Gastric bulbitis is a disease associated with inflammation of the walls of the duodenum. Microbes, harmful bacteria that enter the human body, have a negative effect on the intestinal tract and digestive system. Inflammation or damage to the mucous membrane is directly related to disease of the duodenum, which is a form of duodenitis.
Clinical picture
Patients rarely know what bulbitis is, associating it with stomach pain. The term duodenitis is more common. Inflammation of the mucous membrane of the bulb – bulbus – under the influence of aggressive factors. There are two types of pathology, according to ICD 10:
- catarrhal – mild superficial inflammation;
- ulcerative – damage to the deep layers of cells, including muscle cells.
Damage to the mucous membrane is caused by disruptions in digestion. In the onion, the acidic contents of the stomach are neutralized by pancreatic juices. When the composition of digestive juice changes, spasm of the sphincter of Oddi or narrowing of the ducts, the acid-base balance - the pH of the ampoule - is disrupted. As a result, hydrochloric acid damages the mucous membrane, creating the preconditions for the proliferation of H.pilory and inflammatory processes.
Main types of pathology
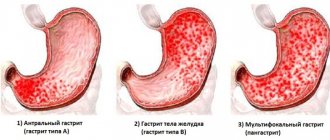
The Sydney classification, in force since 1991, distinguishes several types of duodenitis according to the depth and severity of damage to the mucous membrane:
- focal – single localized foci are identified. Its variety is erythematous bulbitis with oval hyperemic areas as a result of chemical exposure to substances and bacterial activity;
- catarrhal – a chronic course with exacerbations, which are manifested by swelling of the mucous membrane, redness, increased mucus production;
- superficial – manifested by pain in the navel after eating, belching, weakness, lack of feeling of satiety;
- atrophic - appears with a long course of catarrhal inflammation, which leads to thinning of the mucous membrane and decreased function of the glands. The subatrophic process is the initial stage of atrophy;
- diffuse – atrophic form, leading to cell death, fibrosis and increased risk of cancer.
Endoscopic examination allows us to identify the following forms of the disease depending on changes in the mucous membrane:
- erosive bulbitis - manifested by small ulcers on the mucous membrane, hyperemia. Bulbitis with erosions affects the general condition of the patient, causing weakness, fever, vomiting, headaches;
- hyperplastic bulbitis is the proliferation of epithelial cells, coarsening of the mucosa during prolonged inflammation. There are two types of pathology: granular bulbitis with point changes and polypous - with the formation of polyps;
- hemorrhagic – combined with vascular damage, manifested by bleeding local wounds as a result of deep damage to the mucosa;
- follicular - manifests itself in addition to redness of the mucous membrane, enlargement of the lymph nodes and organ (bulbostasis), pain when palpated. Appears against the background of parasitic infections, exposure to chemical factors;
- hypertrophic is the growth of the mucous membrane due to the formation of adenomas (benign tumors) and cysts.
Signs of bulbitis depend on the clinical course. Inflammation may resemble the picture of a peptic ulcer, gastritis, cholecystitis or pancreatitis, and may also occur in a neurovegetative or latent form without manifestations. The pathology can be mixed - for example, pylorobulbitis, in which the pylorus and duodenal bulb become inflamed.
Main stages of pathology
The inflammatory process goes through several stages, determined by cellular changes in the walls of the bulb:
- bulbitis of the 1st degree of activity - the mucous membrane is unchanged, lymphocytes and blood plasma cells are detected in the tissue;
- moderately pronounced bulbitis - occurs with a change in the function and number of villi on the mucous membrane;
- severe or stage 3 is accompanied by severe damage to the villous epithelium, multiple infiltrates and erosions.
Moderate bulbitis is usually manifested by pain of uncertain localization, heaviness in the abdomen, discomfort that intensifies during stress, and spasms in the navel area.
Classification
The disease has some differences in the location of the area with inflammation; therefore, bulbitis is divided into focal - with damage to a specific focus - and total, when complete damage occurs. Bulbitis is also distinguished by other characteristic features, since the inflammatory process can spread to different depths of the mucosa, have a different extent and have other distinctive features. In gastroenterology, the disease is divided into several types:
- Acute – characterized by the development of sharp pain in the stomach, often in the hypochondrium on the right side. It is often accompanied by attacks of nausea with vomiting, in some cases with bile.
