Which birth control pills are non-hormonal?
Non-hormonal contraceptives for women differ from alternative ones in that the quality of the active ones is acquired by substances called spermicides. This composition of medications allows you to avoid adverse changes in the body and health. The principle of action of tablets that do not contain hormones is based on the destruction of sperm, creating an obstacle from mucus on the cervix.
New generation non-hormonal birth control pills have a number of advantages:
- they are allowed to be taken during lactation and pregnancy;
- reception is carried out as needed, and not according to a specific schedule;
- do not irritate the lining of the uterus, do not cause harm;
- allowed to be used for diseases (for example, uterine fibroids);
- the harm of such tablets is limited to allergies;
- able to fight infections in the genitals.
Disadvantages of such drugs:
- use a few minutes before sex;
- It is allowed to take a shower and use soap only after some time has passed;
- not suitable for daily use;
- Allergic reactions may occur.
After the act
Sometimes situations arise when urgent contraception is necessary. Protection is called emergency because its use is intended in emergency situations. Pills against pregnancy after unprotected intercourse are such. Unfortunately, non-hormonal drugs are not available for oral administration. When you use contraceptives after sex, you deal your body a huge blow. It is necessary to use emergency contraceptive pills as rarely as possible - take responsibility for your health.
Contraceptive vaginal pills
There are a large number of types of contraceptives for women and girls. Medicines for vaginal administration are one type. They do not contain hormones, which means they do not cause the problems that may arise from taking hormonal medications. Such contraceptives are the safest birth control pills. There are a large number of such pills on the shelves of modern pharmacies. It is best to leave it to your doctor to determine which ones are right for you.
https://youtu.be/t7FnzPDq8dc
List of hormonal drugs
Hormonal agents have different structures and chemical compositions. Depending on what kind of substances hormonal drugs contain, the types of these drugs are as follows:
- Drugs of protein and peptide structure
- preparations of hormones of the hypothalamus, pituitary gland, parathyroid and pancreas. - Amino acid derivatives
– preparations of the thyroid gland, pineal gland hormones. - Steroid compounds
are preparations of hormones of the adrenal cortex and gonads.
Hormone replacement therapy drugs
Hormone replacement therapy is a complex treatment aimed at restoring the function of the endocrine glands in case of their primary disruption. The effectiveness of this therapy requires constant use of medications. If the body does not receive the required amount of the hormone, the symptoms of the disease only intensify. In many cases, patients must take medications for the rest of their lives. For example, with diabetes, the patient needs to constantly inject insulin.
With a lack of sex hormones, women also have to constantly take hormonal medications. An urgent need for them arises during menopause. Women are prescribed the following hormonal drugs during menopause:
- estrogen-based medications - Premarin, Ovestin, Femoston;
- products based on gestagens - Diane-35, Duphaston;
- combined - Livial, Divina, Klimonorm.
Hormonal drugs for oncology
Hormonal therapy gives good results in the complex treatment of hormone-dependent tumors. Such pathologies include:
- mammary cancer;
- uterine cancer;
- prostate tumor;
- pancreatic tumor;
- kidney cancer
When it is necessary to suppress excess androgen synthesis, estrogen-containing drugs are often prescribed and, conversely, when there is an excess of estrogen, androgen-containing hormonal drugs for men are used. As an example of drugs used in the treatment of oncological tumors, the following hormonal drugs can be distinguished:
- Medrosterone propionate;
- Proloteston;
- Phosfestrol;
- Estracite.
Hormonal contraceptives
Hormonal pills for women are the most famous of medications containing hormones. The mechanism of their action is as follows:
- the drug suppresses ovulation;
- thickens the mucus in the cervix, preventing sperm from penetrating into the uterine cavity.
Hormonal means to prevent unwanted pregnancy are constantly being improved. At the same time, they also have an effect on appearance, stabilizing the functioning of the sebaceous and sweat glands. Many girls call them hormonal acne pills, but this is just an additional effect of use. Among the types of medications actively used by women today, it is necessary to highlight the following:
- Combined contraceptives: Janine, Logest, Diane-35.
- Mini-pills: Microlut, Micronor, Norkolut.
- Injectable contraceptives: dihydroxyprogesterone acetophenide (DHPA), dihydroxyprogesterone caproate.
- Subdermal implants: Implanon.
- Hormonal vaginal rings: Nuvaring.
- Contraceptive patch: Evra.
- Postcoital drugs: Agest, Mifegin, Escapelle.
Symptomatic hormonal drugs
In some cases, hormonal drugs may be prescribed as a means for symptomatic treatment. Hormones are used when it is not possible to eliminate the manifestations of the disease for a long time, for example, in case of allergies. In such cases, hormonal medicine for a runny nose gets rid of it in a matter of minutes. In this case, drugs based on glucocorticoids are used.
They have a pronounced anti-inflammatory and antiallergic effect, but can provoke side effects. Self-administration is prohibited. Among the hormonal drugs in this group:
- Prednisolone;
- Metipred;
- Dexamethasone;
- Hydrocortisone.
How to use
The package contains instructions for use, which detail the mechanisms for using the medicine, but there are general rules and how to use the medicines. Vaginal contraceptives must be taken 10-15 minutes before sexual intercourse. If sex does not occur within 2 hours after using the drug, the procedure will need to be repeated. For ease of administration of the pill, the package may contain a special applicator, with its help the product will be injected deeply.
The instructions for some medications instruct you not to shower or use intimate hygiene products for some time before and after sex. Single-use medications can cause irritation and burning in the intimate area. If symptoms occur, the medication should be discontinued. Before using medicinal contraceptives, you should consult your doctor.
Name of birth control pills
New generation non-hormonal contraceptive pills:
- "Pharmatex"
The activity of the substance lasts from 3 to 4 hours, depending on the form of the drug, after 10 minutes. After insertion, it becomes possible to have sexual intercourse.
- "Ginecotex"
The pill should be inserted along the anterior wall of the vagina within 5 minutes. before sex. The activity lasts for a long time - about 4 hours.
- "Benatex"
The pill must be placed deep, up to the cervix. This should be done about 10 minutes before sexual intercourse.
- "Erotex"
The dosage form of the drug is suppositories. Use it 10 minutes before sex. The substance will be active for 3 hours.
- "Contratex"
The activity of the pill begins after 10 minutes. after administration, lasts up to 4 hours.
