It is unlikely that any modern gynecologist will agree to diagnose a woman without using modern research methods. The most accurate endoscopic method for diagnosing intrauterine pathologies is diagnostic hysteroscopy. This endoscopic examination helps many women find out about problems in their gynecological health.
Diagnostic hysteroscopy of the uterus
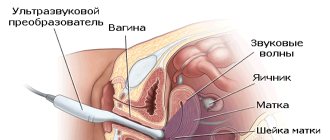
Hysteroscopy of the uterus refers to a procedure for examining the internal surface of the uterus. The procedure is carried out using a fiber optic device that projects the image on a monitor. The doctor moves the device clockwise to assess the condition of the fallopian tubes, endometrium and uterine cavity.
Diagnostic hysteroscopy is, although small, an operation. After all, to penetrate the uterus, it is necessary to expand the lumen of the cervix with mirrors. This requires local anesthesia.
Diagnostic hysteroscopy is called so because this method is the best for diagnosing most diseases of the uterine cavity. At the time of examination, a special probe with LEDs and a micro video camera is inserted into the uterine cavity (this is a hysteroscope).
During diagnostic (office) hysteroscopy, a specialist examines the lining of the uterus to confirm or exclude any disease suspected by the doctor.
This type of study is carried out on an outpatient basis. It is usually prescribed for the initial detection of diseases of the uterus or for monitoring gynecological diseases over time.
Office hysteroscopy usually does not exceed half an hour. Most often, this procedure is recorded on video . This can be convenient for comparative analysis of subsequent studies of the patient.
There is no need to use general anesthesia for diagnostic hysteroscopy. Such a study is absolutely safe, since it does not affect the internal uterine part.
Recovery
Despite the fact that hysteroscopy of the uterus is a minimally invasive surgical procedure, after it is performed, patients have to recover for two weeks. Women must strictly follow all medical prescriptions:
- Take antibiotics.
- Use hemostatic agents in the presence of characteristic discharge. For example, Etamzilat, Diciton.
- Use antifungal drugs, Metronidazole tablets.
- To relieve severe pain and spasms, stronger medications are prescribed.
- If necessary, Oxytocin is used to speed up the intensity of uterine contractions.
Advantages of the method
More recently, for many problems with women’s health (bleeding, habitual miscarriage, chronic inflammation, etc.), diagnostic curettage (popularly “cleansing”) was prescribed. Compared to similar “blind” curettages and other invasive methods, endoscopic hysteroscopy has the following advantages:
- maximum diagnostic accuracy (up to 100%);
- low morbidity with extremely rare complications;
- painless and quick recovery after the study;
- carried out on an outpatient basis;
- the ability to take tissue for examination in a precisely planned location (targeted biopsy);
- optical control of all manipulations in the uterus;
- the possibility of treating uterine pathologies immediately after their diagnosis.
As you can see, this endoscopic method has many advantages over other methods that are less accurate in diagnosis (ultrasound) or more traumatic (diagnostic curettage).
Hysteroscopy method
The hysteroscope is a new generation optical medical instrument for visual diagnosis of the uterus. The tool is a rectangular body with a hose system for supplying gaseous substances and liquids. The hysteroscope is equipped with a video camera and lighting, as well as a channel for introducing special medical devices - forceps, scissors, etc.
Using a hysteroscope, you can not only examine the uterine cavity, but also carry out the necessary surgical or cleansing procedures - remove polyps and neoplasms, remove a piece of tissue for biopsy. The hysteroscope provides a general and panoramic view with magnified images on the monitor. Magnifying the image allows you to examine the mucosa at the cellular level, determining the degree of change in pathological areas.
Hysteroscopy of the uterus is performed both as part of the IVF program and as a method of monitoring treatment results. A distinctive feature of hysteroscopy from abdominal operations is the possibility of performing surgical intervention under the visual supervision of a doctor without the use of a scalpel. The operation is performed in a gynecological chair under intravenous anesthesia with an individual selection of analgesics. In case of contraindications to the use of intravenous anesthesia, mask or other anesthesia is used. The examination is not performed without anesthesia.
Under general anesthesia, the uterine cavity is dilated with a gaseous/liquid substance for better visual inspection. If foreign bodies (remnants of the spiral) and polyps are detected, neoplasms or objects are immediately removed using forceps or clamps. However, if a comprehensive examination is not expected, hysteroscopy is performed not under general, but under local anesthesia.
Indications for hysteroscopy
In what cases does a doctor usually refer a woman for diagnostic hysteroscopy? Most often, a doctor prescribes this test if there is a suspicion of:
- infertility;
- frequent miscarriages;
- pathologies of the structure of the uterus or appendages;
- fistulas between the uterus and other organs;
- presence of fibroids;
- endometriosis;
- adenomyosis;
- suspicion of fragments of the fetal membrane remaining in the uterus (after childbirth);
- complications after childbirth;
- suspicion of a foreign object in the uterine cavity;
- any inflammation in the uterus;
- if you suspect the presence of any tumors (including submucosal fibroids);
- with bleeding of unknown cause;
- with irregular menstrual cycle (at any age).
