No specialist will give you a definite answer to the question of whether people with gastritis are recruited into the army. The reason is the specificity of the disease, which is characterized by the presence of many forms.
A conscript diagnosed with gastritis or chronic duodenitis may receive one of the following fitness categories:
- Category "B". The form of the disease does not exempt one from military service; it imposes restrictions on the choice of type of military service.
- Category "B". The young man is exempt from conscription in peacetime and is enlisted in the reserves.
- Category "G". The commission grants a deferment for undergoing treatment and rehabilitation measures.
The category is determined by a medical commission at the military registration and enlistment office, which makes a decision on the basis of documents received from medical institutions: certificates, test results and examinations.
Chronic gastritis and the army: suitability categories
With different manifestations of gastritis, a conscript may receive a fitness category of “B”, “C” or “D”. The exact answer to the question “whether someone with chronic gastritis will be accepted into the army” will depend on three factors: the frequency of exacerbations, the effectiveness of treatment and the presence of a medical history.
Table 1. Gastritis and suitability categories
| Gastritis | Suitability category |
| Chronic with rare attacks. | "B" |
| Chronic gastritis with impaired secretory and acid-forming functions, frequent exacerbations and malnutrition (BMI 18.5 - 19.0 or less), requiring repeated and prolonged hospitalization (more than 2 months) if inpatient treatment is unsuccessful. | "IN" |
| Chronic gastritis in acute form with disruption of certain gastrointestinal functions, requiring urgent treatment. | "G" |
In most cases, chronic gastritis does not exempt you from the army. This is a common disease that occurs with rare exacerbations caused by eating fatty or spicy foods, lack of diet or bad habits. In military units, the daily routine is strictly regulated and the diet is balanced, which is why conscripts diagnosed with “chronic gastritis” are taken into the army. Moreover, for them the service is even preferable.
Exemption from the army for gastritis is granted to conscripts who:
- consult a doctor with complaints of exacerbation more than 2 times a year;
- forced to undergo long-term treatment in a hospital (at least 2 months in total for 1 year);
- are underweight (BMI less than 19.0);
- have proven gastric dysfunction.
Our clients do not serve in the military
call me back
Get a free consultation by phone:
8 (800) 511-94-97
or request a call back
The more evidence you can collect of the severity of the illness, the more likely the commission will assign fitness category “B”. An important factor in determining suitability is whether the conscript has medical documents indicating that he visited a doctor and the duration of treatment. If there are no such documents, the conscript may be refused referral for additional examination and issued a summons for dispatch.
Advice from the Recruit Assistance Service
The category of suitability for gastritis largely depends on the conclusion of the doctor responsible for the additional examination. It is important to ensure that all studies are carried out without violations, and the records of the gastroenterologist in the direction from the military registration and enlistment office are similar to those indicated in the Schedule of Diseases.
Causes of the condition and types of pathology
Most often, gastroduodenitis is caused not by one, but by a combination of reasons.
The first link in the development of this disease is infection of the body with the bacterium Helicobacter pilory, and its further development is determined by the following points:
- irregular meals;
- frequent stress;
- abuse of spicy and fatty foods;
- constant nervousness;
- drinking alcohol and smoking.
And this is just a number of factors that provoke the emergence and development of this unpleasant disease. The circle of development of the pathological condition is closed by the fact that against the backdrop of stress and constant haste, people do not think about what they eat and how they eat it.
The main directions of the course of gastroduodenitis are:
- Spicy.
- Chronic.
- Aggravated.
The chronic form of the disease emerges from the acute form, which was not treated or treated incorrectly. However, there are cases when its occurrence bypasses such a stage of development as the acute form, and further deterioration of the condition is observed after a certain amount of time.
For a number of reasons, the bacterium begins to develop, increasing in number, irritating the mucous membrane of the gastrointestinal tract (gastrointestinal tract) to such an extent that ulcers begin to appear on it. Well, they, in turn, irritated by gastric juice, give painful sensations that periodically greatly disturb the patient. Is it possible to serve in such a state?
Erosive gastritis and the army
With erosive gastritis, erosions appear on the gastric mucosa - wounds, severe abdominal pain and vomiting occur. In case of exacerbation, the patient requires treatment in a hospital and adherence to a strict diet, therefore people with erosive gastritis are not accepted into the army.
The exemption from conscription will be temporary. If the gastroenterologist confirms the diagnosis after an additional examination, the military registration and enlistment office will grant the young man a deferment for the duration of treatment, but not more than 6 months. After its completion, the conscript will again receive a summons for a medical examination.
