A saddle-shaped uterus is a congenital pathology that is usually discovered by chance during an examination by a gynecologist. There are no clinical manifestations of this deviation in patients. Often, a woman learns about the abnormal structure of the uterus during a gynecological examination. The first thing that worries patients with this diagnosis is whether it is possible to get pregnant with a saddle uterus? If the anomaly is minor, then the saddle uterus is not a barrier to pregnancy. The probability of conception in each specific case is determined individually, since everything depends on the degree and nature of the complexity of the disease. It is impossible to say for sure whether a woman with such a diagnosis will be able to become a mother. It is necessary to consult an experienced doctor and undergo a thorough examination.
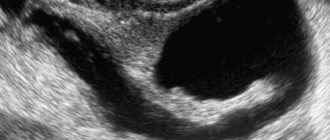
This is what a saddle uterus looks like. A normal uterus does not have an "arch" on top. In Western medicine, there is no diagnosis of a saddle uterus, there is an arched uterus.
Bicornuate and saddle uterus
The causes of the abnormal structure of the female reproductive organ are unknown. There is an opinion that the pathology may be a consequence of the influence of negative factors on a pregnant woman. The uterus of a female fetus begins to form from the 10th week. By week 14 this process is complete.
Under the influence of natural processes, two utero-vaginal cavities are formed. They are separated by a special septum, which usually resolves towards the end of pregnancy. The uterine cavity becomes homogeneous. But in some cases, the saddle-shaped shape of the organ is preserved. This phenomenon is due to the following risk factors:
- Infectious lesions of the body during pregnancy.
- Drinking alcohol, drugs, smoking during pregnancy.
- Genetic abnormalities.
- Professional activities associated with the influence of harmful substances.
- Poor nutrition during pregnancy.
- Poor environmental conditions.
- Endocrine diseases.
- Chronic pathologies.
- Severe fetal hypoxia.
- Metabolic disorders, etc.
According to the majority of doctors, the combination of the influence of external and internal negative factors on the body of a pregnant woman causes abnormalities in the structure of the uterus in the unborn baby. The saddle uterus is one of the types of pathology called bicornuate uterus.
This is what a bicornuate uterus looks like.
With this diagnosis, the organ is divided from the inside by an incomplete septum. Other subtypes of bicornuate uterus:
- With incomplete bicornus, the upper part of the organ is divided, and the size and shape of adjacent cavities are the same.
- A complete bicornuate uterus is characterized by the division of the reproductive organ into two separate cavities.
- The saddle uterus is characterized by a small depression in the fundus, resembling a saddle in shape.
Such anomalies concern only the internal structure of the organ, and they do not cause pathological changes outside the uterus. Its shape and size remain natural. With such a diagnosis, the likelihood of pregnancy decreases significantly, but still, a saddle-shaped uterus is not a death sentence .
Causes of pathology
The genital organs are formed at 10–14 weeks of embryonic development. When the paramesonephric ducts join, two uterine cavities are obtained, between which there is a septum. Gradually, as the fetus grows, it resolves, and at the time of birth, the girl’s uterus is pear-shaped. However, if there is a negative impact on the fetus, a malfunction may occur, due to which the child will be born with abnormalities of the genital organs. Their development is influenced by:
- fetal hypoxia due to the presence of obstetric pathologies or maternal heart defects;
- bad heredity;
- smoking, excessive alcohol consumption, drug use;
- intoxication due to taking drugs prohibited during pregnancy;
- work in hazardous production;
- bad ecology;
- avitaminosis;
- various infectious diseases (rubella, herpes, toxoplasmosis);
- chronic stress;
- endocrine diseases;
- long-term toxicosis.
Symptoms
The main problem is that the saddle-shaped form of the reproductive organ is a pathology that does not manifest itself in any way, the woman’s well-being remains normal, and the menstrual cycle is not disrupted. A woman may not be aware of the disease for a long time. If the internal structure of the uterus is severely distorted, then this can be suspected by the absence of conception during regular sexual activity. But to be sure, you need to be examined by a gynecologist.
For comparison, this is what a normal uterus without anomalies looks like. There are no septa or arch on top, like a saddle uterus
If changes in the shape of the uterine fundus are not so pronounced, then pregnancy is quite real. But, as a rule, this condition is accompanied by various disorders, including miscarriage. There may also be constant threats of miscarriage or premature birth. Irregular structure of the uterus always causes problems during pregnancy.