For uterine fibroids, hysterography is generally irreplaceable. It is this diagnostic method that allows:
- determine the size of the nodes;
- clarify the location of nodal formations;
- choose a treatment method for this pathology.
Recovery after the procedure
The tactics for managing patients after hysteroscopy depends on the general condition of the woman, the type of pathological process and the extent of the operation. Outpatient hysteroscopy does not require compliance with any restrictive measures.
Drugs after hysteroscopy
In the postoperative period of hysteroscopy, the combination drug Safocid (Azithromycin + Fluconazole + Secnidazole) has proven itself well. Safotsid is prescribed to all women who have undergone hysteroscopy on the day of surgery. If surgery does not carry a risk of infectious complications in the postoperative period (removal of endometrial polyp, myomectomy, excision of adhesions), the medicine is prescribed once. In case of a high risk of infection (excision of the septum, chronic endometritis, adenomyosis, foreign bodies), an additional dose of Safocid is taken a week after the operation.
After the hysteroscopy procedure in combination with therapeutic and diagnostic curettage (LDC) of the uterine cavity, bed rest must be observed in the first few hours. The next day, if there are no signs of complications, the patient can be discharged home.
After excision of synechiae, it is recommended to install an intrauterine contraceptive for up to 2 months.
After hysteroscopic plastic surgery of the uterine septum, in some cases estrogen drugs are prescribed to speed up the restoration of the endometrium.
After surgical HS (removal of the septum, synechiae and myomatous nodes, RDV), it is recommended to perform a three-time control ultrasound - after 1, 3 and 6 months. This study is carried out to monitor the functional state of the endometrium after hysteroscopy and identify possible relapses.
Preventive actions
To restore the body after hysteroscopy, it is necessary to observe a number of restrictions and recommendations:
- You should not have sex for a month after hysteroscopy. Regular sexual activity can be carried out only after an ultrasound scan and a gynecologist’s conclusion about the absence of complications of HS.
- It is strongly recommended to stop taking medications that have an antiplatelet effect (acetylsalicylic acid).
- In the first 3 weeks after HS, you need to follow a regimen of restrictive physical activity. From the third week, light aerobic exercise is allowed. Heavy physical activity, accompanied by an increase in intra-abdominal pressure, should be avoided for 3 months.
- For 4 weeks after hysteroscopy, you should not take hot baths, visit saunas, steam baths, swimming pools or solariums.
- Constipation should not be allowed to develop, as this leads to increased intra-abdominal pressure and increases the likelihood of bleeding.
- It is necessary to empty the bladder as often as possible, since its overflow disrupts the blood supply to the uterus, preventing the restoration of the endometrium after hysteroscopy.
- You should stop using hygienic tampons and vaginal suppositories for 3 months after hysteroscopy.
The length of sick leave after hysteroscopy depends on the scope of the intervention. During office hysteroscopy, a certificate of incapacity for work is not issued. Diagnostic HS requires a short period of hospital stay, so sick leave is issued for 2-3 days. Surgical HS sometimes requires a certain period of rehabilitation. Therefore, in some cases, the period of stay on sick leave reaches a week, and if complications develop, up to a month.
In some cases, it is necessary to do a repeat hysteroscopy. Many women worry about the potential harm of this procedure. But it should be said that HS is a rather gentle procedure, especially when it comes to the “office” option. Therefore, even repeated performance of HS is justified if there are appropriate indications.
Contraindications for the study
However, hysteroscopy may not always be used. This diagnostic method is contraindicated for:
- pregnancy (if there are no pathologies);
- heavy uterine bleeding;
- cervical canal cancer;
- narrowed cervix or cervical canal;
- any infections of the female genital area (in the acute stage or recently suffered);
- 3-4 degree of vaginal cleanliness;
- general infectious diseases with intoxication and high fever;
- impaired blood clotting;
- renal or heart failure;
- previous heart attack;
- oncological formations in the stage of decay or growth.
Pregnancy after hysteroscopy
You should plan a pregnancy after hysteroscopy no earlier than a month after the procedure. If, based on the results of an ultrasound and gynecological examination, the doctor concludes that the endometrium and cervix have completely recovered, you can prepare for conception.
In some cases, restoration of the endometrium and myometrium requires more time. After curettage, pregnancy should be planned after 2-3 menstruation. If hysteroscopic treatment of endometriosis was carried out, you should become pregnant after completing a course of hormonal therapy. As a rule, this takes from 3 to 6 months. After myomectomy, excision of synechiae and removal of the septum, a fairly long period of uterine recovery is required, which lasts on average from 4 months to six months.
Preparing for the study
Although this research method is minimally traumatic, it still requires careful preparation. It happens that in the process of taking tests it turns out that hysteroscopy cannot be offered to a woman at the moment (for example, she has been diagnosed with a kidney or acute sexually transmitted infection, etc.)
Therefore, before this endoscopic method, a woman (no later than 2 weeks before hysteroscopy) must:
- Blood test (general, biochemical, coagulability, group determination, Rh factor).