- Catarrhal type or chronic, accompanied by pain in the solar plexus.
- Superficial type, considered the easiest. A characteristic feature is hunger pain, bitterness in the mouth and a feeling of discomfort after eating.
- An erosive appearance, with a gradual increase in pathological symptoms in the form of disturbing night pain, heartburn, bloating, stool instability with constipation and diarrhea.
This inflammatory process in the duodenum can be the result of chronic gastritis and duodenitis. As an independent disease, duodenitis is observed extremely rarely.
Currently reading: What is stomach bulbitis - symptoms, diet and how to treat
Causes of the disease
Damage to the mucous bulb can be primary or secondary:
- Primary inflammations are caused by malnutrition (nutritional), exposure to bacteria, viruses, fungi or parasites, allergic and autoimmune reactions, chemical agents, neuroendocrine disorders.
- Secondary inflammation appears against the background of gastritis, cholecystitis and pancreatitis, duodenal ulcers, circulatory disorders, heart and vascular diseases, and immunodeficiency states.
Bulbitis develops for reasons of heredity or congenital defects in organ development.
A predisposition to inflammation occurs when the function of the duodenum is impaired, in which acidic food chyme is processed with bicarbonates from the pancreas. Pathology is possible with dyskinesia, disorders of the nervous regulation of sphincters between parts of the gastrointestinal tract, anatomical features of the intestine, which make it difficult for juices or food to enter.
Causes of bulbitis additionally include:
- food poisoning;
- alcohol abuse;
- long-term medication use;
- chronic stress, spasm of the diaphragm, disorders of the nervous regulation of gland function;
- smoking;
- helminths, opisthorchiasis, lamblia, shigella, salmonella;
- Botkin's disease;
- inflammatory bowel processes.
Spicy, fatty foods, when combined with other physiological factors, can provoke damage to the mucous membrane.
What is follicular bulbitis?
To understand the causes of follicular bulbitis, you need to know how the bulb (translated from Latin as bulb) - the initial part of the small intestine - is structured and how it functions. Anatomically, the bulbus - the initial section of the duodenum - has the appearance of a short swollen cylinder, truly reminiscent of an onion in shape.
The structure of the mucous membrane of the duodenum is characterized by special resistance to chemical irritants - it is an intermediate option, something between the structure of the gastric and intestinal mucosa, which have fundamental differences in function.
A feature of the structure of the bulb is the narrowing of its lumen at some distance from the entrance, straightening of the longitudinal folds when filled, and greater mobility (it is practically not secured by the ligamentous apparatus). This causes some temporary delay of part of the food bolus coming from the stomach.
The submucosa of the bulbus, like the entire duodenum (duodenum), is penetrated by numerous duodenal glands that produce alkaline mucus to neutralize gastric juice and protect the mucous membrane of the duodenum, and lymphatic capillaries. The excretory ability of duodenum has been poorly studied, since the secretion is difficult to isolate in its pure form, but its purpose is the chemical activation of digestive enzymes entering its lumen.
On one square millimeter of the surface of the mucous membrane of the bulbus there can be up to 100 stomata-exits of glandular elements, the so-called crypts - simply put, ducts through which intestinal secretions and mucus are released into the intestinal lumen, acting as a protective factor. A special structure of the intestinal wall is formed around each of the ducts, which, against the background of inflammation and swelling of the tissue, can become denser, blocking it. The mucous membrane is also densely intertwined with small nerve fibers and blood vessels.
A follicle is a formation in the form of a round, oval or pear-shaped vesicle with liquid contents. Its formation is caused by blockage of the gland - then the follicle is filled with accumulated alkaline secretion that does not receive release, or lymph, which can be supplemented with exudate - liquid secreted by inflamed tissues.
Symptoms of bulbitis
Depending on the severity of the inflammatory process, acute and chronic bulbitis are distinguished. Symptoms depend on the course of the pathology and the degree of damage to the mucous membrane. More often, inflammation is detected during endoscopic examinations for constipation, flatulence, and weakness.
Acute bulbitis is manifested by aching or paroxysmal pain in the epigastrium, directly under the xiphoid process. They can radiate to the right side or to the navel area.
