Differential diagnosis of esophageal cancer: morphological method
To study plasma, blood is taken from a vein, and absolute sterility must be observed.
To collect biological material, absolute sterility is necessary. The patient is seated comfortably, the needle injection site is treated with an alcohol solution. An elastic tourniquet is applied to the forearm above this area. The patient is asked to hold his hand in a fist several times. The injection is then performed, after which the tourniquet is loosened. The syringe delivers venous blood. After the procedure, the resulting mass is transported with a special preservative in individual tubes.
People at risk must undergo an annual routine examination (screening). It is this that allows early detection of the first signs of esophageal cancer.
Early diagnosis of the disease involves esophagoscopy with biopsy. These methods give the specialist the opportunity to identify the initial manifestations of esophageal cancer in people at risk.
Mass screening examinations are used in those categories of the population whose lives are directly affected by negative factors that can provoke the development of a pathological condition:
- persons with a genetic predisposition. The hereditary factor plays a significant role if a person’s blood relatives have a history of any cancer;
- people who have been diagnosed with benign tumors in various tissue structures and internal organs, which are considered potential precancerous pathologies;
- patients with Barrett's esophagus or ulcers of a diabetic, radiation or trophic nature that do not heal for a long time;
- lovers of alcoholic drinks of any strength, as well as heavy smokers.
Like any other tumor, a neoplasm that develops on the walls of the esophageal canal can be called malignant only after the presence of mutated cells is confirmed by the results of a biopsy. The main objectives of diagnostic studies in this case are to confirm the diagnosis, which is directly related to identifying the tumor and assessing the prevalence of the malignant process.
Diagnosis of esophageal cancer is carried out using the following main methods, which are of greatest importance for correct diagnosis:
- X-ray (conventional and contrast).
- Esophagoscopy (endoscopic examination) with biopsy.
- Laparoscopic and thoracoscopic minimally invasive interventions.
- Cytology of swabs, prints and smears from the mucous membrane of the esophageal canal.
Thanks to these diagnostic studies, specialists identify the classification of the tumor process, its localization, degree of development, as well as the presence of metastasis.
Studies carried out in later stages involve identifying abnormal cellular structures in other organs. Metastases from esophageal cancer most often grow into lymph nodes located directly in the mediastinum. With distant metastasis, the liver is affected in 20% of cases, the lungs in 10%, and the appearance of metastases in the brain and bone structures is also often noted.
To identify them, the following diagnostic measures are used:
- CT and MRI can detect the growth of abnormal cellular structures into the lungs, as well as large blood vessels and lymph nodes of the chest.
- Bronchoscopy. This procedure is used to detect metastases in the respiratory system.
- Mediastinoscopic examination. It is carried out using an endoscope and allows you to detect the beginning of metastasis of the peri-esophageal space.
- Plain radiography is performed for a comprehensive examination of the chest organs.
- Ultrasound reveals metastases in the liver.
Diagnosis of esophageal cancer, carried out to identify its metastasis in women, requires a mandatory examination by a gynecologist. Only a doctor of this specialization is able to confirm or exclude the presence of metastatic lesions of the reproductive system in the fair sex.
A malignant neoplasm developing in the esophageal canal is quite easy, due to similar clinical manifestations, to be confused with cardiospasm, achalasia, ulcerative esophagitis, and diverticula. To make a correct diagnosis, if this pathological condition is suspected, a differential diagnosis of esophageal cancer is mandatory. The leading method in distinguishing esophageal canal carcinoma from other gastrointestinal diseases is the morphological method.
To test for the presence of tumor markers-glycoproteins, you need blood, which should be donated in the morning and strictly on an empty stomach. That is, the last meal should be no less than 8 hours before taking the sample. It is also undesirable to drink sweet drinks the night before and take one of the B-group vitamins - B7. The latter distorts the result of the analysis for identifying the CA 72-4 antigen.
It is forbidden to drink alcohol (at least 48 hours before the test). The day before diagnosis, you should avoid heavy physical activity. Before donating blood (one hour), you should refrain from smoking.
