Dysentery is an infection of the gastrointestinal tract, the source of which is localized mainly in the large intestine.
The disease has a bacterial etiology, and its causative agent is microorganisms of the genus Shigella. When pathogenic microorganisms are destroyed, toxins are released into the blood and determine the course and manifestation of pathology.
Shigella retains its vital activity in the external environment for a long time. Also, given favorable conditions, these bacteria are able to multiply in food products - salads, meat, minced meat, boiled fish, dairy products, etc. For this reason, the storage of such products must be taken seriously.
Dysentery: treatment
Properly organized therapeutic nutrition plays a huge role in the successful treatment of dysentery.
All foods rich in fiber that can cause irritation of the intestinal walls should be excluded from the patients' diet. The diet is based on mechanical and chemical sparing of the digestive tract. Patients are recommended boiled or steamed dishes, preferably pureed. The diet can include:
- Meatballs and steamed meatballs;
- Dairy-free boiled porridge;
- Puree soups with weak broths.
Meals are organized at least 5–6 times a day, while reducing the volume of portions eaten.
Considering that the causative agent of dysentery causes serious damage to the intestinal walls, the diet should be followed not only in the acute period, but also at the convalescence stage.
Drug treatment of dysentery includes the prescription of antibacterial drugs, which are prescribed only by an infectious disease doctor, taking into account the characteristics of the clinical picture of the disease, the general condition of the patients, the presence of concomitant diseases, etc.
Ampicillin is usually used to treat dysentery. If the causative agent of the disease is resistant to it, the doctor may prescribe other antibiotics, for example, rifampicin or aminoglycosides.
Frequent stools lead to disturbances in the water-electrolyte balance of the patient’s body
Therefore, from the first hours of the onset of dysentery symptoms, it is important to begin dehydration. For mild degrees of the disease, oral dehydration is performed, for which the patient is recommended to drink special solutions (Regidron, Peditral, WHO powder, etc.) often and in small sips.
In severe cases, correction of the water-salt balance is carried out by intravenous administration of saline solutions and isotonic glucose solution.
With a long course of dysentery, the introduction of immunostimulating agents into the general treatment regimen is justified.
The waste products of dysentery pathogens, as well as ongoing antibiotic therapy, negatively affect the normal intestinal microflora, which can lead to the formation of intestinal dysbiosis and prolongation of the disease. Therefore, eubiotics (bifidumbacterin, lactobacterin, narine, bificol, etc.) are also included in the treatment regimen for dysentery.
In order to normalize the motor activity of the intestine and reduce the manifestations of the inflammatory reaction in it, antispasmodics and astringents are used. Also, many doctors include decoctions of herbal plants (oak bark, chamomile, etc.) as part of the complex therapy of dysentery.
Nutrition for children with dysentery
A therapeutic diet is very important for this disease. In the acute phase, food fasting is recommended. In the first days of infection, the child is allowed to drink tea or water for 12 hours. If the baby is of normal weight, then fasting is extended to a day. Then they gradually begin to give permitted food products:
- steamed fish and meat;
- vegetable and fruit puree;
- porridge cooked without adding milk;
- vegetable soups;
- Introduce fermented milk products very carefully, monitoring the child’s condition.
If the baby is breastfed, then the mother must follow the diet. The volume of fluid consumed for the entire period of therapy is almost doubled. It is recommended to avoid legumes, raw vegetables and fruits, fresh milk, wheat and rye bread.
General information about the disease
The causative agent of dysentery in adults is various types of dysentery bacillus. The pathology is easily confused with other, less dangerous gastrointestinal diseases. Most often, Sonne and Flexner microorganisms are found in patients. Such bacteria inhabit the folds of the colon.
The microorganism enters the external environment in the form of cysts. The sick person is considered a carrier of the pathology. The highest percentage of dysentery patients is registered in cities with low sanitary standards of the population.
Penetrating into the body of an adult, some of the dysentery pathogens die. The remaining microorganisms are transported into the intestinal tract and contribute to the formation of the disease. Parasites leave waste products in the body. The substances are toxic and cause intoxication.