Types of developmental anomalies
Normally, the uterus is pear-shaped and has a cervix, body and fundus, which is dome-shaped. It is formed from two Müllerian ducts, which merge to form a cavity. The bicornuate form occurs with incomplete fusion, and the one-horned form with atrophy of one of the ducts.
A distinction is made between complete or incomplete fusion and, depending on this, it may be:
- complete separation of the uterus, cervix and even vagina by the septum, in this case there are two cervixes and two separate horns, there may be a septum in the vagina;
- the septum divides only the uterus, there is only one cervix, the horns may be evenly developed, or one horn may be smaller than the other and may be atrophied;
- the septum does not completely divide the uterus;
- There is no septum, but there is a flattening of the uterine fundus, this is called a saddle uterus.
Important! A unicornuate uterus can occur when one horn atrophies or when one of the Müllerian ducts atrophies during the period of organogenesis. This pathology is often accompanied by the absence of one kidney. A woman's chance of becoming pregnant is low, since only one ovary can produce an egg, and at the same time, this is the most serious pathology in which it is difficult to bear a child.
A developmental anomaly may also occur when the horn is separated from the cavity; this is a rare but complex pathology that requires surgical intervention in adolescence.
Diagnostics
A female doctor will help establish the correct diagnosis. But you should know that a routine examination in a gynecological chair will not reveal pathology. There are also no external signs of a saddle uterus; you will not be able to independently identify such an anomaly. The most reliable diagnostic method is an ultrasound examination, during which the saddle shape of the uterus is determined. It is recommended to do an ultrasound in the second phase of the menstrual cycle. After all, it is at this time that the endometrium reaches its optimal thickness. But if the deformation is insignificant, then even ultrasound will not detect it. In such cases, additional instrumental methods for diagnosing the saddle uterus are used:
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- hysteroscopy (intrauterine insertion of a special camera of minimal size to examine the condition of the organ);
- metrosalpingography (ultrasound or radiographic examination of the uterine cavity after the introduction of a contrast agent into it).
The saddle uterus can be detected using ultrasound. However, if the severity is mild, ultrasound may not recognize the anomaly.
Forecast
With severe clefting of the uterine cavity, the likelihood of premature birth or spontaneous abortion increases. Management of pregnancy in women with a bicornuate uterus involves the prevention of miscarriage, bleeding and the development of isthmic-cervical insufficiency.
For patients with insufficient volume of the uterine cavity, it is possible to give birth to a child thanks to modern reproductive technologies, namely in vitro fertilization with surrogacy.
Treatment
The saddle shape of the uterus is always detected suddenly. In this regard, doctors usually prefer to monitor the patient for a certain period of time, without using radical treatment methods. A long absence of pregnancy against the background of a deformed uterus becomes a reason for surgical intervention.
The operation is also advisable for miscarriage and frequent miscarriages. Correction is usually carried out through a hysteroscopy procedure. In some cases, it is necessary to operate through incisions in the abdominal cavity. It is important to understand that the diagnosis of saddle uterus is not amenable to conservative treatment. Medicines, injections, and traditional medicine methods will not help the patient. The only way out is surgical correction of the uterine fundus.
Multiple pregnancy
A woman with a multiple pregnancy faces additional challenges. It is difficult for two or more embryos to fit into the uterine cavity, which has an irregular shape. Such a pregnancy is more likely to end in miscarriage. In most women who have a bicornuate uterus and become pregnant with twins, children are located in the left and right horns. They are usually born prematurely and have a low birth weight. The only option for delivery during such a pregnancy is a cesarean section.
How to get pregnant with a saddle uterus
It is possible to conceive a child with a saddle-shaped uterus. If the severity of the anomaly is insignificant and the muscle structure is not changed, then pregnancy will not be long in coming. Women often learn about this diagnosis only at the first screening, around 12 or 13 weeks. If there is a pronounced anomaly in the structure of the uterus, the process of bearing a child can be very problematic and difficult.
Conception position
Many women believe that the success of conception depends on the correctly chosen position, giving preference to the knee-elbow position. But doctors refute this opinion; the position during sexual intercourse does not matter, because disruption of the process of penetration of sperm into the fallopian tubes is not associated with subsidence of the uterine fundus. The problem is whether the endometrium will accept a fertilized egg.
