From this article you will learn: what mitral stenosis is, the main causes of its occurrence. How the pathology develops, its characteristic symptoms. Methods of diagnosis and treatment, prognosis for recovery.
Author of the article: Victoria Stoyanova, category 2 doctor, head of the laboratory at the diagnostic and treatment center (2015–2016).
Article publication date: 07.17.2017
Article updated date: 06/02/2019
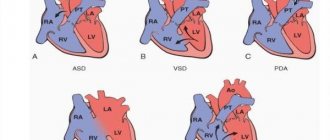
A narrowing of the opening between the left atrium and the ventricle that impedes intracardiac blood flow is called mitral valve stenosis.
During normal heart function, blood flows freely from the atria into the ventricles at the moment the ventricles relax after cardiac output and myocardial contraction (diastole). In pathology for various reasons (infective endocarditis, atherosclerotic plaques), the left atrioventricular orifice decreases in size, narrows (scarring or hardening of valve tissue, fusion of the leaflets), creating an obstacle to normal blood flow:
- insufficient blood enters the left ventricle, cardiac output decreases;
- in the left atrium, due to pressure, the resistance of the walls of the heart chamber increases, they thicken (hypertrophy);
- pulmonary hypertension develops (increased blood pressure in the pulmonary vessels);
- the right ventricle gradually increases in volume (dilatation), its contractile function is impaired.
The result is serious disruption of the heart muscle and blood circulation.
This variant of stenosis (narrowing of the left atrioventricular orifice) refers to acquired defects, the pathology is dangerous for the development of serious complications - malignant arrhythmia (its atrial fibrillation form), death from thromboembolism, bleeding (rupture of aneurysm of the pulmonary vessels), pulmonary edema.
It is impossible to completely cure stenosis; surgical methods can significantly improve the prognosis and prolong life by stages 2 (with mild circulatory disturbances, shortness of breath after exercise) and 3 stages of the disease (with severe circulatory disturbances, shortness of breath at rest).
Before and after the operation, the pathology is treated by a cardiologist, and a cardiac surgeon operates on the narrowing.
What it is?
The mechanism of pathology is as follows:
- The mitral valve is located on the border of the atrium and ventricle of the heart on the left.
Its role is to pass blood from the left atrium to the left ventricle. Normally, this valve is a hole with an area of 4-6 cm2 with two connective tissue flaps. When blood fills the left atrium, the valve flaps open under pressure towards the ventricle and let a portion of blood pass there, and then close tightly. - For a number of reasons, the connective tissue valve leaflets can be subject to organic damage, resulting in scarring degeneration of their tissue.
- Scars, adhesions and adhesions lead to a gradual narrowing of the valve opening - at least 2-3 times. This pathological condition is called mitral stenosis.
- The narrowed opening prevents normal blood flow, since the portion of its simultaneous ejection from the atrium into the ventricle is reduced. Because of this, not all the blood from the atrium is pumped into the ventricle - a situation is created in which the left atrium becomes overfilled and congestion begins in it.
- As a result of constant overflow of blood, the left atrium begins to stretch and increase in size - this is how it “adapts” to the current situation. Following this, the right ventricle, the previous link in the blood circulation, hypertrophies.
- Gradually, the compensatory mechanism of hypertrophy of the left atrium and right ventricle exhausts itself - heart failure and persistent circulatory disorders develop, including pulmonary hypertension.
Complications of the operation
Both in the early and late postoperative periods, there is also the possibility of developing complications:
- infective endocarditis (development of bacterial inflammation on valve leaflets, including biological artificial ones);
- the formation of blood clots as a result of the operation of a mechanical prosthesis with the development of thromboembolism - the separation of a blood clot and its release into the vessels of the lungs, brain, and abdominal cavity;
- degeneration (destruction) of an artificial biovalve with repeated development of hemodynamic disorders.
The doctor’s tactics boil down to regular examination of patients using echocardiography, monitoring the blood coagulation system, lifelong prescription of anticoagulants and antiplatelet agents (clopidogrel, warfarin, dipyridamole, chimes, aspirin, etc.), antibiotic therapy for infectious diseases, abdominal surgeries, and minimal therapeutic and diagnostic procedures in gynecology, urology, dentistry, etc.