- "Patentex Oval"
It is a vaginal suppository that is placed inside the vagina 10 minutes before sexual intercourse.
- "Traceptin"
The pill must be administered 10 minutes before. before sex. Itching and burning may occur.
Birth control pills after 40 years of age must be selected with special care, because the body is prone to developing chronic diseases, and the number of contraindications for taking hormonal drugs increases. The use of non-hormonal contraceptives is suitable at this age even earlier (after 35 years), if you have irregular sexual intercourse. In addition, the drugs have anti-inflammatory and antibacterial effects, which is very important. Medicines of this type are allowed to be used during pregnancy and lactation.
A full sex life is an important component of the relationship between a man and a woman. Long gone are the days when women tried to protect themselves from unwanted pregnancy with the help of traditional medicine and local barrier methods that were shockingly inventive. The modern pharmaceutical market offers a wide selection of contraceptives that are reliable and pleasant to use.
In what cases should women take hormonal pills?
Many girls, when the phrase “hormonal drugs” is mentioned, instinctively feel threatened and afraid. Indeed, in the understanding of most representatives of the fair sex, who have nothing to do with the field of medicine, hormones are pills that have monstrous power and bring a large number of similar effects.
Classification Features
Hormonal medications contain special substances that have properties similar to hormones. The production of the latter elements occurs in human endocrine functions, and they spread throughout the body along with the blood, affecting the systems they need.
Interesting: Leukocytes in Urine During Pregnancy What is it?
The conditional classification of hormonal drugs assumes the existence of several groups.
The pituitary gland produces hormones such as gonadotropin and oxytocin. The products can be used by any woman if it is necessary to take on the treatment of hypothyroidism, when there is insufficient production of her own hormones.
Pancreas - traditionally this group includes basic drugs, for example, insulin and parathyroid glands. This group involves the use of widely known drugs.
Sex hormones are androgens and anabolics. These drugs are taken when it is necessary to normalize reproductive function after undergoing a special consultation with a specialist.
What is treated with hormonal drugs
Although many people are wary of these drugs, it can be said that they play an important role in the lives of many women and are related to essential substances.
Why is hormonal therapy needed:
- Contraception - in this case we mean hormonal therapy during menopause in men and women;
- In order to eliminate inflammatory processes in the body and various types of allergies;
- If it is necessary to get rid of hormonal deficiency - in the form of hypothyroidism, diabetes mellitus;
- The use of hormonal drugs for various types of cancer is justified.
Hormonal pills: benefit or harm?
Modern hormonal drugs are not created for the purpose of helping people actively fight various problems.
That is, by taking only them, you cannot get rid of excess weight or excess hair growth, so taking them solely for cosmetic purposes is the wrong decision. If you decide to take such medications, you should expect that they will only help you get rid of several things.
Taking hormonal medications without a doctor's prescription is STRICTLY NOT RECOMMENDED, since self-medication can lead to irreversible processes.
Only with the help of a competent doctor can you get rid of the problem, create protection and gain confidence in your own health. In this case, hormonal products can not only give you a wonderful internal state, but also improve your appearance, giving your skin beauty.
Many people are convinced that taking hormonal pills is a necessity for changes inside and outside. In principle, if you consult a good endocrinologist and go to a gynecologist, they can refute this myth.
However, in many cases, hormonal drugs are prescribed for the treatment of a wide range of diseases.
Hormonal pills during pregnancy
Insufficient production of hormones can also be encountered during pregnancy, since hypothyroidism is an often unpredictable disease.
If there is a need to take medications designed to help in the fight against illnesses, you can take the drugs, but only if you first consult with your doctor.
Hormonal tablets for mastopathy
Remedies for the presence of this disease are also prescribed by a specialist. Mastopathy is a benign formation in the mammary gland, which grows pathologically and can lead to side effects in the absence of proper timely treatment.
If this disease appears, you need to consult a doctor - a mammologist, who will give several recommendations and help you figure out the treatment.
Hormones for fibroadenoma
The occurrence and development of this disease is strongly influenced by a woman’s hormonal background, so it is necessary for treatment to ensure that the hormones are normal. If this factor is not present, the specialist prescribes high-quality and proven hormonal drugs.
The influence of hormonal levels on conceiving a child is undeniable. Elements such as prolactin, estradiol, progesterone, testosterone and others appear here.
By the time of planning pregnancy, many women are faced with insufficiently well-developed hormonal levels, so they have to make a lot of effort to normalize it. In such cases, your doctor may prescribe hormones.
Benefits of non-hormonal remedies
Despite the increasing demand for oral contraceptives containing hormones, non-hormonal contraceptives are widely used among women of different age categories. The variety of forms used allows you not to limit the sex life of your sexual partners, to get the desired pleasure, and not to lose interest in sexual life.
Vaginal contraceptives are a chemical method of contraception based on the spermicidal effect of the main components of the drugs (nonoxynol or benzalkonium chloride) when applied locally (vaginally).
Release forms
Non-hormonal contraceptives have the following forms:
- candles (suppositories);
- balloons;
- cream;
- aerosol;
- vaginal tablets;
- capsules.
The increased interest in vaginal contraceptives that has arisen in recent decades has been facilitated by media advertising the benefits of this type of contraception. The search for an option to protect against unwanted pregnancy without the use of hormones leads to an alternative - a chemical method of protection.
Indications for the use of chemical contraception
This method is indicated in the following situations:
- lack of regular sexual relations;
- postpartum period and lactation period;
- contraindications to the use of hormone-containing drugs;
- the presence of chronic diseases of the circulatory system, endocrine system and genitourinary system;
- absolute or temporary contraindication to the use of barrier methods of contraception (intrauterine device, cervical cap, diaphragm, condom);
- severe menopausal syndrome, manifested by structural changes in the vaginal mucosa;
- errors in the use of oral hormonal contraceptives.
The almost complete absence of side effects and the absolute availability of purchase make it possible to evaluate the positive characteristics of these funds.
Intrauterine contraception
Intrauterine contraception is one of the most common and effective methods of preventing pregnancy, and in Russia it ranks first in popularity.
Intrauterine contraceptives (IUC) are inert (made of polyethylene) and medicated, containing copper or gestagens. The advantages of this method include high efficiency, no systemic effect on the woman’s body, no effect on breastfeeding, low cost, and rapid restoration of fertility after removal of the IUD.
