The uterus is an internal hollow organ located in the center of the woman's pelvis.
The uterus is not just a multi-layered “muscular sac” for bearing a fetus. Contracting alternately, the tiers of its multidirectional circular muscle layers actively participate in childbirth, in the monthly evacuation of menstrual blood and the destroyed part of the mucosa. The compacted areas of the broad ligaments of the uterus (cardiac ligaments) house and support the large uterine vessels, the lower parts of the ureters.
Treatment of diseases of the uterine body
Adenomatous endometrial polyp
08/28/2018 14123 No comments
What is an adenomatous endometrial polyp? Why is it dangerous and why does it grow? Is it necessary to operate on a polyp? Drug treatment after removal of a uterine polyp...
Read more
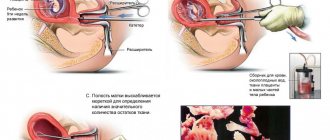
Curettage for endometrial hyperplasia
23/04/2018 28343 36
Is it necessary to perform uterine curettage for endometrial hyperplasia? What tests should I take before the procedure? Progress of the operation. Regime and recovery after uterine curettage...
Read more
Endometriosis and pregnancy
03/19/2018 4634 No comments
Is it possible to get pregnant with endometriosis? When to expect spontaneous pregnancy, and when to resort to IVF? How to treat infertility in older reproductive age...
Read more
Visanne for endometriosis
10/02/2018 25553 7
Visanne for endometriosis - a panacea or..? How to drink - step-by-step instructions. The effect of the drug on the body. Side effects. Reviews…
Read more
Focal adenomyosis
01/27/2018 7432 No comments
Focal adenomyosis - symptoms and signs on ultrasound. Hormones or surgery – what to choose? The best drugs for adenomyosis. What are the dangers of removing the uterus...
Read more
Page 1 of 6 1 …
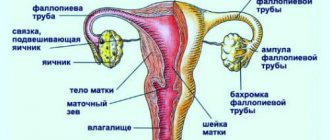
Location and structure of the uterus with appendages
The normal shape of the uterus is pear-shaped. A spherical uterus is a sign of ill health.
Uterine tissue is highly sensitive to the action of sex hormones. Under their influence, the uterine structures can enlarge or atrophy, grow or regress. A non-pregnant uterus is approximately the size of its owner's clenched fist. During pregnancy, under the influence of a specific hormonal background, the uterus increases its volume by about 6 times, its weight by 20 times.
The size of the uterus is variable. They largely depend on the constitution and age of the woman, hormonal characteristics, the phase of the menstrual cycle, the number of pregnancies, and childbirth.
Size of the uterus - average norms
Dimensions of the uterus Anatomical parts of the uterus:
- Body
- Isthmus
- Neck
The walls of the uterus are represented by three layers:
- The endometrium is the inner layer or mucous membrane of the uterus, the site of implantation of the fertilized egg.
- Myometrium - consists of three powerful layers of multidirectional smooth muscle fibers. Some of them extend to the muscle ligaments that hold the uterus in the correct position.
- Perimetry is the outer, strong connective tissue (serous) membrane of the uterus, formed from the peritoneum.
The abdominal space around the uterus, filled with fiber, is called the parametrium.
Return to contents
Anatomy
Parts of the uterus
Parts of the uterus
The uterus consists of the following parts:
- Fundus of the uterus
- This is the upper convex part of the uterus, protruding above the line where the fallopian tubes enter the uterus. - The body of the uterus
is the middle (larger) part of the organ, has a cone shape. - Cervix
- The lower, narrowed, rounded part of the uterus.
The lower part of the cervix protrudes into the vaginal cavity, therefore it is called the vaginal part
, and the upper part of the cervix, lying above the vagina, is called
the supravaginal part
. The vaginal part of the cervix bears the opening of the uterus, leading from the vagina into the canal of the cervix and continuing into its cavity. In nulliparous women, the opening of the uterus has a round or oval shape, and in women who have given birth, it has the shape of a transverse slit. The thick edges of the vaginal part of the cervix, limiting the external opening, are called lips - anterior and posterior. The posterior lip is thinner, the vaginal wall is attached to it higher than to the anterior lip.