Symptoms of bulbitis during an exacerbation are varied:
- nausea and vomiting;
- sweating and weakness;
- poor appetite;
- pain on palpation of the stomach.
Elevated temperature during pathology indicates an acute inflammatory process. The chronic course of the disease is more difficult to recognize, since it is often impossible to clarify when and what hurts.
The clinical variant of duodenitis determines the nature of the pain: at night, on an empty stomach, early or late after eating. Localization can be clear or encircling with irradiation towards the pancreas, navel or left hypochondrium.
Additional manifestations differ in neuroendocrine variants of bulbitis; symptoms and treatment depend on the activation of the parasympathetic or sympathetic nervous system. Against the background of stress, gastric motility and sphincter activity are inhibited, and preconditions for inflammation arise. Violation of nervous regulation is manifested by weakness, increased heart rate, shortness of breath, tremor and sweating.
Chronic inflammation manifests itself:
- diarrhea or constipation;
- belching;
- abdominal pain when pressed;
- increased gas formation;
- feeling of heaviness in the stomach after eating;
- paroxysmal pain;
- decrease in body weight.
Severe vomiting and pain appear against the background of toxic infections caused by intensive proliferation of bacteria, with severe chemical burns of the stomach and bulb.
A common problem is bulbostasis in a child. In children, enlargement of the bulb is associated with spasm of the bulboduodenal sphincter. In this place of the intestine there is circular muscle, which depends on irritation of the vagus nerve. The nervous system activates its work after severe stress.
Treatment options
To eliminate symptomatic signs, certain treatment for duodenal bulbitis may be prescribed, depending on the severity of the disease. There are 4 traditional methods of therapy against inflammation of the mucous membrane:
- use of medications;
- proper lifestyle, diet;
- traditional medicine;
- surgical intervention.
Regardless of the prescribed treatment method for gastric bulbitis, it is recommended to monitor your diet, exercise, avoid stressful situations, and avoid consuming alcohol and tobacco products.
Medicines
Bulbitis should be treated by taking medications:
- antacids in acute form;
- painkillers, antispasmodics;
- antibiotics for chronic, catarrhal forms;
- healing agents for superficial, erosive, ulcerative forms;
- blockers to normalize hydrochloric acid levels;
- histamines;
- chonolitic drugs;
- hormonal drugs (if signs of Crohn's disease are detected);
- complex preparations to improve the functioning of the digestive system;
- vitamin complex;
- saline solutions.
Medicines are aimed not only at relieving the symptoms of the disease, but also to cure bulbitis.
Healthy eating
The diet is prescribed as the main therapy for minor damage to the mucous membrane, for example, moderate bulbitis, and also as an additional measure to the treatment regimen for other forms of the disease. With proper nutrition, it is prohibited to eat fatty, salty, spicy, smoked foods, coffee, canned foods and include in the menu:
- boiled, steamed food;
- vegetable broth;
- fruits vegetables;
- lean meat, fish;
- croup;
- compotes.
For bulbitis and gastritis, the diet provides for split meals - 5-6 times a day. It is necessary to reduce the content of table salt in dishes. Eating with bulbitis means eating liquid, crushed, ground food; large pieces should be avoided. After a week, you can eat fermented milk products.
Folk remedies
Treatment of bulbitis with folk remedies involves the use of medicinal plants as the main ingredients: chamomile, St. John's wort, calendula and others. Herbs are used to make infusions, decoctions, and teas that have antimicrobial and anti-inflammatory effects.
There is a simple recipe for treating bulbitis with folk remedies: pour 50 grams of herbal plant with boiling water and leave for several hours. Honey can be used as an additional ingredient. To prevent treatment with folk remedies, you should drink carrot juice or natural fresh juice.
Surgical intervention
The operation is prescribed for severe duodenal bulbitis with complications, as well as severe internal bleeding, and an ulcer of the duodenal bulb.
Determining the symptoms and treatment of gastric bulbitis is the main thing to eliminate the inflammatory process. To prevent pain and other unpleasant sensations, you should adhere to proper nutrition. Diet for bulbitis is a necessary treatment measure.
Bulbitis of the duodenum and diseases of the digestive system are more correctly treated with proven means. Inflammation of the duodenal lining can be eliminated with drugs and folk remedies.
