The sphincter of Oddi is a smooth muscle valve (orbicularis muscle). It regulates the flow of digestive enzymes from the pancreas and bile from the gallbladder into the duodenum. From ancient Greek, the term “sphincter” means “I squeeze.” Named after the Italian anatomist and physiologist R. Oddi. The scientist was the first to describe the physiological properties and structure of this valve. When its functions are disrupted, a person begins to suffer from indigestion and constantly feels heaviness in the abdomen.
What is the sphincter of Oddi
Sphincters are all types of formations in the body made from muscle tissue. The Sphincter of Oddi valve is part of the digestive tract, more precisely, the papilla of Vater of the descending duodenum. The organ is complex, as it consists of several types of muscle tissue:
- structure compressing the base of the duodenal papilla;
- tissue called “dilator”, responsible for expansion;
- muscle that goes around the entire papilla of Vater.
The organ is multichannel - pancreatic and bile canals, the area around the common canal. Two systems of the body are responsible for the functionality of the sphincter of Oddi - the nervous and endocrine.
When the functions of the sphincter of Oddi are impaired, patients experience various disorders of the gastrointestinal tract and gallbladder. Often the problem is difficult to diagnose, and incorrect treatment is prescribed due to the fact that the medical specialist simply misses the opportunity to disrupt the functioning of this particular small valve in the complex structure of the duodenum.
Sphincter of Oddi dysfunction (SOD) can be congenital or acquired and is considered a benign clinical change, but requires timely diagnosis and adequate treatment.
Anatomical features
Where is the sphincter apparatus located?
The valve is located on the inside of the duodenum - in the area of the papilla of Vater. The location of the sphincter of Oddi was described by F. Glisson almost 2 centuries ago. Research on this topic was published by R. Oddy in 1888. The opening of the ducts occurs in 80% of cases simultaneously. When they are compressed, a so-called ampoule is formed. Digestive secretions accumulate in it.
The sphincter of Oddi controls the release of digestive juices into the duodenum. It prevents the backflow of small intestinal contents. The valve is responsible for filling the gallbladder and increasing pressure in the ducts to normalize the digestive process.
When digesting food, the sphincter of Oddi contracts rhythmically, which is necessary for the release of bile secretion. When not active, the valve is closed and its contractile function slows down. The secretion is not secreted, but accumulates in the area of the gallbladder.
https://youtu.be/sSR_Wp1tyeY
Symptoms of sphincter of Oddi dysfunction
All types of dysfunction of the sphincter of Oddi are considered clinical changes and not a disease. Such conditions are not characterized by the formation and deposition of stones in the structure of the bile ducts.
There are several types of sphincter of Oddi dysfunction:
- Biliary types I and II with painful attacks lasting 20 minutes or more;
- Dysfunction of the Sphincter of Oddi according to biliary type III - pain is intense, attacks become more frequent, various gastrointestinal disorders begin;
- Pancreatic dysfunction of an organ is a pathology with symptoms of pancreatitis, lumbago or dull pain radiating to the back, which decreases if the position of the torso changes.
If the valve malfunctions, the ducts expand, intestinal contents can enter the bile ducts or bile enters the intestines.
Untimely treatment leads to increased symptoms, the emergence of new health problems - disruptions in intestinal function due to changes in microflora, decreased immunity due to decreased bactericidal activity, obesity, since fats from food are practically not broken down and their circulation in the body is disrupted.
Types of pathological process
In practice, based on differences in the clinical picture, there are 3 main types of DSO:
- biliary;
- pancreatic;
- mixed.
Biliary type
This group accounts for the bulk of the DSO, the signs are as follows:
- painful attacks typical of biliary colic - a sharp cramping, spreading to the back, right shoulder, and sometimes the neck;
- data from instrumental studies – expansion of the common bile duct more than 12 mm;
- increasing the contrast removal time to more than 45 minutes;
- laboratory data - an increase in the level of transaminases and alkaline phosphatase by at least 2 times in repeated tests.
According to a manometric study, the biliary type is divided into 3 types, while in the first type there is almost always stenosis (narrowing) of the sphincter, in the second type narrowing is found in 63% of patients, in the third - in 28%. The rest of the disorders are functional (reversible, dyskinetic) manifestations.
Pancreatic type
This type of DSO is clinically reminiscent of chronic pancreatitis, and only a comprehensive examination allows an accurate diagnosis to be made. The main signs are:
- epigastric pain radiating to the back;
- an increase in the blood plasma enzymes amylase and lipase.
A condition resembling chronic pancreatitis is interspersed with pain similar to hepatic colic. Laboratory research data changes only if the material for research is selected during a painful attack. During the quiet period, practically no deviations can be detected.
Mixed type
If the biliary and pancreatic types are distinguished according to the leading syndrome, then with mixed manifestations of dysfunction of the gallbladder and pancreas are approximately equal. Patients are worried not about acute pain, but about heaviness in the epigastrium, combined with dyspeptic disorders.