The disadvantages of the IUD include more abundant and painful menstruation, especially during the first year of using the device, the risk of developing inflammatory diseases of the pelvic organs in the first weeks after insertion of the device, and limited use in young nulliparous women.
Absolute contraindications to the introduction of an IUD:
- acute and subacute inflammatory diseases of the pelvic organs
- often recurrent chronic diseases of the pelvic organs
- malignant diseases of the genitals
- bleeding from the genital tract of unknown cause
- pregnancy (including suspected)
Relative contraindications to the use of IUDs:
- history of pelvic inflammatory diseases
- vaginitis at the time of examination
- menstrual irregularities
- endometriosis
- cervical deformity
- anemia
- tuberculosis
- rheumatic heart disease
- severe allergies, especially to copper
- previous genital tract infections and sexually transmitted diseases within 12 months
- having multiple sexual partners
- treatment with immunosuppressive drugs, etc.
After insertion of the IUD, examination is carried out after 1 month, and then at least once every 6 months.
Advantages of non-hormonal contraceptives
Positive characteristics include:
- absence of side effects associated with changes in hormonal levels;
- do not require control over the application regimen;
- prevent infection by pathogenic flora;
- easy to use, have a pleasant aroma;
- act as a lubricant, moisturizing the vaginal mucosa;
- the best type of contraception during the postpartum and lactation period.
Despite the advantages of non-hormonal contraceptives, like any drug, they also have negative characteristics.
Disadvantages of non-hormonal contraceptives
The disadvantages of non-hormonal contraceptives include:
- lower efficiency compared to drugs containing hormones;
- require preparation for sexual intercourse (preliminary introduction 5-10 minutes);
- with frequent use they cause local allergic reactions in the form of redness, burning and itching;
- contraindication to water procedures after coitus using personal hygiene products;
- reduce their effectiveness during the use of antibacterial or steroid drugs;
- not recommended in the presence of acute inflammatory processes in the vagina and cervix, or with vaginal bleeding.
The choice of a non-hormonal drug must be approached consciously. A consultation with a gynecologist would be most appropriate. The doctor will select non-hormonal birth control pills, taking into account experience of use among different age groups, analysis of effectiveness, indications and individual characteristics of the body.
As practice shows, most women prescribe contraceptives on their own, basing their preference on the opinions of friends who advertise the drugs, as well as thanks to advertising in the media. Often the choice is based on the advice of the pharmacy pharmacist. What topical medications are most effective? Which non-hormonal pills will be better?
The top 10 most used drugs, according to medical statistics, include the following vaginal contraceptives:
- Pharmatex;
- Gynekotex;
- Benzalkonium chloride;
- Erotex;
- Contratex
- Patentex Oval;
- Nonoxynol;
- Traceptin;
- Conceptol.
The drug Pharmatex based on benzalkonium chloride has proven itself well. It is available in the form of vaginal tablets, vaginal tampons, suppositories, and cream. The spermicidal effect of the drug destroys the sperm membrane. The thick mucus that forms interferes with the fertilization process.
Each individual suppository is indicated for one-time use before sexual intercourse. The activity of the drug and the duration of action depend on the form of release of the drug. The most effective is Pharmatex in the form of a cream, which retains its activity for up to 10 hours after insertion into the vagina. In addition, a bactericidal effect was noted against certain types of bacteria and viruses: chlamydia, trichomonas, Staphylococcus aureus and herpes.
Remains of the product can be removed with plain water a few hours after coitus. Any type of local contraceptives should be administered in a horizontal position of the body. The widespread use of Pharmatex by women of all ages determined its inclusion in the top ten most popular means of protection.
Ginekotex vaginal contraceptive tablets are indicated for intravaginal use. The effect is similar to the previous drug, but has a wider range of bactericidal effects, including enterococci, candida, HIV and others. Incompatible with iodine preparations that inactivate the molecules of the active substance. During sexual intercourse, it is enough to insert the tablet once into the vagina. Single-use tablets are taken topically, slightly moistened with water.
The contraceptive effect of Erotex is due not only to the thickening of cervical mucus and the creation of a film that impedes the movement of sperm, but also to the separation of the head from the sperm flagellum. Disposable vaginal suppositories, which are inserted into the vagina, are no less effective than low-dose oral contraceptives.
Erotex, having a broad antimicrobial effect, does not disturb the general microbial landscape of the vagina, is not absorbed by the vaginal walls, and does not enter the systemic bloodstream. Single-use contraceptive suppositories have a pleasant aroma: lemon, rose, lavender, vanilla.
Contratex is presented in the form of vaginal suppositories, which have spermicidal, antibacterial, antifungal and antiviral effects against most strains of pathogenic flora, including resistant species. Intravaginal administration into the vagina ensures the drug is active for 1 to 4 hours.
Traceptin vaginal tablets, which contain potassium hydrogen tartrate, are inserted into the vagina 10 minutes before sexual intercourse. They have active spermicidal and antimicrobial activity.
The drugs Patentex Oval, Nonoxynol and Conceptrol are based on nonoxynol. It reduces sperm motility by creating a chemical barrier. It is better to administer suppositories or cream using a special applicator 10 minutes before intercourse. The active substance nonoxynol has antimicrobial activity against most pathogenic microorganisms: bacteria, viruses, fungi.
Non-hormonal contraceptives remain effective when used correctly. A single dose of the drug can be combined with other types of contraception. A hormonal contraceptive in combination with a non-hormonal contraceptive, taken for the first time before sexual intercourse, significantly increases effectiveness. Non-hormonal drugs combined with barrier methods of protection (condom, IUD, etc.) also increase the chances of success.
Let the choice of an effective non-hormonal contraceptive be entrusted to a gynecologist who has analyzed the general condition of the female body and its individual characteristics.
Among modern contraceptives, a special place is occupied by single-use contraceptive pills, that is, those that are not taken regularly, but only in an emergency. Such situations are considered:
- unprotected sexual intercourse;
- use of unreliable means and methods of contraception during sexual intercourse;
- unsuccessful use of other contraceptives (for example, condom rupture).
Non-drug methods of contraception
The most popular methods of contraception without medications are male condoms, the rhythmic method (based on cervical mucus, basal temperature and tests), and the radical and irreversible option is surgery.
Traditional: mechanical and rhythmic
Traditional is the use of condoms (mechanical contraception) and the rhythmic method.
