Pancreatitis is inflammation of the pancreas. In this case, the enzymes secreted by the gland are not released into the duodenum, but are activated in the gland itself and begin to destroy it (self-digestion). The enzymes and toxins released can enter the bloodstream and seriously damage other organs such as the heart, kidneys and liver.
Complications of pancreatitis
Acute forms of pancreatitis, namely purulent, alcoholic, biliary and hemorrhagic, are often accompanied by such a serious consequence as pancreatic necrosis - the death of pancreatic cells. This diagnosis is considered pathomorphological, that is, it is established during an autopsy of the body of a deceased patient with pancreatitis.
With necrosis of the gland, gradual partial or complete death of the organ cells is observed. Tissues dissolve under the influence of enzymes produced by the gland. This process can be aggravated by infection and peritonitis.
Pancreatitis can occur in acute or chronic form. Acute inflammation is severe, with fever, severe pain and digestive disorders. The earlier treatment for this disease is started, the better the prognosis.
But even if all the doctor’s recommendations are followed, after recovery the patient will feel the consequences of pancreatitis all his life. In most cases, the disease becomes chronic. After all, destroyed pancreatic cells are not restored, so its functions are reduced.
At the same time, women are less likely to develop complications, since they are more responsible about their health, follow a diet and follow doctor’s recommendations. In men, exacerbations occur more often, which leads to faster destruction of pancreatic tissue. The risk of developing serious complications is especially high in those who abuse alcohol.
Complications of chronic pancreatitis are usually divided into general and local. Local complications are splenic vein thrombosis, jaundice, formation of pancreatic cysts and pseudocysts.
Common complications of the progressive chronic form of the disease include:
- Avitaminosis;
- Chronic fatigue and decreased ability to work;
- The appearance of abscesses;
- Left-sided pneumonia;
- Gland cancer;
- Development of diabetes mellitus.
As a rule, with the development of pancreatitis, neighboring organs of the abdominal cavity also suffer. Due to a violation of the outflow of bile, there is a risk of developing obstructive jaundice, fatty degeneration, bleeding, rupture of the spleen and many other diseases affecting vital organs.
Probability of a favorable outcome after treatment of the disease
The earlier pancreatitis is diagnosed and all measures are taken to cure it (drug treatment, surgical methods, strict dietary therapy), the better the prognosis for recovery and future life. Inflammation should not be allowed to become chronic, and if this has happened, then it is necessary to try to minimize the risk of exacerbations. To do this, you need to follow all the recommendations of your doctor regarding medication, nutrition and lifestyle.
Inflammatory pathology of the pancreas is a very dangerous pathological process, which often leads to life-threatening complications that require long-term serious treatment. If you suspect the development of such conditions, the main thing is to immediately consult a specialist (gastroenterologist, surgeon, endocrinologist) and follow all the doctor’s recommendations.
Bibliography
- Mayev. B. Chronic pancreatitis. 2012
- Yamlikhanova A.Yu. Main risk factors and quality of life in patients with acute and chronic pancreatitis. Abstract of the dissertation. Novosibirsk 2010
- Grigorieva I.N., Verevkin E.G., Bragina O.M., Yamlikhanova A.Yu. Nutrition and quality of life in patients with chronic pancreatitis. Russian Journal of Gastroenterology, Hepatology and Coloproctology. 2010 p. 88.
- Grigorieva I.N., Nikitenko T.I., Yamlikhanova A.Yu. Acute and chronic pancreatitis of alcoholic etiology. Materials of the 7th East Siberian Gastroenterological Conference. Krasnoyarsk 2007, pp. 191–198.
https://youtu.be/by7UNc4PKr8
Dangerous phenomena of acute pancreatitis
The danger of the acute form of the disease begins with attacks that can develop instantly and last from several hours to several days. Moreover, the more severely the gland is affected, the longer the attack lasts.
Often during an attack, constant vomiting develops, with bile particles, pain is localized in the upper abdomen, and dehydration occurs. The pain is so intense that it can lead to the development of pain shock in the patient.
Changes in the skin of the abdomen and navel and complexion appear. The tongue is predominantly white, but in severe cases it is brown. The pupils dilate, bloating occurs, the urine darkens, and the stool becomes lighter.
To reduce the risk of severe complications and danger to life, immediate medical attention is required. Treatment is carried out in a hospital.
Types of acute pancreatitis:
Edema is swelling of a diseased organ with small areas of necrosis in the adipose tissue nearby.