Statistics
Mitral stenosis is a commonly diagnosed acquired defect of the mitral heart valve.:
- the disease is detected in approximately 90% of all patients with acquired heart defects;
- 1 person out of 50-80 thousand suffers from this disease;
- in 40% of cases this is an isolated pathology, in the rest it is combined with other anatomical defects in the structure of the heart;
- the risk of clinical manifestations of the disease increases with age: the most “dangerous” age is 40-60 years;
- women are more predisposed to this disease than men: among patients with this defect, 75% of the fairer sex.
Diagnostic methods
Diagnosis begins with examination and conversation with the patient. Determine the presence of characteristic symptoms. After this, electrocardiography is performed. The results of the procedure show enlargement of the atrium on the left and ventricle on the right.
To confirm the presence of pathological changes, two-dimensional and Doppler echocardiography is used. The study determines how severe the mitral regurgitation is and how narrowed the lumen is.
To determine whether or not there are thrombi in the cavity of the left atrium, transesophageal echocardiography is performed.
To identify pathological changes in the lungs, radiography is necessary.
If the diagnosis is confirmed and a stage of decompensation is observed, it is necessary to undergo an examination every year, including ultrasound, daily Holter monitoring, and biochemical blood tests.
In cases where surgical treatment is necessary, catheterization of the heart and great vessels is performed.
Classification of types and degrees
The disease is classified according to 2 bases. As the area of the mitral orifice decreases, 5 successively worsening degrees of the disease are distinguished :
| Degree | Qualitative definition of stenosis | Mitral orifice area (in cm2) | Clinical signs |
| First | minor | more than 3 | no symptoms |
| Second | moderate | 2,3-2,9 | symptoms of the disease appear after physical activity |
| Third | expressed | 1,7-2,2 | symptoms appear even at rest |
| Fourth | critical | 1-1,6 | severe pulmonary hypertension and heart failure |
| Fifth | terminal | the lumen is almost completely blocked | the patient dies |
Depending on the type of anatomical narrowing of the valve opening, the following forms of mitral stenosis are distinguished:
- “jacket loop” type - the valve flaps are thickened and partially fused to each other, easily separated during surgery;
- “fish mouth” type - as a result of the proliferation of connective tissue, the valve opening becomes narrow and funnel-shaped, such a defect is more difficult to surgically correct.
Stages of the disease (according to A.N. Bakulev):
- compensatory – the degree of narrowing is moderate, the defect is compensated by hypertrophy of the heart, there are practically no complaints;
- subcompensatory - the narrowing of the hole progresses, compensatory mechanisms begin to exhaust themselves, the first symptoms of trouble appear;
- decompensation – severe right ventricular failure and pulmonary hypertension, which quickly worsen;
- terminal – stage of irreversible changes with a fatal outcome.
Prevention
It is impossible to completely exclude this disease. But some measures can be taken to reduce the risk of a pathological process. To do this, you should apply the following simple rules in practice:
- nutritious nutrition, with a full range of vitamins and minerals;
- moderate physical activity;
- walks in the fresh air, good rest.
You should, if not completely eliminate, then at least reduce stressful and nervous situations in your life.
It is very important to begin treatment for sore throat in a timely manner. It is this disease that can provoke ailments associated with the cardiovascular system. Monitor your health and seek medical help promptly.
Valve Disease Clinic
The clinical picture depends on the stage and degree of narrowing of the bicuspid valve. With a narrowing of up to 3-4 sq.cm, there are no complaints for a long time; with critical stenosis (less than 1 sq.cm), complaints are always present.
The appearance of a patient with mitral stenosis is characterized by:
- Forced position - sitting with emphasis on the palms.
- "Mitral butterfly" on the face.
- Noisy heavy breathing.
- Marked weakness.
Due to pulmonary hypertension, patients complain of shortness of breath , which gradually becomes constant.
A decrease in cardiac output leads to cardialgia (non-anginal pain in the heart). As a rule, the pain is localized at the apex, accompanied by a feeling of interruptions, freezing or uneven heartbeat. In the lying position, the patient's condition worsens. A characteristic symptom is “night apnea” - sudden suffocation during sleep . Patients sleep on a high headboard and suffer from insomnia.
In the stage of decompensation (right ventricular dilatation), cardiogenic edema develops. Edema increases in the evening, is localized in the lower extremities and has an ascending nature. In the right hypochondrium, nagging pain appears due to stretching of the liver capsule, which protrudes from under the edge of the costal arch. Fluid accumulates in the abdominal cavity (ascites), and the subcutaneous veins of the abdomen dilate (symptom of the “head of the jellyfish”).
