Hepatocellular failure is one of the forms of liver pathology, the origin of which is multi-vector and variable. The long list of probable causes for development mentions primary and secondary factors of damage, endogenous and exogenous starting mechanisms, and different scenarios for the course of the disease, from acute to fulminant forms. As in most cases, when the second largest organ in the human body is damaged, at the initial, latent stage there are vague, general symptoms. Their appearance is usually explained by simple and harmless reasons. but at this time an extremely dangerous condition is already developing.
Definition and reasons
Sudden deterioration of liver function in patients quickly leads to the development of hepatic encephalopathy. Plasma hemostasis is gradually impaired. The reason for this process may be:
- viral hepatitis (B, D, A);
- viral infection (CMV, EBV, HSV type);
- medications such as Paracetamol, Halothane, Phenytoin;
- herbal medicines similar to Chinese herbs;
- toxic substances;
- state of shock;
- acute or chronic pancreatitis;
- liver ischemia;
- sepsis;
- development of acute fatty liver degeneration during pregnancy in women.
Acute liver failure can lead to extensive degenerative, fibrous or necrotic changes in the liver parenchyma. In some cases, liver failure may develop due to impaired hepatic circulation. Quite often, a similar condition occurs with sepsis and portal vein thrombosis.
Drinking alcoholic beverages, anesthesia during surgery, and gastrointestinal bleeding can cause kidney failure. With hepatitis and cirrhosis, liver failure may occur. Pathological changes that develop in acute liver failure are caused by the accumulation of ammonia, amino acid and phenol compounds in the circulatory system.
The compounds quickly have a cerebrotoxic effect on the body, disrupting the water-electrolyte and acid-base balance. Reaching a serious condition, the detoxification process in the organ is disrupted. The liver ceases to take full part in the metabolic processes of various organs.
Acute liver failure can lead to extensive degenerative changes in the liver parenchyma
Diet
Diet in the treatment of liver disease is a mandatory procedure, since the liver receives a significant blow precisely from improper nutrition. The diet includes compliance with the following procedures:
- Reducing the level of protein and fat to 30 grams per day, and carbohydrates to 300.
- It is preferable to eat plant foods, which include: fruits, vegetables, honey, compotes, jelly.
- Consume food only in liquid or semi-liquid form. At the same time, you need to eat little by little, but every 2 hours.
- Eliminate salt from your diet completely.
- If there is no swelling, then you need to drink about 1.5 liters of fluid per day.
Diet plays an important role in the treatment of liver failure, so a combined effect will help you get rid of the symptoms of the disease and return to your previous healthy life.
https://youtu.be/FQnYxfpbbBw
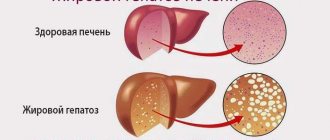
Poisoning with poisonous plants or chemicals, chronic diseases or long-term use of potent medications, all these factors negatively affect the most important organ of the digestive system - the liver.
The gradual death of hepatocytes (liver cells) leads to deterioration and then partial loss of organ functionality.
A disorder of one or all liver functions in the language of specialists is called liver failure (LF), or hepatocerebral insufficiency. The symptomatic complex characteristic of PN syndrome can develop gradually or occur suddenly in the acute form of the pathology.
Types of liver failure
There are several forms of acute liver failure:
- endogenous;
- exogenous;
- mixed.
The endogenous form includes a pathology that develops due to (direct) damage to the parenchyma of an organ. The exogenous form includes liver failure, which is caused by circulatory disorders in the organ. In this case, blood saturated with toxic accumulations is discharged into the general circulation. In mixed forms, both endogenous and exogenous types of deficiency are observed in the body.
According to the level of severity of functional impairment of the organ, experts distinguish several stages of hepatopathy:
- Stage 1, in which there are practically no liver lesions. Using laboratory tests, moderate functional impairment (increased enzyme levels, bilirubin and increased transaminase levels) can be detected.
- Stage 2 is characterized by the appearance of clinical symptoms. Organ pain, attacks of hepatic colic, and hemorrhagic diathesis appear. There is an increased level of hyperbilirubinemia, hypoproteinemia, and dysproteinemia in the blood.