Necrotic is extensive necrosis of the organ itself with hemorrhages, including around it in the fatty tissues.
Under certain factors, for example, excess fat deposits around the organ (obesity), edematous pancreatitis easily turns into necrotizing.
What is a pseudocyst
This is a common complication associated with ineffective treatment of acute pancreatitis.
The formations take the form of “sacs” formed on the walls of the pancreas. There is liquid inside the growths. Such pathologies appear a month after diagnosis. Without equipment, it is impossible to identify pseudocysts. Some symptoms indicate the presence of pathology. Manifest in the form:
- diarrhea and bloating;
- dull pain in the abdomen;
- disorders of the gastrointestinal tract system.
If the patient does not feel discomfort associated with the presence of formations, there is no need to eliminate them. If the size of the cyst increases to six centimeters, bleeding appears. Large formations are treated by pumping fluid out of the cavity.
Complications after acute pancreatitis
How dangerous is acute pancreatitis? If proper treatment is not provided, the disease moves from the acute phase to the severe phase. Severe intoxication occurs from the enzyme trypsin, the effect of which is similar to snake venom. The actions of trypsin cause cerebral edema and kidney function is impaired.
The development of necrosis and dystrophy of the gland is an advanced disease. This disease of destructive forms (damage to toxins, abscess, purulent phenomena) leads to death in 40-70% of cases.
After the acute course of the disease has resolved, ulcers, fistulas, and local erosions and cystic manifestations appear on the surface of the gland and nearby organs. As a result of attacks of the disease, disorders of the nervous system develop. Patients often experience acute psychosis after alcohol intoxication against this background.
After several attacks of acute pancreatitis, the disease often becomes chronic.
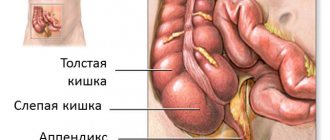
The pancreas is anatomically and functionally connected to many structures of the abdominal cavity. In the immediate vicinity of the gland there are many internal organs: the stomach, liver, gallbladder, duodenum, large blood vessels, as well as the omental bursa (the part of the abdominal cavity formed by these organs, the ligaments between them, as well as the structures of the peritoneum).
Acute inflammation of the pancreas inevitably affects the condition of these organs, causing the following pathological conditions:
- abscess of the omental bursa;
- compression of the common bile duct (common bile duct), which causes obstructive jaundice;
- the appearance of cysts, ulcers, fistulas on internal organs;
- destruction of the walls of blood vessels and the development of internal bleeding;
- vein thrombosis (portal, splenic, mesenteric, portal and others);
- peritonitis (inflammation of the peritoneum when the inflammatory process spreads into the abdominal cavity, rupture of abscesses, ulcers);
- when decay products and microorganisms enter the bloodstream, toxemia and sepsis (blood poisoning) may develop;
- toxic encephalopathy - brain damage due to the influence of toxins on it, especially in acute alcoholic pancreatitis;
- shock state (the pathogenesis of shock varies depending on its cause: infectious-toxic shock develops due to sepsis, painful shock develops due to intense pain syndrome, and hypovolemic shock appears after severe bleeding).
Shock
A state of shock is characteristic of severe pancreatitis.
Manifestations of this condition are:
- Severe sharp pain in the abdominal wall or radiating to the back.
- Blueness of the skin (acrocyanosis). This occurs due to poor blood supply to small capillaries of the skin. As a rule, fingers, ears, and lips turn blue.
- Paleness of the skin.
- Changes in breathing. It becomes more frequent and more superficial.
- Rapid heartbeat with possible arrhythmia.
- Ischemic symptoms. Detected using ultrasound.
- The daily volume of urine is significantly reduced.
- Disturbances in the functioning of the central nervous system. They are expressed in psychomotor agitation.
Pancreatitis causes of the disease
In acute pancreatitis, the pancreas begins to digest its own tissue. The process is accompanied by inflammation of the gland tissue, an increase in the organ's volume, and swelling. Necrosis is observed.
There are 2 forms of pancreatitis:
- An edematous type of disease.
- Pancreatic necrosis of tissue. It is divided into 3 types: fatty; hemorrhagic and purulent.
The edematous form of pancreatitis is characterized by compaction and swelling of the organ tissues, fluid formations are observed in the abdominal cavity, and fragments of necrosis are present.
In the fatty form of the disease the following is observed:
- Violation of the lobular structure of the gland.
- There are fatty spots in the abdominal cavity, omentum and in the gland itself.