The position for conception with a saddle uterus is not particularly important; any position will do.
So, the incorrect shape of the reproductive organ is not a 100% reason why pregnancy will not occur. But at the same time, the saddle uterus is, to a certain extent, considered a small obstacle to the desired motherhood. In any case, with minor deviations in the shape of the organ, a long absence of pregnancy may mean the presence of additional problems in the reproductive system. A bicornuate uterus is often accompanied by other disturbances in the functioning of the urogenital tract.
Structure of the uterus
The uterus of an adult woman has an ovoid shape. Women who have not given birth have a pear-shaped uterus. The structure of the organ can be divided into several parts.
- The fundus is the upper part, protruding above the line of confluence of the fallopian tubes.
- The body is the middle, largest part of the organ.
- The isthmus is the junction of the uterine body and the cervix.
- The neck is the lower part. It is divided into two sections: supravaginal and vaginal.
The organ has two surfaces:
- anterior (vesical): located next to the bladder;
- posterior (intestinal): adjacent to the rectum.
The uterus is supported by the ligamentous apparatus, which includes:
- round ligament;
- own ligament of the ovary;
- broad ligament;
- cardinal ligament (paired).
The weight and size of the uterus may vary from woman to woman. On average, the weight is 40 g (for nulliparous women) -100 g (for those who have given birth). The average length is 5.5 cm, and the width is 3.5-4 cm; in women who have given birth, these sizes increase. The volume of the uterine cavity is 5 cm3. During pregnancy, the size of the organ increases significantly.
The thickness of the uterine wall is 1 cm. It consists of three components.
- The endometrium (mucous membrane) lines the inside of the uterine cavity. The endometrium consists of two layers. Functional (superficial) - during menstruation it is almost completely rejected. Basal (located deep): its function is to restore the functional layer.
- The myometrium (muscular membrane) consists of three layers. External: muscle fibers are predominantly located longitudinally and obliquely. Medium: muscle fibers are arranged circularly. This layer is most developed in the cervical area. Otherwise, it is called the vascular zone, due to the location of large blood vessels in it. Internal: the arrangement of muscle fibers is the same as in the outer layer.
- Parametrium (serous membrane) is part of the pelvic tissue.
Features of pregnancy with a saddle uterus
A pregnant woman diagnosed with a saddle uterus must be constantly under strict medical supervision from the early stages until the end of the gestational process. This anomaly always threatens miscarriage or premature birth. Against the background of deformation of the uterine fundus, the fertilized egg is often attached in the pharynx area. Pregnancy with a saddle uterus is very dangerous and can lead to the following consequences:
- Spontaneous termination of pregnancy.
- Early placental abruption.
- Malposition.
- Bleeding, etc.
Timely preventive and therapeutic measures and careful adherence to doctor’s instructions will help you avoid all this.
Another danger during pregnancy with a saddle uterus is the possibility of an unsuccessful placement of the placenta. This can lead to disturbances in its nutrition and a slowdown in metabolic processes. The entire period of gestation will be complicated by the threat of miscarriage. The stronger the deformation, the more problems await the woman on the path to motherhood.
During pregnancy with a saddle uterus, some complications may occur. The expectant mother should be regularly observed by a gynecologist.
In many cases, an acute threat of miscarriage is accompanied by the formation of a hematoma between the endometrium and the membranes. To maintain pregnancy it is indicated:
- Special medications to prevent miscarriage.
- Antispasmodics.
- Metabolic agents.
- Tocolytics.
- Preparations for normalizing uteroplacental circulation.
It is very important to maintain bed rest and absolute physical and sexual rest throughout the entire pregnancy.
Possible risks
If the shape of a woman’s uterus is not pear-shaped, but saddle-shaped or bicornuate, then this threatens the woman with problems conceiving and bearing a child. Doctors who have encountered anomalies in their practice provide data on the possibility of a normal onset and course of pregnancy in 50% of cases.
The most common problems that may arise in a woman who does not have a pyriform uterus are:
- abnormal placentation;
- pathological presentation of the fetus;
- threat of premature placental abruption;
- risk of premature birth;
- pathologies of labor;
- the occurrence of obstetric bleeding.