Erosive gastritis can cause stomach ulcers and internal bleeding. If such complications develop, the young man has the right to be released from service and enlisted in the reserves.
Expert opinion
Be sure to check out the “Practice” section. We tell you what problems you may encounter when confirming a diagnosis and how to get a military ID card for health reasons.
Ekaterina Mikheeva, head of the legal department of the Assistance Service for Conscripts
Symptoms of the disease
In chronic gastroduodenitis, symptoms are caused by digestive disorders and changes in the state of the nervous system. The patient experiences the following phenomena:
- abdominal pain mainly in the epigastrium, which occurs 1.5-2 hours after eating;
- bloating, rumbling in the stomach;
- poor appetite;
- nausea, sometimes vomiting, frequent sour belching;
- unstable stool with alternating diarrhea and constipation;
- yellowish or grayish coating, teeth marks on the tongue;
- unpleasant taste in the mouth;
- weight loss;
- pale skin;
- sweating;
- irritability.
With atrophic gastroduodenitis, there may be heaviness, distension in the abdomen, belching of air, and rapid saturation. The pain usually has a dull, aching character, and there is a clear connection with food intake. The patient may complain of irritability and sleep disturbances. With exacerbations of gastroduodenitis, the symptoms become more pronounced, and the patient’s ability to work is significantly impaired. During remissions, some manifestations remain, but their intensity weakens.
Chronic gastroduodenitis in children is characterized by a wide variety of symptoms. The duodenum has an endocrine function, so children more often have symptoms of vegetative-vascular dystonia. The child may be bothered by headaches, periodic dizziness, sleep disturbances, increased fatigue, and lethargy.
1.5 hours after eating, weakness, sweating, and increased intestinal motility often appear. Symptoms of hypoglycemia are sometimes observed: trembling, muscle weakness, dizziness. Isolated gastritis or duodenitis is rare in children; usually the inflammatory process immediately affects both the stomach and duodenum.
Treatment of this disease includes several components:
- drug therapy,
- diet,
- mode,
- psychotherapy.
The choice of medications depends on the type and causes of gastroduodenitis. If the examination reveals a Helicobacter pylori infection, then antibiotic therapy is carried out. Usually a combination of 2-3 antibiotics is used. For chronic gastroduodenitis with high acidity, proton pump inhibitors, antacids and antihistamines are used.
Proper nutrition is of utmost importance for gastroduodenitis. During remission, it is necessary to exclude the following foods from the diet:
- fatty meat, poultry and fish;
- spicy dishes (mustard, pepper, horseradish, garlic, etc.);
- strong coffee and tea;
- alcohol;
- strong broths;
- marinades, smoked meats, etc.
The basis of nutrition should be soups (with a second broth), lean meat, poultry, lean fish, cereals, vegetables and fruits. Products can be boiled, stewed, steamed or baked. In case of chronic gastroduodenitis in the acute stage, nutrition should be mechanically, chemically and thermally gentle. You can prepare liquid milk porridges, pureed soups with vegetable or weak meat broth, jelly, and compote. All dishes should be eaten warm.
You should adhere to a certain regime. Adequate sleep and rest, frequent walks, and normal physical activity are necessary.
For chronic gastroduodenitis, treatment with folk remedies can be carried out simultaneously with taking the medications prescribed by the doctor. You can also use folk recipes to prevent exacerbation of the disease. Find more information on this issue, as well as effective recipes, in the article: The healing power of folk remedies against gastroduodenitis.
The etiological factor is the basis for the classification of gastroduodenitis:
- primary (exogenous);
- secondary (endogenous).
Depending on the prevalence, they are classified into localized and widespread. The acidity level is an indicator for dividing gastroduodenitis into the following categories according to the state of secretory function:
- normal;
- reduced;
- increased.
There are several causes of inflammatory disease, which are divided into two groups:
- endogenous;
- exogenous.
Endogenous causes are the basis for focusing on acid formation, disruptions in hormonal regulation of secretion, and a decrease in the level of mucus formation. A predisposition to gastroduodenitis is observed in patients with the following diagnoses:
- diseases of the biliary tract and liver;
- endocrine pathology.
The most common exogenous etiological factors influencing the development of gastroduodenitis are:
- eating cold or hot, spicy food;
- chemical (exposure to pesticides);
- penetration of the bacterium Helicobacter pylori into the body.
Gastroduodenitis requires selection of a treatment regimen
The result of the influence of pathological etiological factors on the duodenal mucosa of the stomach is an inflammatory reaction, which is the initial stage of physiological regeneration of the mucosa, followed by atrophy.