- The abdominal cavity contains serous fluid containing a large amount of enzymes.
With hemorrhagic pancreatitis there are:
- swelling of peripancreatic tissue;
- hemorrhage of areas of the gland is observed, while the cells acquire a black or cherry tint;
- a large number of necrotic plaques;
- the presence of fluid in the abdominal cavity containing not only enzymes, but also enzymes that are toxic.
The purulent form of pancreatitis is characterized by:
- the development of necrotic fragments in the gland and in the tissues around it;
- pus accumulates in the abdominal cavity.
The edematous form of pancreatitis occurs in the following cases:
- changing the usual diet, for example, traveling abroad, to the countries of the East;
- periodic intake of fatty or fried foods;
- frequent drinking; when using methyl alcohol, vinegar essence;
- eating fatty foods after fasting, starvation or diet cancellation;
- after long-term use of toxic medications.
Probability of death
Some complications of acute pancreatitis are very dangerous and can be fatal. Such severe consequences of the disease as shock, sepsis, internal bleeding require immediate hospitalization in the clinic - in the surgery or intensive care unit, as they lead to multiple organ failure (liver, kidney), and the development of coma. To treat abscesses, peritonitis, and bleeding from a large vessel, surgical intervention is necessary, and then intensive care in an intensive care unit.
If the severity of the patient's condition is underestimated, diagnosis is delayed, or there is no effective medical care, the likelihood of death from complications of acute pancreatitis is very high.
Acute pancreatitis, even with proper treatment, can develop into a chronic inflammatory process. Chronic pancreatitis occurs with periods of remission and exacerbations. With each exacerbation of the pathological process, new areas of the pancreas die, and its functions are increasingly disrupted, which gradually leads to the development of serious complications.
Diagnostics
To assess the condition of the pancreas and identify complications from other organs, you will need:
- Ultrasound of the abdominal organs. The safest and most simple diagnostic method. Allows you to assess the condition of the gallbladder, liver, spleen, kidneys and pancreas.
- Magnetic resonance or computed tomography. The most reliable research method.
- Physical examination. Includes examination of the patient’s skin and mucous membranes, palpation of the abdomen, tapping and listening to cardiac and pulmonary sounds.
- Blood pressure measurement.
- Counting breathing and heart rate.
- Measuring body temperature.
- General and biochemical blood tests. An acceleration of ESR, a high level of white blood cells, an increase in amylase, lipase, sugar and liver enzymes are often detected.
- Analysis of urine.
- Culture for sterility. Required if sepsis is suspected.
- Electrocardiography.
- X-ray of the lungs.
- Examination of the abdominal cavity using a laparoscope through a puncture.
- Doppler (ultrasound examination of blood vessels).
- Elastography (measurement of tissue density and elasticity).
If respiratory failure is suspected due to pancreatitis, the following may be performed: spirometry (measurement of external respiration parameters using a spirometer), peak flowmetry (measurement of expiratory flow), measurement of vital capacity of the lungs, study of blood gas composition and acid-base state.
Irreversible changes in the gastrointestinal tract
Under the influence of constant exacerbations of the inflammatory process and destruction of pancreatic cells, the dead areas of the organ are replaced with connective tissue (scarring, fibrosis or sclerosis of the pancreas) - this is an irreversible change in the anatomy and physiology of the gland. Such areas are no longer useful in terms of performing exocrine or endocrine functions.
Pathological changes gradually develop in other organs of the digestive tract. The mucous membranes of the stomach, duodenum, gallbladder, bile ducts, and esophagus are subject to inflammatory changes. In the stomach and esophagus, erosions appear on the walls and, as a result, sclerosis of the walls, strictures (narrowing of the lumen) of the hollow organ. Inflammation of the gallbladder (cholecystitis) contributes to stagnation of bile and the formation of stones in the bladder. Damage to liver cells causes liver lipomatosis (replacement of dead hepatocytes with adipose tissue). The inflammatory process in the walls of the small intestine is dangerous due to the formation of intestinal obstruction.
The course of the disease is protracted, and pathology gradually develops. There are three forms of development:
- Mild - when the ducts remain unchanged, there is a slight increase in the organ, a slight change in structure.
- Moderate - the presence of cysts less than 10 mm, unevenness of the gland duct, infiltration (penetration of substances into the organ by one third), uneven edges and contours, thickening of the walls.
- Severe – the presence of cysts more than 10 mm, an unevenly dilated duct, a complete change in the structure and enlargement of the gland.