Surfaces of the uterus
The uterus has anterior and posterior surfaces. The anterior surface of the uterus, facing the bladder, is called the bladder
, and the back one, facing the rectum, is
intestinal
. The vesical and intestinal surfaces of the uterus are separated from each other by the right and left edges, to which the fallopian tubes approach at the junction of the body with the fundus. The upper corners of the uterine cavity narrow into funnel-shaped depressions into which the uterine openings of the tubes open.
Myometrium of the uterus
Structure of the uterine wall
The wall of the uterus consists of three layers:
- Perimetry
(
Serous membrane
) - is a direct continuation of the serous cover of the bladder. Over a large area of the anterior and posterior surfaces and fundus of the uterus, it is tightly fused with the myometrium; At the border of the isthmus, the peritoneal cover is attached loosely. - Myometrium
(
Muscularis
) - the thickest layer of the uterine wall, consists of three layers of smooth muscle fibers with an admixture of fibrous connective tissue and elastic fibers;
External longitudinal
(
subserosal
) - with longitudinally located fibers and in small quantities with circular ones, as was said, tightly fused with the serous cover.Endometrium of the uterus
- The middle circular
layer is the thickest layer, most strongly developed in the cervical area. It consists of rings located in the area of the tube angles perpendicular to their axis, in the area of the uterine body in a circular and oblique direction. This layer contains a large number of vessels, mainly venous, which is why it is also called the vascular layer. - The internal longitudinal
(
submucosal
) is the thinnest, with longitudinally running fibers.
(
Mucous membrane
) - forms the inner layer of the walls of the uterus. It consists of a layer of columnar epithelium lining the surface of the gland, and a lamina propria of connective tissue associated with the myometrium. It is penetrated by simple tubular glands that open onto the surface of the epithelium, their deepest parts reaching the myometrium. Scattered among the secretory cells are groups of ciliated cylindrical cells. The endometrium consists of two layers - a superficial, thick layer called the functional layer, and a deeper layer called the basal layer.
Cervix
Cervix.
View from the vagina. This is a relatively narrow segment of the uterus, the wall of which consists primarily of dense collagen tissue and only a small amount of smooth muscle and elastic tissue. The cervical canal is flattened, and its mucous membrane consists of a tall columnar epithelium that produces mucus, and the connective tissue lamina propria, which is a fibrous connective tissue containing cells. On the front and back surfaces of the canal there are two longitudinal ridges and smaller palm-shaped folds extending from them at an acute angle. Contacting each other at the confluence of the canal, palm-shaped folds prevent the penetration of contents from the vagina into the uterine cavity. In addition to ridges and folds, the canal contains numerous branching tubular glands. The vaginal portion of the cervix is covered with squamous non-keratinizing epithelium, which usually extends a short distance into the cervical canal, where it becomes the characteristic columnar epithelium. Thus, in mature girls and women, the border between the transition of columnar epithelium into flat non-keratinizing epithelium - the histological border - corresponds to the external os of the cervix. In girls under 21 years of age, the cylindrical epithelium can descend below the border of the external os and extend onto the vaginal part of the cervix, creating a picture of cervical erosion, so such a diagnosis is untenable in young people due to natural anatomical features.
Ligaments of the uterus
Along the edges of the uterus, the sheets of peritoneum, covering its vesical and intestinal surfaces, come together and form the right and left broad ligaments of the uterus. The broad ligament of the uterus consists of two layers of peritoneum - anterior and posterior. The right and left broad ligaments of the uterus are directed to the lateral walls of the small pelvis, where they pass into the parietal layer of the peritoneum. In the free upper edge of the broad ligament of the uterus, between its layers, the fallopian tube is located. Somewhat below the attachment of the ovarian ligament to the uterus, the round ligament of the uterus originates from the anterolateral surface of the uterus. This ligament is a dense fibrous cord of round shape, 3-5 mm thick, containing muscle bundles and located between the leaves of the broad ligament of the uterus. The round ligament of the uterus is directed downward and anteriorly to the deep opening of the inguinal canal, passes through it and, in the form of separate fibrous bundles, is woven into the tissue of the labia majora, without touching the pubic symphysis. At the base of the broad ligaments of the uterus, between the uterus and the walls of the pelvis, lie bundles of fibrous fibers and muscle cells that form the cardinal ligaments of the uterus. With their lower edges, the cardinal ligaments of the uterus connect to the fascia of the urogenital diaphragm and keep the uterus from lateral displacement.