- Stage 3 is considered the most severe. To the signs of the previous stage are added hepatic encephalopathy and hepatic coma, which develops against the background of gross impairment of the functionality of the organ.
Stage-by-stage development mechanism
The mechanism of development of liver failure is determined by structural and functional disorders in liver cells (hepatocytes), leading to their cytolysis and necrosis (death). The immune system begins to perceive damaged hepatocytes as pathological agents, and an autoimmune process is realized that destroys liver cells.
The death of areas of parenchyma leads to disturbances in the basic functions of the liver:
- hemodynamic;
- excretory;
- antitoxic and phagocytic;
- metabolic.
At the initial stage, long-term compensation of liver functionality is possible, but the progression of the disease inevitably leads to its impairment. Toxins that are not neutralized by the liver begin to enter the blood, which leads to damage to the most important systems, in particular the central nervous system. This shows up:
- dysfunction of motor-vegetative activity;
- mental disorders;
- weakening of the intellect.
Continued damage to the organ leads to a disorder of the biliary system and cholestasis. As a result, an excess amount of bilirubin enters the blood, causing an enlargement of the liver and a toxic-allergic reaction from most organs. Decomposition products not neutralized by the liver affect the brain, leading to encephalopathy, and damage to large areas of the central nervous system leads to hepatic coma.
Symptoms
At the clinical stage of the disease, the patient experiences the following symptoms:
- drowsiness;
- periods of excitement are replaced by prolonged apathy;
- attacks of nausea;
- gagging;
- lack of appetite;
- yellowness of the skin;
- diarrhea;
- swelling;
- hemorrhagic diathesis;
- ascites;
- fever and intoxication of the body.
Before the coma, dizziness, auditory and visual hallucinations, slowness of speech and thinking begin to appear, insomnia is replaced by constant drowsiness, confusion, tremors of the limbs, varicose veins of the anterior abdominal wall. The patient experiences motor agitation. Bleeding from the nasal passages is systematically observed.
A harbinger of coma is considered to be pain in the hypochondrium, the appearance of a liver odor from the mouth, and a decrease in the size of the organ. In hepatic coma, the patient loses consciousness, experiences convulsions, hypothermia, and arrhythmia. The patient exhibits manifestations of pathological reflexes.
Treatment of acute hepatic renal failure should be carried out in the intensive care unit
Liver failure in children
In case of liver failure at a young age, doctors identify some differences that are not characteristic of the adult manifestation of the disease. In childhood, it is very difficult to determine the signs of hepatic encephalopathy. Experts believe that impaired blood clotting may be a reason for further diagnosis for liver failure.
Hepatic coma.
Hepatic coma is the most severe manifestation of decompensated hepatic cell failure (HCF). PCN can be acute or chronic. Hepatic coma can develop as a result of chronic liver diseases: hepatitis, cirrhosis.
3 stages of hepatic cell failure (HLF) (both acute and chronic):
1. Compensated stage. 2. Subcompensated stage. 3. Decompensated stage.
- In stage 1, the following manifestations begin: poor alcohol tolerance, hepatomegaly, positive stress tests.
- In the 2nd stage: general weakness, poor nutrition syndrome, hepatomegaly, jaundice, endocrine and skin signs, edema, slight ascites, moderate increase in the activity of AL, AST, thymol and sublimate are moderately positive, decrease in albumin.
- In the 3rd stage , everything is the same, only there is also severe weakness and jaundice, pronounced ascites and edematous syndrome, for the first time hemorrhagic syndrome, diathesis, low-grade fever. Laboratory data are clear. Hepatic coma is characterized by severe brain damage from cerebrotoxic substances (ammonia, phenol). There are pathological reflexes.
Classification.
- Endogenous PC or true, or hepatocellular or decay (can be with cirrhosis and hepatitis). With this coma in the liver there is deep dystrophy, necrosis, functions are impaired. Both ammonia and phenols are poorly inactivated and penetrate into the brain.