The above factors inevitably lead to disruption of the full functioning of secretory and motor functions. In practice, it has been noted that in most cases the inflammatory disease is accompanied by duodenal dyskinesia, increased motility and tone of the stomach.
Changes in the structure of the mucous membrane are accompanied by corresponding symptoms; in addition, the manifestation of symptoms is influenced by the condition of the stomach and metabolic disorders. Characteristic symptoms that appear at all stages of the disease are lethargy, insomnia, pallor, weakness, and vitamin deficiency. Depending on the level of metabolic disorder, the above symptoms appear.
To achieve positive results in the treatment of gastroduodenitis, you need to be patient and consistently follow the doctor’s prescriptions. You should definitely adhere to the physical and nutritional regime, diet, take antacid drugs (Vicalin, Almagel), drugs that stimulate reparative processes, depending on the specific characteristics of the disease - mineral water, multivitamins, sedatives and antispasmodics.
Ideally, it is recommended to carry out comprehensive treatment of diseases of the digestive system.
- Puree soups, based on fish, mushroom and meat with the addition of vegetables and cereals.
- Lean meats: boiled chicken, beef, rabbit; steamed and stewed cutlets, lean ham, lean herring (carefully soaked).
- Fermented milk products, low-fat milk, sour cream, mild cheeses.
- Soft-boiled eggs, mashed omelette and well-cooked porridge, flour dishes, with the exception of baked goods.
- Fruits, vegetables (raw, boiled), juices, coffee, tea, cocoa.
- The permissible amount of salt is within 12-15 g. It is recommended to take vitamins C, B1, B2, PP.
- Five meals a day.
Drinks and food should be warm, not hot or cold. Eating solid food is strictly prohibited; foods must be chewed thoroughly. Ideally, food should be divided into several small portions. Considering that chronic gastroduodenitis has distinctive features, compared with alternating exacerbations with periods of remission - the cyclical course of the disease, it is necessary to adhere to the following principles:
- during an exacerbation, the patient must remain in bed for an average of 7-8 days; A prerequisite is compliance with a special diet; in practice, it has been confirmed that proper nutrition can significantly speed up the treatment process and reduce pain.
- In order to neutralize Heliobacter Pilori, it is recommended to carry out drug therapy, including bismuth tripotassium dicitrate, macrolide, amoxicillin. Depending on the individual characteristics of the patient’s condition, the treatment course takes 7–10 days; to combat increased stomach acidity, H2-blockers of histamine receptors and omeprazole are prescribed;
- In practice, the effectiveness of physiotherapy has been proven, positive results will not take long, in addition, if possible, you should attend exercise therapy and undergo sanitary-resort treatment.
Festive meat pudding
1. metronidazole and de-nol (on average, the duration of treatment ranges from 10-14 days), tetracycline antibiotics (on average, the course of treatment is 7-10 days); 2. omeprazole and clarithromycin and supplemented with metronidazole (on average, the course of treatment is 7 days); 3. amoxicillin and metronidazole (course of treatment 10 days), ranitidine (2 times a day before meals for 2 weeks).
The prescription of a specific treatment regimen depends on the specific characteristics of the disease. When the first signs of an inflammatory disease appear, you must immediately contact a qualified gastroenterologist, who, after an examination, will prescribe treatment appropriate to the patient’s condition.
In order to prevent gastroduodenitis, it is necessary to observe a general, dietary, physical regimen, ensure a balanced diet, and lead a healthy lifestyle. Timely treatment and compliance with the rules of the rehabilitation period are considered the most effective method of preventing peptic ulcer disease.
When identifying problems of the gastroduodenal zone in children, it is necessary to strictly adhere to the rules of age-appropriate nutrition and protect the child from emotional and physical stress. It is necessary to regularly visit a pediatric gastroenterologist and carry out timely therapy.
Untimely and improper treatment of gastroduodenitis and chronic gastritis is the cause of relapse of acute conditions. As a person gets older, there is a decrease in a person’s performance, and rapid fatigue is observed. Neglect of doctor’s prescriptions is the most common mistake; you must completely trust a qualified specialist.
Chronic duodenitis and the army
Gastroduodenitis is inflammation of the mucous membrane of the stomach and duodenum. What decision the military registration and enlistment office will make regarding a conscript diagnosed with duodenitis and whether he will be accepted into the army with this disease is stated in article 59 of the Schedule of Diseases.