Vessels and nerves of the uterus
The blood supply to the uterus occurs due to the paired uterine artery and branches of the internal iliac artery. Each uterine artery passes along the lateral edge of the uterus between the leaves of the broad ligament of the uterus, giving off branches to its anterior and posterior surfaces. Near the fundus of the uterus, the uterine artery divides into branches leading to the fallopian tube and ovary. Venous blood flows into the right and left uterine venous plexus, from which the uterine vein originates, as well as veins flowing into the ovarian, internal iliac veins and venous plexuses of the rectum.
Lymphatic vessels from the fundus of the uterus are directed to the lumbar lymph nodes, from the body and cervix to the internal iliac lymph nodes, as well as to the sacral and inguinal lymph nodes.
The uterus is innervated from the inferior hypogastric plexus along the pelvic splanchnic nerves.
https://youtu.be/UHWTodAjhyg
Treatment of saddle uterus
Before starting treatment, the doctor will conduct a diagnosis. For this purpose, the following examination methods are used:
- Magnetic resonance imaging. The essence of the method is to take a series of photographs. They are carried out at different levels of internal organs.
- Ultrasound of the uterus and appendages. It should be borne in mind that ultrasound does not always reveal an anomaly. If significant deformation is present, an increase in the bottom width is determined during transverse scanning. The indicator value increases by 6-8 mm. Additionally, there is thickening of the myometrium. The value of the indicator increases to 10 and 14 millimeters. The myometrium protrudes into the uterine cavity. The most optimal option for conducting an ultrasound examination for diagnosing pathology is to conduct an ultrasound using a vaginal sensor. The action is best performed in the second half of the cycle.
- Hysteroscopy. The essence of the method is the introduction of an optical device into the uterine cavity. With its help, it is possible to carry out a visual inspection of the organ cavity. If a developmental pathology is present, the method will allow it to be identified.
- Hysterography and hysterosalpingography. The methods are X-ray examination. To carry them out, a contrast agent is injected into the uterus. The specialist then takes a series of images of the organ. A sign of the presence of a saddle shape is the corresponding depressions.
In most cases, the pathology is not treated. Therapy is prescribed only if there are problems with the ability to get pregnant or the inability to bear a child. In this case, plastic reconstructive surgery is prescribed, which is performed through hysteroscopy. This means that no visible incision is made. The woman will not have to endure prolonged anesthesia. After surgery, the chance of pregnancy and bearing a child increases 10 times.
If pathology is detected in a pregnant woman and she experiences obstetric complications, conservative treatment is carried out. Patients are prescribed hormonal medications, the list of which may include Utrozhestan or Duphaston. Additionally, tocolytics and antispasmodics can be used. The woman must remain in bed. To improve blood flow between the uterus and placenta, drugs that normalize metabolism and blood clotting are used.
Additionally, general strengthening of the body is carried out. This is done to improve immunity. The doctor may prescribe vitamins and minerals, as well as proper nutrition. In some cases, it may be necessary to increase the tone of the uterus and train the pelvic floor muscles. To do this, you need to perform special exercises. The attending physician will tell you about the specifics of the procedure. Exercises help strengthen the pelvic floor muscles, strengthen the muscles of the vagina, improve the regulation of intra-abdominal pressure, as well as blood circulation. Additionally, physical therapy may be prescribed.
Pathologies
Developmental anomalies
- Aplasia (agenesis) of the uterus
- extremely rarely, the uterus may be completely absent. There may be a small infantile uterus, usually with a pronounced anterior incursion. - Duplication of the uterine body
is a defect in the development of the uterus, which is characterized by duplication of the uterus or its body, which occurs due to the incomplete fusion of two Müllerian ducts at the stage of early embryonic development. As a result, a woman with a double uterus may have one or two cervixes and one vagina. With complete nonfusion of these ducts, two uteruses with two cervixes and two vaginas develop. - Intrauterine septum
- incomplete fusion of the embryonic rudiments of the uterus in various variants, can lead to the presence of a septum in the uterus - a “bicornuate” uterus with a clearly visible sagittal depression at the bottom or a “saddle-shaped” uterus without a septum in the cavity, but with a notch at the bottom. With a bicornuate uterus, one of the horns may be very small, rudimentary, and sometimes unlaced. - Hypoplasia is underdevelopment of this organ in a woman. In this case, the uterus is smaller than it should be normally.