Types of male contraceptives
Mechanical male contraception remains in first place in popularity. It allows men to regulate the process of childbirth and is as affordable as possible in terms of price and availability. At the same time, an extremely important advantage is protection against HIV infection and diseases transmitted through sexual contact. Condoms are available in several types:
- ultra-thin – make it possible to feel your partner better;
- different designs, adding variety to sexual relations - black, colored, with aromas, flavoring additives, pimples, ribbed, luminous;
- increased size (larger than standard by 10 mm in length and 2 mm in width);
- especially durable (thickened);
- anatomical (completely encircles the penis);
- lubricated with an anesthetic, which dulls the sensitivity of the penis, thereby prolonging sexual intercourse;
- treated with spermicide, which enhances the contraceptive effect.
Physiological rhythmic: cervical, temperature, symptothermal, tests
The method of protection for determining safe days is called rhythmic and can be carried out in the following ways:
- by cervical mucus (cervical) - before the release of the egg from the follicle (ovulation), it is released in large quantities, transparent, and slippery to the touch, from this time and for 4 days after you need to avoid sexual intercourse;
- measuring the temperature in the rectum - it drops sharply during ovulation, the dangerous period is from the beginning of menstruation to a minimum and another 3 days after;
- calendar - with a 28-day cycle, fertilization is most likely from 7 to 17 days, and with an unstable one - from 26 to 30 days (8-19, that is, almost the middle); for individual calculations, the rule is used: minus 18 days from the shortest cycle (beginning ) and minus 11 from the longest (end);
- symptothermal - a combination of mucus monitoring and temperature measurement helps to more accurately determine the time of ovulation.
The effectiveness of this method can be significantly increased with the help of tests. They are sold in pharmacies in 2 versions - a miniature microscope that examines saliva (Vesta, Arbor, Eva-test) and strips for dipping into urine (the principle is similar to a pregnancy test), the most popular are “Solo”, “Be sure”. When used correctly, testing is much more reliable than other rhythmic options.
Irreversible method
The surgical method is irreversible, since the operation is aimed at the complete impossibility of conception in the future. Extremely rare cases of fertilization are explained by incomplete intersection of the tubes or spermatic cords and amount to 1-2 per 1000 operated patients. Before deciding to undergo sterilization as a method of preventing pregnancy, it is important to consider:
- restoring the patency of the fallopian tubes after ligation often has no effect;
- There remains the possibility of artificial insemination, which will require lengthy and expensive preparation.
Therefore, sterilization always takes place only after written consent and awareness of all risks.
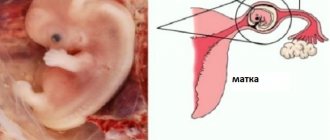
In women, surgical options include tubal ligation or tubal severance. There is also complete removal of the uterine cavity, but this operation is used exclusively for diseases. Often such surgical interventions take place after a caesarean section, when subsequent pregnancies threaten the woman’s life.
Access to the tubes is possible through the abdominal wall with the introduction of an endoscope. This option is called laparoscopic sterilization. A substance that hardens (sclerosant) can also be inserted through the vagina.
Complications of sterilization include:
- damage to neighboring organs (especially with adhesions, adhesions after inflammation or surgery);
- intolerance to anesthesia;
- inflammatory process;
- pain in the lower abdomen, bleeding;
- ectopic (ovarian) pregnancy.
For men, the ducts through which sperm move are removed. The operation is performed under local anesthesia and is easier to tolerate than in women. Options:
- introduction of sclerosant, silicone plug;
- bandage, clip;
- thermal effects (diathermocoagulation);
- excision with a scalpel.
Male sterilization
It is important to note that male sterilization does not appear immediately; you need to get tested after 3 and 4 months. If there are no germ cells in the sperm twice, then the operation is considered successful. Infrequent adverse effects include:
- subcutaneous hemorrhage in the scrotum;
- inflammation of the testicles;
- penetration of infection into the wound.
Disposable contraceptives - effectiveness of use
Today, hormonal drugs are the most effective contraceptives. Various manufacturing companies conduct their own research on this issue. For example, Postinor guarantees that pregnancy will not occur in 95 cases out of 100 if it is taken no later than 24 hours after sexual intercourse. It should be noted, and this applies to all single-use birth control pills, since earlier use guarantees the greatest effectiveness.
Popular drugs
There are a large number of names of disposable birth control pills on the Russian market today. Based on their composition, they can be divided into two main groups: those containing mifepristone and those containing levonorgestrel. They act in different ways, but achieve the same goal - preventing pregnancy.
An example of a drug containing mifepristone is Ginepristone or Zhenale, as well as their analogues. A special feature of their use is a fast two hours before use and two hours after.
Levonogestrel is contained in Postrinor, Escapelle and other drugs. The Postinor package contains two tablets, which must be taken alternately with an interval of 12-16 hours. Escapelle has twice the dosage, so its use is limited to one dose.
How do disposable contraceptives work?
Single-use contraceptives for women inhibit ovulation, that is, the release of a mature egg from the ovary, and also prevent the reproductive cell from attaching to the wall of the uterus if it is fertilized. In this regard, after using the drug, a woman experiences menstrual-like bleeding within a few days - this should not be feared, this is an expected effect. Afterwards, the cycle is restored, but this may take some time, even several months, so it is highly not recommended to use disposable contraceptives more than twice a year.
It should be noted that these one-time contraceptives do not protect against sexually transmitted diseases, therefore, to avoid them, additional precautions must be taken.
Contraindications
All contraindications for use must be identified by a gynecologist, who must be consulted before taking the drug. Among the main prohibitions are pregnancy, age under 16, severe chronic diseases, etc.
Single-use contraceptives should not be used during breastfeeding. If such a need arises, feeding should be stopped for up to two weeks - the period depends on the type of drug. Contraindications to taking medications are also described in the instructions.
Side effects
In addition to the expected side effect, in the form of bleeding after using a single contraceptive, it is rare, but headache, nausea, and vomiting may occur. If vomiting occurs less than 3 hours after taking the tablet, you must take a new one.
There may also be pain in the lower abdomen and various allergic reactions. To reduce side effects, it is not recommended to resort to NSAIDs (non-steroidal anti-inflammatory drugs - ketorol, ibuprofen, etc.) for 8-12 hours after taking Ginepristone and its analogues.
Single-use contraceptive pills are a very effective contraceptive, but it should be remembered that they have a number of contraindications and undesirable effects, so you should consult a specialist before use.
