Peptic ulcer of the stomach and duodenum occurs due to destructive changes in the mucous layer of these organs, which are in direct contact with food, and which are the main protective barrier against the aggressive, strongly acidic environment of the contents. When the mucous layer is destroyed, its protective function decreases, which over time leads to an increase and deepening of the pathological focus, up to the complete destruction of the stomach wall. That is, a through hole is formed, or a perforated ulcer.
- Anatomical and physiological features of the stomach
- Causes of ulcer development
- Symptoms and emergency care
- Clarifying diagnostics
- Types of operations for perforated ulcers
- Consequences
What is a perforated gastric ulcer?
A perforated stomach ulcer belongs to the category of severe, life-threatening diseases.
A perforation occurs in the wall of the organ and the contents flow directly into the abdominal cavity. As a result, peritonitis develops, which requires immediate surgical intervention. Currently, in Russia, perforated ulcers have been diagnosed in almost 3 million people. Relapses occur in 6% of patients. Men are more often affected by the disease. The hormone estrogen produced by the female body has a restraining effect on the activity of the secretory glands of the gastric mucosa.
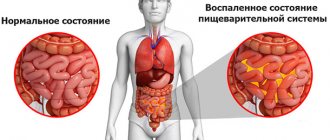
The disease is characterized by a chronic course with periodic relapses in the autumn-spring period. A gastric ulcer is a defect of the epithelium (sometimes with damage to the submucosal layer), which is characterized by changes in tissue trophism. The process occurs against the background of the aggressive effects of pepsin, bile and hydrochloric acid.
Classification
Making a diagnosis includes a number of criteria that allow you to correctly define the disease. Experts use an expanded classification, which is reflected in the table.
Table 1. Classification of gastric ulcer
arising for other reasons
average – 5-10 mm;
large – up to 30 mm;
gigantic – more than 30 mm – in the stomach,
more than 20 mm – in the duodenum
with atypical manifestations (with atypical pain syndrome, without pain with other signs, asymptomatic)
with a low level of secretion;
with normal secretion levels
red scar stage;
white scar stage
with rare exacerbations once every 2-3 years;
Sometimes there are mucosal defects that are located opposite each other. Such ulcers are called kissing ulcers. In most cases, they form in the area of the duodenal bulb.
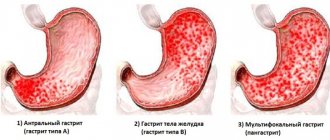
Localization
Ulcerative defects caused by the influence of secretory factors are localized in the upper parts of the digestive tract. In most cases, they are located in the stomach, less often in the duodenum. Therefore, the lesions are divided topographically according to the place of origin.
Table 2. Classification by localization
Etiological and provoking factors play a role in the formation of the pathological process. Currently, the proven cause of gastric ulcer is infection with the bacterium Helicobacter pylori.
It is detected in 80% of cases of the disease. The development mechanism includes 3 stages:
- The pathogen secretes enzymes. One of them is urease, which breaks down urea to form ammonia, which leads to excess secretion of hydrochloric acid in response to increased mucus pH.
- Helicobacter cytotoxin causes a local inflammatory reaction and death of epithelial cells.
- In response to the introduction of a bacterial agent, glandular cells produce pepsinogen and gastrin. An increase in their concentration disrupts the acidity of the stomach and contributes to the development of chronic inflammation.
Of secondary importance are provoking factors, which together increase the risk of the disease.
Other causes of stomach ulcers:
- A burdened family history – cases of pathology in close relatives.
- Psycho-emotional lability.
- Stresses that cause ischemia of the gastric mucosa.
- Poor quality nutrition, irregular eating habits.
- Alcohol abuse, smoking.
- The presence of genetic markers - congenital deficiency of alpha1-antitrypsin, p2-macroglobulin, fucoglycoproteins, glycosamines, increased number of parietal cells, low ability to produce blood aglutinogens AB into the stomach.
- Blood type 0 (I) positive.
- Concomitant intercurrent chronic diseases - pancreatitis, hepatitis, liver cirrhosis, cardiovascular pathology, respiratory diseases, diabetes mellitus, hyperparathyroidism, Zollinger-Ellison syndrome.