- General urine analysis.
- Study of flora from the genital tract (smear for infection and oncocytology).
- Testing for dangerous infections (HIV, syphilis, hepatitis).
- Colposcopy.
- Ultrasound of the pelvic organs.
- Fluorography.
- ECG.
- Examination by a therapist.
Based on the test responses received, the therapist makes a conclusion about the safety of hysterography for the patient and confirms consent to this type of study.
During the conversation with the therapist, the patient must indicate that she is taking any medications.
It is especially important to tell your doctor about the use of these medications:
- non-steroidal anti-inflammatory drugs;
- anticoagulants;
- blood thinners.
These drugs can cause bleeding and complicate hysteroscopy.
Before the study, it is necessary to prescribe certain medications to women who are at high risk of complications. In this case, antibiotics, antifungal drugs, and tranquilizers may be prescribed. The risk group includes women whose bodies are weakened due to diabetes, obesity, and chronic infections.
Types of hysteroscopy
Office hysteroscopy
Office hysteroscopy is one of the options for performing hysteroscopy, it is performed in the gynecologist’s office, which is where its name comes from, and differs from the classical one in that it is mainly a diagnostic procedure, rather than a surgical intervention.
Hysteroscopy before IVF
Before IVF, hysteroscopy is a recommended procedure to ensure that the uterus is healthy and ready to bear a child. Failed IVF attempts are usually due to embryonic factors such as genetic problems or problems with the woman's uterus. In the past, many fertility clinics routinely performed hysteroscopy on women who had not had IVF cycles to look for abnormal uterine growths or scar tissue and remove them. There are other, non-invasive methods to evaluate the uterine cavity, including hysterosonography, where a small amount of salt water is injected into the uterus and an ultrasound is performed to evaluate the uterus. Hysteroscopy is usually performed in cases where the abnormality has already been identified during other studies.
When is hysteroscopy performed?
Depending on the reason for the examination, endoscopy of the uterus may be prescribed:
- When gynecological diseases are detected - on days 6-9 from the start of menstruation (the first phase of the cycle). It is on these days that the condition of the uterine cavity is ideal for examination with a hysteroscope.
- If you suspect endometrial hyperplasia - any day.
- For intrauterine adhesions - before the onset of menstruation.
- To determine the cause of infertility (assessment of the functional uterine layer) - on the 20-24th day from the start of menstruation (the middle of the secretory phase). At this time, the condition and volume of the internal epithelium is clearly visible.
Where and how is hysteroscopy of the uterus performed?
Most gynecology departments in hospitals have the ability to perform diagnosis or surgery using a hysteroscope. You can find numerous clinical diagnostic centers on the Internet that perform hysteroscopy of the uterus, and read reviews about the professionalism of doctors. After choosing a clinic, you need to wait for the interval between the 7th and 10th day of the menstrual cycle, since on these days ideal conditions have been created in the uterine cavity for the visibility of the endometrium.
An important feature of this manipulation is that the doctor does not make a single incision - the instruments are inserted through the patient’s vagina. Before the operation, the external genitalia and inner thighs are treated with an alcohol solution. Then, using vaginal speculum, the cervix is exposed and treated with alcohol. Afterwards, a probe is inserted that measures the length of the uterine cavity, and then Heger dilators are introduced, which gradually open the cervical canal for the free outflow of fluid when the uterus begins to bleed.
A hysteroscope connected to a light source, video camera, and fluid supply system is inserted through the cervical canal. Multiple enlargements of the uterus on the monitor give the doctor the opportunity to accurately carry out surgical treatment, including curettage, removal of polyps or other necessary procedures. After the operation is completed, the hysteroscope is removed from the cavity, and closure of the cervix occurs spontaneously. For more information about this operation, watch the video:
Hysteroscopy: preparation, implementation, rehabilitation
How to prepare for research
To undergo hysteroscopy, the patient must prepare as follows:
- Avoid using douches and do not use vaginal suppositories or tampons.
- Avoid sexual intercourse 2 days before the study.
- Take food no later than 19 pm, and water no later than 24 hours.
- Mandatory evening enema with clean water.
- Emptying the bladder before the study.
- Taking a shower, treating the pubis and perineum (shaving).
- Take antibiotics 2 hours before the test (to prevent complications).
- Taking mild sedatives for nervous excitement or anxiety (valerian, peony, motherwort).
- Take hygiene products with you (cotton socks and shirt, pads, towel, disposable sheet).
Postoperative period
Consequences
Possible consequences after hysteroscopy:
- After the procedure for medicinal purposes, minor bleeding in the vagina is possible, because... blood vessels are injured. They usually last no more than 5 days.
- Also, after the operation, pain in the lower abdomen of mild to moderate intensity may appear (may radiate to the lumbar region). They usually last no more than the first 10 days.
- After anesthesia, the patient may also be bothered by: general muscle weakness, depressed state, depressed mood. These are the consequences of anesthesia, which may also include chills, fever, and headache.