There comes a time in every woman’s life when she thinks about protecting herself from unwanted pregnancy. Currently, pharmacy shelves offer a wide range of hormonal tablets that are highly effective. However, in the minds of Russian women the memory of their side effects associated with excess weight gain is still alive.
In this regard, many representatives of the fair half of humanity prefer to use contraceptives that do not contain hormones, despite their low effectiveness. What non-hormonal contraceptive pills do pharmacists offer women, and what new generation hormonal contraceptives do not have side effects on the female body?
Currently, women of reproductive age are increasingly resorting to chemical protection against pregnancy provided by non-hormonal pills. However, they justify their name only by their form, although they are not tablets as such. These drugs are not taken orally, like traditional hormonal contraceptives, but are inserted into the vagina.
These drugs contain spermicides - substances that destroy sperm within a short period of time, preventing them from penetrating the fallopian tube. Their active substance is benzalkonium chloride or nonoxynol.
How exactly do non-hormonal contraceptives work?
- Coming into contact with a sperm, spermicides destroy the flagellum, interfering with its further movement.
- When interacting with the head of the sperm, the membrane is damaged, which leads to its death.
- Causes thickening of mucus in the cervical canal of the cervix, which becomes a reliable obstacle to the advancement of weakened sperm.
Preparations based on spermicides are also available in other substances, which include the following forms:
- vaginal suppositories;
- vaginal creams and gels;
- tampons;
- diaphragms are soft, dome-shaped caps that cover the cervix.
Regardless of the form of release, the use of non-hormonal contraceptives allows you to create a reliable protective barrier against fungi and other diseases transmitted during unprotected sexual intercourse. This is facilitated by substances included in the preparations that have bactericidal and antimicrobial effects.
A distinctive feature of non-hormonal methods of contraception is that they must be used immediately before intimacy. At the same time, they retain their effectiveness for several hours.
Barrier contraception
The barrier method is a method in which a contraceptive physically blocks the access of sperm to the uterus. Fertilization does not occur because the sperm does not connect with the egg. Such contraception may include:
- Male condom;
- The female condom is less known and popular than the male condom. It allows you not only to avoid unwanted pregnancy, but also to prevent infection with many sexually transmitted diseases. The female condom is a small pouch with elastic rings that secure it into the vagina. The material from which it is made is polyurethane. The female condom, just like the male condom, can break. If this contraceptive is used correctly, its degree of protection is 90%;
- Uterine caps are also a little-known method of contraception in which a cap is placed on the cervix. They come in different shapes and sizes. You cannot protect yourself from sexually transmitted diseases using caps. The difficulty is that for installation you will have to resort to the help of a specialist. The negative aspects include the possible development of allergies due to the close contact of the mucous membrane and latex.
Degree of reliability
The effectiveness of certain contraceptive drugs is assessed using the Pearl scale. The study is conducted among 100 women using this particular method of contraception. This indicator is based on information about how many women among the subjects managed to become pregnant despite protection. And the lower the indicator, the higher the effectiveness of the group of drugs being evaluated.
In this case, this indicator is 8-36. This means that from 8 to 36 women out of 100 become pregnant even with protection from unwanted pregnancy.
When is the use of non-hormonal drugs indicated?
Despite the rather low efficiency, non-hormonal contraceptive pills have a number of advantages compared to hormonal methods of contraception.
- They can be used for various gynecological diseases, for example, uterine fibroids, as well as in the presence of hormone-dependent tumors.
- These drugs do not enter the stomach and are not absorbed into the blood, and therefore are not able to affect the liver, blood vessels and other body systems.
- They can be used for rare sexual contacts.
- They have a bactericidal and antimicrobial effect, which hormonal agents lack.
Non-hormonal contraception will provide reliable protection for women breastfeeding babies. They are used if women are contraindicated to use COCs or other types of contraceptives.
These drugs will help prevent pregnancy in women of Balzac age (40-45 years). At this age, the menstrual cycle is no longer regular. However, the possibility of pregnancy has not yet been ruled out.
Physiological. Natural methods of contraception
The method is based on knowledge of the most probable time of ovulation, and therefore the occurrence of pregnancy during the entire menstrual cycle. The menstrual cycle is the time from the first day of menstruation to the start of the next menstrual bleeding. The physiological method of contraception can only be used with a regular menstrual cycle.
Rules for calculating the fertile period (“dangerous days”):
- track the duration of 3-4 menstrual cycles;
- subtract 11 (for greater efficiency 8-10) days from the number of days in the longest menstrual cycle;
- 18 (to increase efficiency 19-21) days are subtracted from the number of days in the shortest cycle.
For example: long cycle 33 days – 11 days = 22; short cycle 28 days – 18 days = 10; Thus, from the 10th day from the start of menstruation to the 22nd day are the most “dangerous days” for conception, when you should avoid sexual relations or use barrier methods or interrupted sexual intercourse. The effectiveness of the method is 85-90%.
There are other physiological methods of contraception that calculate “safe days” by measuring rectal temperature; when assessing the condition of cervical mucus, when using ovulation tests.
So, when using ovulation tests, 4 days after receiving a positive test are considered “dangerous” for conception.
Disadvantages and contraindications
Such drugs are inserted into the vagina. Moreover, this must be done at least 10 minutes before the intended sexual contact. This means the absence of any unpredictability in sex and the need to discuss with your partner the time of each coitus. When using these drugs, it is not recommended to shower immediately before or after sexual intercourse. The time you need to wait is specified in the instructions for each drug.
Non-hormonal medications contain acid, which can irritate the mucous membrane, causing itching and burning in the vagina. However, these products are not recommended to be used regularly, since their long-term use can lead to disruption of the microflora in the vagina, causing the development of dysbacteriosis. There are no contraindications for the use of these contraceptives. The only exception is individual intolerance to their components.
Hormonal contraception
There are many methods of hormonal contraception. They are divided into two groups:
- Preparations containing an analogue of the hormone estrogen;
- Preparations that do not contain an analogue of the hormone estrogen.