The Tu M2-RK enzyme is isolated from feces for laboratory research, so you also need to prepare for this test for tumor markers for intestinal cancer. A small amount (about a tablespoon by volume) of feces is placed in a special sterile container and delivered to the laboratory. It should be borne in mind that laxatives or an enema should absolutely not be used for defecation - the material must be obtained naturally.
The timing of tests for different tumor markers for colorectal cancer differs:
- results for antigens CA 19-9, CA 242 and CEA will be ready within 24 hours;
- detection of glycoprotein CA 72-4 will take from 3 to 7 days;
- Stool examinations last a week.
The conclusions issued in the laboratory make it possible to decipher information about the results.
Interpretation of results
Antigens of the digestive tract are high-molecular compounds that enter the biofluids of the human body from mutated cells of the gastrointestinal tract or normal cells affected by a tumor growing nearby. As already mentioned, a certain type of protein often indicates damage to a certain part of the gastrointestinal tract.
Often the first antigens of the stomach and intestines are found in the plasma of venous blood, and the final one, Tu M2-PK, is obtained from the coprogram. The doctor makes a preliminary diagnosis with the following picture: a significant increase in the normal values of CA 242 and Tu M2-PK, an increased concentration of the substances CYFRA21-1, CEA, CA 72-4, CA 19-9, as well as the presence of CA 125 (optional). However, to reliably confirm the diagnosis, further comprehensive examination is always required.
How to take it
The study of gastrointestinal tumor markers is carried out using blood, urine and feces. You have to choose the most suitable option. If you do not want to donate blood, it is permissible to choose another medium. In this case, the diagnostic range of markers will be lower. The most common method is a blood test. For a good and accurate value, you should follow a diet for a number of days, and on the day of the procedure, come with an empty stomach in order to donate blood with the correct result.
The last meal is taken no later than 12 hours before the expected delivery. It is necessary to remember this rule. Many doctors recommend not eating the night before the test. A couple of days before the appointed date, give up sweet foods. Juice, sugary sodas and tea will compromise the accuracy of the test.
Blood is not suitable for analysis if a person takes B vitamins. This is critical if the test targets markers like 72-4. It is better to stop taking the drug the day before the test. In case of urgent need, the time is reduced to 8 hours.
The study of the Tu M2 PK marker is considered special. For research, the biological medium is stool analysis. Enemas and the use of laxatives are contraindicated. Due to its specificity, the result takes longer to determine than a blood test. The waiting time is 4 – 10 days.
Limitations in the use of the tumor marker method are highlighted. Examination of blood taken for nonspecific indicators gives incorrect ideas about the structure of morbidity. High values of individual indicators do not necessarily indicate tumor-like growths. Tumor markers for intestinal cancer are also isolated during inflammatory and structural changes in organs, and they are not associated with the spread of malignant neoplasms.
Factors and pathologies affecting analysis parameters
Deciphering the test by a non-specialist should be excluded, since the quantitative indicators of specific biomolecules can also increase with the emergence of benign formations or against the background of certain inflammatory diseases. Often, tumor markers can be positive against the background of the following diseases:
- cirrhosis;
- cholecystitis;
- Crohn's disease;
- bronchitis/pneumonia;
- colon abscess;
- stomach ulcer;
- nonspecific ulcerative colitis.
Gastric ulcer can affect the results of gastrointestinal tumor markers.
If we talk about the specific intestinal marker Tu M2-PK, then its concentration may well be increased in smokers and in cases of bacterial infection of the gastrointestinal tract.
Preparing for the study
To obtain reliable results from a test for gastrointestinal tumor markers, you should properly prepare for it. Preparation for the analysis does not have any specifics and is similar to the preparatory measures involving the collection of venous blood. Doctors advise adhering to the following requirements:
- do not drink alcohol 72 hours before the test;
- stop taking medications 24 hours before the test (except for urgently needed ones, which are known to the doctor);
- the day before the test, you need to lighten your diet by excluding spicy, fatty and fried foods.
The application of such simple rules allows you to count on accurate results. However, no matter how correct the preparation for the test is, this does not protect against the likelihood of a false positive result, since a wide variety of reasons can lead to an increase in the number of specific proteins. This is why experienced specialists insist on repeating the test in all cases.
