Gastroenteritis is a lesion of the epithelial membrane (catarrh) of the stomach and duodenum, predominantly of an acute nature. Catarrh of the stomach and proximal small intestine can be caused by infectious pathogens (viruses and bacteria), as well as external and internal factors, such as poor diet or uncontrolled use of medications. Symptoms and treatment of gastroenteritis in adults differ from children and adolescents: in patients over 18 years of age, the disease usually occurs in a milder form, which significantly reduces the risk of complications and serious consequences for the body.
Gastroenteritis: symptoms and treatment in adults
Causes
Acute infectious gastroenteritis can be caused by viruses, bacteria or parasites. The most common viral gastroenteritis is caused by:
- noroviruses;
- rotaviruses;
- astroviruses;
- adenoviruses.
In people with weakened immune systems, diarrhea can also be caused by cytomegalovirus or enterovirus.
Bacterial gastroenteritis is diagnosed less frequently than viral gastroenteritis. It is often caused by the following pathogens:
- salmonella;
- cambilobacter;
- shigella;
- Escherichia coli (especially serotype O157:H7);
- clostridia (Clostridium difficile).
Parasitic lesions of the gastrointestinal tract are usually caused by Giardia and Cryptosporidium. Sometimes infectious gastroenteritis becomes chronic. This often occurs in people with weakened immune systems or with existing gastrointestinal diseases.
Other causes of chronic inflammation of the gastric and intestinal mucosa are as follows:
- poor nutrition;
- bacterium Helicobacter pylori;
- stress;
- long-term use of certain medications (non-steroidal anti-inflammatory drugs, cytostatics, etc.);
- allergic reactions;
- bad habits (smoking, alcohol abuse).
How to treat gastroenteritis?
Modern medicine even today does not yet have effective drugs that affect the etiology. The basic principles on which the treatment of gastroenteritis in adults is based are:
- Refusal to eat on the first day of the acute course.
- Drink plenty of fluids.
- At the end of the acute period, a light diet is prescribed.
- Daily routine with mandatory bed rest.
- The use of multienzyme drugs, including Abomin, Polyzyme, Pancreatin, Festal.
- The use of powerful adsorbents and astringents.
- Rehydrants in the form of intravenous drips.
- Plasma replacement and detoxification solutions - Regidron, Refortan are recommended to drink.
To prevent the development of dehydration, you can prepare a saline solution at home. To do this, you need to dissolve 1 tbsp in 1 liter of boiled water. l. table salt and 2 tbsp. spoons of sugar. Also, to replenish fluid and electrolyte losses, you can use pharmaceutical powders for preparing rehydration solutions, such as Rehydron or Oralite. It is also useful to drink sweet tea, rosehip decoction and jelly. You need to take liquid often, but in small portions (no more than 50 ml at a time) so as not to provoke an attack of vomiting.
In case of severe dehydration, when oral rehydration is not enough, intravenous administration of solutions (5% glucose solution, saline solution, rheopolyglucin) is possible. Infusion therapy is also an indication for severe intoxication syndrome, which can be observed with gastroenteritis. Often in patients with gastroenteritis, symptoms of vitamin deficiency are detected, so vitamin therapy is used. In outpatient settings, patients are recommended to use multivitamin complexes.
It should be noted that antibiotic therapy can only be prescribed by a doctor. You should not try to treat gastroenteritis with antibiotics on your own. If the disease was caused by a virus, this group of drugs will be completely ineffective. At the same time, the negative effect of antibiotics on the intestinal microflora can only worsen the condition.
To restore the affected mucous membrane of the stomach and intestines, enveloping and astringent agents (bismuth preparations) are prescribed. For the same purpose, it is possible to use preparations based on plant materials (tansy, St. John's wort, serpentine grass). Physiotherapy is also effective in treating gastroenteritis. Patients are prescribed paraffin baths, warming compresses, inductothermy, and ozokerite. With gastroenteritis, the composition of the normal intestinal microflora is often disrupted, so taking eubiotics is advisable. In some cases, antibacterial drugs are used.
Symptoms
The nature and severity of symptoms of gastroenteritis vary. The acute version of the disease usually has a sudden onset and is accompanied by the following symptoms:
- lack of appetite;
- nausea;
- vomiting;
- pain and cramps in the abdomen;
- diarrhea (sometimes with blood or mucus).