- Exogenous or portocaval or shunt PC . Only in patients with cirrhosis does it occur with portal hypertension and the presence of portocaval anastomoses.
- Mixed PC. There is also a hepatic moment. Endogenous and also anastomoses - blood discharge, shunt option.
- Hypokalemic PC (not officially accepted).
Coma is practically poisoning of the brain with cerebrotoxic substances. play a major role . Pyruvic acid, lactic acid, tryptophan, methionine, and tyrosine are also important. In healthy people, ammonia is completely neutralized in the liver, and ammonia and phenol are formed. Phenols in the liver cell combine with glucuronic acid, therefore they are neutralized and non-toxic. For precoma and coma to begin, 80-85% of the liver cells must fail (massive liver necrosis, etc.).
Ammonia and phenol penetrate the brain membrane, making it permeable, followed by H and Na into the cell, and K comes out, leading to intracellular kalemia and pyruvic acid also penetrates inside, acidosis begins, then respiratory alkalosis. The penetration of Na and H leads to the penetration of water, cerebral edema and acidosis begin. Redox processes are inhibited, and the brain gradually falls asleep. Cerebral edema is one of the leading causes of death. Pulmonary edema, renal failure, and hypovolemic shock are in the background.
Diagnosis
When taking an anamnesis, it is important to take into account the use of medications and herbal remedies, previous surgery, transfusion of blood products, travel to remote corners of the planet, mushrooms eaten or hereditary liver diseases.
The specialist, as a rule, writes out a referral for the patient to undergo:
Symptoms of liver necrosis
- general blood test;
- blood group analysis, arterial blood gasometry;
- analysis of the level of paracetamol in blood serum;
- screening toxicological analysis;
- virological research;
- electroencephalography (at stages 1 and 2 of the disease, triphasic waves are used, at stages 3 delta waves should be used);
- pregnancy test (for women).
Diagnostics
Which doctor should I contact?
When the first signs of illness appear, there is no need to hesitate to visit a gastroenterologist or hepatologist. Modern diagnostic methods will make it possible to diagnose the disease in the early stages, which will reduce its severe consequences.
The initial consultation consists of taking a medical history, examining the skin, and palpating the abdomen. Then the doctor will prescribe a number of laboratory and instrumental examination methods that will help confirm or refute the doctor’s suspicions, determine the stage of the disease and other changes in the body’s functioning.
Which examination to take?
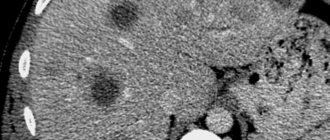
Diagnosis of liver failure consists of:
- General blood test.
- Liver blood samples.
- Blood biochemistry.
- General urine analysis.
- Analysis for antibodies to the hepatitis virus.
- Ultrasound of the abdominal cavity.
- Computed tomography (CT) and magnetic resonance imaging (MRI).
- Liver biopsies.
The results of the examination will help the doctor draw up a complete clinical picture of the disease, make the correct diagnosis, and prescribe the necessary treatment.
Treatment
Treatment of acute hepatic-renal failure should be carried out in the intensive care unit. Specialists take into account hemodynamic and metabolic parameters, water and electrolyte imbalance, and the rate of infection development. It is very important to choose a medical center where the therapy will be carried out. It is desirable that it provides organ transplantation services.
General principles of treatment
The patient is fed through a nasogastric tube. The patient needs about 65 g of protein daily and 30 kcal of energy value per kg of weight. It is unacceptable to use foods containing glutamine in your diet. For prophylactic purposes, H2 blockers are used for acute hemorrhagic gastropathy.
For preventive purposes, it is recommended to take antibiotics and antifungal medications. Medicines must have a wide spectrum of action. Conducting diagnostic tests for infections. In this case, it is advisable to take a chest x-ray and undergo a microbiological test of blood, sputum and urine.
If there is an indication for liver transplantation, the patient can be saved only if the transplantation takes place within 2 days
Symptomatic therapy
Symptomatic treatment is carried out according to the following scheme:
- Therapeutic methods aimed at preventing Hepa-Mertz hepatic encephalopathy.
