Ileitis - what is it?
Ileitis is an inflammation localized mainly in the final part of the small intestine and covering adjacent tissues.
Leads to the formation of polypoid or scar-ulcerative formations. It affects not only the thermal part of the small intestine, but also the duodenum, jejunum, and colon. Mostly, ileitis is diagnosed in people aged 20 to 40 years, more often in men. It occurs two times less often in rural populations than in residents of large cities. According to scientific data, in 70% of cases, pain in the right iliac region is a symptom of chronic ileitis. In general, the described pathology accounts for 6% of all intestinal inflammation.
Classification of ileitis
According to the criterion of damage to the small intestine, the following are distinguished:
- isolated ileitis;
- ileitis, combined with inflammatory processes in the stomach and colon;
- ileitis affecting the entire intestine.
Due to the occurrence of ileitis, it happens:
- parasitic;
- medicinal;
- infectious;
- enzymatic;
- nutritional;
- postoperative;
- toxic.
It can also be primary or secondary (resulting from another gastrointestinal disease).
Taking into account enzymatic activity, doctors distinguish:
- atrophic ileitis;
- non-atrophic ileitis.
According to the characteristics of the course, inflammation can occur with or without complications in three forms:
Types of ileitis
Depending on the location of inflammation, ileitis is divided into two types:
- First type. These include: – damage to only one part of the small intestine; – damage only to the ileocecal region (the zone of transition of the small intestine to the large intestine); - damage to only one segment of the colon.
- The second type includes: – damage to several parts of the small and large intestine; – simultaneous damage to the intestines and stomach, esophagus, and oral mucosa.
Forms of ileitis
Taking into account the characteristics of the course of ileitis, gastroenterologists classify it into three forms:
- Primary attack (acute symptoms dominate).
- Chronic intestinal ileitis - there are no acute symptoms, the disease lasts more than six months.
- Recurrent ileitis - symptoms often recur, exacerbations alternate with remission for more than six months.
Depending on the characteristics of the clinical picture, it happens:
- acute ileitis (inflammation of the ileum);
- chronic jejunoileitis, accompanied by impaired absorption of nutrients;
- jejunoileitis, complicated by small intestinal obstruction syndrome (the jejunum and ileum become inflamed, the process of passing feces through the intestines is disrupted);
- granulomatous proctitis (multiple small tumor-like formations form on the wall of the rectum),
- granulomatous colitis (small tumor-like granulomas form on the wall of the large intestine).
https://youtu.be/lRUUEQ6aFcs
Classification
By level of damage
- Localized (only the ileum, most often the terminal area, is affected).
- Widespread (with the transition of the inflammatory reaction to other parts of the small or large intestine).
- Ileitis, combined with gastritis, pancreatitis and other pathologies of the gastrointestinal tract.
Due to the occurrence
- Infectious ileitis (viral, bacterial, fungal, parasitic).
- Medicinal (inflammation caused by prolonged exposure to the mucous membrane of certain medications).
- Toxic (biological or chemical toxins).
- Autoimmune (Crohn's disease).
- Enzymatic (aggressive action of its own enzymes: atrophic and non-atrophic ileitis).
- Nutritional factors (poor nutrition, junk food, lack of a meal plan).
- Postoperative ileitis.
With the flow
- Easy degree.
- Average.
- Heavy current.
Also, ileitis can be acute and chronic (the process lasts more than 6 months), which depends on the cause, age, characteristics of the immune system’s response, and therapeutic measures.
According to the nature of intestinal tissue damage
- Catarrhal inflammation (affects only the mucous membrane).
- Erosive (formation of deep erosions up to the muscular or serous layer, sometimes with perforation of the intestinal wall). The most unfavorable variant of the course of terminal ileitis.
Causes of ileitis
The most common cause of infectious ileitis is Yersinia infestation. Less commonly, inflammation in the ileum is caused by:
- salmonella;
- coli;
- staphylococci.