Dysentery can be difficult to treat in older people
Dysentery occurs worst in older adults. In this case, the body is not able to cope with pathogenic microorganisms. Treatment should begin immediately.
Dysentery in children and adults is accompanied by inflammatory processes in the gastrointestinal tract. When it becomes chronic, negative symptoms may completely disappear. Treatment of such a disease will be difficult.
Shigella bacterium
Gram-negative bacilli are the root cause of widespread dysentery. The immobile rod, also known as the Shigella bacterium, is quite tenacious:
- The dysentery bacillus can withstand heating temperatures up to +60C for ten minutes;
- When exposed to sunlight, Shigella lives for half an hour. She is not afraid of low temperatures, she can exist at -160C;
- In dairy products or on unwashed vegetables and fruits, its lifespan is two weeks;
- Enterobacteriaceae are not afraid of gastric acid, so they thrive in that environment.
Despite such vitality of Shigella. They also have their own characteristics. Let's look at them:
- Inability to exist in capsule form or spores;
- Easy and rapid reproduction in a simple environment;
- The severity of the disease depends on the type of bacilli. The most dangerous of them are the stationary Grigoriev-Shiga sticks;
- Easy tolerance to drought and extreme cold;
- Dies from boiling and treatment with disinfectants.
Popular Six ways an adult can catch rotavirus
Shigella is a dysentery bacteria that has several stages of disease development, and various pathogens with their own abilities and structure. Let's get acquainted with the most basic of them.
| № | Name | Features of the species |
| 1. | Shigella Sonne. | Over the past decades, due to the Sonne pathogen, dysentery has spread throughout the CIS countries. Most often they are found in dairy products, so it is recommended to boil the milk after purchase. |
| 2. | Shigella Flexner. | Due to Shigella subspecies Flexneri, dysentery was rampant in America and Africa in the middle of the last century. Today this species is found in these areas. |
| 3. | Shigella Grigorieva-Shigi. | This dysentery bacillus is considered one of the most dangerous bacilli of the disease, as it leaves behind the most serious complications. The Grigoriev-Shiga rod produces a neurotoxin. Today it is sown both in the CIS countries and in European countries. |
| 4. | Shigella Body. | This subspecies is the root cause of dysentery. |
| 5. | Dysenteric amoeba. | The reason for the development of this type of Shigella is the types of protozoan microorganisms. An amoeba infection is capable of thoroughly destroying its walls once it gets into the human stomach. This virus has much in common with dysentery, hence its name. |
When harmful, sedentary bacilli enter the body, they not only cause poisoning, but also fundamentally spoil the normal functioning of the microflora. During Shigella activity, other pathogenic microorganisms also begin to become active. As a result, the balance is disrupted and the digestive tract malfunctions.
Carriers of bacilli can be insects and flies that have direct contact with the environment. People can infect each other through contact and household contacts. Infection can occur due to poor personal hygiene and unwashed fruits. For the disease to begin to progress, 200-300 viable Shigella are enough for the body.
Shigella dysentery
Sh infection Dysenteriae was the main cause of bacillary dysentery at the beginning of the last century. Now Shigella dysentery has lost first place, and has been overtaken in the championship by two other species - Shigella Sonne and Flexner. Most often they can be found where there are large crowds of people, for example, in prison cells.
Dysentery infections occur through the mouth or they are excreted in feces. After entering the gastric juice, some of the Shigella die, releasing endotoxin, which poisons the body. The remaining enterobacteria enter the colon, where they conduct their life activities. Ulcers may form in the stomach.
In case of household contact infection, the disease can develop under the following conditions:
- when shaking hands with a sick person;
- with unwashed hands after coming from the street or toilet.
- products can be contaminated by flies and insects that carry microparticles of contaminated feces.
Dysentery outbreaks may increase more if an infected person, for example, works in a kitchen where food is prepared for a large number of people. Therefore, collective diseases of shigellosis are more often observed in industrial canteens, kindergartens and school institutions. When swimming in open waters, you can also easily pick up a dysentery bacillus, where there are a lot of bacilli carriers.