- Prevention of brain swelling. The patient's head and torso are elevated by 30°. For epileptic seizures, the patient is prescribed Phenytoin, which is administered very slowly. It is very important to periodically evaluate the patient for symptoms of increased intracranial pressure.
- Coagulopathy, in which vitamin K is administered in a dosage not exceeding 10 mg. For bleeding, fresh frozen plasma should be administered. For each kg of the patient’s body weight, 15 ml of plasma will be required. Transfusion of platelet concentrates may also be required.
- In case of hemodynamic disorders and renal failure, a certain intravascular volume is maintained. Experts recommend using colloidal solutions. If blood pressure exceeds 50-60 mm Hg. Art., you need to use adrenaline, norepinephrine or dopamine. In some cases, pulmonary artery catheterization and renal replacement therapy are required.
- Metabolic disorders. A large number of biochemical parameters makes it necessary to regularly monitor and compensate for various disorders. In cases where there is a predisposition to hypoglycemia, continuous administration of glucose may be required.
- Empirical antibiotic therapy is used in patients with pneumonia, urinary tract infection, sepsis, and spontaneous bacterial peritonitis.
Etiological treatment
Etiological therapy is required in cases of poisoning with drugs based on paracetamol, poisoning with assorted mushrooms, autoimmune hepatitis, acute fatty liver during pregnancy, ischemic liver damage.
Liver transplantation
Patients who need liver transplantation are:
- with organ damage that occurred due to an overdose of paracetamol, exceeding the creatinine norm, or reaching stage 4 encephalopathy;
- with liver damage of a different etiology (childhood, a long period of jaundice, which the person suffered before the onset of encephalopathy, increased bilirubin levels, the presence of viral hepatitis caused by halothane, toxic damage to the organ).
Quite often, the cause of liver dysfunction is an excess dosage of paracetamol or another drug.
Extracorporeal liver function support
Extracorporeal support of liver function can often be used in case of hepatic encephalopathy in order to maintain the metabolic and detoxification functions of the organ before the start of the liver transplantation period. During the methodology, methods such as:
- MARS, which combines albumin dialysis and adsorption;
- FSPA – liver dialysis;
- SPAD, characterized by albumin dialysis in a single-transition albumin dialysate system;
- CVVHDF is a combined technique with continuous venous-type hemodiafiltration.
general information
Short description
Notes
This subheading includes : - hepatic coma, unspecified; - hepatic encephalopathy, unspecified; - hepatitis (acute, fulminant, malignant), not classified elsewhere, with liver failure; - necrosis (of liver cells) with liver failure; - yellow atrophy (dystrophy) of the liver with liver failure.
Excluded from this subheading : - “Alcoholic liver failure” K70.4
Period of occurrence
Minimum incubation period (days): 7
Maximum incubation period (days): 84
October 17-19, Almaty, Atakent
200 participating companies, seminars and master classes, discounts, prize draws
Get an invitation card
October 17-19, Almaty, Atakent
200 participating companies, seminars and master classes, discounts, prize draws
Get an invitation card
Prevention
Quite often, the cause of liver dysfunction is an excess dosage of paracetamol or another drug. For preventive purposes, it is unacceptable to self-medicate. All doctor's recommendations must be strictly followed.
Any seemingly harmless medicine can lead to liver failure if the dose is calculated incorrectly. You should also take herbal medicines and herbal complexes with caution.
If you get vaccinated against hepatitis in a timely manner, you can protect yourself from the deficiency caused by this disease. Viral hepatitis causes irreparable harm to the body. It can be transmitted through sexual contact, through syringes and needles. People often become infected with the disease by getting piercings and tattoos, or by using other people's razors for shaving.
As a preventative measure, it is prohibited to use unfamiliar mushrooms and plants in the diet. When working with chemicals, it is important to wear a respirator. In case of acute liver failure, it is unacceptable to self-medicate! You should consult a doctor as soon as possible for help and undergo the examinations he recommends.
Only prompt treatment can save a person’s life and restore lost health. If an urgent liver transplant is required, it is important to choose a reputable clinic with experienced doctors. This is the only way to be sure of a positive outcome of the operation.