- Possible perforation of the uterus - puncture of the wall of the organ with a surgical instrument.
Recommendations
To reduce the manifestations of discomfort after hysteroscopy of the uterus, it is recommended to follow simple recommendations for the postoperative period.
Any surgical intervention is associated with the risk of infection. Therefore, if a doctor prescribes antibacterial, anti-inflammatory, antimicrobial drugs, then you should follow the recommendations and observe the frequency, dosage and duration of use. This helps reduce the likelihood of an inflammatory process to a minimum.
If you are very concerned about painful sensations, then it is appropriate to take a drug from the NSAID group, for example, Ibuprofen, Tenoxicam, Nimesulide, Diclofenac, etc. The drugs have a combined effect on the body: they reduce inflammation, reduce temperature, and relieve pain.
If the patient has been bothered by elevated body temperature for more than 5 days, acute pain that is not relieved by painkillers, discharge mixed with pus or an unpleasant odor, heavy bleeding and other alarming symptoms, you should immediately go to the hospital.
What should not be done after hysteroscopy of the uterus?
- Use tampons. It is better to give preference to sanitary pads.
- Have sex. To exclude infection, you should limit sexual activity for the first 2 weeks after surgery.
- Take hot water treatments.
- Use vaginal suppositories.
- Perform intense physical activity.
Pregnancy
When is pregnancy possible after hysteroscopy? Depending on the purpose of the procedure and the established diagnosis, there may be several options regarding the timing of pregnancy:
- If the procedure was carried out for diagnostic purposes, then a healthy woman can become pregnant immediately after it.
- If the procedure was carried out for therapeutic purposes, then the onset of pregnancy is regulated by the characteristics of the pathological process, the volume of surgical intervention, as well as the recommended recovery time (usually 3-6 months).
The time when you can plan a pregnancy without fear for your health and the health of the child is individual in each case and can only be determined by a doctor, having previously assessed all the risks for the woman and child.
How does office hysteroscopy work?
Before the procedure, the doctor lubricates the patient’s genitals and thighs with an antiseptic solution. The cervix is fixed and treated with ethanol. Then a probe is inserted into the cervix, and its length is measured. After dilation of the cervical canal, it is washed, and secretions are drained from it. Then the hysteroscope is inserted into the uterus, from where the mucous membrane and the shape of its cavity and relief are examined. At the same time, data on the color, thickness and condition of the orifices of the fallopian tubes is analyzed.
The normal uterine cavity looks like an oval, with the thickness and vascular pattern of the endometrium according to the cycle:
- before ovulation, the endometrium is abundantly supplied with vessels;
- after ovulation, the endometrium becomes folded and thickened;
- before menstruation, the endometrium becomes thickened, velvety, with areas of hemorrhage.
Procedure technique
The technique of performing hysteroscopy involves a certain sequence of actions:
- The patient is placed on a gynecological chair, her legs are secured with belts.
- The genitals are sanitized using antiseptic solutions.
- Anesthesia is administered.
- The cervix is fixed using gynecological speculum, its canal is expanded to perform rinsing and drainage of fluid.
- Hysteroscopic equipment is inserted into the uterine cavity.
- The mucous membranes are examined, the shape and condition of the organ and pipes are assessed.
- When lesions are identified, therapeutic manipulations are performed.
What is revealed during hysteroscopy
Most often, endoscopy of the uterus reveals the following problems:
- Uterine fibroids : represented by myomatous nodes. It looks like tumors: light pink, round, with smooth edges, they can look like thickenings (protrusions) in the muscle layer. The issue of possible resection of nodes during subsequent hysteroresectoscopic myomectomy is often addressed.
- Formation of polyps : looks like an increase in the mucous membrane with outgrowths of the endometrium. Endometrial polyps can hang into the uterine cavity, be single or numerous. Often, during surgical hysteroscopy, polyps are also removed and sent for histology.
- Endometrial hyperplasia : based on the thickening of the uterine lining, which is measured. With diffuse hyperplasia, the possibility of malignant degeneration of individual growths is determined.
- Internal endometriosis (or adenomyosis) is often difficult to identify and requires sufficient specialist experience. They may appear as white spots with blood spots.
- Glandular endometrial cancer can be suspected and confirmed by histological examination of a piece of tissue. Often this is the only way to timely detect this type of neoplasm.
Hysteroscopy is the most revealing study: it is capable of 100% identifying polyps in the uterus.
Carrying out the operation
The surgical intervention is carried out in the operating room, the patient first undergoes tests and prepares for the procedure. The operation is performed by a qualified gynecologist in the presence of an anesthesiologist, assistant and nursing staff.
The patient is given an anesthetic intravenously or mask anesthesia is used. In exceptional cases, paracervical anesthesia may be used - anesthesia of the tissues of the cervical area. After anesthesia, the doctor expands the cervical canal, inserts a hysteroscope and fills the cavity with gas or solution for better visualization.
The techniques for performing gas and liquid hysteroscopy differ. Let's look at them separately.