- Long-term use of certain medications - NSAIDs, cytotoxic drugs, hormones.
A perforated stomach ulcer belongs to the category of severe, life-threatening diseases. A perforation occurs in the wall of the organ and the contents flow directly into the abdominal cavity. As a result, peritonitis develops, which requires immediate surgical intervention.
Perforated (perforated) gastric ulcer (ICD10 code - K25) is one of the most severe pathologies of the abdominal cavity. It is a penetrating injury to the gastric wall that occurs at the site of a chronic or acute ulcer. This complication is common and ranks second after acute appendicitis.
This disease occurs in all age categories, including children, but perforation of a stomach ulcer occurs more often in men in the age group of 20-50 years than in women.
In a fairly short period (several hours), the patient develops purulent inflammation of the abdominal cavity. In the absence of prompt assistance, the disease can be fatal. With a perforated ulcer, as a result of recurrent inflammation, a through hole appears in the walls of the digestive organs.
If a hole appears inside the organ, severe bleeding may occur. The main danger is that the contents of the stomach or intestines end up in the abdominal cavity.
Diagnostics
Diagnostics may be complicated by temporary improvement in the patient's condition when there are no pronounced clinical symptoms and the perforation is covered by neighboring organs or the omentum. In this case, a comprehensive examination is prescribed, which includes:
- X-ray (in the pictures you can see accumulations of gases in the right hypochondrium under the diaphragm);
- Ultrasound examination of the abdominal cavity (determines the presence of gas in the abdominal cavity, crescent-shaped diaphragm, diffuse abscess);
- Endoscopy (using a probe to determine the degree of perforation and location of the hole);
- General and biochemical blood test (determines the degree of intoxication during peritonitis, as well as the level of leukocytes in the presence of inflammation);
- Laparoscopy (performed to confirm the diagnosis, especially in an atypical form).
If it is difficult to make a diagnosis, an FGDS (fibrogastroduodenoscopy) is performed - straightening the gastric walls with the help of a powerful air flow.
Possible complications and consequences
If you do not seek medical help in a timely manner, severe purulent complications of a perforated ulcer, including generalized sepsis, may develop. Such conditions are life-threatening.
Postoperative complications of a perforated ulcer may include:
- bronchopneumonia;
- peritonitis;
- failure of the sutures with repeated release of intestinal contents into the peritoneal cavity;
- gastrointestinal bleeding;
- violation of the evacuation function of the stomach.
Patients with immunodeficiency and the elderly are more at risk of developing postoperative complications of a perforated ulcer.
A perforated ulcer is a life-threatening condition, resulting in death in approximately 8% of cases, even with timely diagnosis and surgical treatment. Relapses occur in less than 2% of cases. When surgical intervention is performed 12 hours after the onset of the disease and later, postoperative mortality increases to 20–40%. Treatment of a perforated ulcer at the stage of diffuse peritonitis is often delayed and does not have a positive effect.
If timely treatment of a stomach ulcer is ignored, it may perforate, which leads to various serious complications. During the formation of holes, the contents escape into the free abdominal cavity, which has a detrimental effect on the human body. Also, with perforation of the stomach, pressure and temperature can often increase and vomiting may occur.
Possible complications include the following:
- diffuse peritonitis;
- postoperative pneumonia.
In addition to the above complications, perforation of the stomach and duodenum can be fatal.
Symptoms
The symptoms of the disease and its stage depend on the clinical form of the perforated ulcer. There are 2 forms of development of perforation:
In a typical form, the following stages are distinguished:
The duration of pain and its severity depends on the degree of filling of the stomach, the location and size of the through wound. Painful sensations first arise in the epigastric region, then spread to the entire abdominal cavity, while the patient tries not to move, since the pain symptom intensifies with movement and tension of the abdominal muscles. The pain is so unbearable that a person in a lying position presses his knees to his stomach, trying to alleviate his condition at least a little.
Another symptom in a typical form is the presence of gas in the abdominal cavity, which enters it along with food. The presence of gas is determined by percussion (tapping on the abdomen) based on the response sound. Gas can spread diffusely throughout the abdominal cavity, but is most often localized under the diaphragm.