The first signs of a saddle uterus
The pathology has no distinctive signs by which a woman could suspect the disease. Usually its detection is associated with pregnancy or attempts to conceive a child. The anomaly can be present in an absolutely healthy woman. Very often she does not even suspect the presence of a saddle uterus. It is impossible to identify this feature of the organ during a classic gynecological examination. Even ultrasound does not always make it possible to establish the presence of such a deviation. An exception to the rule is ultrasound examinations during pregnancy.
Diseases
A symptom of many diseases of the uterus can be uterine leucorrhoea.
- Prolapse and prolapse of the uterus
- Prolapse of the uterus or a change in its position in the pelvic cavity and its displacement down the inguinal canal is called complete or partial uterine prolapse. In rare cases, the uterus slips directly into the vagina. In mild cases of uterine prolapse, the cervix protrudes forward at the bottom of the genital opening. In some cases, the cervix prolapses into the genital slit, and in particularly severe cases, the entire uterus prolapses. Uterine prolapse is described based on how much of the uterus protrudes. Patients often complain of the sensation of a foreign body in the genital fissure. Treatment can be either conservative or surgical, depending on the specific case. - Uterine fibroids
are a benign tumor that develops in the muscular lining of the uterus. Consists mainly of elements of muscle tissue, and partly of connective tissue, also called fibromyoma. - Uterine polyps
- Pathological proliferation of the glandular epithelium, endometrium or endocervix against the background of a chronic inflammatory process. Hormonal disorders play a role in the genesis of polyps, especially uterine ones. - Uterine cancer
- Malignant neoplasms in the uterine area.
Endometrial cancer
- Endometrial cancer refers to cancer of the endometrium (the lining of the uterus) that spreads to the walls of the uterus. - Cervical cancer
is a malignant tumor localized in the area of the cervix.
is a disease in which cells of the endometrium (the inner layer of the uterine wall) grow outside this layer. Since endometrioid tissue has receptors for hormones, the same changes occur in it as in normal endometrium, manifested by monthly bleeding. These small bleedings lead to inflammation in the surrounding tissues and cause the main manifestations of the disease: pain, increased organ volume, infertility. Treatment of endometriosis is carried out with gonadotropin-releasing hormone agonists (Decapeptyl depot, Diferelin, Buserelin-depot)
- Inflammation of the lining of the uterus. This disease affects the functional and basal layers of the uterine mucosa. When it is accompanied by inflammation of the muscular layer of the uterus, they speak of endomyometritis.
- This is a defect in the epithelial lining of the vaginal part of the cervix. There are true and false erosions of the cervix:
- True erosion
refers to acute inflammatory diseases of the female genital organs and is a frequent companion to cervicitis and vaginitis. It usually occurs against the background of general inflammation in the cervix, caused by sexually transmitted infections or conditionally pathogenic vaginal flora, under the influence of mechanical factors, malnutrition of the cervical tissue, menstrual cycle disorders, and hormonal imbalance.
- there is a common misconception that ectopia is the body’s response to the appearance of erosion, since the body is trying to replace a defect in the mucous membrane of the vaginal (outer) part of the cervix with columnar epithelium lining the uterine (inner) part of the cervical canal.
Often this confusion arises due to the outdated point of view of some doctors. In fact, ectopia is an independent disease that has little to do with true erosion. The following types of pseudo-erosions are distinguished: Congenital ectopia
- in which the cylindrical epithelium can be located outside the external os of the cervix in newborns or move there during puberty.
- cervical ruptures during abortion lead to deformation of the cervical canal, resulting in post-traumatic ectopia of the columnar epithelium (ectopion). Often (but not always) accompanied by an inflammatory process.
Symptoms of a saddle uterus
There are no distinctive symptoms indicating the presence of a saddle uterus. It will not be possible to suspect an anomaly on your own before pregnancy. Deformation of 1 organ has virtually no effect on the process of conception and gestation. However, if the problem is severe, it may be accompanied by a dysfunction of the urinary system, a narrow pelvis or an ectopic septum. Sometimes a woman suffering from the pathology may experience pain during sexual intercourse. This is due to the fact that the blood supply to the walls of the organs is insufficient.