Mixed type
Do you have intestinal diseases? — Take the online test!
Symptoms
Symptoms of DSO are nonspecific, so at the initial stage it is difficult to establish that the health problem is caused by dysfunction.
- nausea;
- vomit;
- abdominal pain;
- flatulence;
- heaviness in the upper abdomen.
The symptoms of discomfort are always associated with food intake and occur 3 or 5 hours after eating, especially fatty or fried foods, eating canned food or other irritating foods. Often attacks of pain occur at night.
In some patients, discomfort is accompanied by increased body temperature, chills, and pain on palpation of the abdomen. According to international criteria, pain or discomfort must last for at least 3 months.
At the same time, there are signs that make it possible to distinguish between different types of DSO.
| Type of pathology | Specific manifestations |
| Biliary | severe or moderate pain in the epigastric region or right hypochondrium, lasting at least 20 minutes |
| Pancreatic | pain in the left hypochondrium, which decreases when the torso is tilted forward |
| Mixed | girdle pain |
Loading …
The main cause is considered to be metabolic disorders in the liver, but the following are also important:
- changes in the composition of bile,
- violation of the discharge of bile, its stagnation;
- dyskinesia of the common duct or the junction of the bile and pancreatic excretory ducts;
- careless surgical treatment, during which the sphincter of Oddi is injured, even minimally;
- excessive growth of pathological intestinal microflora.
Gastroenterologists still consider hepatic cell dyscholia to be the main reason for the formation of DSO. This is a condition in which insufficient amounts of cholecystokinin are produced. The substance is a natural regulator of the tone of the gallbladder and its ducts.
Under the influence of cholecystokinin, the sphincter tone increases until the bladder is filled with bile. Once it is full, the sphincter relaxes so that bile can flow freely. After cholecystectomy, the sphincter tone changes, and bile either stagnates or continuously leaks.
This changes the production of hormone-like substances that regulate metabolism in the pancreas, causing secondary pancreatitis.
Diagnostics
When making a diagnosis, they rely on a combination of signs, since there is no single one that would indicate this pathology. Laboratory and instrumental methods are usually combined.
- bilirubin concentration;
- alkaline phosphatase;
- aminotransferases;
- lipases and amylases.
A change in concentration is considered diagnostically significant if venous blood is collected no later than 6 hours from the moment of the attack.
- Ultrasound of the abdominal organs - dilation of the common bile duct and pancreatic duct is determined. To clarify, they give a high-fat breakfast, and then monitor changes in the size of the common bile duct every 15 minutes for an hour. An expansion of more than 2 mm is a clear sign of DSO. To determine the function of the pancreatic duct, a test with secretin is done. Normally, after administration of the medicine, the duct should expand, but return to its original size within half an hour. If the reduction took more than 30 minutes, then this is also a sign of DSO;
- CT scan of the hepatoduodenal section – the size and structure are clearly visible;
- ERCP - retrograde cholangiopancreatography. The method is invasive, that is, it penetrates directly into the sphincter and ducts. Contrast is injected using a probe, then radiography is performed. If the common bile duct is dilated by more than 12 mm, and the rate of contrast evacuation exceeds 45 minutes, then the diagnosis becomes undoubted;
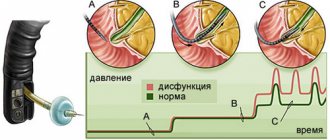
- Manometry is a direct measurement of sphincter tone. A smooth muscle relaxant may be used during the study. The method is technically complex, has many contraindications, and complications occur, so its use is limited.
Treatment
Treatment consists of several important methods that are used simultaneously.
- 4 meals a day, dinner immediately before bedtime - creates conditions for complete emptying of the bladder;
- limiting animal fats (maximum – a little fat in the broth);
- complete exclusion of fried foods;
- a large amount of processed fruits and vegetables, the amount should be sufficient for daily stool;
- consumption of bran.
This is a reduction of body weight to a physiological norm, when BMI (body mass index) corresponds to age and gender. Mandatory minimum physical activity - daily walks, climbing stairs, light fitness.
Causes of pathology
After the discovery of the Sphincter of Oddi, its detailed description and identification of organ dysfunction, for a long time medical specialists studied the reasons that provoke it. Even now, the exact factors for the development of congenital changes have not been determined.
If we talk about acquired dysfunctions of the valve between the duodenum and bile ducts, then their provocateurs are:
- pancreatitis and other diseases of the gallbladder, stones in its ducts;
- inflammatory processes in the gastrointestinal tract and some infectious diseases;
- long-term use of medications from the group of antibiotics;
- duodenitis of the stomach or duodenum;
- postoperative complications when removing the gallbladder;
- disruptions in the functioning of the endocrine or nervous systems.
For some patients, endocrinologists, gastroenterologists, and therapists recommend regularly undergoing comprehensive diagnostics of the functionality of the Sphincter of Oddi.