Additionally, malaise, muscle pain, and general weakness are sometimes associated. The abdomen becomes painful upon palpation, and in rare cases, tension in the abdominal muscles occurs. With gastroenteritis, rumbling is often heard - an important sign that allows you to distinguish inflammation from intestinal paresis. Frequent vomiting and diarrhea lead to loss of fluid and electrolytes and, as a consequence, hypotension and tachycardia. In severe cases, shock, vascular collapse and oliguric renal failure occur.
Abdominal pain is one of the symptoms of chronic gastroenteritis Photo: shutterstock.com
In chronic gastroenteritis, the symptoms are less pronounced. Often the leading symptom is discomfort or pain in the abdomen. Sometimes the pain is quite intense, which may indicate the presence of ulcers, erosions or microdamages of the gastrointestinal tract. Dyspeptic disorders (nausea, belching, heartburn), bloating, increased bowel movements or, conversely, constipation are typical.
Over a long period of time, chronic gastroenteritis leads to malabsorption of nutrients (malabsorption syndrome). Signs of hypovitaminosis and protein deficiency occur: hair loss, brittle nails, weight loss, weakness, fatigue, etc.
How does the disease manifest itself?
As a rule, the clinical picture of acute gastroenteritis appears in a short time, namely within a couple of hours or days after the influence of the provoking factor. The period before the onset of symptoms in acute gastroenteritis of an allergic or toxic nature is shorter than others.
The infectious form of the pathology can develop within 5 days after interaction with the pathogen (consumption of food, water, contact with a sick person). The first symptoms that occur with the disease are nausea and vomiting. The contents of the stomach are usually released once, but in severe forms there may be repeated and debilitating vomiting.
Nausea and vomiting are accompanied by abdominal pain, which is localized in the epigastric region and around the navel; additionally, bloating and rumbling in the abdomen and loss of appetite appear. Diarrhea comes a little later. The stool is repeated and can reach ten times a day.
The feces are first mushy, and then liquid, foamy, contain fragments of undigested food, and have a different color from the norm (bright yellow, dark green, green, orange). Usually the stool is free of blood and mucus. In some cases, mucus appears in the stool after some time.
The clinical picture of acute gastroenteritis is similar to that of acute gastritis
In acute gastroenteritis of allergic origin, abdominal pain and vomiting usually first occur, which brings relief. After emptying the stomach, the general condition quickly improves. Toxic gastroenteritis usually causes a short-term fever that appears early in the disease.
If gastroenteritis is caused by an infection, then the body temperature rises a couple of hours after the manifestation of the disease and may not return to normal for several days. If vomiting and diarrhea occur, you should consult a doctor, since in the absence of treatment, severe intoxication and dehydration may develop.
With a lack of fluid, the skin and mucous membranes become dry, the hands and feet become cold, a coating appears on the tongue; if you pinch, the skin slowly returns to its original position. This condition is especially dangerous for young children, since irreversible changes can occur in a short period of time.
If fluid loss is 10% of body weight or more, then convulsions, impaired consciousness, tachycardia, drop in blood pressure, and severe weakness may occur. With severe dehydration, body temperature drops to 35 ⁰C and the number of urinations decreases, up to their complete absence.
Gastroenteritis is dangerous due to dehydration and intoxication.
Depending on the clinic, acute gastroenteritis occurs:
- mild severity (normal body temperature, vomiting and diarrhea up to three times a day, no dehydration has developed);
- moderate severity (temperature does not exceed 38.5 ⁰C, vomiting and diarrhea no more than 10 times per day, moderate dehydration);
- severe (severe fever, severe dehydration, signs of central nervous system dysfunction, diarrhea and vomiting more than 15 times a day).
The clinical picture of acute gastroenteritis depends on the species of the pathogen. With a disease of a bacterial nature, the course is usually more severe than with a viral one; intoxication syndrome and fever are characteristic.
With bacterial gastroenteritis, the cells of the mucous tissue are damaged by toxins, so severe cramping pain often occurs along the intestines. In case of viral etiology, the leading factor is not abdominal syndrome, but dehydration; there are signs of respiratory infection.
https://youtu.be/M_qXQYlCLeg
Diagnostics
The diagnosis is made based on the existing symptoms (loose stools, vomiting, fever, etc.). Additionally, medical history data is taken into account, for example, recent travel, drinking water from open reservoirs, contact with sick people, etc. Oral use of antibiotics (within the last two to three months) should raise suspicion of Clostridium difficile infection.
To clarify the etiology of gastroenteritis, a clinical examination of stool is performed:
- enzyme immunoassay (search for antibodies to certain pathogens);
- PCR method (polymerase chain reaction) to identify pathogen antigens;
- bacteriological examination of stool, placing it on nutrient media and determining sensitivity to antibiotics.