The most common hormonal contraceptives for women:
- COCs are the most reliable contraceptive. Pregnancy becomes impossible due to suppression of ovulation. The most famous myth associated with the use of COCs is the story of excess weight. Fortunately, drugs in this category have not affected weight for a long time. Some girls have an increased appetite, however, this is rare. Many believe that the risk of thrombosis increases. This is also not true unless you have hereditary diseases associated with high blood pressure and blood clots;
- The vaginal ring works in the same way as COCs. The method of application differs. The ring is inserted into the vagina. Next, it releases the right amount of hormones that suppress ovulation. This method is not very convenient, since the ring may cause discomfort to the girl or even fall out;
- The hormonal patch is very convenient to use. You just need to stick it on the skin. Hormones enter the body through the blood;
The above methods belonged to the group of contraceptives containing estrogen.
Next we will talk about methods of contraception with drugs that do not contain estrogen.
- Mini-pills are pills that do not stop ovulation, but thicken the cervical fluid. This makes it difficult for sperm to enter the uterus. Mini-pills are a safer contraceptive, but less effective than estrogenic methods;
- Subdermal implants work in the same way as mini-pills. The implant is sutured under the skin and it releases the required dose of the progestogen hormone (progesterone) for more than one year;
- The intrauterine device immobilizes sperm. In addition to the fact that it mechanically prevents the embryo from attaching to the wall of the uterus, it also releases dosed hormones. The IUD is a common and reliable contraceptive. Installed for several years. You should visit a gynecologist once a year. The ability to bear children is restored immediately after removal. The disadvantage is the possibility of the device falling out during menstruation. Menstrual pain may get worse at first.
Review of popular contraceptives
All non-hormonal tablets are divided into groups based on which of the active ingredients is included in their composition.
Names of contraceptives based on benzalkonium chloride:
- Pharmatex is most popular due to its low cost combined with high efficiency. It is available in the form of vaginal tablets, cream, suppositories and even tampons. Regardless of the dosage form, the drug begins to act 10 minutes after ingestion, without losing its properties for 3-4 hours.
- Ginotex are ring-shaped tablets. It is recommended to administer them no later than 5 minutes before contact. The effect of the tablet lasts for 4 hours.
- Genotex are tablets whose action is identical to previous drugs.
- Erotex is a non-hormonal contraceptive suppository, the effect of which begins after 10 minutes and ends after 3 hours.
- Contratex are candles that begin to perform their functions after 10 minutes and end after 4 hours.
Names of contraceptives based on nonoxenol:
- Patentex Oval are highly effective suppositories that are inserted into the vagina 10 minutes before expected intimacy. They retain their effect for up to 10 hours.
- Nonoxenol is a contraceptive suppository that has the same characteristics as the previous drug.
It should be remembered that before each subsequent sexual intercourse, non-hormonal contraceptives must be reintroduced.
Women's doctor column: LARC - contraception for the lazy
When I was young and beautiful, I was extremely concerned with the question: “How can I protect myself from pregnancy in such a way that it is reliable, safe, and dust-free.” Alas, there is too little harmony in the world. The ideal contraceptive has not yet been invented. Either it’s not reliable, or it’s difficult, or it’s fraught. Everything here is like in life: there are many men, there is no one to choose. It’s the same with contraception - there is a lot of choice, but nothing is nice.
Condoms
- a wonderful thing, but they have several serious drawbacks. Firstly, they end. Secondly, they disrupt the romantic flow of foreplay (at least, it seemed so to me before). I immediately rejected all kinds of cervical caps and diaphragms, due to their low effectiveness and terrible confusion.
Spermicides
- chemical substances that mercilessly kill sperm - have to be injected into the vagina before sexual contact and then: “Wait, dear, the pill hasn’t foamed yet.” Even the non-foaming Pharmatex aroused weak enthusiasm in me.
Birth control pills
– the crown of human thought – you need to drink every day. I’ll be honest, in my youth I only lasted three months. The daily intake turned out to be completely beyond my capabilities. I endlessly missed pills, forgot to buy a pack on time, which brought my body to a state of complete menstrual chaos.
Many years later, in some Western manual on contraception, I found a separate contraindication: “Taking COCs is not recommended for women who are unable to take the drug regularly.” Perhaps the authors had some kind of cognitive deviation in mind, but I smiled at my reflection: “Yolki, this is about me!”
Intrauterine devices required a mandatory visit to the gynecologist. In addition, in those ancient times, spirals were placed only and exclusively on women giving birth. In principle, this is a completely fair approach. IUDs in young women are fraught with the development of inflammatory diseases of the pelvic organs with the further prospect of infertility. Youth is flighty, partners change, infections remain. Even today, it is possible to offer an IUD to a nulliparous patient with many, many reservations.
I even seriously looked at the option with Depo-Provera. This is a progestin-only drug that was administered intramuscularly every three months. It was distinguished by excellent contraceptive reliability, but had a number of “buts” - from very noticeable weight gain to menstrual irregularities in a wide range.
In today's contraceptive market, it is simply paradise for the lazy. In the English literature, long-acting reversible contraceptives are called Long-Acting Reversible Contraception (LARC).
The first LARC - a “lazy” drug - was the Evra contraceptive patches.
from . "Evra" is a TTS (transdermal therapeutic system). Each patch releases 150 mcg of norelgestromin and 20 mcg of ethinyl estradiol per day. Like any other hormonal contraceptive, the use of Evra begins on the 1st day of menstruation. The patch is applied to the skin of the abdomen, or buttocks, or wherever you like. The main thing is that there is less hair in this area and that tight clothing does not fit tightly. We wear the patch for exactly 7 days, on the eighth day we throw it away and stick a new one in a new place. Then everything is simple: three weeks with a patch, a week without a patch.
The next great idea was the NuvaRing vaginal rings.
NuvaRing should not be confused with old cervical caps and diaphragms. This is a complete hormonal contraception. Each day, the ring releases 15 micrograms of ethinyl estradiol and etonogestrel (a derivative of 19-nortestosterone) into the vagina. The ring is inserted into the vagina on the 1st day of menstruation. It's simple: 21 days with a ring, 7 days without a ring, 21 days with a ring, 7 days without a ring. Naturally, a new cycle means a new ring.
If a monthly trip to the pharmacy for a new ring or patches seems like a heavy burden to you, you should take a serious look at contraceptive implants.
On the Russian market these are Implanon and Implanon NKST.
Both implants are a flexible rod the size of a matchstick that is inserted under the skin in the shoulder area. The implants contain exactly the same progestogen as the NuvaRing ring - etonogestrel in the amount of 68 mg. There is no estrogen component, but this can be considered both an advantage and a disadvantage - to each his own.