With gas
A portion of carbon dioxide is injected into the uterine cavity, expanding the space. The doctor monitors gas pressure and the filling level of the uterus. If the gas is supplied without violating the rules, the patient does not experience complications. If gas supply rules are violated, heart failure and even death can occur.
The gas technique is not used if there are traces of bloody discharge in the cavity - this interferes with clear visualization. Also, gas is not used during surgical interventions.
USEFUL INFORMATION: Embryo cryopreservation
Using solutions
Hysteroscopy using solutions to enlarge the uterine cavity is the most popular procedure. Saline solution, glucose, glycine or simply distilled water are used as the basis for solutions. Can there be complications after the administration of liquid solutions?
Complications are possible with any examination technique. In this case, there is a risk of postoperative infectious tissue damage. However, hysteroscopy of the uterus using solutions is considered the most gentle compared to gas.
The advantage of therapeutic hysteroresectoscopy is the ability to preserve the integrity of the uterine body while eliminating neoplasms from it. A simple operation on the uterus does not require preliminary preparation and can be performed in a gynecologist’s office. We are talking about polyps and small processes, the elimination of which is not difficult.
During a simple operation, fragments of the fertilized egg or an ingrown intrauterine device can be removed. Foreign bodies and a thin intrauterine septum are also removed in the office.
Carrying out complex operations involves a large amount of work; they are carried out using special equipment and in appropriate conditions. Sometimes preparation for a complex operation requires a course of hormone therapy. It is also practiced to combine hysteroscopy with laparoscopy.
Recovery period
Typically, examination with a hysteroscope has no consequences for the patient. Such patients do not need any medical supervision.
Complications and bleeding after hysteroscopy are extremely rare.
But still, after this procedure, the doctor usually gives the woman the following recommendations:
- temperature measurement;
- washing the genitals twice a day;
- exclusion of any stress and sex for a period of 2 weeks;
- taking antibacterial drugs to prevent the development of a bacterial infection;
- assessment of discharge after manipulation: short-term discharge of moderate volume is considered normal;
- to relieve possible pain, analgesics (Analgin, Ibuprom, Nimesil, Baralgetas) are used for 2-3 days;
- it is advisable to use birth control for 1-2 months after the procedure;
- It is not recommended to use vaginal tablets, suppositories or tampons for 2 weeks;
- For several days after the study, visiting a bathhouse, sauna, or swimming pool is undesirable, and bathing in a bathtub is better replaced with a shower.
All such precautions are necessary to prevent complications. Usually, by 3-5 days after the manipulation, the woman returns to her usual lifestyle.
Question answer
Despite the fact that hysteroscopy of the uterus has long been performed in all major hospitals, women continue to ask a large number of questions.
When is the best time to do it?
Hysteroscopy of the uterus is performed on certain days of the menstrual cycle:
- from 5 to 10;
- from 15 to 18;
- in emergencies from 5 to 15.
How long does the procedure take?
The duration of the procedure directly depends on the tasks assigned to doctors and the severity of the pathology. Surgical interventions can be carried out within 10 minutes or last for several hours.
How often can you do it
Due to the fact that hysteroscopy of the uterus is performed under general anesthesia, it cannot be performed often. The frequency of the diagnostic and treatment procedure should be determined by a gynecologist, who will take into account all possible risks and complications for the woman’s health.
Possible complications
Typically, office hysteroscopy rarely causes serious complications for women's health. Let's consider possible complications and help with them:
- Spastic pain in the lower abdomen. This is understandable, since the body underwent instrumental intervention. Here we can take analgesics.
- Flatulence after anesthesia. It is normal and goes away quickly.
- Bleeding. Scanty and spotting discharge after the procedure is considered normal. A violation is indicated if spotting lasts longer than two days after the manipulation. In this case, the doctor usually prescribes hemostatic and contracting drugs.
- Endometritis (inflammation of the uterine lining). Its symptoms are pain in the lower abdomen, bloody purulent discharge from the vagina. Treatment requires comprehensive treatment, using antibacterial drugs and eliminating intoxication.
The first menstrual bleeding after the procedure is not a pathology. If the discharge becomes purulent, abdominal pain and fever appear, you must consult a doctor!
Possible risks
When performing hysteroscopy, the following risks may arise:
- due to a violation of the integrity of the vessels, bleeding opens;
- trauma to the uterus with surgical instruments;
- the occurrence of hematomas;
- infection of the organ, with subsequent development of the inflammatory process.
Attention! After hysteroscopy of the uterus, patients may experience pain in the lower part of the peritoneum. For several days, women will experience bloody discharge, which may contain clots and purulent impurities.
Hysteroscopy before IVF
Hysteroscopy before IVF is very desirable, but not strictly necessary.
Office hysterography is especially often used for accurate diagnosis before in vitro fertilization surgery. Sometimes it is combined with a small curettage (therapeutic and diagnostic hysterography).
Diagnostic hysteroscopy before IVF allows you to choose the most optimal IVF protocol scheme and the most effective treatment method in cases of many disorders.