Incorrect placentation
A pregnant woman with an abnormal uterine shape (not pear-shaped), due to the specific structure of the organ, has a high risk of developing placenta previa.
- Incomplete: the placenta partially covers the internal os.
- Complete: the placenta completely covers the internal os.
- The placenta does not cover the internal uterine os, but is located too low.
For a woman with an abnormal and non-pyriform uterus, abnormal placentation is at risk of developing complications:
- Bleeding: may occur and be a concern several times throughout pregnancy. The cause is premature placental abruption. It develops due to an increase in the size of the organ and insufficient elasticity of the placental tissue. Premature detachment threatens miscarriage. A feature of bleeding with abnormal placenta previa is the absence of pain;
- fetal hypoxia: the detached area of the placenta stops supplying the fetus with oxygen and other nutrients;
- decreased blood pressure in women;
- delayed fetal development;
- Iron-deficiency anemia.
The abnormal location of the placenta in the bicornuate form is due to the attachment of the egg in an abnormal place. In the pyriform organ, the embryo is able to fully attach.
Malpresentation
Often with a bicornuate form, the growing fetus is located incorrectly in it. This anomaly in the structure of the organ is most characterized by a transverse position and breech presentation. Unlike abnormal forms, pyriform provides longitudinal presentation.
The transverse position is characterized by the fact that the fetus lies across the pelvis. In this case, delivery is possible only by caesarean section.
With a breech presentation, the baby is positioned towards the exit of the uterus with its pelvic end. Theoretically, with proper obstetric care, natural childbirth with this pathology is possible. But, since the bicornuate form can cause discoordination of labor and weakness of labor forces, in most cases the woman is given a surgical delivery. The final decision is made by the doctor delivering the baby, guided by the characteristics of the individual patient.
Fetal anomalies create an additional risk of bleeding. In the pear-shaped uterus, the fetus is given the opportunity for normal maturation and growth.
What does this mean?
Approximately 22% of women aged 18-35 have a pear-shaped uterus. The main parameters are presented in the table.
| Form | Pear-shaped. The wide part is turned upward. |
| Top part | Referred to as the "bottom". |
| Bottom part | Also called the isthmus, it ends at the uterine cervix. Communication with the vagina occurs using a special rope. |
| Length | 7-8 centimeters. |
| Width | 4-5 centimeters. |
| Weight | 50-60 grams |
What does it mean? A pear-shaped organ cannot be completely called a pathology. This form was laid down by nature. The main purpose is to bear only 1 fetus.
Prevention
To prevent a saddle uterus from occurring, even before planning a pregnancy, a woman should observe the following preventive measures:
- timely treatment of infectious diseases and inflammatory processes of the reproductive system;
- prepare well for pregnancy, undergo the necessary examination and start taking vitamin and mineral complexes;
- lead a healthy lifestyle;
- balance your diet so that it contains many plant components;
- visit a gynecologist regularly;
- register with a gynecologist during pregnancy up to three months.
This deviation is not a death sentence, so a woman can conceive, carry and give birth to a completely healthy baby. She just needs to be careful about her health.
Functional changes during the monthly cycle
The monthly (menstrual) cycle is a complex of periodic changes in the endocrine system, ovaries and endometrium, aimed at conception. Cycle length may vary and range from 3 to 5 weeks (or 28 ± 7 days).
Functional changes in a woman’s body occur in three stages.