The risk group includes patients with chronic digestive problems, women taking hormonal medications, pregnant women and those who have reached menopause, patients with underweight, unstable mental health, diabetics and anyone who has crossed the age threshold of 50+.
Diagnostics
It is possible to identify disturbances in the functioning of an organ only through a set of diagnostic measures:
- Analysis of biomaterials - blood (advanced general and biochemical), feces, urine;
- Ultrasound examination of the sphincter of Oddi using provocative agents;
- Cholescintigraphy with an isotope injected into the ducts;
- ERCP (endoscopic retrograde cholangiopancreatography) - helps to accurately determine the diameter of the ducts and the speed and efficiency of their work;
- Manometry using a triple-lumen catheter.
The collection of biological materials is performed during the development or maximum activity of an attack of pain, or within 6 hours after it. This allows you to most accurately determine the indicators of alkalis and other substances that indicate the activity of the organ.
During ultrasound with provocative agents, the exact dimensions of the ducts are determined, blockages and their exact location are identified. Cholescintigraphy shows, using the example of an isotope introduced into the ducts, whether the natural motility of the muscle tissue of the Sphincter of Oddi organ is disrupted. During monometry, a three-lumen catheter is inserted and the pressure level of the muscle tissue is measured.
Forms of the disease
According to the etiological factor, the following forms are distinguished:
- primary (developing without previous pathology);
- secondary (resulting from the underlying disease).
By functional status:
- dyskinesia with hyperfunction;
- dyskinesia with hypofunction.
In order to classify the type of sphincter of Oddi dysfunction in accordance with objective data, the following diagnostic criteria were proposed during the Rome Consensus (1999):
- classic pain attack;
- at least a two-fold increase in the level of liver enzymes (AST, alkaline phosphatase) in at least 2 consecutive studies;
- slowing down the evacuation of contrast agent for more than 45 minutes when performing endoscopic retrograde cholangiopancreatography;
- expansion of the common bile duct up to 12 mm or more.
Types of dysfunction determined according to the criteria:
- Biliary I – characterized by the presence of all of the above symptoms.
- Biliary II is a classic attack of biliary pain in combination with 1 or 2 diagnostic criteria.
- Biliary III – isolated pain syndrome without other signs.
- Pancreatic is a pain syndrome characteristic of inflammatory processes in the pancreas (in combination with an increase in the level of pancreatic enzymes).
Treatment of Sphincter of Oddi dysfunction
Treatment of Sphincter of Oddi dysfunction depends on the reasons that provoked the development of the pathology and the characteristics of the body of each individual patient, and the presence of other chronic diseases.
Treatment should solve several problems at once: eliminating pain, spasms and pressure in the muscle tissues of the Sphincter of Oddi, normalizing the intestinal microflora, treating an infection if it was the provocateur. Treatment for Sphincter of Oddi dysfunction is:
- based on dietary regulation;
- medicinal;
- surgical (endoscopic).
Regardless of the treatment method, it is very important to stick to your diet. It is the basis for normalizing the functioning of the gallbladder, duodenum and the valve between them.
It is necessary to exclude from the diet everything that can provoke increased production of bile, irritate the mucous membranes of the intestines and stomach, refuse unhealthy dishes prepared in haste, in cafes, as well as a raw food diet - vegetables and fruits that have not been heat-treated.
Drug treatment of the Sphincter of Oddi involves taking medications from several groups:
- Painkillers and antispasmodics - analgesics, Papaverine or Drotaverine, No-shpa;
- Antibacterial agents - Enterofuril or Rifaximin, drugs based on fluoroquinolones;
- Medicines with a high content of ursodeoxycholic acid to eliminate biliary insufficiency, for example, Ursosan or Ursofalk;
- Myotropic drugs with a choleretic effect - Mebeverine and Gimecromone.
Drug therapy may be accompanied by folk remedies, but only after approval by a medical specialist. Most often, doctors recommend supplementing the treatment of Sphincter of Oddi dysfunction with decoctions or aqueous tinctures of corn silk, St. John's wort, immortelle or agrimony herb.
Surgical treatment is prescribed only in cases where other methods do not give a positive result. Surgeries for Sphincter of Oddi dysfunction are most often performed using an endoscope. The duodenal papilla of the organ is dissected, balloon expansion of the muscle canals is performed, and temporary stents are installed in them.
It is possible to inject purified medical botulinum toxin to prevent hyperactivity of muscle tissue.
Prevention and prognosis
Disruption of the sphincter of Oddi occurs in every third patient. Doctors make favorable prognoses, but only if patients strictly follow their recommendations.
The main condition for successful treatment is timely, correct diagnosis, identification of Sphincter of Oddi dysfunction, and determination of the type of problem. This is possible when the patient describes his feelings as accurately as possible.
Prevention measures include proper nutrition, giving up bad habits, physical activity and emotional stability. The rules of prevention are simple and easy to follow, especially when it comes to health and a good quality of life.
© 2020 – 2020, . All rights reserved.