Processes in chronic pancreatitis
In the pancreas, stagnation of secretion occurs, since the ducts at the outlet are narrowed, trypsin and other enzymes are activated inside the gland. The danger of chronic pancreatitis is that the main tissue - parenchyma - is replaced by connective tissue, which is not capable of reproduction. The result is exocrine (enzyme deficiency) and endocrine (insulin deficiency) insufficiency.
The production of the necessary enzymes in the required quantities decreases. Substances are unable to enter the intestines to digest food due to changes in the ducts.
The production of insulin, necessary for the normalization of metabolism (metabolism), is an important function, but if there are disturbances, the production of the hormone decreases or stops completely. Self-destruction occurs and pancreatic necrosis develops. The tissues and cells of the gland gradually die. Pathological changes create a danger of destructive effects on other parts of the body.
Dangerous complications:
- obstructive jaundice (with an increase in the anterior part of the pancreas);
- duodenal stenosis (narrowing);
- purulent phenomena - the formation of abscesses of the organ and nearby tissues or organs;
- inflammation of the peritoneal walls (peritonitis);
- blood poisoning (sepsis);
- bleeding;
- cholestasis (changes in bile flow);
- thrombosis of the splenic veins;
- diabetes mellitus of all types, including type 1;
- formation of hematomas, cysts up to 10 mm or more;
- tumor growth;
- hypovolemic shock (loss of blood volume circulating in the vessels, and extremely rapid);
- acute renal failure.
Against the general background of the disease, bleeding gums, skin rashes, and brittle nails develop.
Statistical data
World statistics show that every year up to 800 people out of a million become ill with a disease such as acute pancreatitis. Men suffer from this type of pancreatitis much more often than women. The age of the patients has a fairly wide range, and this is directly related to the reasons why acute pancreatitis occurred. If acute pancreatitis arose and developed due to excessive alcohol consumption, the average age of patients is 39 years. If the cause of this disease is cholelithiasis, then the average age of patients is 69 years.
Consequences of pseudotumor chronic pancreatitis
The form of the disease in which the pancreas significantly increases in size is called pseudotumor. Chronic pancreatitis in this form has the following consequences for the body:
- jaundice, which occurs due to pinching of the bile ducts by the pancreas;
- an increase in the size of the spleen due to compression of the corresponding vein;
- portal hypertension, which is expressed by a significant increase in the veins of the esophagus and the appearance of ascites (fluid) in the peritoneum due to compression of the portal vein.
The described consequences are typical for one form or another of pancreatitis, but their occurrence in less typical cases cannot be ruled out.
Consequences of hemorrhagic pancreatic necrosis
The most severe condition is observed with hemorrhagic pancreatic necrosis. A person can die within 24 hours after the first signs of the disease develop. The prognosis for the fatty type of pancreatitis is determined by the area of distribution of necrosis, as well as the amount of swelling of the pancreas.
If you quickly consult a doctor, the disease can be “extinguished” in the first phase; Allowing the transition of pancreatitis to the next stage threatens the gradual passage of each of them and the development of serious complications.
The consequences may be:
- Pancreatogenic shock, endogenous intoxication.
- Peritonitis.
- Abscess or phlegmon of the retroperitoneum.
- Necrosis of part of the stomach and colon.
- Pancreatic fistulas.
- Bleeding from the gastrointestinal tract.
- Acute renal, liver failure.
- Acute pulmonary injury.
- Brain swelling.
The mortality rate of acute pancreatitis is up to 15%, with hemorrhagic forms and with large-focal or total necrosis - up to 70%. The main danger of chronic pancreatitis is exacerbations with fatal outcomes, the development of diabetes mellitus and pancreatic cancer.
How to determine the disease
The edematous form of acute pancreatitis is recognizable by the following signs:
- Pain under the ribs on the left side and in the abdomen, radiating to the dorsal region;
- Fatigue, an unusual state of tiredness;
- Weak condition;
- Pain in the head, often a state of nausea occurs;
- Problems with stool;
- Attacks of vomiting.
When the disease occurs, the signs and symptoms are similar to those of other diseases. Doctors note that the abdomen is soft and there is no bloating. Problems in the heart and lungs are also not detected. The pain is recorded in the left side of the body under the ribs, patients report pain in the lumbar region. Typically, pain occurs after eating fatty foods and drinking alcoholic beverages, mainly after long feasts that combine both causes.
Patients with edematous pancreatitis report the impossibility of lying in a horizontal position on their back. The pain gets worse when turning from side to side.