After all, even initially successful IVF does not always end in normal pregnancy and the birth of a full-fledged baby. And the reason for this is precisely the diseases of the female genital area that were not diagnosed in a timely manner and not cured.
Many intrauterine diseases of a woman can negate the expensive procedure of in vitro fertilization.
That is why it is best to conduct a hysteroscopic examination before repeated deaths occur during embryo transfer or termination of such a desired pregnancy. Until now, the ultrasound method has been used in this case. However, he is not able to identify all uterine pathologies in the initial stage.
The use of hysteroscopy during IVF allows:
- assess the patency of the cervical canal;
- cauterize erosion;
- diagnose undiagnosed endometrial pathologies;
- perform a cervical biopsy;
- remove polyps;
- cut the adhesions.
Hysterography is especially recommended before IVF for the following disorders:
- narrowing of the cervical canal (polyps, narrowing);
- intrauterine pathologies (hyperplasia, fibromatous nodes, endometriosis, dystrophy);
- several unsuccessful IVF attempts.
Beautiful women should not be afraid of office hysteroscopy or neglect this type of examination. In many situations, this endoscopic method is simply irreplaceable, as it can promptly identify serious gynecological pathologies, which include glandular cancer of the uterus. In other cases, the hysteroscopy method makes it possible to promptly identify and treat intrauterine pathologies, thereby facilitating the successful completion of an expensive IVF procedure.
What happens during hysteroscopy
Hysteroscopy is usually performed in outpatient or day hospitals. This means that the patient does not have to stay in the hospital overnight. Hysteroscopy is routinely performed on days 7-9 of the cycle, and menstrual bleeding (periods) is a relative contraindication to the procedure
It may not be necessary to use an anesthetic for the procedure, although local anesthesia (where medications are used to numb the cervix) is sometimes used. General anesthesia (narcosis) may be used if the patient is scheduled for hysteroscopy for treatment during the procedure.
During hysteroscopy:
the patient lies on a chair; an instrument called a speculum may be inserted into the vagina to keep it open (the same instrument used for the cervical screening test), although this is not always necessary; The hysteroscope is placed into the uterus and fluid is gently pumped inside to make it easier for the doctor to see inside; the camera sends images to a monitor so the doctor can detect and/or treat any abnormalities.
A hysteroscopy can take up to 30 minutes, although it may only last 5-10 minutes if it is only done to diagnose a condition, or investigate symptoms.
During the procedure, patients may experience some discomfort, similar to periods of cramping, while it is performed, but it should not be painful.
This type of modern research for diagnostic and therapeutic purposes
Diagnostic hysteroscopy consists of an internal examination of the uterus using specialized probes with a built-in microvideo camera. A diagnostic test is necessary to establish or clarify a gynecological diagnosis.
Surgical intervention in the form of hysteroscopy is used in the following cases:
- removal of benign tumors such as uterine fibroids;
- there is excessive growth of the endometrium, which is uterine polyps;
- if endometrial cancer develops;
- removal of residual placental particles after childbirth;
- there are foreign bodies in the uterine cavity;
- perforation of the uterine walls.
As a diagnostic test, this procedure is often used to clarify or confirm the following factors and diagnoses:
- to identify the causes of uterine bleeding;
- disruption of the monthly menstrual cycle in women, including during the premenopausal period;
- various discharges in excessive quantities;
- bleeding during menopause;
- inability to bear a child, constant miscarriages or suspicion of infertility;
- to clarify the consequences, as well as as a control diagnosis after previously undergone gynecological surgical interventions;
- clarification of results and obtaining more accurate information during the course of hormone therapy;
- if the postpartum period is severe or with the development of negative consequences and complications.
Despite the fairly wide range of indications for the procedure, there are factors that may become an obstacle to the use of such a diagnostic method.
Contraindications include:
- various infectious diseases (sore throat, flu, pneumonia);
- the presence of third or fourth degree of purity of the patient’s vaginal smear;
- serious diseases and pathological processes of the cardiovascular system, as well as kidney or liver diseases;
- normal pregnancy;
In addition, contraindications include the presence of profuse uterine bleeding.
Hysteroscopy - what is it?
Modern medicine knows many different diseases of the genital area. And in some cases, to make a final diagnosis, the doctor needs to carefully examine the inner wall of the uterus. Hysteroscopy provides exactly this opportunity.
What is this procedure? Its essence is quite simple - the examination is carried out using a special hysteroscope apparatus. It is equipped with optical fiber, which allows the doctor to carefully study the structure and, if present, pathology of the inner wall of the uterus, viewing them on a large screen.
In fact, obstetrics and gynecology widely use this technique for both diagnostic and therapeutic purposes.
Main complications and their treatment
The presence of mild nagging pain in the lower abdomen is a normal reaction of the body to intervention. If the pain is strong enough, unabated, and difficult to relieve with painkillers, you should consult a specialist, as this may be an indicator of serious complications as a result of the operation. There are a number of other problems that the patient may encounter after uterine histology and surgical procedures.