Shiga exotoxin was identified by a Japanese microbiologist, after whom this type of Shigella was named. Serotype I is capable of having the following effects on the body:
- poisoning of the body with varying degrees of severity;
- damage occurs to the central nervous system and the walls of blood vessels;
- negative manifestations also affect the peripheral nerve ganglia;
- the liver and other vital organs are affected.
Symptoms of the disease and diagnosis
Shigella can remain outside the human body for quite a long time. After infection, a person will not feel any symptoms for some time, as the incubation period of the disease begins. Usually it ranges from two days to a week. This time is influenced by the state of a person’s immunity. The stronger it is, the longer it will take for bacteria to take root in the body.
If symptoms appear, it is very important to visit a doctor immediately to begin the necessary treatment. The sooner it begins, the less harm will be caused to the body and the easier it will be to get rid of the consequences of the disease.
The primary symptoms of intestinal dysentery include:
- intoxication;
- low blood pressure;
- pain in the peritoneal area.
The patient's temperature rises sharply, he feels severe weakness and dizziness, chills and exhaustion. Abdominal pain is different from normal illness. First, a person feels a dull pain in the peritoneum, which gradually gives way to a stabbing pain. The localization of pain also gradually shifts to the lower left part of the abdomen. If the patient needs to empty his bowels, then this pain intensifies.
Other symptoms of the disease may vary depending on its form. With mild dysentery, all symptoms are mild and blurred. They manifest themselves clearly and can be mistaken by a person for a simple malaise.
In some cases, pain may occur during bowel movements or the urge to defecate. The illness in this case lasts from several hours to two days.
Moderate dysentery is accompanied by a high fever, which usually lasts for several days. Abdominal pain now occurs not only before bowel movements, but also at other times. They have a cramping character. The urge to defecate is quite frequent. A person can visit the toilet up to 20 times a day.
In this case, the feces are liquid and have various impurities:
- slime;
- blood;
- pus.
The patient feels weak, his skin is pale, and a whitish coating may be visible on the tongue. This condition can last for a week. Moreover, complete restoration of the intestinal mucosa with proper treatment will occur only after 2 months.
A severe form of dysentery is accompanied by a very high body temperature - up to 40 degrees. The person feels severe weakness and lack of appetite. He regularly experiences attacks of nausea, vomiting, and also has hiccups and diarrhea. In this form, the disease can last up to 10 days. In this case, recovery will be very slow and difficult. Complete regeneration of the intestinal mucosa can only occur after two months or even more.
In some cases, a severe form of the disease can develop into a more severe form. In this case, in addition to diarrhea, the patient experiences various kinds of systemic pathologies (heart failure, problems with other internal organs).
If dysentery is not treated, the disease can become chronic. Its symptoms will last for months, and remissions will be short-term.
Only a doctor can diagnose dysentery. He does this based on the symptoms and complaints from the patient. To make an accurate diagnosis, studies such as:
- blood analysis;
- Analysis of urine;
- serological study;
- stool examination.
A blood test will show an increased number of white blood cells, and proteins, red blood cells, and casts may be detected in the urine. Antibodies and antigens of dysentery bacteria are present in the blood.
When examining stool, three types of tests are performed:
- microscopic;
- bacteriological;
- scatological.
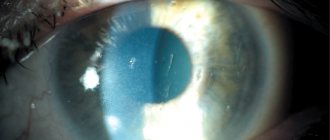
If necessary, the doctor may also prescribe a sigmoidoscopy. Using this procedure, you can examine the mucous membrane of the rectum and colon and identify the presence of erosions, swelling and redness.
After dysentery, a person develops immunity for several weeks, protecting him from re-infection. But after a month he disappears.
How is the infection transmitted?
The predominant route of transmission of Shigella is through household contact and food. Water transmission is of less importance. The source of shigellosis is a person with varying degrees of clinical symptoms. The greatest danger to others is not even a sick person (he is isolated and receiving the necessary treatment), but a patient with erased clinical symptoms and a bacteria excretor.