The manifestation of such a symptom as constant pain in the left hypochondrium is an indicator for testing for cancer markers.
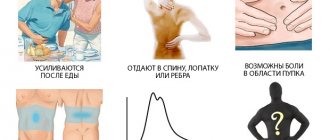
A blood test for pancreatic cancer is performed if the patient has the following clinical symptoms and signs:
- Girdle pain, predominantly localized in the left hypochondrium, radiating to the back and sternum. It is often confused with attacks of gastritis or angina.
- Dyspepsia. The latter is manifested by constant sour belching, lack of appetite and nausea.
- Loose stools. Very often, spots of fat appear in it, which has not been transformed in the gastrointestinal tract.
- The presence of diffuseness and anechoic inclusions in the organ during ultrasound examination of the abdominal cavity.
- Visualization of the formation using computed tomography or magnetic resonance imaging.
- Palpation of a lump in the left hypochondrium along the midline.
- Rapid weight loss with normal nutrition. Cancer cells devour nutrients from the food they eat.
- Abdominal enlargement due to ascitic effusion.
- Enlarged lymph nodes. Most often, the axillary and retroperitoneal lymph nodes begin to be palpated.
X-ray is the simplest, most effective and widely available diagnostic method for identifying a tumor of the esophagus. It makes it possible to examine the esophageal canal in unity with the organs adjacent to it. Experts in clinical practice note the high physiology of this method - with its help, a diagnostician can easily monitor the performance of the propulsive (promoting food) function by the esophageal canal.
Practicing oncologists in their medical activities rely on the following radiographic capabilities:
- detection of the presence of a tumor lesion in the initial organ of the gastrointestinal tract, in most cases accompanied by ulcerations of its surface and the presence of fistulous tracts;
- detection in one of the zones of the esophagus of a narrowing of its lumen and an overlying suprastenotic (directly dependent on stenosis) expansion;
- determination of the location (depending on the division of the esophageal canal into segments), as well as the shape and size of the carcinoma.
Diagnosis of esophageal cancer will not be complete if it lacks laboratory methods.
First of all, the presence of an oncological process in the esophageal canal is indicated by the following indicators of a general blood test:
- the presence of iron deficiency anemia, which always accompanies carcinoma, is confirmed by a decrease in hemoglobin levels (in men it does not exceed 130 g/l, and in women 120 g/l);
- a significant increase in erythrocyte sedimentation rate (above 20 mm/s for adults);
- decrease in the quantitative indicator of eosinophils (leukocytes).
To clarify the diagnosis of oncology, a blood test for tumor markers is required. In case of esophageal cancer, the presence in the bloodstream of an increased amount of certain protein structures characteristic of malignant processes allows the oncologist to suspect the development of carcinoma and prescribe the patient a full-fledged instrumental diagnosis.
Brief characteristics of pancreatic oncology
Pancreatic cancer arises from pancreatic tissue. The incidence of this tumor is increasing from year to year. Risk factors are the same reasons that lead to inflammatory diseases. This is alcohol consumption, smoking, overeating spicy and fatty foods, diabetes mellitus, liver cirrhosis, neglect in the treatment of pancreatic inflammation.
The tumor looks like a dense, lumpy nodule. Usually occurs in the head of the gland, less often in the tail. The most common form of pancreatic cancer is adenocarcinoma.
Important. Metastases spread first by lymphogenous and then by hematogenous routes. The kidneys and liver are often affected.
Pancreatic cancer most often does not show any symptoms until the final stage. And after symptoms appear, a person “burns out” in literally 1-2 months.
We also recommend viewing: Conducting and results of ultrasound of the pancreas
Sometimes typical symptoms of a malignant tumor may appear. Decreased appetite, sudden weight loss, body weakness, fatigue.
Rarely, cancer of the body and tail of the pancreas can manifest as pain in the stomach, which will radiate to the lumbar region.
Positron emission tomography PET
This method of diagnostic research, carried out using an endoscope, allows you to study the structure of tissue structures at a depth of up to 2 mm. To carry it out, laser light waves that are completely safe for the body are used. With their help, it is possible to make an accurate diagnosis even at preclinical stages.