A blood test may be prescribed to check the level of electrolytes, liver and kidney function indicators (transaminases, urea, creatinine, etc.). A complete blood count with white blood cell count helps differentiate bacterial and viral gastroenteritis.
Fibrogastroscopy is necessary for the diagnosis of ulcers, erosions and neoplasms of the gastric and duodenal mucosa Photo: Pavel L Photo and Video / Shutterstock.com
Fibrogastroscopy is necessary for the diagnosis of chronic gastroenteritis. It allows you to identify microdamages of the gastrointestinal mucosa, ulcers, erosions, and neoplasms.
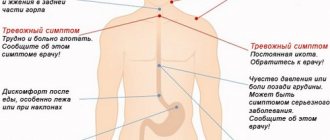
When do you need to see a doctor urgently?
In mild cases, gastroenteritis, as a rule, does not require specialized medical intervention and goes away on its own within 4-7 days. Signs of an urgent need to seek specialized medical help are the appearance of the following symptoms:
- vomiting that does not stop for 2 days;
- diarrhea that does not stop for 3 days;
- the appearance of muscle cramps;
- a rise in body temperature above 39 °C;
- a feeling of dry mouth, scanty urination or its complete absence;
- the presence of blood elements in feces or vomit;
- the appearance of visual hallucinations.
In acute gastroenteritis, dehydration may develop, threatening the patient's life, up to the formation of circulatory failure and anuria. If the disease is not treated, the following pathologies may develop: dysbacteriosis, toxic shock, toxic damage to the heart, liver, kidneys, and the disease may become chronic.
Treatment
Therapeutic measures include the following aspects:
- rehydration (oral, parenteral);
- antiemetic drugs;
- antidiarrheal drugs;
- antibiotics for the bacterial nature of the disease;
- probiotics, gastroprotectors.
For moderate to severe diarrhea, bed rest is recommended.
Rehydration
For oral rehydration, special solutions are used (Regidron, Humana Electrolyte, etc.). Even if the patient is vomiting, small sips of liquid should be taken. In case of significant dehydration, drugs for intravenous administration are used (Quartosol, Chlosol).
Children become dehydrated much faster than adults. Even with mild disease, adequate rehydration is required.
After symptoms subside and there is no vomiting, you can gradually eat solid food. It is better to start with easily digestible carbohydrates (bananas, bread, mashed potatoes). Then protein products (fish, lean meat) are added. In the subacute period, lactose intolerance often occurs, so it is better to avoid dairy products for a while.
Antiemetics
If vomiting recurs and surgical pathology has been ruled out, the doctor may recommend one of the following medications:
- Metoclopramide;
- Ondansetron.
In outpatient practice, Ondansetron is used in the form of lozenges. Usually a single dose is enough to stop a child from vomiting. If symptoms persist, re-diagnosis is required.
Antidiarrheals
They are used to treat patients older than 2 years. Remember that antidiarrheal drugs can make the condition worse in people with Clostridium difficile or Escherichia coli O157:H7 infection, so only a doctor should prescribe them.
The most effective antidiarrheals are:
- Loperamide;
- Diphenoxylate.
Antimicrobial drugs
Even with proven bacterial gastroenteritis, antibiotics are not always needed. They are usually recommended strictly according to indications and taking into account stool culture. This point should be especially taken into account in children with suspected Escherichia coli O157: H7 infection. In them, antibiotics increase the risk of hemolytic-uremic syndrome.
At the same time, antibiotic therapy is the basis for the treatment of chronic gastroenteritis associated with Helicobacter pylori. In this case, combination regimens using two or three drugs are recommended.
Probiotics and gastroprotectors
Gastroprotectors (Rebagit, Rebamipide) have a protective effect on the cells of the gastric mucosa. They are indicated for gastroenteritis of any etiology (infectious, drug-induced, allergic), especially in the presence of ulcers and erosions of the gastrointestinal tract.
Probiotic drugs (Linex, Bifiform) are mainly used to treat chronic gastroenteritis. In acute diarrhea, they shorten the duration of the disease; in chronic form, they help normalize intestinal function.
What is chronic gastroenteritis?
Causes
- poor nutrition;
- abuse of spicy foods and alcoholic drinks;
- food allergies;
- harmful working conditions;
- radiation exposure;
- helminthic infestations.