With dilatation of the right ventricle, visible pulsation in the area of the costal angle (cardiac impulse), hemoptysis and pulmonary edema develop.
Auscultatory signs
When listening to the heart, a complex of specific symptoms is revealed that make up the auscultatory picture of mitral stenosis:
- The opening tone of the bicuspid valve is heard before the first sound; with mitral stenosis, it is caused by the splitting of the 2nd tone into two components.
- Clapping first tone.
- At the second point of auscultation there is an accentuated second tone.
- At the apex of the heart there is a diastolic murmur, which intensifies after test physical activity in the presence of mitral valve stenosis.
- Extrasystoles and tachycardia may be heard.
The three audible tones form a specific symptom that is detected only in this disease - the “quail rhythm”. With developing pulmonary edema, moist fine rales are heard in the lower parts of the pulmonary fields.
Auscultation with mitral valve stenosis can show disorders as they arise.
More about the auscultatory picture of mitral valve stenosis in this video:
Description of hemodynamics
The disease refers to defects with enrichment of pulmonary circulation. The narrowing of the valve opening causes an increase in pressure first in the left atrium, then in the pulmonary veins. The atrium enlarges and dilates, its contractility decreases.
Pulmonary hypertension develops, which causes contraction of the muscle cells of the capillaries of the lungs . In response to microvascular spasm, the pressure in the pulmonary trunk system and the right (venous) ventricle increases. The right ventricle expands and gradually dilates. Venous stagnation develops in the systemic circulation.
Hypoxia caused by a lack of arterial blood first manifests itself as acrocyanosis. Subsequently, cyanosis becomes universal (affects all skin and mucous membranes).
This video describes the hemodynamics that are characteristic of mitral valve stenosis:
Symptoms
Mitral valve stenosis can be asymptomatic for a long time. From the moment of the first infectious attack (after rheumatism, scarlet fever or tonsillitis) until the first characteristic complaints of a patient living in a temperate climate appear, about 20 years may pass, and from the moment of the appearance of severe shortness of breath (at rest) until the death of the patient, about 5 years pass. In hot countries, this heart defect progresses faster.
With mild mitral valve stenosis, patients do not complain, but upon examination, many signs of disturbances in the functioning of the mitral valve may be revealed (increased venous pressure, narrowing of the lumen between the left atrium and the ventricle, an increase in the size of the left atrium). A sharp rise in venous pressure, which can be caused by various predisposing factors (physical activity, sexual intercourse, pregnancy, thyrotoxicosis, fever and other conditions), is manifested by shortness of breath and cough. Subsequently, as mitral stenosis progresses, the patient's endurance to physical activity sharply decreases, they subconsciously try to limit their activity, episodes of cardiac asthma, tachycardia, arrhythmias appear (extrasystole, atrial fibrillation, atrial flutter, etc.) and pulmonary edema may develop. The development of hypoxic encephalopathy leads to dizziness and fainting, which are provoked by physical activity.
A critical point in the progression of this disease is the development of a permanent form of atrial fibrillation. The patient experiences increased shortness of breath and hemoptysis. Over time, signs of pulmonary congestion become less pronounced and proceed easier, but constantly increasing pulmonary hypertension leads to the development of right ventricular failure. The patient complains of swelling, severe weakness, heaviness in the right hypochondrium, cardialgia (in 10% of patients) and signs of ascites and hydrothorax (usually right-sided) may be detected.
When examining the patient, cyanosis of the lips and a characteristic raspberry-cyanotic blush on the cheeks (mitral butterfly) are determined. During percussion of the heart, a shift of the borders of the heart to the left is detected. When listening to heart sounds, an increase in the 1st tone (clapping tone) and an additional 3rd tone (“quail rhythm”) are determined. In the presence of severe pulmonary hypertension and the development of tricuspid valve insufficiency, bifurcation and intensification of the second tone is detected in the second hypochondrium, and a systolic murmur is detected above the xiphoid process of the sternum, which intensifies at the peak of inspiration.
Such patients often have diseases of the respiratory system (bronchitis, bronchopneumonia and lobar pneumonia), and the detachment of blood clots forming in the left atrium can lead to thromboembolism of the vessels of the brain, limbs, kidneys or spleen. When blood clots block the lumen of the mitral valve, patients experience severe chest pain and fainting.