Oncologists take into account the following indications for performing a PET study:
- determination of the primary location of mutated cellular structures in the esophageal canal;
- identifying the stage of development of the tumor process;
- planning the upcoming course of radiation therapy and assessing its effectiveness;
- timely detection of the onset of recurrence of the disease.
The main advantage of positron emission tomography is the absence of any adverse reactions. This procedure, which has no absolute contraindications, is effectively used for dynamic monitoring of patients of any age, both during the treatment course and after its completion.
Indications for testing
The main indications for determining gastric tumor markers in the blood:
- The age of the patients is over 40 years.
- Complaints of heaviness, pain in the epigastric region, aversion to meat foods.
- Nonspecific symptoms: sudden weight loss, severe weakness, lack of appetite.
- Stomach cancer in close relatives.
- Peptic ulcer, tumor, stomach polyps or other diseases of the gastrointestinal tract.
Persons with a hereditary predisposition to this pathology need to undergo fibrogastroduodenoscopy once a year and donate blood for tumor markers.
Organs of the gastrointestinal tract
The digestive system is the most massive in the human body. The length of the digestive canal in the body of an adult male reaches an average of 10 meters. The development of a malignant process in any part is accompanied by similar symptoms. Lack of bowel movements for 4 days, constipation, and bloating can be warning signs of many types of cancer. To determine the exact location, you need to understand the structure of the intestinal tract.
Tumor markers for stomach cancer are normally found in every person, like their other varieties. If these standards increase, we can talk about the development of oncological or benign pathology. In some cases, inflammatory diseases can also increase the amount of these substances.
Causes of stomach cancer
How and why stomach cancer develops is not completely clear. But the influence of certain factors has been proven in which the likelihood of a tumor increases. These include:
- Chronic atrophic gastritis, especially against the background of hyperplastic processes of the epithelium. This disease was found in 60% of patients with stomach cancer. In this case, the localization of the process was important. For example, when atrophy is located in the antrum of the stomach, the risk of developing cancer increases 18 times, and with total damage to the organ - 90 times.
- Helicobacter Pylory infection. The likelihood of developing stomach cancer in such patients is 3-4 times higher than in the general population.
- Nutritional features. Containing a large amount of hot, spicy, pickled, salty foods, fast food, smoked meats and fats in the diet statistically significantly increases the likelihood of developing tumors of the gastrointestinal tract, including the stomach.
- Presence of adenomatous polyps. Such neoplasms have a relatively high risk of malignancy, so they are recommended to be removed in a timely manner.
- Smoking.
- History of gastric ulcer. When an ulcer is located in the body of the stomach, the risk of developing a malignant neoplasm increases by 2 times.
- History of gastric surgery. Increases the risk of developing cancer by 4 times.
- Menetrier's disease, which is characterized by hypertrophic gastropathy or hyperplastic giant-fold gastritis.
- Drunkenness and alcoholism.
- Pernicious anemia. Anemia with a malignant course, which develops due to the inability to absorb vitamin B 12. It is also accompanied by immunodeficiency conditions, which increases the risk of developing a malignant tumor by 10%.
- Hereditary predisposition. The presence of malignant stomach tumors in close blood relatives increases the risk of developing cancer in this location by 5-20%. It is believed that Napoleon Bonaparte and his father died from this disease.
- Immunodeficiency states.
- Working with carcinogenic substances.
Tracheobronchoscopy (bronchoscopy)
This diagnostic method is primarily aimed at identifying metastases in the respiratory tract of a cancer patient, that is, the growth of synchronous tumors into the bronchi.
To carry out the procedure, a thinner endoscope is used, inserted through the nasal or oral cavity.
The use of this diagnostic method for carcinoma of the esophageal canal allows us to achieve the following goals:
- determine with the greatest accuracy the extent of the pathological process in the airways;
- assess the condition of the epithelial mucous structures covering the inner surface of the bronchial tree;
- identify the presence of narrowings in the bronchi and trachea caused by external compression of them by metastatic regional lymph nodes.