A patient with erased (moderately severe) clinical symptoms may not pay due attention to his health and may be treated independently, which does not always allow Shigella to be completely destroyed.
The bacteria excretor does not feel any discomfort, and therefore maintains a normal lifestyle, infecting a large number of surrounding healthy people. This condition can last for weeks or even months. It is especially dangerous if such a bacteria excretor, by the nature of his professional activity, is engaged in the preparation and dispensing of food (kitchen worker, distributor, barmaid), transportation, storage and sale of food products, in particular those that are not subject to subsequent heat treatment (baked goods, salads, dairy products). products).
We recommend reading:
How does dehydration manifest during diarrhea and how to treat the pathology?
Shigellosis infection is possible in the following ways:
- in direct contact with a sick person (in the family, when caring for a patient);
- when visiting a cafe or buffet where a bacteria-isolating employee works;
- when consuming contaminated food (poorly washed vegetables and fruits, etc.);
- non-compliance with the rules of sanitation and hygiene in the process of gardening work, on a tourist trip.
Susceptibility to shigellosis is equally high in all age groups, but children are most often affected. An important feature of shigellosis is the formation of type-specific immunity. A person experiences illness caused by one variant of Shigella, but this does not protect him from infection and development of clinical symptoms caused by another variant of Shigella.
Phases of shigellosis
Signs of dysentery caused by shigellosis are formed due to two phases of the inflammatory process.
Initial
The factors of natural resistance of the body are of primary importance:
- the presence of lysozyme in saliva and mucus;
- hydrochloric acid of gastric juice;
- condition of the intestinal wall;
- activity of the intestinal flora (the causative agent of dysentery is exposed to other intestinal bacteria).
Depending on these factors, the following options are possible:
- the invading dysentery pathogens are destroyed by natural defense factors, the disease is absent;
- pathogenic microbes bypass the intestines without causing changes and enter the external environment (transient bacterial carriage is formed in a similar way);
- Penetrating into the wall of the final section of the small intestine, microorganisms release toxins and cause inflammation and intoxication.
With the latter option, the development and severity of shigellosis symptoms depends on the massiveness of the received dose of cells. If the patient receives quite a lot of Shigella from food, then the clinical picture of dysentery is caused by an “explosion” of toxin release and is accompanied by the shortest incubation period, vivid manifestations of intoxication, and a predominance of symptoms of damage to the stomach and small intestine (gastritis, gastroenteritis).
The phase lasts up to three days. Self-destruction of pathogenic bacteria or spread to the large intestine is then possible.
Subsequent (second)
How large the area of damage to the large intestine is depends on the patient’s defenses. With immunodeficiency, the entire intestine is involved in inflammation. Shigella penetrates the epithelial cells, multiplies in them and destroys structures, forming areas with necrotic tissue.
Grigoriev-Shiga dysentery is accompanied by the penetration of pathogens into the lymphatic vessels and nodes. But more often, only a local inflammatory process remains and does not cause spread throughout the body.
Due to the effect of toxins on lymph and blood circulation, damage to the nerve plexuses of the intestine, pain syndrome and frequent loose stools are formed.
The pain differs in nature depending on the type of damage to the muscle fibers. When the circular muscles contract, the upper sections of the intestine become overcrowded, and the underlying ones become empty, the pain is of the nature of spasms, false urges, little feces are excreted, the contents of the stool are mucus and inflammatory products.
If the longitudinal muscles contract, the pain is longer, more painful, and false urges do not go away after defecation. Defects in the mucous membrane are caused by disturbances in protein synthesis during dysentery and increased desquamation of the epithelium. The overall effect of toxins contributes to:
- development of intoxication (in severe cases up to toxic shock), toxins are carried by blood to organs and tissues, causing overirritation of the centers of autonomic innervation in the brain, at the level of the abdominal nodes, segments of the spinal cord;
- inhibition of the sympathoadrenal system of the adrenal glands occurs, the predominant action of the vagus nerve creates conditions for a drop in pressure and frequent bowel movements;
- due to dysfunction of digestion and kidneys, all types of metabolism change, water and electrolytes are lost to the point of dehydration, a lack of vitamins, proteins and carbohydrates provokes a disruption in the absorption of oxygen by cells and energy synthesis.