Some note the occurrence of diarrhea. The reason is a lack of enzymes. Complicated types of disease lead to the process of intoxication of the body.
Effect on the digestive system
The most common complication of pancreatitis is disruption of the gastrointestinal tract. Decreased production of basic digestive enzymes leads to poor digestion of food. Because of this, there is a deficiency of many vitamins and minerals. In addition, intestinal function is disrupted, and ulcers or erosions often develop on its walls. The patient constantly experiences discomfort, he often experiences diarrhea, constipation, and flatulence. In the most severe cases, this condition leads to intestinal obstruction.
A prolonged inflammatory process can provoke diseases of neighboring organs. The gallbladder is most often affected. The bile ducts exit into the duodenum along with the pancreatic ducts, so they are the first to be affected by the inflammatory process. Cholecystitis, biliary dyskinesia, and cholelithiasis develop. And if the enlarged gland blocks the ducts, stagnation of bile may occur and obstructive jaundice develops. In this case, only surgery can save the patient.
Gastritis, peptic ulcers, esophageal erosions, and gastroduodenal reflux are also frequent companions of pancreatitis. Sometimes degeneration of liver cells and the development of lipomatosis may begin.
Disorders in the cardiovascular system
In the cardiac system and blood vessels there are disturbances in the functioning of these organs. There is tachycardia (increased heartbeat), cardiopathy (increase in heart size, heart failure, unstable heart rhythm), and decreased blood pressure.
The vessels narrow, oxygen does not reach the organs in the required quantity, and vascular spasms occur. Blood clotting worsens, unexpected nosebleeds occur.
When pancreatic enzymes enter the bloodstream, this negatively affects the functioning of all organs. An inflammatory process in the pancreas can disrupt the functioning of the cardiovascular system. This is due to insufficient liver function, lack of essential microelements and an increase in the size of the gland. As a result, the heart rhythm is disrupted and blood clotting decreases. The consequence of this may be tachycardia, atrial fibrillation, and frequent bleeding. Vascular spasms also occur, and blood pressure may decrease.
Treatment
The edematous form of pancreatitis requires conservative treatment. Moreover, an improvement in the condition of the organ is noted within a few days. The pain goes away, the vomiting condition passes. It will take three weeks for complete healing.
After a person with edematous pancreatitis is admitted to the hospital, gastric lavage is prescribed. Then follows a strict diet, only warm mineral water is allowed. Antispasmodics are prescribed (as a rule, droppers are placed using these medications). They use drugs aimed at reducing the production of enzymes in the pancreas. Treatment is aimed at stopping pathological processes. To neutralize hydrochloric acid, doctors use antacids.
Diet
The patient is recommended to fast; after a day of restriction, the use of alkaline mineral water is allowed. Drinks allowed:
- dried fruit drink;
- tea;
- fruit juices.
The approximate amount per day is 1.5 liters of liquid. After a week of fasting, light vegetable soups, liquid porridge without milk, carrot and potato purees and jelly are introduced. If the patient feels well, it is possible to include crackers, boiled or steamed meat and fish dishes, and a small amount of low-fat cottage cheese in the diet.
The main principle of nutrition is fractional. Daily food is divided into 6 times, consumed in small portions. Despite the individual approach in each case, the following nutritional conditions are required:
- Absence of alcoholic beverages and fatty foods on the patient’s menu;
- Exclusion of fruits and vegetables that promote secretory activity;
- You should not eat spicy or fried foods;
- It is worth giving up bread made from rye flour and baked goods.
Intoxication psychosis
Intoxication psychosis is typical for people who abuse alcohol. Expressed in uncontrolled behavior, hallucinations, hyperthermia.
There is a risk of developing vascular thrombosis from the breakdown products of pancreatic tissue.
Late complications occur 15–20 days a week from the onset of the disease and are caused by the addition of an infection.
Purulent pancreatitis, parapancreatitis, peritonitis. Characterized by high body temperature, fever and excessive sweating. There is a risk of developing sepsis, abscesses and phlegmon of the abdominal cavity, as well as cysts and fistulas of the stomach or pancreas.
Pneumonia and pleurisy (most often left-sided). Symptoms:
- difficult shallow breathing;
- dyspnea;
- chest pain and wheezing;
- bluishness of the skin.
Causes and treatment of acute edematous pancreatitis: how and with what to relieve swelling of the pancreas?
