of mechanical damage to the abdominal organs, uterus and ovaries. Damage refers to both injuries (impacts) and the result of surgical intervention in the mucous membranes of organs. In gynecology, the most common is considered to be an adhesive process formed during an ectopic pregnancy or a pathological rupture of the ovary.
Why do adhesions appear?
The peritoneum, located in the abdomen, fixes the organs in the correct position. Its visceral layer secretes a small amount of fluid (secretion) that prevents friction. When inflamed, it becomes sticky and viscous. Fibrin is deposited, connecting the affected tissues. Collagen settles into the formed areas of adhesion, forming adhesions that deprive the organs of mobility. This is how the body tries to fence off the pathological focus.
The adhesive process is accompanied by almost all gynecological operations. After extensive interventions it occurs in 60-90% of cases. Women are often to blame for the appearance of adhesions, missing the first symptoms of PID, not rushing to make an appointment with a gynecologist and triggering the disease.
STDs lead to the formation of adhesions. Microorganisms from the vagina penetrate the uterus, tubes and ovaries, causing tubal infertility, which makes it impossible to get pregnant naturally. The penetration of infection is facilitated by abortion, childbirth, and gynecological manipulations, for example, installation of a spiral.
Clinical picture
Let us consider the clinical course of adhesive disease in women. It is worth immediately noting that a clinical diagnosis is made if the formation of adhesions leads to complications in the functioning of internal organs. Such complications include:
- Intestinal obstruction and, as a result, indigestion;
- Pelvic pain that is chronic;
- Infertility, pathological miscarriage.
With intestinal obstruction, the patient experiences a decrease in the intestinal lumen due to the proliferation of fibrin. As a result, feces are not expelled in full, gases are retained in the intestines, the nerve endings of the abdominal wall are stretched, and blood circulation in the arteries is disrupted. The patient complains not only of pain in the lower abdomen, but also of dry mouth, painful bloating, vomiting, and constipation. Treatment consists only of surgery, since drug therapy is ineffective. The patient needs to cut adhesions and cleanse the intestines.
Symptoms of pelvic pain with adhesions
Since the adhesions stretch and displace the genital organs as the fibers grow, the patient reflexively feels these changes on herself:
- My stomach hurts for several hours in a row;
- Pulling in the lower back;
- Acute pain during ovulation;
- Painful menstruation;
- Drawing discomfort during sexual intercourse, as well as after urination and during defecation.
Adhesive disease limits the mobility of the uterus and ovaries, which leads to a constant pulling sensation in the pubic area and perineum. The danger of this condition is that at any moment a disruption of blood circulation can occur, which will lead to internal bleeding.
Unwanted pelvic adhesions
Various infections that seep into the fallopian tube cause blockage of the immune systems. Because of this, the adhesive process does not meet resistance from the body. In a word, the woman is sure that she does not need urgent treatment for adhesions and continues to live as before. Because of this, adhesions in the pelvis progress. Lack of treatment leads to a severe stage of the disease and then it is too late to wonder how to get rid of adhesions in the pelvis without surgery. Another problem is becoming relevant - how do adhesions in the pelvis hurt after surgery? Since postoperative adhesions in the pelvis, unfortunately, are not uncommon. But this is a topic for another discussion.
Treatment of adhesions with medications
Drug treatment of adhesions should be prescribed by a gynecologist after examination. Drug therapy is considered effective for pelvic inflammatory disease. The patient is prescribed antibiotics and anti-inflammatory drugs:
- Prednisolone is a hormonal agent that regulates the process of hormone production (prescribed for primary infertility and menstruation disorders);
- Neotrizol – vaginal tablets with an antibacterial effect;
- Dicloberl is an analgesic and antibacterial agent that promotes the resorption of fibrin fibers;
- Diclofenac is an anti-inflammatory drug;
- Longidaza, Terrylitin - agents that break down adhesions;
- Immunity correctors and vitamins that are necessary to normalize the patient’s well-being.
If drug treatment is ineffective, the woman is referred for surgery. To destroy adhesions and multiple fibrin fibers in the uterus and ovaries, laparoscopy methods are used. Timely surgery helps restore female reproductive function in 50% of cases. After treatment, patients are recommended to undergo a gynecological examination every few months, since the formation of adhesions is repeated.
Symptoms of adhesive disease in women are characterized by sharp, nagging pain in the pubic region, lower abdomen, and lower back. In patients, menstruation is disrupted and primary infertility may develop. The stronger the process of infestation of the genital organs with fibrin fibers, the brighter the symptoms of the disease. Moreover, pain of this kind is not relieved by painkillers and antispasmodics. This is the first thing that should alert a woman if she decides to resort to self-help. Treatment of adhesions is possible, but only after a thorough gynecological examination. In 80% of clinical cases, the functionality of the ovaries and uterus is restored.
Friends! If the article was useful to you, please share it with your friends or leave a comment.
Your comment:
| 05/31/2019 at 20:55 Anton:
Please call me back at Anton's number.
What to do: treatment methods
Treatment of adhesions in the pelvis can be carried out using both traditional medical methods and alternative medicine.
https://youtu.be/fYgJ6YU5X-A
Medication
If we talk about the traditional medical practice of getting rid of adhesive sutures, doctors will recommend you two options: conservative therapy or surgical intervention.
Conservative therapy is to eliminate the cause of the disease as quickly as possible. If it is, for example, an infection, then it can be eliminated with antibiotics and other medications, but if the adhesions are a consequence of endometriosis, it is necessary to undergo a course of hormonal treatment.
The doctor may also recommend enzyme therapy - this is taking fibrinolytic drugs that dissolve fibrin. Another common method is physiotherapy and magnetic laser therapy.
If the disease progresses and new adhesions form, doctors will advise you to resort to surgery, during which the adhesions are cut and removed. Surgical procedures can be performed using a laser, water and an electric knife.
Important! There is a risk that after the operation the adhesive process will resume with renewed vigor. To avoid this, doctors create a kind of barrier in the abdominal cavity between healthy and diseased areas: special preparations are injected into the peritoneal cavity that protect it from the pelvic organs, envelop the sore areas with a special membrane, which dissolves after the damaged area heals.