Thanks to bronchoscopy during the diagnosis of cancerous lesions of the esophageal canal, it is possible to identify both single and multiple metastases that have grown into the respiratory organs. This, in turn, gives the specialist the opportunity to select the most adequate course of therapy, allowing to prolong a person’s life for the longest possible period for this disease.
What does the analysis say?
When assessing the results of tests for tumor markers, we must not forget about the influence of additional factors that increase this indicator. These include pregnancy, inflammatory processes, bad habits, and many chronic diseases.
Also, increased amounts of tumor markers in biological fluids may indicate other diseases - benign tumors, cirrhosis of the liver, pancreatitis, stomach ulcers, bronchitis, rheumatism, nephropathy and others.
But for dynamic monitoring of the effectiveness of anti-cancer therapy, tumor markers are indispensable and reliable. Deciphering tests for tumor markers allows you to see the improvement or deterioration of the patient’s condition and the body’s response to the treatment.
If during chemotherapy or radiation an increase in the concentration of markers is observed, this indicates the death of tumor cells and a turn towards recovery.
The procedure has a completely different meaning after the operation or the end of treatment: their increase in this case signals the activation of the pathological process and is a signal to continue treatment or to choose another method.
What are gastrointestinal tumor markers?
Tumor markers of the gastrointestinal tract are protein compounds formed in cancerous tumors. They also talk about problems in the tract that require further investigation and treatment. The information content is quite high, but not sufficient for a clear diagnosis. It cannot be said that a patient has cancer based on an increase in the number of tumor markers of the stomach and other digestive organs. After all, their level can increase with compactions of a non-oncological nature.
Pathological protein compounds, if present, can be detected in the blood and urine. If they exist and there are a lot of them, this is a serious reason to undergo a full examination in a specialized institution.
Since oncology of the digestive system is common and cases of detection of tumors in young people are becoming more and more frequent, diagnosis becomes especially necessary and should be as informative as possible in order to identify the pathology at the time of its inception or at least at the stage of early development. In this case, the chance of recovery is much higher than if the detection is recorded later.
Tumor markers of the gastrointestinal tract are protein compounds formed in cancerous tumors. They also talk about problems in the tract that require further investigation and treatment. The information content is quite high, but not sufficient for a clear diagnosis. It cannot be said that a patient has cancer based on an increase in the number of tumor markers of the stomach and other digestive organs. After all, their level can increase with compactions of a non-oncological nature.
Consult an Israeli specialist
Types of substances that signal cancer
| Tumor marker | Characteristic |
| CA-242 | Increased concentrations are detected in malignant neoplasms of other parts of the gastrointestinal tract |
| Present in inflammatory pathologies of the pancreas, cystic formations in it | |
| Tu M2-RK | Ensures the occurrence of biochemical processes in newly formed malignant cells |
| CA 125 | Produce structural elements of the respiratory and digestive organs of the human embryo |
| In sporadic cases, the substance is found in patients with gastrointestinal cancer | |
| SA 72-4 | Biologically active substance, a high concentration of which is found both in pancreatic tumors and during pregnancy |
| SA 19-9 | Can produce bronchial cells |
| The value increases with neoplasms localized in the small and large intestines |
Biopsy
This diagnostic procedure is nothing more than instrumental and laboratory tests. For esophageal cancer, they involve directly taking a tissue sample from the affected organ and further examining it microscopically. A biopsy, according to experts, shows a fairly high success rate, since the correct diagnosis is made in 95% of cases.
With the help of this study, practicing oncologists receive the following information about a malignant neoplasm developing in the esophagus:
- the relationship of the tumor to certain treatment methods - radiation and chemotherapy;
- prognosis of carcinoma development.
The results obtained during the biopsy allow the specialist to most adequately select the method and the volume of surgical intervention required in each specific case, that is, partial or complete removal of the gastrointestinal tract organ damaged by oncology.
Prevention of gastric cancer
Prevention of gastric cancer
A significant mortality rate moves this cancer to 2nd place in terms of danger to life. As a rule, carcinoma is detected in patients after 40 years of age. But quite often stomach cancer is diagnosed in the younger generation, and this is primarily due to an incorrect lifestyle. When making recommendations regarding cancer diseases, experts direct their attention to the moments that provoke their formation. The exact causes of cancer are unknown. But there are a number of things that increase the risk of a tumor. These can also include:
- Incorrect diet (abuse of greasy, salty, fried foods).