Other symptoms of a perforated ulcer in a typical form:
False improvement - all acute symptoms subside, the patient thinks that the disease has receded. Symptoms at this stage:
Painful sensations subside as a result of the release of exudate - an anti-inflammatory fluid secreted by the surrounding capillaries in the abdominal wall, and a decrease in the sensitivity threshold of nerve endings. Taking painkillers speeds up the process of false improvement in well-being. But this condition does not last long; after 6–12 hours of imaginary well-being, the patient’s condition sharply worsens.
Peritonitis is the spread of a bacterial infection throughout the abdominal cavity.
The following symptoms are characteristic:
- nausea, vomiting;
- bloating;
- increase in body temperature to 38–49 degrees;
- dehydration, anuria;
- tension of the abdominal walls;
- dry mouth, coating on the tongue;
- increased heart rate - up to 120 beats;
- earthy skin color;
- sunken cheeks, eyes.
Gradually the temperature drops to 36 degrees and below, the level of hemoglobin, potassium and leukocytes in the blood increases. Medical assistance at this stage no longer helps.
An atypical form of perforation is observed when there is a small through hole in the stomach, the bottom of the wound is covered by neighboring organs: the liver, gall bladder or omentum. During the course of the disease there are 2 stages:
Perforation is the opening of a through wound into the abdominal cavity and minor entry of food into the abdominal cavity. The same symptoms are observed as in the typical form, but the pain is less pronounced.
Feeling better – 40–50 minutes after perforation, symptoms subside, the bottom of the hole is covered with folds of the gastric mucosa or abdominal tissue. If the hole is tightly covered and food no longer enters the abdominal cavity, then a perforated ulcer can heal on its own. Under the influence of unfavorable factors, perforation can progress and turn into a typical form of the disease.
Diet after surgery
With the help of diet, it is possible to reduce the load on the gastrointestinal mucosa. In order for the epithelium to recover faster, the patient will need to eat soft food that is easily digested. It is important to exclude foods that have aggressive effects on the walls of the gastrointestinal tract. In addition, products should not contribute to an increase in the secretion of acid, which provokes the occurrence of pathology.
The attending physician adjusts not only the patient’s diet, but also the conditions for consuming food. You will need to eat small portions at least 5 times a day. It is imperative to stop drinking alcohol and smoking. This is due to the fact that alcohol burns the mucous membrane, which causes severe pain.
If we talk about the harmful substances that are in cigarettes, they also irritate the walls of the digestive tract. Because of this, serious consequences often occur after surgery. Treatment prohibits the consumption of carbonated drinks, as well as strong tea and coffee.
In addition, the patient will need to remember the following nutritional rules for gastric disease:
- You should not drink large amounts of liquid or overeat, as this causes stretching of the stomach walls.
- Monitor the temperature of the food, which should not be excessively cold or hot.
- Chew foods thoroughly.
Diagnostics
The symptom of dagger pain, diffuse pain throughout the abdomen, rapid deterioration of the patient’s condition and a history of peptic ulcer disease will allow a diagnosis of gastric perforation to be made with a high degree of certainty.
The diagnosis will be confirmed by physical, instrumental and laboratory examination data. You should be wary of covered perforation - in this case, the symptoms may be blurred, and the diagnosis will be incorrect, but at any moment the covering organs or tissues may be displaced, and the contents of the stomach will re-enter the abdominal cavity (despite the fact that the peritoneum is already compromised).
At the shock stage, physical data are as follows:
- upon examination, even by the appearance of the patient, one can ascertain a rapid deterioration in the general condition. In an attempt to alleviate the condition, the patient takes a forced position - lies on his side, pressing his knees to his stomach (the so-called fetal position, which reduces stretching and irritation of the peritoneum). The skin and visible mucous membranes are pale and moist, the tongue remains moist, but is slightly coated with a white coating, the amount of which will increase as the pathology progresses;
- when palpating (feeling) the abdomen, there is pronounced tension in the abdominal wall, severe pain throughout the entire abdomen, but symptoms of peritoneal irritation are either absent or mild;
- when percussing (tapping) the abdomen, pain is also noted throughout the abdomen;
- during auscultation (listening with a phonendoscope) of the abdomen - the data at this stage are not very informative, although a weakening of peristaltic noise may already appear.