Also, mitral valve stenosis can be complicated by relapses of rheumatism and infective endocarditis. Repeated episodes of pulmonary embolism often result in the development of pulmonary infarction and lead to the death of the patient.
Etiology and risk factors
The causes of the disease in most cases are:
- rheumatic diseases (rheumatism, systemic lupus erythematosus, scleroderma) – 80-90% of cases;
- atherosclerosis – 6%;
- infectious diseases (angina, syphilis and other sexually transmitted diseases, sepsis, tick-borne diseases) – 6%;
- infective endocarditis;
- heart muscle injuries;
- valve calcification of non-rheumatic nature;
- heart tumors.
Thus, it can be seen that there is rheumatic and non-rheumatic mitral valve stenosis.
Risk factors are the frequency and severity of infectious diseases, inadequate treatment of autoimmune and other provoking diseases, genetic predisposition (pathology is transmitted through the maternal line in 25% of cases).
Main causes of mitral valve stenosis
The most common causes of scars and adhesions (adhesions) of valve leaflets are tissue damage as a result of an infectious disease, metabolic disorders (hyperlipidemia, the formation of cholesterol plaques) and heart injury:
- rheumatism, rheumatoid arthritis and infective endocarditis (80%);
- atherosclerosis;
- calcification (hardening of tissues as a result of calcium deposits in cells);
- syphilis;
- myxoma (benign tumor of the heart);
- congenital heart disease with atrioventricular septal defect (Lutembashe syndrome);
- aortic insufficiency (deficiencies of the aortic valve leading to disturbances in intracardiac blood flow);
- intracardiac thrombi;
- heart and chest injuries;
- ionizing radiation;
- intoxication with drugs (preparations based on plant extracts of wormwood).
Sometimes the cause of repeated narrowing of the mitral valve is surgery (30%) to eliminate stenosis (commissurotomy, valve replacement).
Symptoms of pathology
Manifestations of the defect are divided into pulmonary, cardiac and general.
General symptoms:
- Decreased performance.
- Insomnia.
- Weakness.
- Forced sitting position.
- Pale skin combined with cyanosis.
Pulmonary symptoms:
- Dyspnea.
- Difficulty noisy exhalation.
- Cough for no apparent reason.
- Tendency to respiratory diseases.
- In later stages - hemoptysis.
Heart symptoms:
- Frequent heartbeat.
- Cardialgia.
- Reduced blood pressure.
- Atrial fibrillation.
- Ascending edema of the lower extremities.
Features of the skin
The first manifestation of the defect is pale skin . As hypoxia progresses, acrocyanosis develops - blue discoloration of the lips, earlobes, and fingertips. In the stage of decompensation, cyanosis becomes widespread, and bluish discoloration of the mucous membranes occurs.
A specific symptom is characteristic - “mitral face” - pronounced pallor of the face combined with a crimson blush on the cheeks and cyanosis of the lips. Despite the presence of these symptoms, a diagnosis is not made based on skin changes.
Causes of hemoptysis
The appearance of blood streaks in the sputum is due to cardiogenic pulmonary edema.
Developing pulmonary hypertension underlies spasm of microvasculature vessels - capillaries, arterioles and venules.
Microvascular spasm further aggravates hypertension , resulting in damage to the vascular walls. Through damaged vessels, blood begins to flow into the lung tissue. During the process of self-cleansing of the lungs, blood mixes with mucus and is coughed up by the patient (hemoptysis).
Heart rhythm disturbance
The disease is characterized by early onset of arrhythmia. Rhythm disturbances are caused by hypertrophy of the venous ventricle and left atrium , as a result of which the heart chambers cannot contract simultaneously. The following types of arrhythmias are distinguished:
- Atrial fibrillation.
- Ventricular tachycardia and fibrillation.
- Atrial flutter.
- Atrioventricular blockade.
- Extrasystole.
Pressure gradient
The pressure gradient is the difference in pressure between the left chambers of the heart. Normally, the pressure in the left ventricle is 33-45 mmHg, in the atrium - 3-6 mmHg.
With bicuspid valve stenosis, the pressure initially becomes equal in both chambers . As it progresses, the pressure in the atrium becomes greater than in the ventricle, on the basis of which the following classification of the defect is made:
- Slight stenosis (gradient is 7-11 mmHg).
- Moderate (12-20 mmHg).
- Significant (more than 20 mmHg).
The magnitude of the gradient also reflects the degree of pulmonary hypertension.