- Tobacco smoking. It has been proven that carcinogens that enter the body through smoke increase the likelihood of developing cancer.
- Significant gastrointestinal ailments.
- Heredity.
- Injuries.
- Surgical intervention. The risk group includes patients who have undergone surgery to remove part of the stomach.
Prevention of stomach cancer involves eliminating all provoking factors. First of all, experts recommend promptly treating ailments that can later turn into cancer. An equally important aspect of prevention is proper diet. A balanced diet that contains vitamins and the exclusion of fried, smoked, spicy foods from the menu will help prevent the worsening of existing gastrointestinal ailments.
https://youtu.be/e_qv8qz_tDo
Types of tumor markers of the digestive system
Based on the increasing number of requests from patients with suspected gastrointestinal cancer, examination for tumor markers of the gastrointestinal tract is becoming especially popular. Since we are talking about diagnosing different organs that are part of the tract system, as well as the patient’s age, possible causes of the disease, family history of the disease and other points, a whole group of protein compounds is studied.
| REA | carcinoembryonic antigen of protein origin. Allows you to identify a malignant compaction in the area of the small and large intestine. Produced during intrauterine development. It is found in some quantities in the body of adults. An increase in their number indicates the formation of a node, including a benign one |
| CA125 | shows pathological formations in the area of the sigmoid colon |
| CA242 | may signal a risk of cancer formation in the rectum and colon |
| CA19-9 | these are tumor markers of the liver and pancreas, also synthesized in the bronchi, digestive organs, and intestines. They are of carbohydrate origin and are considered the main ones when there is no right to make mistakes in the treatment of diseases of the esophagus and intestines. They also allow detection of malignant tumors at an early stage. It is highly informative and reliable when monitoring the treatment of cancer patients |
| CYFRA21-1 | necessary to detect a tumor in the rectum |
| AFP (alpha fetoprotein) | helps identify oncology in the sigmoid and rectum |
| LASA-P | the most universal indicator of the presence of malignant formations in the gastrointestinal tract, including on the mucous membranes of organs |
| CA72-4 | used primarily for repeated examination during and after treatment of cancer of the stomach, intestines and ovaries. Produced by carcinoma. Due to the high reliability of the test, it is actively used in examinations, but only in combination with other tumor markers |
| TuM2 | tumor markers of the gastrointestinal tract, indicating the development of cancer in the intestinal area, metabolic disorders in cancerous structures |
| hCG (human chorionic gonadotropin) | a hormone that is produced to protect the fetus from the effects of the mother's immunity. It is an essential element of screening during diagnosis and treatment of intestinal and hepatic pathological seals |
Tumor marker indicators
Deciphering the results of the level of concentration of tumor markers helps to establish the presence of a pathological process in the organs of the digestive system.
The normal amount of proteins in the blood is:
- CA 242- 0-30 IU/ml;
- CEA – 0-5.5 ng/ml;
- CA 72, LASA – P – 3.8-4 IU/ml;
- Tu M2-PK – 1.5 IU/ml;
- AFP – 15 ng/ml;
- CA 19-9 – 3.4 IU/ml;
- CA 125 – 2.5 IU/ml;
- CYFRA 21−1 – 3.3 IU/ml;
- SCC – 1.5 ng/ml.
Exceeding the norm for the carbohydrate antigen CA 242 means the formation of cancer cells in the pancreas and large intestine. The stage of development of the disease is determined through a structural study of the okomarker. Early diagnosis of increased CA 242 levels guarantees positive dynamics in cancer treatment.
The presence of cancer is indicated by an excess of CEA concentration. A specific protein value greater than 5.5 units is a sign of a pathological change in the structure of the colon.
It is impossible to independently determine the presence of organ damage based on clinical examination data. Standardized concentrations of specific and nonspecific proteins in specialized medical institutions and private laboratories differ. This is due to the characteristics of the equipment used in the study.