Operations
Soviet poster campaigning against criminal abortion
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on September 13, 2012 . |
- Abortion
(not to be confused with the term "spontaneous abortion", meaning "miscarriage") is an operation aimed at terminating a pregnancy. It is usually performed in the first 20 weeks (sometimes up to 9 months under circumstances permitted by law or the criminal nature of abortion) in a hospital setting. - Vacuum aspiration
or the so-called “mini-abortion” is an intervention aimed at terminating pregnancy at an extremely early stage - from twenty to twenty-five days without expected menstruation. It is a minimally invasive operation and can be performed on an outpatient basis. - Caesarean section
(Latin: caesarea “royal” and sectio “incision”) - childbirth using abdominal surgery, in which the newborn is removed not through the natural birth canal, but through an incision in the abdominal wall of the uterus. - Hysterectomy
- (Greek hystera uterus + Greek ectome ectomy, removal; it is possible to write hysterectomy; another common name is hysterectomy) - a gynecological operation in which a woman’s uterus is removed.
Childbirth
Saddle uterus and childbirth. What is the likelihood of vaginal delivery or caesarean section? It has been proven that by the third trimester no changes in the uterus can be detected due to stretching of its muscle fibers and an increase in size. In the absence of contraindications to vaginal delivery, with correct presentation of the fetus and the absence of low placentation, it is recommended to complete the birth naturally. If there is an abnormal position of the fetus, placenta previa or low placentation, then a caesarean section has to be resorted to.
Natural childbirth can be complicated by weak labor forces, premature placental abruption, tight placental attachment, or early postpartum hemorrhage. All these complications are associated with the irregular shape of the uterus and the inability to contract adequately. Only the doctor decides how to conduct childbirth with a saddle uterus in each specific case individually, but it should be understood that a doctor who plans a vaginal birth at any time can end it with a cesarean section if complications arise during childbirth.
Links
| Woman's uterus at Wikimedia Commons |
- BSE.sci-lib.com. — The meaning of the word “Uterus” in the Great Soviet Encyclopedia. Retrieved September 2, 2008. Archived August 24, 2011.
- Reference-anatomia.ru. — Article “Uterus” in the Handbook of Human Anatomy. Retrieved September 2, 2008. Archived August 24, 2011.
- Golkom.ru. — Article “Uterus” in the Concise Medical Encyclopedia. Retrieved September 2, 2008. Archived August 24, 2011.
Notes
| Human reproductive system | |
| Men's | Penis • Glans • Foreskin • Testicles • Scrotum • Vas deferens • Ejaculatory duct • Seminal vesicles • Urethral canal • Corpus cavernosum • Prostate gland • Prostatic uterus • Sperm • Epididymis • Bulbourethral glands |
| Women's | Vulva • Clitoris • Labia minora • Majora • Bartholin glands • Vaginal vestibule • Vagina • Female U-point • Hymen • Uterus (Cervix) • Fallopian tubes • Ovaries • Epididymis |
Causes and prevention of saddle uterus
Until now, the exact reasons leading to the occurrence of pathology have not been established. However, factors have been identified that increase the likelihood of the defect occurring. The formation of organs in the embryo occurs in the third month of pregnancy. The paramesonephric duct merges, which leads to the appearance of organs of the reproductive system. They are divided by a partition into 2 cavities. Subsequently, its resorption should be carried out. However, if any factor has a negative impact on the development process, embryogenesis may fail. This can lead to an anomaly. The following can have a similar effect on the embryo:
- the occurrence of stressful situations or depression of the mother;
- chronic oxygen deficiency;
- vitamin deficiency during pregnancy;
- cardiac abnormalities;
- intoxication during gestation;
- infectious diseases suffered during pregnancy;
- the presence of pathology of the endocrine system;
- Smoking, poor environment, taking illegal drugs, drinking alcohol or working in hazardous industries can provoke the appearance of pathology.
There is no specific prevention of the occurrence of a saddle uterus. All actions to prevent an anomaly are aimed at eliminating the risks that could provoke its occurrence. If a woman does not want her child to encounter pathology, she should give up smoking, drinking alcohol and drugs. Illnesses during pregnancy should be treated promptly. You need to try to protect yourself from stress and eat well, saturating yourself and your child with all the necessary substances.
A woman should adhere to a healthy lifestyle. It is necessary to visit a gynecologist at least once every six months. During pregnancy, the frequency of visits increases to 1 time per 14 days during the first and second trimester and to 1 time per week in the third trimester. It is necessary to register with the antenatal clinic before reaching 12 weeks of pregnancy. Conceiving a child needs to be planned. A woman with a saddle uterus should undergo evaluation and preparation. Chronic and other diseases must be treated.