60–70 mcg of etonogestrel enters the systemic circulation daily (the release rate decreases to 25–30 mcg/day after 3 years). This amount is sufficient to stably suppress ovulation in 99% of cycles. If the implant is inserted in the first days of menstruation, the contraceptive effect occurs immediately and lasts three years.
It is important to understand that no one was ordered by the court to wear Implanon for all three years - it can be removed at any time at the woman’s request. If three years have passed and contraception is still needed, removal of the old implant and insertion of a new implant can be done on the same day.
Clear advantages of LARC:
- Minimal chances of messing up. The use does not depend on sexual intercourse, women’s motivation and compliance with the dosage regimen.
- Women like it. People refuse to use LARS methods much less often than they stop drinking pills or using condoms, returning to the good old (crossed out) interrupted sexual intercourse.
- These methods are highly effective. Much more effective than PPA, condoms, spermicides.
- There is no need to frequently visit the pharmacy to replenish supplies.
- The effect is reversible, the ability to conceive is quickly restored after removal.
Of course, everything in the world has its price. Some people are annoyed by the “lumps of dirt” that accumulate around the contraceptive patch. Some people don’t like more active mucous discharge when using the ring. For some, Implanon causes fairly intense acyclic bleeding that cannot be corrected.
However, the advantages of LARS methods are so undeniable that most experts consider this area a priority. True, sometimes it seems to me that any idea can be taken to the point of absurdity. By 2018, we expect a contraceptive chip to enter the market. This device will be injected under the skin and is valid for 16 years. Throughout this time, the chip will release 30 mcg of levonorgestrel per day, providing reliable contraception.
Levonorgestrel is well known to us and has been well studied. This gestagen was part of the 2nd generation COC, provided reliable control of the cycle, but had a small “but” - androgenic activity. In life, this could manifest itself as an increase/appearance of acne and seborrhea. It was in order to get rid of these undesirable effects that pharmaceutical companies had to make a qualitative leap and come up with the next generation of gestagens - antiandrogenic or neutral. On the other hand, levonorgestrel has been successfully used for a long time in the hormone-releasing Mirena IUD; acne complaints are extremely rare. This is probably due to the fact that Mirena is located in the uterine cavity, and the entry of the drug into the systemic circulation is extremely small. Interestingly, they plan to add a control panel to the chips, with which the patient can turn off the chip and become pregnant.
Life will show how popular this miracle of hostile technology will be. In the meantime, don’t be lazy to use contraception “for the lazy.” Have safe sexual intercourse!
Oksana Bogdashevskaya
Photo 1-3.5 - thinkstockphotos.com, 4- implanonimplant.com
Products by topic: condoms, Pharmatex, contraceptive spiral, Implanon, levonorgestrel
Features of choice
How to determine which non-hormonal birth control pills are better? Considering their low cost, price is not a decisive factor when choosing. However, as the experience of women who have already experienced all existing forms of non-hormonal contraceptives shows, suppositories are suitable for women suffering from vaginal dryness. When using them, there is no need to use lubricants.
There are also unpleasant phenomena associated with the fact that when the tablet dissolves, a characteristic hissing sound is heard, and foam is released from the vagina. In addition, even using the best medications, it is possible that irritation, itching and burning may occur not only in women, but also in their partners. Each woman’s body reacts differently to certain substances. Therefore, determining which non-hormonal contraceptives are better will have to be done through trial and error.
Hormonal contraceptives
Every year, an increasing number of women prefer the use of hormonal oral contraceptives, which is explained by their high efficiency. They not only reliably protect against unwanted pregnancy, but also have a beneficial effect on the female reproductive system. Among other contraceptives, new generation contraceptives took pride of place on the pedestal.
All modern hormonal preparations for oral administration are divided into four types, based on the amount of hormones they contain.
- Microdosed contraceptives contain a minimal amount of hormones, which practically eliminates their side effects. The active ingredient in such drugs is ethinyl estradiol, a synthetic analogue of estradiol. Because of this, they are used to treat acne and painful menstruation caused by hormonal imbalances. Such drugs can be used both by very young nulliparous girls and by mature women who have never taken hormonal contraceptives.
- Low-dose contraceptives also contain synthetic estradiol in combination with progesterone. Such drugs will be an ideal means of preventing unwanted pregnancy for young women who have already given birth. In addition to the contraceptive effect, these medications help eliminate manifestations caused by excessive levels of male sex hormones in the body. These include hair growth in inappropriate places, acne and male pattern baldness.
- Medium-dose contraceptives contain synthetic analogues of estradiol with progesterone. They are intended for mature women who have given birth. Like the previous option, these drugs are designed to normalize hormonal levels. However, they cannot be used during breastfeeding.
- High-dose contraceptives contain increased doses of estradiol and progesterone. Such drugs are most often used for medicinal purposes to restore hormonal levels. To protect against unwanted pregnancy, new generation birth control pills are recommended for women who have given birth after 35 years of age.
Female surgical contraception
We are talking about sterilization - an irreversible process that is considered the most effective for preventing unwanted pregnancy. Indications for sterilization of a woman are only the desire to stop the possibility of conception. But this issue should be approached extremely carefully - the process is irreversible, although there are expensive microsurgical operations that can “turn back time.” Surgical contraception is often used for medical reasons - for example, a woman has severe malformations of the cardiovascular, respiratory, urinary systems, blood diseases, or malignant neoplasms. Contraindications to sterilization are:
- acute inflammatory diseases of the pelvic organs;
- infection of generalized or focal localization;
- benign tumors developing in the pelvis;
- severe cachexia;
- diabetes mellitus/diabetes insipidus;
- adhesive disease of the pelvic organs and/or abdominal cavity;
- umbilical hernia – applies only to surgical contraception using the laparoscopic method.
Please note: there is still debate about sterilization of women with diagnosed mental disorders and mental retardation - these pathologies are not a medical indicator for surgical contraception.
Laparoscopic tubal ligation
Now this is the most popular method of surgical contraception - the method has many advantages. For example, after such a surgical intervention there is no scar left on the skin, the rehabilitation period is very short, and patients tolerate such an intervention well. Please note: laparoscopic tubal ligation on an outpatient basis is not excluded - the woman is given local anesthesia, and 2 hours after completion of the procedure and in the absence of any visible changes in well-being for the worse, the patient can go home.