Surgical complications
Surgical consequences resulting from hysteroscopy are observed mainly after the removal of polyps, fibroids and other formations in the uterine cavity. Similar complications may arise in the event of injury to the cervix as a result of collection of the endometrium during histology.
Treatment in this case includes examination using laparoscopy and possible suturing of injured tissue. If the damage is small, a course of antibiotics, anti-inflammatory drugs and medications is prescribed, the effect of which is aimed at contracting the uterus.
In rare cases, the results of liquid hysteroscopy of the uterus lead to the development of air embolism. This is a rather dangerous complication that occurs as a result of air entering the patient’s circulatory system. Sometimes an air embolism can even be fatal. If this disease is detected, immediate resuscitation measures are required.
During outpatient recovery, it is necessary to take your own temperature daily. It is its increase that becomes the first sign of the onset of the inflammatory process.
Heavy discharge
Slight pain and light bleeding are the norm after hysteroscopy and histology of the uterus. But you need to learn to distinguish them from inflammatory processes and other complications.
Moderately spotting blood discharge of normal color without a strong odor is the norm in the first time after hysteroscopy. Subsequently, they may change to brownish, yellow or bloody.
Too much discharge, with the presence of clots, an atypical color with a strong smell of rot, is an indicator of the presence of infectious processes or an existing injury. The complete absence of blood discharge is also considered abnormal - this may be a sign of pathology or the development of inflammation. In these cases, you should definitely consult a gynecologist.
Does hysteroscopy require special training?
Regardless of the purpose of the study, the doctor must draw up a plan for preparing the patient. The standard plan includes a number of activities:
- instrumental gynecological examination and manual vaginal examination;
- laboratory tests of blood, urine, vaginal and urethral smears;
Before hysteroscopy, you must undergo a gynecological examination and smear tests.
- consultation with a general practitioner;
- examination by an anesthesiologist to decide on the type of anesthesia;
- fluorographic examination of the lungs;
- electrocardiogram;
- according to indications - ultrasound examination of the pelvic organs and colposcopy.
In addition, if necessary, additional consultations with specialists and clarifying studies may be prescribed.
Preparation
Preparation for hysteroscopy with RDV is standard - as for minor gynecological operations, these are detailed tests:
- blood and urine
- on the microflora of the genital tract,
- for common infections (HIV, hepatitis, syphilis).
This implies a complete gynecological examination and for anesthesia, an ECG and fluoroscopy of the lungs, consultation with a therapist and other specialists are required, if the state of health requires it.
On the eve of the manipulation, the colon is cleansed; before the intervention, you must refuse to eat.
Hysteroscopy with RDV requires a short hospital stay for optimal preparation and a calm attitude. The best time is three to four days before the expected menstruation, when, under the influence of hormones, the cervical canal has expanded as much as possible, and the endometrium is almost ready for rejection.
Consequences of hysteroscopy
Since all manipulations are carried out under the control of a special video camera, this helps reduce the risk of serious complications several times. But despite this, every patient should know how to prepare for hysteroscopy of the uterus, and what consequences may arise after this.
If a biopsy was taken during hysteroscopy, the doctor must record the histology results and interpret them. Depending on this, the issue of further treatment and when to plan a pregnancy after hysteroscopy will be decided.
Most often, complications arise after unsuccessful diagnostic hysteroscopy or therapeutic hysteroresectoscopy. In gynecological practice, the following types of complications are distinguished:
- surgical pathologies;
- bleeding;
- endometritis;
- infection;
- infertility;
- air embolism.
Surgical complications of hysteroresectoscopy include uterine perforation, which occurs due to mechanical damage to the walls. This pathology is usually observed after unsuccessful expansion of the cervical canal or probing of the uterine cavity. During hysteroresectoscopy, damage to the intestinal walls can also occur.
Surgical complications usually occur in elderly patients, with poor visibility due to the introduction of the device (hysteroscope). This could be an operation to remove a polyp in the uterus or any other surgical intervention. Treatment after hysteroscopy in this case will include laparoscopy, during which the resulting hole is sutured. For a small hole, conservative therapy is carried out, which consists of a course of antibiotics and drugs to contract the uterus to stop the bleeding.
Endometritis may appear after the introduction of pathogenic organisms into the uterine cavity. It is accompanied by severe pain in the lower abdomen, purulent or bloody discharge and high fever. Treatment of endometritis involves the use of detoxification therapy and antibiotic therapy.
In some cases, air embolism may occur, which can sometimes be fatal. In order to avoid this, during the procedure the doctor must carefully ensure that air does not enter the system of tubes through which the liquid is supplied.
Advice: recommendations after hysteroscopy, which will be given by the attending physician in the postoperative period, will help to avoid complications.
Bleeding after hysteroresectoscopy
If heavy bleeding from the genital tract does not go away within a few days, consult a doctor immediately
Uterine bleeding can occur after hysteroscopy or surgery for various reasons. Such consequences occur against the background of perforation or trauma to the cervix. Treatment depends on the nature and severity of bleeding. In the presence of deep damage to the myometrium and large vessels, laser coagulation is performed. Also, if there is no proper effect, a hysterectomy (removal of the uterus) may be prescribed to eliminate the complication. In order to avoid such consequences, all manipulations should be carried out with caution. It is imperative to consult a doctor.