Symptoms
Treatment of chronic gastroenteritis
| Group of drugs | Mechanism of therapeutic action | Representatives | Mode of application |
| Vitamin preparations | Normalize metabolic processes and improve nutrition of the tissues of the stomach and intestinal walls. Strengthens the immune system and the general condition of the patient’s body. | Pangexavit | 1 tablet 3 times a day, for a course of 30 days. |
| Undevit | Orally after meals, 2 tablets 3 times a day. Duration 20-30 days. | ||
| Antimicrobials | Causes the death of bacteria and protozoa. | Enteroseptol | Orally, 1-2 tablets after meals, for a course of 10-12 days. |
| Intestopan | Orally, 1-2 tablets 3 times a day, for a course of 2 weeks. The tablets are crushed and washed down with water. | ||
| Astringents | A film is formed on the damaged mucous membrane that protects against irritating substances. | Thealbin (tanalbin) | 1 tablet inside. (0.3-0.5 g) 3-4 times a day. |
During treatment, it is necessary to follow diet 4 (4-a, b) and completely eliminate alcohol.
are used as an astringent and anti-inflammatory agent :
- Oak bark decoction. 2 tbsp. the bark is poured with a glass of boiling water and heated in a water bath for half an hour. Cool, squeeze, add boiled water to 200 ml. Take 1/4 cup 4 times a day on an empty stomach.
- Infusion of bird cherry fruits. 2 tbsp. dried berries are poured into a glass of boiling water. Let it brew for 20 minutes. Accepted according to the same scheme.
- Infusion of blueberry fruits. 2 tsp dry or 4 tsp. pour fresh berries with a glass of cold water and leave overnight. Take 2 tbsp during the day.
Treatment of gastroenteritis
mineral waters of low and medium mineralization. The mechanism of action of mineral waters has not been fully studied. As a result of treatment, the production of gastric juice and digestive enzymes is normalized, and inflammation is reduced.
For chronic gastroenteritis it is recommended:
- Ekateringofskaya;
- Zheleznovodskaya;
- Izhevskaya;
- Essentuki No. 4;
- Narzan.
Mineral waters are taken 20-30 minutes before meals in small sips 3-4 times a day, 100-150 ml. The course of treatment is 30-45 days. Treatment can be done at a resort or at home.
Physiotherapy for gastroenteritis
improves blood circulation and trophism in the tissues of the stomach and small intestine. During treatment, the innervation and functioning of the digestive organs are normalized:
- inductometry is indicated for reduced acidity of gastric juice;
- decimeter therapy for gastritis with increased secretion;
- galvanization and electrophoresis with antispasmodics;
- exposure to diadynamic currents;
- ultrasound therapy;
- paraffin and ozokerite applications;
- heating pads on the area of the stomach and small intestine.
Treatment is carried out in courses of 10-15 procedures every six months.
Prevention of chronic gastroenteritis
- Maintaining a healthy diet;
- adherence to daily routine;
- treatment of diseases of the digestive system.
It is recommended to avoid:
- alcohol consumption;
- smoking;
- overeating;
- excessively spicy and fatty foods;
- occupational hazards.
Prognosis and prevention
The prognosis is favorable in most cases. With timely treatment of acute gastroenteritis and adequate rehydration, recovery occurs. Deaths are relatively rare; for example, with rotavirus infection they account for only 3.5%. Chronic gastroenteritis also has a favorable prognosis. However, careful diagnosis is required to determine the cause of the disease. Treatment is longer; lifestyle and nutritional adjustments are necessary.
Specific prevention has been developed only for rotavirus gastroenteritis. According to WHO recommendations, the vaccine (Rotarix, Rotatek) should be included in the compulsory vaccination plan.
Nonspecific prevention includes:
- adequate heat treatment of products;
- using water from proven sources, boiling;
- compliance with personal hygiene rules (hand washing, disposable tableware, etc.).
Correcting your lifestyle and giving up bad habits will help you avoid chronic inflammation. Meals should be divided (every 3-4 hours), and long breaks between meals should be avoided. Medicines should be taken strictly as prescribed by the doctor and not self-medicated.
Acute gastroenteritis in children
Asymptomatic carriers of infection are usually identified among adults. In children, gastroenteritis, on the contrary, occurs in the most acute form.
Timely identification of such asymptomatic carriers of infection in schools, kindergartens and other institutions plays a huge role in the prevention of acute gastroenteritis in children. Children under 3 years of age are most susceptible to viruses. The source of gastroenteritis infection in children under one year of age is often the mother herself. The risk group includes babies with congenital diseases, various forms of immunodeficiency, or children who are bottle-fed.
Post-infectious immunity of gastroenteritis is short-lived.