- when monitoring hemodynamics, the pulse becomes rarer (sometimes the lower limit of normal, which has never been observed in a particular patient), blood pressure decreases.
At the stage of imaginary well-being, physical data will be as follows:
At the stage of peritonitis, the following physical examination data are determined:
The main methods for confirming gastric perforation are instrumental diagnostic methods, namely:
- survey fluoroscopy and graphy of the abdominal organs - thanks to it, it is possible to identify gas and effusion in the abdominal cavity, which appeared here due to their penetration from the stomach;
- Ultrasound examination of the abdominal organs (ultrasound) - it can be used to detect effusion in the abdominal cavity;
- esophagogastroduodenoscopy (EFGDS) - using an endoscope, a pathological hole in the wall of the stomach is visually identified. EGD should be carried out with caution so that if the endoscope accidentally enters the lumen of the hole, it does not expand it and does not aggravate the release of gastric contents into the abdominal cavity;
- diagnostic laparoscopy - performed if doubts arise when making a diagnosis, as well as if an atypical (covered) gastric perforation is suspected;
- diagnostic laparotomy - if the symptoms are unclear or vague, surgeons may open the anterior abdominal cavity for diagnostic purposes. When perforation is confirmed, diagnostic laparotomy automatically becomes a routine medical operation, during which the hole in the stomach wall and the consequences of the perforation are eliminated.
Laboratory diagnostic methods are not decisive in the diagnosis of gastric perforation, but they are used in complex diagnostics to obtain an overall picture - the following are used:
- general blood test - an increase in the number of leukocytes and ESR confirms the progression of the inflammatory process during peritonitis;
- general urinalysis - with severe peritonitis, the amount of urine decreases, the specific gravity increases, erythrocytes and leukocytes are detected in the urine.
How to treat a perforated ulcer
Surgery for this diagnosis is most often performed using classic laparotomy (dissection of the anterior wall of the peritoneum). In some cases, it is possible to suturing a perforated ulcer if it is small. Suturing is done when purulent inflammation lasts more than six hours. Complications are possible after this operation. The postoperative period requires long-term drug therapy for recovery.
Conservative treatment takes place only in two cases:
- with decompensated somatic pathology;
- with a decisive refusal of surgical intervention by the patient.
Mandatory conditions for such treatment are:
- age under 70 years;
- less than half a day from the start of perforation;
- stable hemodynamics;
- absence of tension pneumoperitoneum.
The treatment complex includes pain relief, the use of antisecretory drugs and antibiotics, detoxification and anti-Helicobacter therapy.
Treatment
Treatment is carried out by surgical intervention; the choice of method depends on the form of the perforation, the stage of the disease, the age of the patient, the location of the perforation, and its size. Basic methods:
Suturing a perforated ulcer.
The method is indicated for a small perforated hole, peritonitis, a serious condition of the patient, and also in the absence of bleeding in the area of the ulcer. This type of operation is performed in 90% of cases of treatment of perforated ulcers.
For young people, surgery is indicated in the absence of a peptic ulcer; for older people, surgery is prescribed due to the likelihood of complications developing with other surgical methods. The operation is performed under local or general anesthesia.
https://youtu.be/5Erp5o2Ic2A
Excision of a perforated ulcer.
The method is used for chronic peptic ulcer disease, before suturing the perforated hole. A through wound is almost always smaller in size than the area of the ulcer in the gastric wall, so simply suturing the wound, without excision of the ulcer itself, can lead to the re-development of perforation. During excision, healthy areas are captured to minimize the risk of recurrence of the disease.
How to eat after surgery?
After 5 days have passed after surgery, a person can drink small amounts of drinks. With their help, it is possible to improve the functioning of the digestive organs and strengthen the immune system. It is recommended to make a decoction of rose hips, to which you can add a little honey.