Accurate detection of cancer is possible with a comprehensive determination of intestinal tumor markers. Prescribing a combined analysis of specific and nonspecific proteins increases the likelihood of a correct diagnosis. The types of laboratory tests are determined by the doctor depending on the purpose of blood sampling: establishing the presence of a tumor, the location of the spread of cancer cells, monitoring the progression of pathology.
Bone scintigraphy to determine metastatic bone lesions
This diagnostic procedure is an instrumental research method, which is a scan of the bone structures of the skeleton using a radioactive contrast dye taken in a minimal volume. Thanks to this technique, specialists can examine the bones of cancer patients much better and more deeply than with radiography.
Bone scintigraphy is performed in two stages:
- a special substance is injected by drop method (intravenously) - radioactive strontium or the isotope technetium, which is a contrast dye;
- After 3 hours, the second stage of the examination begins - direct scanning of the whole body. The procedure is performed 2-3 times to obtain more accurate results. The duration of this examination is approximately one hour.
The method of scanning bone structures makes it possible to detect in the early stages the beginning of metastases growing into bone structures, their size and quantity. Based on the results of the study, the patient is prescribed an adequate course of treatment, which may include surgery, chemotherapy and radiation.
Decoding
When studying tumor markers, the doctor differentiates between pancreatic cancer or other diseases. Based on the magnitude of their concentration, conclusions can be drawn not only about the presence or presence of an oncological process in the body, but also about the stage of carcinoma and metastases.
The level of malignant antigens in the blood of a healthy person is equal to the normal criteria. Less commonly, these values indicate that the disease is at an early stage. That is, normal tumor markers practically do not indicate cancer mutations.
The higher the concentration of antigens, the more extensive the malignant process in the body. If the readings deviate slightly from the norm, most likely we are talking about problems such as:
- pancreatitis;
- cholelithiasis;
- benign ovarian tumors;
- cirrhosis, hepatitis.
Process and technique of analysis
The need for such tests does not always arise. Often, such specific proteins are only a confirmation or refutation of the data that the doctor already has, but only indirectly indicate the possibility of oncology. Indications for taking this screening test will be:
- the appearance in the patient of ambiguous signs of the onset of a cancerous formation in one of the sections of the gastrointestinal tract;
- monitoring the effectiveness of radical surgical treatment or chemotherapy;
- the need to obtain data to predict the course of the oncological process;
- systematic monitoring for precancerous diseases.
A test for gastrointestinal tumor markers should be carried out without fail if a person has any digestive problems with constant fatigue and elevated temperature. In addition, you should take tests for tumor markers in the following cases:
- with a prolonged period of dysphagia: nausea and aversion to certain types of food;
- the patient is over 40 years old and has a family history of cancer;
- duplicate causeless increases in temperature up to 37-37.5 degrees;
- significant reduction in body weight.
In addition, in addition to primary diagnosis, markers are often used to monitor the treatment process, in particular, to detect relapses, the appearance of secondary cancer or metastases.
Testing for oncology is mandatory for all persons over 50 years of age who have a hereditary predisposition and are employed in enterprises whose activities involve chemicals and toxic substances (primarily workers with extensive work experience).
Timely testing makes it possible to identify tumor markers for cancer of the pancreas, stomach, esophagus and other organs at an early stage, which increases the risk of recovery.
In addition to the above, the main indications for analysis are:
- Primary and prognostic examination of the oncological process in the stomach and intestines, as well as their mucous sides.
- Checking the effectiveness of ongoing treatment procedures.
- Observation after treatment and prevention of relapse and metastases.
To determine the tumor marker for cancer of the stomach and other tract organs, it is necessary to refuse any food 8 hours before the examination. You can only drink still water.
Next, the patient sits down on the couch, and the doctor takes blood from a vein in the standard way. Please note that in this case, capillary blood can also be used (extracted from a finger by cutting the upper phalanx with a feather).
The resulting samples pass through special equipment in which the serum is separated from the blood. Antibodies are introduced into the resulting material in an amount corresponding to the number of markers that should be identified. After this, a chemical reaction occurs, the result of which reveals the normality or growth of pathological substances.
The most qualitative result is provided by the aggregate indicator of the quantity of all studied markers.