In severe cases of dysentery, the intestinal wall is destroyed, and the body is additionally poisoned by necrotic tissues. Patients lose a significant amount of protein. The capillaries around the site of inflammation become thrombosed, further impairing the nutrition of the muscle layer.
Paresis (immobility) develops. Conditions for intestinal perforation appear. Due to a violation of the flora, a person develops secondary immunodeficiency. Particular importance in the development of dysentery is attached to autoimmune processes. Restructuring in response to antigen toxins causes the formation of antibodies to the colon epithelium.
The process reaches its maximum in the second week of illness. Increased release of histamine, acetylcholine, and serotonin into the blood further aggravates inflammation. Allergization is higher in patients prone to transition to chronic dysentery.
How to distinguish the symptoms of dysentery from other stomach disorders?
Since the main symptoms of dysentery are disturbances in the functioning of the gastrointestinal tract, it is easy to confuse it with certain diseases.
Amoebiasis
Amebiasis is an intestinal infection. It got its name from the pathogen - amoeba.
Since it is a type of dysentery, both diseases are characterized by the same symptoms:
- diarrhea mixed with mucus or blood, the frequency of which reaches 4-6 times per day, and in severe cases 10-20 times;
- acute pain in the lower abdomen, intensifying during bowel movements;
- moderately severe intoxication syndrome (lethargy, slight increase in temperature, dizziness);
- in severe form, formation of erosions and ulcers in the intestines is possible.
The symptoms of amebiasis differ from shigellosis only in the absence of their sharp manifestation (acute short-term fever with a sharp increase in temperature). Only with the help of bacteriological and laboratory tests can intestinal infection be differentiated.
Toxic infections in products, salmonellosis
These diseases are also characterized by damage to the digestive system and general intoxication of the body, which is accompanied by symptoms such as nausea, vomiting, and frequent loose stools.
A clear difference from dysentery will be the absence of tenesmus (false urge to have a bowel movement) and pain in the sigmoid colon. With salmonellosis, signs of intoxication of the body are clearly expressed, and the stool acquires a greenish tint with a fetid odor.
Typhoid fever
Typhoid fever is characterized by spastic colitis (irritable bowel syndrome), which causes cramping, gas formation, alternating diarrhea and constipation.
Body temperature rises for a long period of time.
Cholera
Cholera is characterized by the presence of copious watery stools without pathological changes or impurities. Signs of poisoning of the body are weakly expressed. Rapid dehydration occurs, resulting in severe thirst and dry skin.
Colitis
The main distinguishing feature of this disease is that colitis is not of infectious origin, and therefore is not contagious. The symptoms are the same as for dysentery. The only difference in symptoms is that the feces have a distinct fetid odor, gas formation is disturbing, and in some cases, acidic stool occurs. Also, against the background of colitis, dysbacteriosis always develops.
Colon cancer
Oncological diseases, as a rule, occur without visible signs. In severe form they have metastases.
Symptoms of the disease, such as bloody feces or toxicosis, appear with an advanced form of intestinal cancer.
Haemorrhoids
Hemorrhoids are manifested by noticeable pain during bowel movements, itching in the anus, and prolapse of nodes. This is a non-infectious disease.
Features of dysentery in children
In 90% of cases, babies under one year of age develop colitis of varying severity, occurring together with a disorder of the digestive system. There may be no loose stools, but the discharge contains remnants of unprocessed food, greenish and bloody inclusions, and mucus. In contrast to the symptoms of dysentery in children 2 years of age and older, infants have a swollen stomach and discomfort during bowel movements. A feature of the disease at this age is the undulating course of dysentery, that is, with relapses and exacerbations. Repeated infection increases clinical manifestations. Compromised immunity is considered a prerequisite for the development of other intestinal infections caused by rotavirus, staphylococcus, and amoebas. The pathology provokes pneumonia over a long period of time.