A pathological disorder of the functionality of the pancreas of an inflammatory nature can have both an edematous form of development and a necrotic one. The most popular is acute edematous pancreatitis. Pancreatic edema is a rather dangerous sign, with a high risk of developing an abscess, and in which the ducts are filled with an impressive amount of epithelial exfoliated cellular structures and leukocytes. Remember: swelling of the pancreas creates all the conditions for all breakdown products to enter the blood plasma and contribute to intoxication of the entire body.
Complications of pancreatitis
Inflammation in the tissues of the pancreas causes serious complications. Diseases such as diabetes mellitus and pancreatic cancer are diagnosed in patients with chronic pancreatitis quite often.
Diabetes
Diabetes mellitus of a pancreatogenic nature develops as a result of the death of cells of the endocrine pancreas - the islets of Langerhans, which produce the hormone insulin. If there is a shortage of it, sugar supplied from food is not utilized by liver or muscle cells, but remains to circulate in the patient’s blood. This condition is called hyperglycemia. High blood glucose levels can lead to impaired consciousness and hyperglycemic coma. Constantly increased sugar content causes characteristic diabetic complications - damage to the retina, kidneys, and all blood vessels of the body (diabetic angiopathy).
To prevent the development of these dangerous consequences, a patient diagnosed with diabetes must constantly monitor glycemic levels, receive insulin replacement therapy, and be observed by an endocrinologist.
Pancreatic necrosis
Destruction of pancreatic tissue, or pancreatic necrosis, occurs due to the destructive effect of its own enzymes on the organ. Retaining in the gland due to a violation of the outflow of pancreatic juice into the lumen of the duodenum, proteolytic enzymes begin to damage all surrounding tissues: pancreas, gall bladder, stomach, peritoneum, causing life-threatening complications (peritonitis, abscesses, ulcers).
If pancreatic necrosis is suspected, an urgent consultation with a surgeon is necessary and an operation is performed - resection of part of the pancreas or the entire organ, depending on the lesion.
Oncology
Malignant neoplasms often develop in tissues exposed to prolonged inflammation. Pancreatic cells with pancreatitis change their structure, mutate, and become vulnerable to the influence of free radicals and other oncogenes. As a result, they turn into a malignant form and begin to multiply uncontrollably: this is how carcinoma (malignant tumor) is formed. The most commonly diagnosed cancer of the pancreas is a tumor of the epithelial cells of the organ. Calculous pancreatitis with the formation of stones in the excretory ducts of the gland is especially dangerous in terms of oncology.
A terrible diagnosis - pancreatic cancer - is a consequence of chronic pancreatitis. Resection of part of the affected area or removal entirely is necessary. If the affected organ is removed, for the normal functioning of the body, you will need to take medications for life:
- replacement enzymes;
- lipotropic (amino acids involved in lipid and cholesterol metabolism);
- insulin (to normalize blood sugar levels).
Pancreatitis is considered difficult to treat, but if measures are taken in time, there is a chance to stop the destruction. Compliance with simple rules, constant use of medications and careful attention to the body will reduce the consequences of pancreatitis and save health and life.
Pancreatitis and pregnancy: consequences for the child
Inflammation of the pancreas in the first trimester of pregnancy has a negative effect on the course of pregnancy. The risk of developing preeclampsia, an acute condition that can lead to spontaneous abortion, increases. In addition, a woman may be bothered by severe repeated vomiting, leading to dehydration.
The conditions listed above negatively affect the health of the fetus. If measures are not taken in time, he will not receive the necessary nutrients, and hypoxia and dehydration may develop.
Disease prevention
To eliminate the risk of developing the consequences of pancreatitis, it is necessary to promptly consult a specialist for diagnosis and timely treatment of the disease. The following will also help avoid possible complications:
- balanced diet;
- reducing alcohol consumption;
- fractional meals (frequent meals of small portions of food);
- sufficient physical activity.
Taking medications wisely (do not overuse them) and avoiding stress will also help keep your pancreas healthy.
Sources
https://gastrotract.ru/bolezn/pankreatit/chem-opasen-pankcreatit.html https://pankreatit03.ru/posledstviya.html https://gastrolekar.ru/pankreatit/chem-opasen.html https://netpankreatitu .ru/o-zabolevanii/opasnye-oslozhneniya.html https://ponosov.net/opasnye-posledstviya-pankreatita.html https://zhktok.ru/bolezn/pankreatit/oslozhneniya-hronicheskogo-pankreatita-i-ego-posledstviya .html https://peptic.ru/pankreatit/vidy-i-prichiny-2/posledstviya-pankreatita.html