Viral acute ileitis is a consequence of the negative effects of rotoviruses and enteroviruses. Giardiasis and helminthic infestations lead to a chronic form of the disease.
Common causes of ileitis include:
- allergic reactions;
- alcoholism, smoking;
- constant consumption of fatty and spicy foods;
- poisoning with heavy metals, poisons, chemical reagents;
- hereditary predisposition;
- intestinal surgery;
- taking certain medications.
Ileitis can also be a symptom of typhoid fever, tuberculosis, and ulcerative colitis.
Features of work
The secret secreted by the ileum, like the entire small intestine, is intestinal juice, with the help of which parietal (membrane) and cavity digestion is carried out. About two liters can be released per day. Intestinal juice is formed due to chemical and mechanical irritation of the food lump (chyme) of the intestinal walls. The dense part of the juice are epithelial cells - special cells on the villi of which the necessary enzymes accumulate and then are released into the intestinal lumen, which promote the hydrolysis (decomposition with water) of food and the absorption of necessary substances. The main enzyme in intestinal juice is enterokinase.
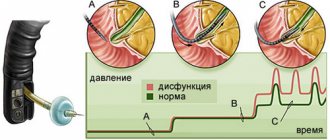
Thanks to the peristaltic contraction of one layer of intestinal muscles, the chyme, treated with enzymes, moves further into the large intestine. At the same time, its contents are mixed with the help of pendulum-like waves created by another layer of muscles.
Cavity and parietal digestion are closely interconnected. During the cavity, food is hydrolyzed to intermediate substances, and intermediate substances during the membrane process continue to be broken down and begin to be absorbed with the help of intestinal motility (motor function), mucosal villi and an increase in pressure inside the intestine. The environment in the ileum during the digestion process is alkaline.
Terminal ileitis – inflammation of the ileum
When a patient develops such a dangerous and difficult-to-treat disease as Crohn's disease, very often the pathological inflammation spreads to the ileum, thereby provoking the occurrence of terminal, or otherwise called reflux ileitis. It is always chronic and localized in the distal small intestine. Sometimes it can be combined with a pathological lesion that affects the duodenum, small intestine and cecum.
The morphological picture of ileitis usually reveals catarrhal-hemorrhagic inflammation, which is accompanied by a narrowing of the lumen in the digestive organ due to sclerosis of the walls with the formation of numerous erosions on them, developing into severe ulcerations. All this causes obstruction in the affected organ, which requires only surgical treatment.
In terminal ileitis, as in Crohn's disease, the etiology is not clear enough. Among the factors that provoke the occurrence of the disease, experts mostly identify the following:
- Genetic predisposition (heredity). The greatest tendency to develop the disease is in those people whose close relatives were susceptible to nonspecific pathologies of the digestive organs;
- An autoimmune reaction that occurs in the body;
- Imbalanced diet, exposure to bad habits and frequent stressful situations;
- Secondary viral or bacterial infections that occur in the body against a background of weakened immunity.
In addition, some experts believe that the cause of terminal ileitis, which is expressed by the development of inflammation in the ileum, is the failure of the valve located between the large and small intestines, called the bauhinian valve.
There are also opinions that this cause is a consequence of pathology. There is no clear opinion on this topic yet. All that can be said with certainty is that this valve is always involved in the process of development of ileitis.
Functions of the cecum
The main function of the cecum is the absorption of the liquid component from chyme - a semi-liquid lump consisting of semi-digested food, enzymes and acids of gastric juice, bile of exfoliated epithelium, and various microorganisms. The wall of the cecum is similar in structure to the large intestine. The mucosa has small folds of muscle fibers; it contains goblet cells and Lieberkühn's glands - tube-shaped depressions of the epithelium that are important for normal intestinal motility. The role of the appendix is also very serious. Its numerous follicles are protection against hostile foreign agents and perform a barrier function.