10 days after surgery for a perforated gastric ulcer, the menu includes some dishes that improve the activity of the gastrointestinal tract. It is acceptable to eat vegetable puree soups, viscous porridges, steamed protein omelettes, and steamed cutlets made from lean meats. The patient will need to follow this diet for at least 30 days.
Causes
In most cases, the development of perforation of an ulcer inside the stomach and duodenum is caused by an advanced stage of a simple chronic peptic ulcer.
The most common factors that cause symptoms of perforated gastric and duodenal ulcers are:
- exacerbation of symptoms of a chronic duodenal ulcer;
- frequent overeating, as a result of which the walls of the digestive organs are subjected to severe stretching;
- increased acidity;
- alcohol abuse, excess fatty foods;
- frequent physical overexertion.
However, these factors can cause a perforated ulcer only if a chronic form of peptic ulcer is already present in the human body.
It is worth remembering that these reasons are due to an imbalance in the internal protective functions of the mucous membranes of the digestive organs and aggressive factors, the main part of which is also produced by the internal organs of the human body (hydrochloric acid, digestive enzymes). An exception is the bacterium Helicobacter pylori, which lives in the body of a large number of people, but has a pathological effect on organs only under the influence of various unfavorable factors.
Most researchers are of the opinion that the key factor under the influence of which a peptic ulcer causes perforation is the bacterium Helicobacter pylori. This is confirmed by the fact that 90% of people with ulcers are infected with such microorganisms. In addition, antibacterial therapy for this disease has a positive effect, which indicates the bacterial origin of the pathology.
However, the mere fact of infection is not enough, since most of the entire population of the Earth is a carrier of the bacterium Helicobacter pylori; not everyone is susceptible to duodenal ulcers.
Healthy recipes
Vegetable salad
You will need to take 1 potato and a quarter of beets. Rinse the vegetables thoroughly and boil. Then cool and peel. Cut into small strips and add a little salt. Season with a small amount of olive or vegetable oil and stir. Serve with finely chopped greens.
Chicken with apples
You will need chicken fillet and 3 small apples. The meat is washed, listened to with a kitchen towel and seasoned with a little salt. The fruits are peeled, the insides are removed and cut into thin slices. They are placed in a baking sleeve, fillet is placed on top, the top of which is also covered with apples. The oven is preheated to 200 degrees, then the dishes are placed there for 30-40 minutes.
Take a head of vegetable, an egg, a glass of low-fat milk, 2 tablespoons of sour cream. Cauliflower is divided into inflorescences, washed and boiled. The boiled vegetable is passed through a sieve or crushed with a blender. Heated milk is added to the chopped cauliflower and put on fire. When the soup boils, mix the egg with sour cream and add it to the dish, stirring and bringing to a boil again. Before use, the soup must be cooled to room temperature so as not to burn the mucous membrane of the gastrointestinal tract.
Symptoms, diet and surgery for perforated gastric ulcer
The first rule for recovery and reducing the risk of relapse is strict adherence to the doctor’s instructions. An exception to the rule “if you can’t, but really want to” doesn’t work. During the postoperative period, a strict diet is established. It can last from 3 to 6 months. The diet becomes more complex gradually.
The daily number of meals is up to 6 times, in small portions.
All foods taken must be puree or semi-liquid.
Food should be steamed or boiled
Salt should be taken in limited quantities
You should also limit your intake of simple carbohydrates (sugar, chocolate, baked goods) and liquids.
On the 2nd day after the operation, mineral water, fruit jelly, and weak, slightly sweetened tea are allowed.
After 2-3 days, the diet is replenished with rosehip decoction, pureed soups and porridges made from rice and buckwheat. Vegetable puree soups made from boiled carrots, pumpkin, zucchini, potatoes or beets. You are allowed to eat a soft-boiled egg and a steam soufflé made from pureed cottage cheese.
On the 10th day after the operation, puree from boiled carrots, pumpkin, zucchini or potatoes is introduced into the diet. Gradually introduce steamed cutlets, soufflés, purees, quenelles, meatballs or zrazy from lean meats or fish. They add cheesecakes, puddings, and cottage cheese casseroles. You can also use fresh pureed cottage cheese. In addition, whole milk and non-acidic dairy products (acidophilus, yogurt, matsoni) are introduced.