Indications
So, we should start with the diseases and pathological conditions for which the study is carried out. Indications for endoscopic diagnostics are:
- Heavy menstrual bleeding. Heavy periods are usually associated with hormonal imbalances in a woman’s body. Hormonal levels can change as a result of age-related reasons, incorrect hormonal therapy and contraception.
- Contact bleeding from the vagina (after sexual intercourse, gynecological examination). Blood from the vagina, in this case, may indicate damage to the cervix. Diseases of the uterine cervix, in which blood may be released, include: erosive changes in the cervix, leukoplakia, polyps, erythroplakia, and cancer.
- Bleeding after menopause. Uterine hemorrhages after the onset of menopause can be associated with uterine fibroids, uterine polyps, endometriosis, ovarian diseases, endometrial hyperplasia, and malignant neoplasms.
A – norm; B – endometrial hyperplasia
- Suspicions of pathological processes in the endometrium, when other diagnostic methods do not allow an accurate diagnosis.
- Monitoring the effectiveness of treatment of certain gynecological diseases. In this case, the condition of the endometrium and other indicators of hormonal influence are monitored.
- Pathological course of pregnancy. In this case, the procedure is performed only if there is a high risk to the life of the pregnant woman. Otherwise, conducting research is strictly prohibited, as it can lead to injury to the unborn baby and disruption of the amniotic sac.
- Difficulty in removing the intrauterine device. An intrauterine device is inserted into a woman’s body for a certain period of time. If the product is installed incorrectly or the coil is overdue, problems may arise when removing it. In such cases, hysteroscopy may be used.
Hysteroscopy can be used to remove an ingrown intrauterine device.
Is it possible to use suppositories before hysteroscopy?
Vaginal suppositories are used primarily for local therapy and have an anti-inflammatory or antiseptic effect. Their use before hysteroscopy is not prohibited, but the choice of drugs must be treated with extreme caution. It is advisable to use products approved or recommended by the gynecologist.
Important! Suppositories are mandatory if an imbalance in the vaginal microflora was identified during the preliminary examination.
Hormonal suppositories and medications that contain hormones and act in the same way as intrauterine contraceptives should be stopped at least a week before surgery. The use of any suppositories on the day of the procedure is undesirable. In some cases, it is advised to stop using them the day before the planned hysteroscopy.
Treatment
The basics of therapy during the recovery period can vary greatly depending on: the type of intervention, the initial diagnosis, the general condition of the patient, the complexity and extent of the procedure performed, its result and many other factors.
If the purpose of histology was curettage of the endometrium, removal of placental tissue or remnants of the fertilized egg, as well as if resection of uterine fibroids, polyps and synechiae was performed, treatment will be based on taking tablet antibiotics.
Alternative methods
Today there is nothing to replace diagnostic hysteroscopy with RDV, but treatment without RDV is possible and has advantages for some pathological conditions of the uterine mucosa.
Modern hysteroscopes allow the use of laser and electric current to remove large amounts of tissue; the disadvantage is that nothing remains for analyzing the cell structure under a microscope, because the entire pathological substrate is “burned out”.
With electrical destruction, the likelihood of bleeding is higher, with laser ablation it is lower than with conventional RDV. Laser ablation virtually eliminates perforation of the uterine wall.
In terms of the stages of manipulation, hysteroscopy using modern alternative technologies is no different from the standard RDV.
Our clinic conducts a full range of gynecological examinations; we will choose the most optimal and informative for you, making your stay within the walls of our clinic not only healthy, but also enjoyable.
Book a consultation 24 hours a day
+7 (495) 151-14-53
Contraindications
Contraindications to GS are:
- Chronic diseases in the stage of decompensation.
- Acute infectious diseases.
- Sterility of the genital tract III-IV degree, including thrush; in this case, before performing hysteroscopy, preliminary treatment is required, followed by re-analysis of smears.
- Cervical stenosis.
- Common cervical cancer.
- Pregnancy.
- Previous uterine bleeding.
- Pathology of the blood coagulation system.
- Shock.
It should be noted that some of these contraindications are relative. Therefore, in emergency situations, the doctor is required to weigh the benefits of hysteroscopy and the potential harm due to the presence of these contraindications.
What can you see during the examination?
What does hysteroscopy allow you to see and what procedures can be performed with its help in the uterine cavity?
- assess the condition of the mucous membrane;
- check the presence and size of the orifices of the fallopian tubes;
- diagnose intrauterine neoplasms;
- diagnose organ malformations;
- establish the presence of fetal remains or amniotic sac after a medical abortion or miscarriage;
- evaluate the effectiveness of hormone therapy for certain gynecological problems;
- confirm the need for surgical intervention;
- take a piece of tissue for histological examination;
- control the process of “scraping” of the uterine cavity in order to prevent the development of complications.
Despite the universality of the procedure, not all women can undergo the study.