Symptoms of terminal intestinal ileitis
Many patients with diagnosed nonspecific pathologies of the digestive organs often have a question: how to recognize this inflammatory disease of the ileum? This question is quite complex, because the symptoms of terminal ileitis are very similar to other diseases, and accurate research is necessary to determine the diagnosis.
In addition, this pathology of the digestive organs is almost always accompanied by manifestations that seem foreign at first glance: joint or kidney pain, inflammatory processes developing on the skin and mucous membranes, and eye pathologies. But, despite the fact that such symptoms are very difficult to attribute to the development of terminal ileitis in the body, some of them should alert the patient and set him up to visit a specialist to clarify the diagnosis. The main signs that usually accompany the development of this disease and their intensity roughly indicate its stage are the following:
- Unreasonable loss of appetite and severe weight loss;
- Attacks of nausea, always turning into vomiting;
- Pain in the ileum, reminiscent of colic;
- An increase in temperature to 39-40 degrees and a feverish state that occurs for no apparent reason;
- Cramping pain reminiscent of an attack of acute appendicitis.
General information
The pathology has ICD-10 code K50.0 - Crohn's disease of the small intestine. The disease is also known as terminal catarrhal or regional inflammatory process. The pathology is common, almost everyone has experienced the disease. The disease is more often found in adult men.
With terminal inflammation, the clinic manifests itself as follows: the distal part of the intestine loses its ability to absorb. Redness and swelling of the tissues of the mucous membranes of the ileum, pain, and increased body temperature occur.
Types of pathology
The disease is found in different forms:
- Combined form - a number of parts of the gastrointestinal tract are affected.
- Chronic (erosive) intestinal ileitis is the presence of persistent inflammatory agents in the ileum. This type is divided into stages: exacerbation stage, partial remission stage, complete remission stage.
- Acute ileitis is a pathology with pronounced symptoms and severe pain. As a rule, this form does not last long and is quickly treatable. Sometimes this variety does not even require medical intervention.
Crohn's disease - prognosis
It is impossible to completely cure terminal ileitis; a person will have to adhere to a diet all the time, engage in therapy and prevent the pathology. So far it is only possible to control Crohn's disease - the prognosis for life is favorable, provided:
- compliance with dietary recommendations;
- giving up bad habits;
- regular visits to a gastroenterologist;
- timely treatment and prevention of complications.
A gastrointestinal disease such as terminal ileitis occurs spontaneously, and it is quite difficult to cure. The consequences of ignoring the problem can take horrifying forms. What is the essence of this disease and how to cope with it?
This kind of disease refers to intestinal problems. At its core, ileitis is an inflammatory process in the ileum of the small intestine, which is accompanied by the formation of ulcers and polyps, destruction of the mucous membrane up to the appearance of purulent fistulas. Most often, the disease develops in a young body between the ages of 15 and 20 years.
This disease is also known as reflux ileitis or Crohn's disease. The forms of manifestation may take the form of a sudden attack of colic, an acute recurrent nature, or a moderate one with permanent digestive upset. The chronic form does not allow you to eat normally and causes constant discomfort, which can lead to complete refusal to eat.
Causes of the anomaly
In children, the causes of acute ileitis include the consumption of a number of foods (carbonated drinks, chips, crackers), failure to comply with personal hygiene rules, and the presence of helminths in the body.
In adults, the chronic version of the disease is common. Sources of discomfort:
- inactive lifestyle, sedentary work;
- the presence of pathogenic agents in the intestine;
- viral and chronic diseases of the digestive system;
- aphthous stomatitis.
Factors that can cause chronic or acute pathology are:
- the body's tendency to allergic reactions;
- smoking;
- addiction to alcoholic beverages;
- poor nutrition;
- intoxication of the body;
- working in hazardous industries or living in an environmentally unfavorable area;
- course treatment with medications that have side effects on the digestive system;
- metabolic disease;
- genetic predisposition;
- operations on the gastrointestinal tract.