Symptoms of dysentery in children 2 years of age lead to rapid dehydration of the body, which results in:
- heart rhythm disturbance;
- clouding of mind;
- renal failure;
- weight loss;
- fatal outcome.
It is important to seek qualified medical help at the first symptoms of the disease.
Diagnosis of dysentery
Symptoms of dysentery can tell an adult about his infection, but only an infectious disease doctor should confirm the diagnosis and select the correct treatment.
Shigellosis is determined by collecting the patient's medical history and undergoing a series of clinical tests:
- General blood test.
- Coprograms (stool analysis).
- Bacteriological culture of stool for pathogenic intestinal flora.
- Laboratory research.
- Sigmoidoscopy.
If there are any abnormalities or inflammatory processes in the body, a general blood test will show this.
Some indicators will be increased:
- leukocytes;
- neutrophils;
- monocytes;
- ESR.
Thus, blood test data will help to exclude diseases of a cardiac nature and neurology. Thanks to this study, malfunctions in the systemic functioning of the entire body are visible, and possible risks and complications are identified.
Fecal analysis (coprogram) allows you to see inflammatory processes and deterioration of the digestive organs, as well as ulcerative and spastic colitis (inflammation of the colon, accompanied by spasms), which will help the doctor choose the right treatment method.
Bacteriological culture of stool for pathogenic intestinal microflora will help identify the cause of malfunctions in the body
This analysis is a very important study, since it allows not only to diagnose the presence of Shigella, but also to determine their variety. And most importantly, it will help determine the sensitivity of dysentery bacilli to antibiotics
All of the above studies are only 80% reliable, so they are prescribed in aggregate. However, the most effective method for determining infectious diseases in medicine is considered to be serological diagnosis, in which antibodies and antigens in the patient’s blood are studied in the laboratory.
It is the response of his body to foreign objects, including bacteria, that gives the right to make an accurate diagnosis with an almost 100% guarantee. In practice, IRHA (indirect hemagglutination reaction) is widely used, in which a medical worker introduces Shigella antigens into the patient’s blood and monitors the reactions of immune system cells to them using a microscope.
To diagnose erased and asymptomatic forms of dysentery, sigmoidoscopy will be effective. This procedure is very unpleasant for many patients, because a rectoscope (a device that is a thin tube equipped with an eyepiece and an air supply device) is inserted into the intestines through the anus.
Thanks to this research technique, the doctor is able to see a full picture of the course of the infection and detect erosions, ulcers and hemorrhages. The procedure itself does not require any preparation, is safe, and most importantly, painless, although it is accompanied by unpleasant sensations.
Prevention
Specific prevention of shigellosis can be carried out using a vaccine or bacteriophage. Immunity after such events is short-lived and relaxed, that is, there is no 100% protection. Shigellosis is effectively prevented by sanitary and hygienic measures:
- you need to wash your hands;
- wash vegetables and fruits thoroughly;
- follow food preparation rules;
- on tourist trips to hot countries, drink only boiled water.
Read more: Measures to prevent intestinal infections
Shigellosis is a disease with a favorable outcome if you consult a doctor in time and follow all his recommendations.
In continuation of the topic, be sure to read:
- The most common infectious bowel diseases
- Escherichiosis: details about the infectious disease
- Details about typhoid fever: symptoms, characteristics of the pathogen, analysis and treatment
- How is rotavirus intestinal infection manifested and treated?
- Intestinal flu: symptoms and treatment in adults
- Details about dysbiosis and methods of its treatment (diet, medications)
- Proctitis: symptoms and treatment methods (diet, drugs, surgery)
- Intestinal infection: symptoms and treatment methods (diet, medications)
- Intestinal dysbiosis in children: symptoms and treatment (diet, medications)
- Intestinal tuberculosis: first signs, diagnosis and treatment
Diagnosis and treatment features
In this case, the pathogen is determined by the state of the patient’s stool. Some express methods are used, in particular, immunofluorescence analysis and some others, which are prescribed individually each time. Another method of processing feces is used, according to which blood streaks are identified in feces - they indicate damage to the intestinal mucosa and explain all the negative symptoms.