Clinical guidelines on mitral valve stenosis from the Ministry of Health of the Russian Federation can be downloaded from this link.
Drug treatment of the disease
Treatment of mitral disease is divided into conservative and surgical. These two methods are used in parallel, since drug support for the patient is especially important before and after surgery.
Drug therapy includes the prescription of the following groups of drugs:
- Beta blockers are drugs that reduce the load on the heart by slowing the heart rate and reducing vascular resistance, especially when blood stagnates in the vessels. Concor, Coronal, Egilok, etc. are most often prescribed.
- ACE inhibitors – “protect” blood vessels, heart, brain and kidneys from the negative effects of increased vascular resistance. Perindopril, lisinopril, etc. are used.
- ARA II blockers - lower blood pressure, which is important for patients with stenosis and concomitant hypertension. The most commonly used drugs are losartan (Lorista, Lozap) and valsartan (Valz).
- Drugs that have antiplatelet and anticoagulant effects prevent increased thrombus formation in the bloodstream and are used in patients with angina pectoris, a history of heart attack, and atrial fibrillation. Aspirin Cardio, acecardol, thromboAss, warfarin, clopidogrel, xarelto and many others are prescribed.
- Diuretics are one of the most important groups in the presence of chronic heart failure, as they prevent fluid retention in the arteries and veins and reduce afterload on the heart. The use of indapamide, veroshpiron, diuver, etc. is justified.
- Cardiac glycosides are indicated for decreased contractile function of the left ventricle, as well as in persons with persistent atrial fibrillation. Digoxin is mainly prescribed.
In each case, an individual treatment regimen is used, determined by a cardiologist depending on the manifestations of the defect and echocardioscopy data.
Patients' complaints
Symptoms of mitral stenosis appear gradually: at first they bother the patient only after physical activity, then they are observed even at rest. It is typical for the clinic of mitral valve stenosis that patients complain of:
- shortness of breath or cardiac asthma;
- cough, which may be dry at first, and then becomes wet - with an increased content of sputum, foamy and even mixed with blood;
- increased fatigue and weakness;
- frequent dizziness and fainting;
- thermoregulation disorders;
- hoarseness of voice;
- frequent bronchitis and pneumonia;
- pain in the heart area - most often from the back between the shoulder blades;
- tachycardia.
The patient's appearance is characteristic: he is pale, and a feverish blush is noticeable on his cheeks, the tip of the nose, lips and fingers are bluish, the veins in the neck are swollen, swelling on the body and a swollen abdomen may be noticeable.
Lifestyle with mitral stenosis
For a patient with this disease, it is imperative to follow the following recommendations: eat well and properly, limit the amount of liquid and table salt you drink, establish an adequate work and rest schedule, get a good night's sleep, limit physical activity and eliminate stressful situations, stay in the fresh air for a long time.
A pregnant woman needs to register with the antenatal clinic in a timely manner to decide on prolonging pregnancy and choosing a method of delivery (usually by caesarean section). With a compensated defect, pregnancy proceeds normally, but with severe hemodynamic disturbances, pregnancy is contraindicated.
Diagnostics
The doctor makes a diagnosis of mitral stenosis, relying not only on the history and examination, but also on the results of such instrumental studies:
| Type of diagnostic test | Characteristic signs of mitral stenosis |
| Electrocardiogram (ECG) | Enlargement of the left atrium and right ventricle. Tachyarrhythmia. |
| Phonocardiogram | Characteristic murmur of mitral stenosis. Valve clicking sound. |
| X-ray of the heart | Enlargement of the left atrium and right ventricle. Expansion of the shadow of the vena cava and pulmonary artery. Change in lung pattern. Valve calcification. |
| Heart ultrasound with Doppler (EchoCG - echocardiography) or transesophageal ultrasound | Changes in blood flow to the heart. Reduction in the area of the mitral orifice. Enlargement of individual chambers of the heart. |
| Invasive research methods with cardiac catheterization | Increased pressure in the left atrium and right ventricle. |
To clarify the diagnosis and determine treatment tactics for mitral valve stenosis, computed tomography and diagnostic bypass surgery may sometimes be required . As a rule, the diagnostic methods given in the table are sufficient to make the correct diagnosis and carry out a differential diagnosis of mitral stenosis with the following pathologies:
- aortic valve stenosis or aortic insufficiency;
- pulmonary hypertension;
- heart tumor;
- pericarditis;
- thyrotoxicosis.