Diagnosis of the disease
Primary diagnosis of the disease is aimed at excluding similar pathologies. Terminal ileitis is an inflammation in which it is impossible to examine the ileum with a probe. Making a diagnosis solely on the basis of the patient's description of symptoms often leads to a superficial treatment path being chosen.
Pathology is reliably diagnosed during physical examination. The correctness is evidenced by the patient’s dry tongue with a white coating and pain in the right lower abdomen on palpation. If the patient has bloating, percussion will be ringing.
The following are recognized as informative diagnostic procedures:
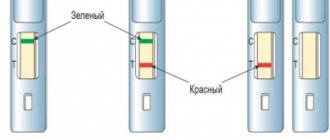
- radiography of barium movement (the small intestine is examined);
- Ultrasound of the abdominal and pelvic organs;
- general and biochemical blood tests;
- stool examination for blood, viruses and bacteria;
- coprogram.
Diagnosis of small intestine cancer
How to recognize colon cancer at an early stage? This determines what treatment will be used, the patient’s condition and the prognosis for survival.
Diagnosis of small intestine cancer is carried out using popular methods:
Fibrogastroscopy
- X-ray examination;
- fibrogastroscopy;
- angiography of the vessels of the peritoneal cavity;
- laparoscopy;
- colonoscopy;
- CT and MRI;
- biopsy examination: determine the type of cells and the degree of their malignancy;
- electrogastroenterography: detect disturbances in small intestinal motility characteristic of cancer.
How to identify intestinal cancer, the symptoms of which do not manifest themselves in anything specific? During this period, it is very important to confirm or refute the suspicion of cancer, because the sooner treatment begins, the easier it is for the patient to endure its stages, the greater the chance of a positive result. When symptoms appear, the oncological process can be considered advanced, and the moment of early treatment will be missed.
Important! Early symptoms include a “young” state, which should alert any person - this is a reluctance to work or do household chores due to increased weakness and fatigue. The skin becomes pale and “transparent”. The patient constantly has heaviness in his stomach, he does not feel like eating at all. Following this, dyspeptic disorders appear: nausea, vomiting, pain and heartburn even from water.
When visiting a doctor, a blood test for colon cancer is immediately prescribed and examined. A general basic blood test can reveal anemia, the patient's condition, and the presence of inflammation. According to the level of ESR and hemoglobin - problems in the liver, kidneys and blood. The composition of the blood may indicate certain diseases, including cancer.
Tumor markers for small intestinal cancer are detected in the blood. The most informative and common tumor markers are alpha-fetoprotein, total PSA/free PSA, CEA, CA 15-3, CA-125, CA 19-9, CA 72-4, CYFRA 21-1, hCG and cytokeratin.
For example, using the tumor markers CA 19.9 and CEA (carcinoembryonic antigen), screening diagnostics of colon cancer is carried out. If CEA is determined, then you can find out the staging before surgery and monitor the patient diagnosed with colorectal cancer after it. If the disease progresses, then the level of CEA in the serum will increase. Although it may grow not in connection with a tumor, in later stages colorectal cancer can be detected without an increase in CEA in the blood.
Read here: Gastrointestinal cancer: features of cancer
Endoscopic diagnosis and open intestinal biopsy are the main methods for confirming small intestinal oncology.
Treatment and prevention
Therapy is carried out in a hospital setting. This allows you to prevent unwanted complications of the pathology. Treatment is carried out by gastroenterologists and infectious disease specialists. Ileitis is curable, but after discharge from a medical facility, home treatment until complete recovery can last for months.
Treatment of ileitis
Conservative treatment involves a mandatory gentle diet. The patient should eat small meals 5-6 times a day. The diet should contain protein and fermented milk products. Spicy, coarse, fried and fatty foods are strictly prohibited. To facilitate the body’s recovery from digesting food, the patient is prescribed enzyme preparations and probiotics. It is mandatory for a person to be prescribed vitamin-mineral complexes. If the disease is due to a genetic predisposition, the patient must constantly follow the nutritional recommendations.