Another stage of diagnosis is sigmoidoscopy, which identifies certain signs that reveal the presence of inflammatory algorithms in the final sections of the large intestine. As a result, after the presented examination, a rehabilitation course can begin. It is strongly recommended not to carry it out at home and not to follow folk or other non-professional recipes. In this case, there is a high probability of complications and other negative consequences.
During the treatment of dysentery, a special role should be given to diet. It is necessary to exclude foods that are rich in plant fiber from your regular diet, because it irritates the intestinal area. Food must be served boiled or pureed. It is highly recommended to consume soups, cereals (cooked exclusively in water), soufflés and meatballs
At the same time, it is very important that the amount of food consumed increases when single servings of a particular dish are reduced
Considering the seriousness of the changes that have occurred as a result of dysentery, it is necessary to adhere to the specified diet for several weeks or even a month after the onset of recovery. In some cases, antimicrobial drugs are used, which are effective in moderate and severe forms.
It is this that makes it possible to stabilize the water and salt balance.
In cases where dysentery continues for a long time, experts recommend the use of medicinal components that improve the general state of the immune system. This is what will make it possible to restore all body functions in the shortest possible time.
It is very important to restore normal intestinal microflora during treatment for dysentery. For this purpose, some bacterial components are used, namely Bifikol, Bifidumbacterin
If there is a suspicion of the development of an epidemic or subsequent worsening of the condition, it is necessary to take care of placing the patient in a hospital. It should be noted that it is the elderly who suffer the most from dysentery. In addition, their body is the slowest to recover subsequently, and therefore it is they who are strongly recommended to monitor personal hygiene and the cleanliness of the food they eat. It is in this case that it will be possible to exclude the development of complications and other critical consequences that negatively affect the functioning of the body and the gastrointestinal tract.
Important! HOW TO SIGNIFICANTLY REDUCE THE RISK OF CANCER?
Time limit:
Navigation (job numbers only)
out of 9 tasks completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
Information
TAKE THE FREE TEST! Thanks to detailed answers to all questions at the end of the test, you can REDUCE the likelihood of disease by several times!
You have already taken the test before. You can't start it again.
The test is loading...
You must log in or register in order to begin the test.
You must complete the following tests to start this one:
results
Time is over
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- With answer
- With a viewing mark
- 1.
Can cancer be prevented?
- Yes
No
- you can only reduce the risk
- 2.
How does smoking affect the development of cancer?
- promotes
does not contribute
- smoke don't smoke, nothing will happen
- I find it difficult to answer
- 3.
Does excess weight affect the development of cancer?
- has no effect
yes, it does
- Being overweight has nothing to do with cancer at all.
- 4.
Does exercise help reduce the risk of cancer?
- yes, sport kills cancer cells
No
- I find it difficult to answer
- 5.
How does alcohol affect cancer cells?
- promotes development
no way, alcohol only kills the liver
- it is beneficial and helps destroy cancer cells
- 6.
Which cabbage helps fight cancer?
- broccoli
hare or wood sorrel
- cabbage white
- 7.
Red meat affects which organ cancer?
- rectum
stomach
- gallbladder
- 8.
Which of the proposed remedies protect against skin cancer?
- regular baby moisturizing cream
sunscreen
- honey
- 9.
Do you think stress affects the development of cancer?
- Yes
no, they just kill the nervous system
- I find it difficult to answer
Complications and preventive measures
The consequences of the disease appear with untimely and improper treatment. The most common are:
- pneumonia;
- anemia;
- peritonitis;
- pericolitis;
- rectal prolapse;
- intestinal bleeding;
- malnutrition.