As with chronic gastritis, it is difficult to get relief from this disease. People with duodenitis are recruited into the army if the disease occurs with a slight disruption of secretory function and rare exacerbations. In such cases, the draft commission assigns the category “B-3” to the young man. If seizures occur during service, the serviceman will be sent to a military hospital for treatment.
You can get a military ID with category “B” if:
- the disease requires long-term hospitalization,
- the disease is accompanied by impaired secretory and acid-forming functions, frequent exacerbations and a decrease in body mass index less than 19.
The answer to the question of whether they take a bullet into the army will be similar. This pathology is a type of duodenitis, in which the duodenal bulb becomes inflamed. If the conscript cannot confirm to the members of the military medical commission the presence of serious functional impairments and frequent exacerbations, the conscription commission will recognize him as fit for service. With a diagnosis of “bulbitis,” the army can release for up to 6 months if at the time of conscription the disease is in the acute stage and requires treatment.
general information
The doctor examines conscripts based on the “Schedule of Diseases”, which was approved by the Russian Government. This schedule includes illnesses, the presence of which exempts the young man from service. Gastritis is related to 59 and 61 articles simultaneously. Article 59 concerns gastrointestinal diseases and consists of three subparagraphs.
Article 61 stipulates illnesses for which a conscript receives a deferment from the army. A deferment is granted in two situations:
- acute gastritis was discovered during the recruitment period;
- the chronic form of gastritis has worsened.
To take a deferment legally, the young man must present a medical certificate or sick leave. If the disease has not been confirmed by a doctor, the conscript will be forced to return to his duties.
Legal grounds
Young people are recognized as fit to perform their duty to their homeland and a deferment is granted on the basis of a special Schedule of Illnesses. The state of health is assessed by the commission at the time of the examination, and entries in the medical record for the last 12 months are taken into account. Article No. 59 mentions reflux esophagitis, among other gastrointestinal diseases.
Theoretically, young people are not accepted to serve if they are confirmed:
- Gastroduodenitis;
- Gastritis;
- Reflux esophagitis.
Next, there is a clarification when reflux esophagitis is a reason for deferment and recognition as unfit for service. Doctors are required to confirm pathological changes in the functions of the gastrointestinal tract, malnutrition, frequent exacerbations, unsuccessful inpatient treatment, and the need for hospitalization for 2 months.
In other words, they will not be allowed to serve only if the illness is severe. There must be appropriate confirmation from specialists and the results of instrumental examinations. Over the past 12 months, hospital stay for treatment must have been at least 60 days in total.
Pancreatitis at military age
Pancreatitis combines a complex of diseases and symptoms when the exocrine function of the pancreas is disrupted. Normally, the organ produces special enzymes (amylase, lipase, protease) that are required for the digestion process. While in the pancreas, they are inactive, but when they enter the duodenum, pancreatic juice is activated.
Inflammation in the tissues of the pancreas is caused, as a rule, by a chronic course with alternating periods of exacerbation and remission. The manifestation and frequency of exacerbations depend on the severity of inflammation, general condition, the person’s immune strength, the prerequisites for the appearance of pancreatitis, and most importantly, on the patient’s adherence to treatment, adherence to all the doctor’s advice and prescriptions regarding therapy, diet and lifestyle.
The symptoms of acute (or exacerbation of chronic) pancreatitis are quite complex:
- Intense pain of a girdling nature, in some cases radiating into the chest;
- Nausea, vomiting, which does not bring relief to the patient;
- Increased gas formation, flatulence, bloating;
- Stool upset, diarrhea;
- General malaise, dizziness;
- Decline in blood pressure;
- Increase in body temperature.
After blocking the attack of pain and achieving remission, the patient’s condition becomes better, but sometimes after eating, bursting pain in the abdomen, a feeling of nausea, and upset stool may be observed.
In the army, it is impossible to fully adhere to all the specialist’s recommendations for preventing exacerbations of pancreatitis for the following reasons:
- There is no possibility of following dietary table No. 5, which is designed for patients with pancreatitis;
- Regular fairly heavy physical activity;
- Possible difficult morale, frequent stress;
- Inability to receive correct, ongoing drug therapy.
Taking into account the degree of decrease in the functionality of the pancreas and the frequency of exacerbations, suitability for military service is determined.
How to confirm the diagnosis for the military registration and enlistment office?
If you suspect gastritis, you should seek help from specialists and undergo an examination. The confirmed diagnosis, extracts of laboratory and instrumental diagnostic methods must be preserved. With each relapse, you need to go back to your doctor and record everything in your medical record. With all the documents you need to go to the military registration and enlistment office for a commission. This is the only way to confirm the diagnosis.