Minilaparotomy
A miniature incision is made in the anterior abdominal wall - the size does not exceed 6 cm. The advantages of this method of surgical contraception are that there is no need to use expensive equipment and quick rehabilitation.
Sterilization with colpotomy access
The rectal uterine space is opened with scissors and the fallopian tube is removed into the resulting wound until its fimbria appears. The suture is placed in the middle of the fallopian tube, but somewhat closer to the fimbria. Then they tie the tube with a thread and pull it closer to the surgeon, then the tube is crushed and ligated. The same algorithm of actions is used for the second fallopian tube. Please note: the ends of all suture threads are cut only after the surgeon has finished working on the two fallopian tubes. The incision is closed with a mattress suture. Advantages of sterilization with colpotomy access:
- can be performed in any gynecological hospital;
- there are no cosmetic defects on the anterior abdominal wall;
- there is no need to use expensive equipment and specific tools;
- the pursued goal (sterilization) is achieved immediately after surgery.
Very often, a sterilization operation is performed during a cesarean section - there is no additional stress on the body, the woman’s well-being does not change, the periods of lactation and recovery after childbirth pass without changes, and the hormonal levels do not change. Timing for surgical contraception:
- in the second phase of the menstrual cycle - delayed sterilization;
- 6 weeks after birth naturally;
- immediately after an artificial termination of pregnancy, but only if the abortion was without complications.
It is strictly contraindicated to carry out sterilization after childbirth if an acute infectious disease was diagnosed during childbirth or during pregnancy, if the anhydrous period of labor exceeded 24 hours. Possible complications in the postoperative period:
- bleeding;
- intestinal damage;
- postoperative infection.
These complications are rare events, but a woman who agrees to surgical contraception should be aware of them. Please note: doctors warn that in the first 10 years after sterilization surgery, the probability of pregnancy remains within 2%. Female contraception – a wide choice, wide possibilities. It is necessary not only to independently decide on the choice of means of protection against unwanted pregnancy, but also to obtain competent advice from a gynecologist.
Tsygankova Yana Aleksandrovna, medical observer, therapist of the highest qualification category.
21, total, today
( 42 votes, average: 4.64 out of 5)
Bacterial vaginosis - all about the infectious disease
Hydrosalpinx: symptoms and treatment
Related Posts
Emergency contraception
These drugs are used in emergency situations and help prevent pregnancy after unprotected sexual intercourse. They are recommended for use in the following cases:
- in case of violent acts or if the condom is damaged;
- with infrequent sexual intercourse.
Contraindications to their use include bleeding disorders, heart and vascular diseases, liver and kidney failure, malignant tumors and smoking.
Features of taking pills
How long can you take oral contraceptives, and do you need to change them? They must be taken daily and preferably at the same time. It is recommended to start taking them on the first day of menstruation. These drugs are intended for long-term use. However, women taking hormonal contraceptives should visit their gynecologist annually. If there are no contraindications, you can continue taking contraceptives.
With long-term use of COCs, menstruation may stop altogether, and this is not a pathology. However, if a woman forgot to take her birth control pill and the last day of her period is long past, this may be a sign of pregnancy. After discontinuation of contraceptives, the menstrual cycle is completely restored within 1-2 months. In this case, pregnancy can occur immediately or after a short period of time. You can take birth control pills for several years. If they do not cause any side effects in a woman, they should not be changed. Otherwise, the body will experience stress.
The safest contraceptive method for women
To choose the safest method for women, it is important to undergo an examination by a gynecologist; the doctor takes into account the risk factors and characteristics of each period of life:
- teenagers - suppositories, condoms, tablets with hormones no earlier than 2 years after a stable cycle, physical maturity (height from 1.60 m), absence of excess body weight and heart disease, blood vessels, and when changing partners, hormonal drugs and a condom are needed ;
- young women who have not given birth and have not become pregnant - long-term tablets, and 3 months before the planned conception - rhythmic, suppositories, condoms;
- breastfeeding - spiral, mini-pill, condom, injection;
- after childbirth - tablets, spirals, injections, capsule filing, suppositories and condoms;
- the family does not plan to have children, the period before menopause – sterilization, implant, injections, IUD, pills;
- menopause (the ability to form single eggs occurs up to 5 years after the cessation of menstruation) - condom, suppositories, cream, vaginal tablets.
Watch this video about the most effective methods of contraception:
Natural methods of contraception
Methods of preventing unwanted pregnancy without hormones have been used for a long time. Despite the wide range of modern contraceptives offered by pharmacists, they still remain relevant today.
One of them is based on counting the days of ovulation. On average, the duration of the menstrual cycle is from 28 to 30 days. In its first half, the follicle matures. And ovulation occurs in the second half of the cycle. The ability to fertilize a mature egg remains for 2-3 days. In this case, sperm can take a wait-and-see position for 4 days. Therefore, special care only needs to be taken for about a week in the middle of the cycle.
In some cases, the days of ovulation can be determined by measuring basal temperature, which rises on the most dangerous days. However, the reliability of calculations and temperature measurements in the rectum cannot guarantee full protection.
Some couples practice coitus interruptus. However, even in this case, pregnancy cannot be ruled out, since a small amount of sperm may be contained in the lubricant secreted by the partner’s penis. In this case, the likelihood of pregnancy increases depending on how many sexual acts have been performed.
What is contraception
Contraception is a method of preventing the fusion of sperm with an egg and its fertilization, carried out through various contraceptives. Some of them can be used to protect against sexually transmitted infections, as well as to treat diseases of the female reproductive system and stabilize the menstrual cycle. Contraceptives are actively used for rational family planning: with their help, men and women have the opportunity to make their own decisions about the time of having offspring.
Modern methods of contraception are very diverse
All methods of preventing unwanted pregnancy have different effectiveness. To evaluate it, a percentage or Pearl index is used. It represents the number of unwanted conceptions per 100 girls and women using this method for contraception. The lower the Pearl index, the higher the contraceptive effect the drug has. An increase in this indicator may be affected by:
- improper use of a method of protection against unwanted pregnancy;
- switching from one method of contraception to another without following the doctor’s recommendations;
- individual characteristics of the body of a woman and a man;
- the presence of acute or chronic diseases that affect the chosen method of contraception.
In European countries and America, the most popular means of contraception are hormonal contraceptives. In Russia and the Baltic countries, condoms and coitus interruptus are widely used.