The most effective method of prevention is teaching your child:
- observe the rules of personal hygiene;
- do not put your hands to your mouth;
- do not suck fingers;
- Wash your hands before eating.
These simple rules will protect your child from contracting dysentery.
Forms of dysentery and variants of its course
Based on the clinical features of the disease in question, as well as its duration, the following variants and forms can be determined:
- Acute dysentery: colitic typical dysentery;
- atypical dysentery (it, in turn, can be gastroenterocolitic and gastroenteric);
- continuous chronic dysentery;
In addition to these types of dysentery, its course can also be characterized by a factor in the form of shigella bacterial excretion, which, in turn, can be subclinical or convalescent.
The indicated variants of the disease depend directly on a number of concomitant causes, which in particular include the initial condition of the patient, the time frame within which treatment began from the onset of the disease, the nature of therapy, etc.
The specific type of pathogen that provoked dysentery also plays a certain role. For example, if we are talking about dysentery provoked by Shigella Sonne, then its course is usually characterized by a mild, or even completely erased, atypical form, which, in turn, excludes the possibility of developing destructive changes in the intestines. Also, the disease in this case is characterized by the short duration of its course and the correspondence of the symptoms to the gastroenteritis or gastoenterocolitic variants of the forms.
If we are talking about a disease provoked by Shigella Flexner, then most often there is a typical colitic variant of the course, characterized by severe damage to the colon mucosa and no less pronounced concomitant symptoms. By the way, over the past few years, it is this option that has been responsible for cases of subsequent development of severe forms of dysentery with the appearance of a number of complications.
With dysentery provoked by Shigella Grigoriev-Shiga, it is appropriate to talk about the severity of its course, as well as the tendency to such serious conditions as severe dehydration (dehydration), infectious-toxic shock, and sepsis.
Complications and preventive measures
The ineffectiveness of therapy, as well as the lack of treatment for the symptoms of dysentery in adults and children, provoke dangerous consequences:
- expansion of the colon, leading to death;
- sepsis;
- ulcerative lesions of the intestinal mucosa, which provoke bleeding;
- hemolytic-uremic syndrome.
Preventive measures are personal hygiene. Wash your hands after visiting the toilet, public places, walking, and before eating. Thorough processing of products before consumption. If someone in the family is sick with dysentery, then disinfection of the premises is mandatory.
External signs
The following stages of dysentery can be distinguished: incubation period, peak of the disease, stage of decreasing intensity of symptoms and complete recovery.
The initial stage of the disease is associated with an incubation period, which can last from several hours to 7 days. It all depends on how many bacteria have entered the body.
The peak of the disease is associated with acute manifestations and deterioration of the condition. Flexner's dysentery is the most difficult to tolerate. Recovery occurs by the end of the second week, but subject to proper treatment. Complete recovery of the body can take up to 2 months. Even after the condition improves, the person remains a carrier of the infection.
The main symptoms of dysentery are the following:
- a rise in body temperature to high levels (above 39 degrees), the body feels hot and chilly;
- a person complains of weakness, weakness;
- pain in the head, left side of the abdomen;
- in most cases, blood pressure decreases;
- heart rhythm is disturbed.
The first signs of dysentery look like this:
- an adult patient has a frequent urge to defecate, which is accompanied by severe abdominal pain;
- during illness, dry mouth is felt;
- presence of attacks of false urge to defecate;
- no appetite;
- nausea leading to vomiting.
The nature of stool in dysentery varies depending on the stage of the disease. The stool becomes thinner as it approaches the acute period. The color of the stool is greenish interspersed with blood and mucus. The frequency of loose stools reaches 17 times per day.
Dysentery during pregnancy leads to serious complications. The pathology is dangerous for both the woman and the fetus. The risk of premature birth or miscarriage increases due to increased contraction of uterine tone. The woman experiences an increase in temperature, severe weakness, constant nausea, and repeated vomiting.
How does the infection spread to the child? The baby can become infected during childbirth, there is a high risk of intrauterine infection of the fetus, so treatment is carried out only within the walls of a hospital using gentle medications.