Only after a month does it become possible to consume bread products: dried bread, stale bread, crackers.
After 2 months, it is allowed to add fresh sour cream to food and consume kefir.
After surgical treatment of a perforated gastric ulcer, patients need to follow a certain diet to restore the functioning of the digestive system and prevent re-perforation.
The details of the diet may vary depending on the extent of the operation performed, but its general points are the same.
- During the first 3 days after surgery, fasting is recommended; otherwise, increased peristalsis and secretion may result in divergence of surgical sutures.
- From the 4th day, jelly and diluted compotes are allowed, as well as light slimy porridges and vegetable soups with water.
- When 1-1.5 weeks have passed after the operation, steamed chicken and fish cutlets, soft-boiled eggs and vegetable puree can be added to the daily menu.
Perforation of a stomach ulcer is an event that requires lifelong adherence to a strict diet. Frequent meals (at least 4-5 times a day) in small portions are recommended. Long periods of fasting and attempts to suppress hunger with snacks and other “junk” foods are strictly prohibited.
The first rule for recovery and reducing the risk of relapse is strict adherence to the doctor’s instructions. An exception to the rule “if you can’t, but really want to” doesn’t work. During the postoperative period, a strict diet is established. It can last from 3 to 6 months. The diet becomes more complex gradually.
- The daily number of meals is up to 6 times, in small portions.
- All foods taken must be puree or semi-liquid.
- Food should be steamed or boiled
- Salt should be taken in limited quantities
- You should also limit your intake of simple carbohydrates (sugar, chocolate, baked goods) and liquids.
On the 2nd day after the operation, mineral water, fruit jelly, and weak, slightly sweetened tea are allowed.
10 days after the operation, the menu includes mashed potatoes, carrots, and boiled pumpkin. All dishes must be chopped, not spicy, not salty, not fatty. Bread can be added to the diet only after a month.
In general, after surgery, clinical recommendations are to follow a special diet for a period of 3 months to six months.
After switching to a regular diet, it is recommended to adhere to the rules of a healthy diet; it is useful to eat natural foods, such as fresh vegetables and fruits, dairy products, and dietary meat. Smoking and drinking alcohol is strictly prohibited.
Gastric removal
Complete removal of the stomach or gastrectomy is performed when the ulcer becomes malignant. To remove an ulcer, the abdominal cavity is opened and the location of the tumor is assessed.
If the upper part of the stomach and esophagus are affected, an additional diaphragmatic incision is made. Together with the stomach, the ligamentous apparatus, part of the omental layer, and a section of retroperitoneal fat are removed. The stomach is cut off at the junction of the esophagus and the duodenal region. After excision of the body of the stomach, the lumen of the esophagus and duodenum are sutured.
The operation to completely remove the stomach is classified as complex. This concerns the patient’s health status, the technical abilities and knowledge of the surgeon who will perform the surgery. Surgical treatment often results in a lot of complications. This is due to the technical difficulties that arise when carrying out such treatment. Final removal is highly traumatic for the body.
The patient loses the ability to digest food physiologically. In addition to digestive problems, a patient operated on in this way experiences a complication associated with the hematopoietic system. The stomach produces special biologically active substances that normally stimulate the processes of erythropoiesis. In addition, patients begin to be bothered by the complication of backflow of food mass from the small intestine into the esophagus.
If the fusion of sutures between the remaining parts of the digestive system is delayed and disrupted, the process is considered an extremely serious complication. With this development of events, the patient has almost no chance of recovery. If the outcome of the operation is favorable, the patient is discharged from the hospital after two weeks.
Pain shock stage
During this period, the patient feels acute pain in the abdomen. Patients compare it to the blow of a dagger: it is a sharp, severe and acute pain. At this time, vomiting may occur, the patient has difficulty getting up, his skin is pale and cold sweat may appear.
Breathing is rapid and shallow, pain occurs when taking a deep breath, blood pressure is low, but the pulse remains within the normal range: 73-80 beats per minute. With a perforated duodenal ulcer, the abdominal muscles are tense, so palpation is difficult.