A relapse can happen at any time, and can also be absent if the instructions and prescriptions of doctors are strictly followed. At the time of passing the military commission, the disease may be in remission, so only documents from previous examinations can prove the complexity of the situation. The commission may decide to send for re-examination or issue a verdict on deferment or immediate release.
Diagnostic methods
It is practiced to identify diffuse and focal hyperemia of the mucous membrane, hypertrophy, and edema through endoscopic examination. In certain cases, the mucous membrane becomes thinned, pale, with smoothed folds. These signs are characteristic of the atrophic process; it should be noted that determining the presence of atrophy and its degree is possible exclusively with the help of histological studies.
Histological diagnosis of the duodenum and gastric mucosa is a prerequisite for determining the degree of development of dystrophic and inflammatory processes. Determination of the state of the secretory function of the stomach.
Intragastric pH-metry provides the ability to determine the pH of the body and the antrum of the stomach using built-in electrodes and a special probe. The normal pH level of the body of the stomach on an empty stomach is considered to be 1.7-2.5 (children over 5 years old); after exposure to a stimulant (histamine) - 1.5-2.5. Neutralization of acid is ensured by the antrum of the stomach, the pH of which should be more than 5; accordingly, the difference between the antrum and body pH should exceed 2 units.
A decrease in values in the stimulated and basal fractions is a sign of decreased secretory function. When certain indicators of any faction increase, one can conclude that the secret function has increased.
Intragastric pH-metry - diagnosis of gastroduodenitis
In most cases, in patients at an early age, chronic gastroduodenitis is accompanied by increased or normal secretory function; a decrease in levels may indicate the manifestation of an individual norm. A decrease in the level of gastric secretion is characteristic of severe atrophic forms of gastritis, which are extremely rare at an early age.
To obtain reliable information regarding motor function, it is necessary to perform antroduodenal manometry. In addition, assessment of motor function through electrogastrography (EGG), ultrasound (with preliminary filling of the stomach with liquid) is practiced.
The use of fluoroscopy to diagnose CGD is not practiced; it is an effective method for assessing evacuation function.
A mandatory step in determining the type of gastroduodenitis, followed by the appointment of effective treatment, is the diagnosis of HP infection. Diagnosis of helicobacteriosis is classified into two groups:
- The histological method has proven its effectiveness in practice; it has been given the status of a golden method in diagnosing helicobacteriosis.
- Bacterioscopy - detection of HP in cytological smears from a biopsy specimen.
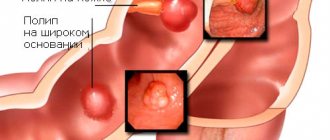
Erosion on the gastric mucosa
The main difference between erosive gastritis and other types is the risk of ulcers. At the first stage of the disease, erosions are small in size, and the lesions gradually grow, causing pain and causing stomach upsets. Doctors distinguish between two types of the disease: primary and secondary. In the first case, the disease develops spontaneously, in the second, the appearance is influenced by the presence of other disorders in the body.
Among other factors that cause destruction in the stomach, there is excessive use of medications. Steroid hormones, painkillers and anti-inflammatory medications, and digitalis-based drugs are considered especially harmful. Alcoholism develops erosive gastritis. Alcoholic drinks are harmful to the body as a whole, mainly affecting the digestive organs, especially the epigastrium.
In medical science, there is a generally accepted typology:
- Acute erosive – develops and is difficult. The occurrence is influenced by physical and chemical factors. This type of disease requires urgent treatment;
- Chronic erosive - sometimes called hemorrhagic. As a rule, it becomes the result of an unhealthy lifestyle, sometimes due to medications;
- Antral erosive gastritis - erosions occur in the lower segment of the epigastrium under the influence of Helicobacter pylori bacteria;
- Erosive reflux - with this disease, the contents of the duodenum splash into the stomach. The mucous membrane becomes irritated and erosions form on the surface.
https://youtu.be/8nxjjERrxco
Symptoms of the erosive type differ little from other types of gastritis. Dangerous due to its long hidden latent period. As a rule, the patient learns about the pathology at a late stage. It is recommended to immediately consult a doctor at the first signs of stomach upset to prevent erosion from progressing and developing into an ulcer. When diagnosing, tests are collected and endoscopy is mandatory.
In the case of the erosive type, the conscript is considered unfit in certain situations; with the disease, there is a risk of stomach ulcers. If the condition of the young man’s body is not serious, he is drafted into the army.