If the patient suffers from nausea and vomiting, temporary fasting and therapy with antibacterial agents are necessary. Infusion therapy is performed to prevent dehydration. To maintain vitality, the patient is prescribed droppers with protein solutions, glucose, and electrolytes.
For prolonged diarrhea, sorbents and astringent medications help.
To reduce the severity of pain, effective antispasmodics are prescribed.
Acute ileitis has a favorable prognosis. If ileitis is chronic, the prognosis depends on the extent of the damage to the intestinal mucosa. If the patient follows all the doctor’s clinical recommendations, the final result is equivalent to recovery, but the risk of relapse for this type of inflammation is quite high.
Advanced forms are difficult to treat. The result of this course of the disease is a gradual depletion of the body against the background of a deficiency in the supply of nutrients to organs and tissues. However, dehydration due to extreme inflammation of the ileum is extremely rare.
Ignoring doctor's recommendations, gross violation of diet, or refusal to treat chronic ileitis can lead to the death of the patient.
https://youtu.be/NUMU_cRNlAs
Prevention
Prevention is based on the following:
- Compliance with diet. It is necessary to monitor the quality of food and the content of vitamins.
- Quitting alcoholic drinks and smoking.
- Seek medical help promptly if signs of viral diseases are detected or if a digestive disorder occurs.
- Active lifestyle. Regular physical activity will help keep your body's muscles toned.
Crohn's disease - treatment
Due to the lack of precisely known causes of the described chronic pathology, special therapy to eliminate it has not yet been developed. All options for treating Crohn's disease come down to stopping the inflammatory process, preventing complications and relapses. The main methods of therapy are medication and diet. In the presence of severe consequences of terminal ileitis, surgical intervention is performed.
Crohn's disease: treatment - drugs
The main direction in the treatment of the disease is to relieve inflammation and restore the normal digestive process. Terminal ileitis - treatment involves taking the following pharmacological agents:
- glucocorticoids – Prednisolone, Methylprednisolone;
- salicylates – Mesazaline, Sulfasazalin;
- immunosuppressants – Methotrexate, Azathioprine;
- topical hormones – Budesonide, Beclazone;
- antibiotics – Rifaximin, Ciprofloxacin;
- genetically engineered biological drugs – Etanercept, Infliximab and others.
Crohn's disease continues to be researched, so scientists are constantly looking for new ways to combat terminal ileitis. The following are considered promising options:
- integrin receptor blockers – Vedolizumab;
- live donor or genetically modified bacteria;
- sorbents;
- conjugated linoleic acid;
- DNA sequencing;
- nanotechnological drugs;
- enzymes;
- plasmapheresis;
- stem cells – Polychrome;
- placement in a hyperbaric chamber;
- marijuana products - Naltrexone;
- plasma absorption;
- vaccines against inflammatory bowel pathologies;
- preparations based on pig worm eggs (TSO) and others.
Diet for Crohn's disease
All gastroenterologist patients with this diagnosis are required to be prescribed a special diet. The diet for terminal ileitis is selected taking into account the nature of the disease and the presence of complications. The milder the degree of pathology, the more products are allowed for consumption. Diet for Crohn's disease requires exclusion:
- fresh flour and bakery products;
- snacks;
- rich broths;
- vegetable and cereal soups;
- smoked meats;
- milk and dairy products;
- fatty meat, fish;
- canned food;
- barley, millet, pearl barley porridge;
- legumes;
- any sweets;
- vegetables;
- cold and carbonated drinks;
- cocoa or coffee with milk.
- dishes made from lean fish or minced meat, steamed or boiled (soufflé, cutlets, etc.);
- crackers made from premium flour;
- calcined or pureed unleavened cottage cheese;
- weak or low-fat broths with the addition of egg flakes, meatballs, slimy cereal broths (from semolina, rice);
- eggs (soft-boiled, steam omelet);
- butter as a seasoning for dishes;
- grated raw apples;
- pureed oatmeal, rice, semolina porridge with water;
- green tea;
- coffee or cocoa with water;
- berry fruit drinks;
- diluted fruit juices;
- jelly;
- rosehip decoction.