This video describes the features of echocardiography for mitral stenosis, which will be shown by this diagnostic method:
What is the prognosis for patients with mitral stenosis of varying degrees of severity?
Without surgical treatment, the life expectancy of patients with MS is 40-45 years, about 15% of patients overcome the fifty-year mark.
Invasive treatment of mitral valve stenosis can significantly prolong and improve quality of life. The 10-year postoperative survival rate is 85%.
The most unfavorable prognosis is for patients with stages IV and V, when the compensatory capabilities of the myocardium are insufficient and permanent damage to internal organs develops. Drug correction of emerging complications helps to slightly prolong life.
Features in children
The causes of mitral stenosis in children may be systemic autoimmune diseases:
- Rheumatism.
- Dermatomyositis.
- Systemic lupus erythematosus.
- Polymyositis.
In the vast majority of cases, the etiology of the defect in a child is untreated tonsillitis and the lack of bicillin prophylaxis after streptococcal infection.
The disease is characterized by the same hemodynamic changes as in adults, but the clinic has some features:
- Retarded physical development.
- “Mitral face” rarely develops.
- The disease is not complicated by atrial fibrillation.
- The “quail rhythm” is rarely heard; protodiastolic and prediastolic murmurs at the apex of the heart are more typical.
Special symptoms:
- Frequent fainting.
- Pronounced epigastric pulsation (up to the development of a “heart hump”).
Treatment methods:
- Conservative (preparation for surgery)
- Surgical (valve replacement).
The prognosis without treatment is unfavorable . The operation is performed in the first month after diagnosis and is successful in more than 90% of cases. The life expectancy of treated patients is 55-65 years.
Are there any complications?
Before surgery, in the case of severe stenosis and in the presence of heart failure, the risk of serious rhythm disturbances and thromboembolic complications is quite high.
After surgery, this risk is minimized, but in rare cases, unfavorable conditions such as infection of the postoperative wound, bleeding from the wound in case of open surgery, and re-development of stenosis (restenosis) may occur. Prevention is a high-quality intervention, as well as timely prescription of antibiotics and other necessary drugs.
Treatment methods
Medication
Conservative drug therapy for this defect is of secondary importance . Its main purpose:
- Treatment of diseases that provoked pathology (autoimmune, infectious).
- Neutralization of disease symptoms when surgical intervention is impossible or in the preoperative period. For this purpose, diuretics (Furosemide, Veroshpiron), cardiac glycosides (Digoxin, Celanide), adrenoblockers (Atenolol), anticoagulants (Warfarin, Heparin), vitamins and minerals are prescribed.
Drug therapy, along with diet and minimizing physical activity, is the leading method of treating patients with the disease in the compensation stage.
Conservative therapy is carried out:
- Into the compensation stage.
- If the general condition of the patient is satisfactory.
- With a slight degree of valve narrowing.
Drugs used:
- Diuretics – for the development of cough and hemoptysis (veroshpiron).
- Cardioprotectors – trimetazidine, riboxin.
- Anticoagulants - if there is a threat of thrombosis (atrial fibrillation): heparin, warfarin.
- In patients without arrhythmia with mitral stenosis, beta blockers (bisoprolol, metaprolol), calcium channel blockers (nifedipine) are used.
- In patients with arrhythmia, antiarrhythmics (amiodarone) are used.
- Bronchodilators (ipratropium bromide).
- Mucolytics (expectorants - mucaltin).
Surgical
But more often, patients consult a doctor when the symptoms of the disease are already severe - in this case, the classic treatment is surgical intervention. The operation is also performed in situations where drug treatment cannot compensate for a heart defect in the form of mitral stenosis, and the indications for surgical treatment are as follows:
- Pulmonary artery pressure is more than 60 mmHg.
- Thrombosis of the left atrium.
- Narrowing of the valve to 1 sq.cm.
- Decompensation of the defect (heart failure).
In this case, the following types of operations can be performed:
- Balloon valvuloplasty is a minimally invasive operation using coronary artery bypass surgery under X-ray and ultrasound control. It is performed for uncomplicated mitral stenosis of 2-3 degrees.
- Commissurotomy is an operation to dissect the valve leaflets to restore the area of the opening. It can be performed transthoracically or open heart. Indications for this method of surgical intervention are a high degree of narrowing of the mitral orifice and complications of stenosis (adhesions, blood clots, stagnation of blood in the lungs).