Remember that if there are indications, you should not delay the analysis, especially since in a good clinic the cost of tumor markers of the gastrointestinal tract is affordable and incomparable in price with the treatment that may be needed.
Before the study, the patient needs to prepare, namely, adhere to a low-calorie diet.
- Preparatory. On the eve of the test, the patient should adhere to a diet low in fat, simple sugars, food with dyes, preservatives, stabilizers, flavor enhancers and other chemical molecules.
- Ready on the day of the laboratory visit. You should not eat immediately before blood collection. You can only drink water. Physical and psycho-emotional stress should be avoided. Ignoring these rules will result in skewed results.
- Performing blood sampling. For this, the patient is seated in a comfortable position, his left hand is placed on the table and the elbow is slightly bent. A special tourniquet is placed on the forearm. The patient is asked to make a movement with his hand, as if he were pumping up an expander. Then a puncture is performed, the tourniquet is released and the blood mass is drawn into the syringe.
- Transportation of material. If the laboratory equipment does not allow highly specific tests, the blood is transported to another place. To do this, biological material is placed in special tubes on which the patient’s name or code number is marked.
- Material processing. In the laboratory, the blood mass is centrifuged and markers are determined using special analyzers.
When is an analysis for tumor markers of stomach cancer necessary?
It is necessary to do a study if any digestive problems often arise against the background of chronic fatigue and fever.
The analysis is also indicated for those who are over 40 years old or have a family history of cancer. In addition, regular screening during and after treatment is necessary. In the first case, the level of tumor markers informs about the effectiveness of treatment, and in the second, it signals an impending relapse long before its manifestation.
Videolaparoscopy and videothoracoscopy
Video endoscopic technology, widely used in surgery, is now increasingly used in oncology clinics. Practicing oncologists began to actively use video thoracoscopy and video laparoscopy in their daily clinical practice. Using these diagnostic and surgical methods, specialists can see at least 87% of lymph nodes affected by metastasis in the chest and abdominal cavity, which are not detected during MRI, ultrasound and CT examinations. Also, thanks to these methods, a fairly effective operation to remove them is possible.
The essence of these methods is as follows:
- Laparoscopy. It is carried out using a special device - a laparoscope, which is a telescopic tube with a lens system and a video camera. It is inserted through small incisions made in the abdominal cavity.
- Thoracoscopy. This is an endoscopic method for examining the chest organs. During the procedure, the endoscope is inserted through a small incision made in the intercostal space.
These diagnostic techniques allow specialists not only to conduct a complete visual examination of internal organs, starting with the liver, and regional lymph nodes, but also to take biopsy material.
What to do if the diagnosis of cancer is confirmed?
The final diagnosis of bowel cancer is not a death sentence. As soon as the doctor has identified a malignant formation, treatment must begin. It is strictly not recommended to visit grandmothers, grandfathers, herbalists, and psychics. This way you can survive to stage 4 with metastases and painful death.
Cancer, especially in the initial stages, is successfully treated with:
- operations;
- radiation therapy;
- drug treatment (chemotherapy, cytostatics, hormonal drugs).
Moreover, at the initial stages of the disease, organ-preserving operations are performed.
In later stages, radical methods of therapy (resection) are resorted to, and additional radiation and chemotherapy are required.
If it is not advisable to undergo surgery for a malignant tumor or all possible treatment methods have been exhausted, they resort to palliative care.
The success of therapy largely depends not only on the stage of the disease, but also on the patient’s attitude towards treatment. If you initially imagine yourself to be terminally ill, then it is more difficult to expect a positive effect.
In continuation of the topic, be sure to read:
- Details about intestinal colonoscopy: preparation and procedure
- How to check the intestines for oncology?
- How to use a rapid test from a pharmacy to determine occult blood in stool?
- Preparation and performance of MRI of the intestine
- Preparation and performance of computed tomography (CT) of the intestine
- Endoscopic methods for examining the intestine: description and preparation
- What does an intestinal biopsy show and how is the procedure performed?
- Histological examination of intestinal tissue: preparation and implementation
- How to detect and treat polyps in the intestines?
- Details about bowel cancer: stages, symptoms, treatment and prognosis