It is important to eat often and in small portions, take additional minerals and vitamins, especially groups B, A, D, E and K. If necessary, the doctor can adjust the given diet option (table 4 according to Pevzner) in accordance with the following parameters:
- features of the pathology;
- severity of clinical manifestations;
- severity of symptoms;
- the presence of concomitant ailments and complications;
- human well-being;
- side effects from drug therapy.
Crohn's disease - treatment with folk remedies
Many alternative recipes help to quickly stop the inflammatory process and restore proper digestion. Folk advice on how to treat terminal ileitis should be combined with drug therapy. Separately, natural remedies have too weak an effect, so they are used as additional health measures.
- chamomile flowers – 30-35 g;
- boiling water – 200-210 ml.
- Pour hot water over the plant material.
- Leave for 1-3 hours.
- Drink the entire dose of medication before meals.
- Repeat up to 5-6 times a day.
Crohn's disease - consequences
The disease in question has a chronic course, therefore it constantly progresses and often leads to dangerous conditions. Crohn's disease - complications:
- release of feces into the abdominal space;
- anal fissures;
- ulceration of the mucous membranes;
- dysbacteriosis;
- colon cancer;
- abscesses;
- fistulas
Due to impaired absorption of nutrients, Barilla Crohn's disease is accompanied by:
- exhaustion with severe weight loss;
- hypovitaminosis;
- dysbacteriosis.
Symptoms
How to recognize ileitis? Symptoms of the disease are often similar to other diseases, so without accurate research it is almost impossible to make a diagnosis. It may be accompanied by completely foreign phenomena at first glance: skin rashes, inflammation of the mucous membranes of the mouth, eyes and nose, pain in the joints and kidneys.
But if some obvious signs appear, you need to be wary and get examined by a doctor. Their intensity will approximately indicate the stage of the disease. The main symptoms of terminal ileitis:
- increased body temperature for no apparent reason;
- abdominal pain similar to an attack of appendicitis;
- fever;
- pain in the ileum;
- colic;
- nausea and vomiting;
- bloating;
- anemia;
- diarrhea mixed with blood, mucus and pus;
- loss of appetite, refusal to eat;
- weight loss.
The more pronounced these manifestations of the disease are, the more severe the disease.
Causes
Intestinal ileitis can occur for a number of reasons, one of them is an infection that provokes the development of an inflammatory process. It can enter the body with food or penetrate from other organs along with mucus and blood. This often occurs due to disturbances in the functioning of the bauhinium valve, which separates the small and large intestines. This causes stagnation of intestinal contents, which leads to infection.
Another reason is poor nutrition and bad habits. Poor quality food, harmful products, and alcohol irritate the intestinal mucosa, which leads to its damage. A sedentary lifestyle further aggravates the situation. This factor generally causes about half of all existing diseases.
Ileitis can also be caused by:
- autoimmune reaction of the body;
- weakening of the immune system after illness, which leads to the development of secondary infection;
- genetic predisposition to gastrointestinal diseases.
The combination of several predisposing factors usually leads to more severe and rapidly progressive ileitis.
Consequences
Without treatment, the disease, which is already difficult to cure completely, tends to take a long time. Chronic ileitis will torment the patient throughout his life. With progressive destruction of the intestinal mucosa, acute attacks of pain, bloody diarrhea become more frequent, and the temperature rises. Inflammation spreads to other parts of the intestine, affecting not only the small intestine, but also other areas.
If no measures are taken, intestinal obstruction develops in the future. Its inner membrane becomes covered with scars and ulcerative lesions, pus accumulates, which leads to extensive peritonitis. Fistulas penetrate even into neighboring organs, metabolic processes are disrupted, and protein deposits accumulate in the organs. In this case, surgery cannot be avoided.