We recommend: What herbs can you drink for gastritis?
Diagnostics
A comprehensive examination is required to make a diagnosis. The patient is asked about symptoms, dietary habits and lifestyle, and a chart of previous complaints is studied. An examination is carried out, the abdominal cavity is palpated. The doctor assesses tension in the abdominal muscles and the presence of pain.
X-rays of the duodenum help identify structural abnormalities, spasms and tumors.
Fibrogastroduodenoscopy (FGDS) determines changes in the appearance of the mucous membrane: swelling, redness, severity of the capillary network and the presence of defects. It is possible to prescribe an ultrasound examination and fibroesophagoduodenoscopy.
Laboratory diagnostics are carried out:
- The level of pH - acidity is measured, which allows us to draw a conclusion about the type of gastritis.
- The contents of the duodenum are analyzed for the presence of infection if a bacterial or parasitic lesion is suspected.
- A blood and stool test reveals the inflammatory process, the causative agent of intestinal infection.
If necessary, enzyme immunoassay and PCR diagnostics for Helicobacter pylori are performed. Identified polyps are subjected to histological examination.
How to treat bulbitis
Treatment of bulbitis with medication is aimed at eliminating the cause of the pathology and reducing symptoms:
- Antibiotics are used when H.pilori is detected against the background of an inflammatory process.
- Bismuth tripotassium citrate helps against Helicobacter, and also reduces the activity of pepsin, heals ulcerative lesions, increases the production of mucus and bicarbonates, leveling the pH.
- Proton pump inhibitors are prescribed for hyperacidity and heartburn.
- M-anticholinergics and H2-histamine blockers help reduce the production of hydrochloric acid and relieve spasm of the sphincter muscles.
- If it is psychogenic in nature, treatment of bulbitis includes sedatives.
Herbal preparations are actively used:
- Sea buckthorn and rosehip oils help heal the mucous membrane;
- mucus production is enhanced with licorice root extract.
If hemorrhagic bulbitis is accompanied by intense hemorrhages, vessel ligation can be performed during gastroduodenoscopy. Surgical treatment methods are needed for debilitating ulcerative bulbitis, when it is not possible to reduce the acidity of the stomach. Vagotomy involves cutting the nerve that regulates the production of hydrochloric acid.
How to treat bulbitis at home?
As prescribed by the doctor, drink Borjomi mineral water, carrot juice, teas based on chamomile, St. John's wort. Home methods include jelly, liquid porridge, and rely on nutrition.
It often happens that in case of acute duodenitis they are admitted to the hospital to detoxify the body after consuming alcohol or smoked foods. Sometimes gastric lavage with the introduction of saline is required. In adults with duodenitis against the background of pancreatitis, Delargin is administered intravenously to suppress secretory function.
Bulbitis can also be treated with physiotherapy, which relieves inflammation using electrophoresis with novocaine, and spasm with papaverine.
Diet
Therapeutic nutrition reduces inflammation and promotes healing of the mucous membrane. In the hospital, dietary table No. 1 is prescribed, as for peptic ulcers.
The patient is recommended to steam dishes, make pureed soups and purees. Rough food will injure the mucous membrane. Eating 5-6 times a day eliminates hunger pains and regulates the production of hydrochloric acid and mucus.
It is recommended to limit fatty, spicy, canned foods. You should completely avoid soda and alcohol. The diet for bulbitis allows fermented milk products, cereals, jelly, lean meat or poultry, non-acidic fruits and vegetables.
Prevention
Prevention of follicular bulbitis consists of following the recommendations below, which help prevent the disease:
- Maintaining proper nutrition with a balanced diet (the predominance of simple and natural food without artificial additives and substitutes);
- Quitting bad habits (alcohol, cigarettes);
- Timely treatment of gastrointestinal diseases (stomach ulcer, chronic pancreatitis, cholecystitis);
- Taking preventive courses and following diet No. 1 to eliminate possible relapses of bulbitis;
- Exclusion of long-term use of drugs with strong effects (non-steroidal anti-inflammatory drugs, antibiotics).
The prognosis for the treatment of follicular bulbitis is generally positive, since with timely detection and treatment of the disease, a long period of remission and the absence of unpleasant symptoms can be achieved.