| Cycle phase | Changes in the ovaries | Changes in the endometrium |
| I Lasts from 7 to 22 days | Follicular phase | Menstrual phase |
| In the pituitary gland, under the influence of gonadoliberin, the synthesis and release of FSH1 and LH2 into the blood begins. Under the influence of FSH, several follicles mature in the ovaries, one of which becomes the main (dominant). This follicle begins to synthesize estradiol in large volumes, which, in turn, causes an increase in the synthesis of gonadotropins. The concentration of GnRH increases in proportion to the growth of the dominant follicle until a sharp release of LH from the adenohypophysis occurs. | If the egg has not been fertilized, epithelial detachment occurs. This is manifested by menstrual bleeding. | |
| II Duration – about 3 days | The dominant follicle continues to grow and secrete estradiol. A follicle that has reached maturity and is ready for ovulation is called Graafian vesicle (GV). The LH surge is the final stage of HP development. There is a release of dissolving enzymes that destroy the follicle wall. A mature egg, ready for fertilization, emerges from the GP cavity. | |
| III Lasts 13 – 14 days | Luteal phase | Secretory phase |
| After rupture, the walls of the GP collapse, and a new endocrine organ is formed - the corpus luteum (CL). VT releases estradiol, progesterone and androgens. If the egg has been fertilized and successfully attached to the uterine wall, the VT secretes progesterone until the placenta has formed and begins to secrete estrogen and progesterone. If pregnancy does not occur, the VT is destroyed, which causes a decrease in progesterone and estrogen levels. | Estrogen and progesterone cause the endometrial glands to mature. These glands begin to actively secrete, preparing the endometrium for attachment (implantation) of a fertilized egg. If pregnancy does not occur, in the absence of the influence of estrogen and progesterone of the corpus luteum, the endometrium begins to swell and necrotize. Eventually it is rejected and the cycle starts again. | |
FSH – Follicle stimulating hormone.
LH – Luteinizing hormone.
Structural features and functions
The structure and location of the uterus are subject to frequent changes. It is influenced by internal organs, the period of gestation, and processes that occur every menstrual cycle.
The condition of the cervix determines the onset of ovulation. During this period, its surface becomes loose, the mucus becomes viscous, and it drops lower than on other days of the cycle.
In the absence of conception, menstruation occurs. At this time, the upper layer of the uterine cavity, the endometrium, is separated. In this case, the internal pharynx expands to allow blood and part of the mucous membrane to escape.
After the cessation of menstruation, the pharynx narrows and the layer is restored.
The functions of what the uterus is needed for are defined:
- reproductive - ensuring the development, gestation and subsequent expulsion of the fetus, participation in the formation of the placenta;
- menstrual - the cleansing function removes part of the unnecessary layer from the body;
- protective - the neck prevents the penetration of pathogenic flora;
- secretory - mucus production;
- supporting - the uterus acts as support for other organs (intestines, bladder);
- endocrine - synthesis of prostaglandins, relaxin, sex hormones.
to contents ^
Inflammatory diseases of the cervix
Almost every fifth woman is diagnosed with various inflammatory diseases of the cervix. Although medicine does not stand still and is constantly evolving, the likelihood of inflammation remains high.
It can make itself felt at any age, resulting in complications:
- erosion - small defects or disorders of the mucous membrane;
- erythroplakia - a disease of the outer membrane, which is diagnosed by the appearance of a red spot;
- papillomavirus infection and candylomas - requires regular tests and visits to the gynecologist;
- cancer diseases.
Due to the internal structure of the cervix, the likelihood of inflammation increases. At a certain age, when the tissues of the inner wall of the uterus undergo restructuring, there will be a high probability of violations.
Some fabrics tend to literally displace others, and quite slowly. This process does not always go smoothly, without consequences and complications. This can seriously undermine women's health.
Influencing factors:
- periodic hypothermia;
- colds;
- viral and bacterial infections;
- diseases of the endocrine system;
- various mechanical injuries;
- not following a proper diet;
- frequent stressful situations and overwork.
The above factors greatly undermine the immune system and the functions of the body as a whole, which leads to interruptions in the functioning of some organs and the appearance of formations.
You should not delay treatment, because a benign tumor can turn into a malignant tumor if left untreated. Here the question will arise not only about the health, but also the life of the patient.
Classification
A saddle-shaped bicornuate uterus may not be the only defect of the reproductive system. In parallel with it, pathological changes in the vaginal walls or in the cervix can be detected.
Scientists distinguish several types of uterine shapes:
- one-horned;
- two-horned;
- double, but there are other forms.
The bicornuate uterus, in turn, comes in three types:
- Full two-horned. In this case, the division of the organ occurs into two peculiar “horns” in the area of the sacrouterine folds.
- Incomplete bicornuate. It also has two branches similar to “horns”, but they are identical only at the top.
- Saddle-shaped. Expansion is observed in the transverse section, and there is also indentation in the bottom area. It is shaped like a saddle.
In the latter view, the split into two “horns” is practically not visible. A characteristic feature of such a defect is that a woman may not even be aware of it, because she absolutely does not feel any pain.