- Valve replacement , which uses mechanical or biological prostheses, is used in cases of severe mitral stenosis and the impossibility of eliminating it by cutting the valve leaflets.
In the case of a stage of severe decompensation of the pathology (grade 4-5), any corrective surgery is contraindicated , and patients are prescribed only palliative drug treatment.
Treatment
It is completely impossible to cure stenosis of the left atrioventricular orifice; drug therapy effectively delays progress, but does not interrupt it. As a result, the pathology is eliminated by surgical methods, but at stages when the manifestations of heart failure become obvious and irreversible (dilatation of the right ventricle), the functions of the heart are impaired and begin to complicate the patient’s life.
After surgical intervention at stages 2 or 3 of the disease, it is possible to improve the prognosis and life expectancy of the patient, however, stenosis tends to recover (restenosis, 30% within 10 years).
It is less common to operate at stage 4 - due to complications of cardiovascular failure, it is impossible to significantly improve the prognosis and prolong the patient’s life.
Drug treatment
The purpose of drug treatment for mitral valve stenosis:
- Suspend the progress of pathology (in the early stages).
- Eliminate symptoms of heart failure and oxygen starvation of tissues and organs.
- Prevent the formation of blood clots, the development of infectious complications (infective endocarditis), atherosclerotic plaques, reduce the risk of re-narrowing, restenosis after surgery and thromboembolism.
A complex of drugs is combined based on the stages of stenosis and the severity of symptoms of heart and pulmonary failure.
| Group of drugs, names of drugs | For what purposes is it prescribed? |
| ACE inhibitors (Prestarium, lisinopril) | Reduce blood pressure by blocking the conversion of angiotensin, increase the content of substances that have a beneficial effect on the functions of cardiomyocytes (heart cells) and blood vessels, increase cell resistance in conditions of oxygen deficiency |
| Adrenergic blockers (Corvitol, Coronal, Nebilet) | Normalize heart rhythm, regulate cardiac output, reduce blood pressure |
| Anti-ischemic drugs (nitroglycerin, sustak, nitrong) | Dilate blood vessels, stimulate peripheral microcirculation, enhance metabolism and gas exchange in tissues |
| Cardiac glycosides (digitoxin, digoxin) | Regulates the rhythm and strength of heart contractions |
| Antithrombotic drugs (thrombo, aspirin cardio, chimes) | Mitral valve stenosis is often complicated by thromboembolism; drugs in this group prevent thrombosis by reducing platelet aggregation (sticking together) and thin the blood |
| Anticoagulants (heparin) | Thin the blood, prevent the adhesion of blood cellular elements (platelets and red blood cells) |
| Diuretics (thiazide, indapamide) | In combination with antihypertensive drugs, they regulate blood pressure (lower it) and eliminate severe swelling |
| Antibiotics (penicillin series) | Suppress the development of bacterial microflora, prevent infectious complications in mitral valve stenosis |
All invasive procedures in patients with mitral valve stenosis should be carried out against the background of antibiotic therapy to prevent the development of bacterial infection. When the content of triglycerides and cholesterol is high, drugs from the statin group (lovastatin, atorvastatin) are used to prevent atherosclerotic plaques.
Surgery
When the mitral valve is narrowed, there are many contraindications to surgery:
- critical narrowing of the mitral valve (cardiac ejection fraction less than 20%, orifice area less than 1 sq. cm);
- terminal stage of the defect (increasing changes ending in the death of all tissues of the body);
- any acute processes (infectious diseases, exacerbation of chronic diseases, acute cerebrovascular accidents, myocardial infarction, etc.).
The goal of any operation is to restore hemodynamics, relieve the main severe symptoms, improve blood supply to organs and the patient’s prognosis.
| Name of methods | How to do it |
| Commissurotomy | Excise adhesions, adhesions, scars in the area of the mitral valve that prevent it from functioning |
| Balloon vulvoplasty | A special probe with an expanding balloon at the end is brought to the heart through large vessels. At the site of stenosis, it is inflated several times, enlarging the atrioventricular opening |
| Valve replacement | Used for severe deformations of the mitral valve, it is removed and replaced with an artificial or biological implant |
The risk of developing postoperative complications (early and late) increases depending on the degree of pathology and the severity of symptoms of heart and pulmonary failure (the earlier the operation is performed, the lower the risk):
- thrombus formation at the prosthetic site;
- thromboembolism;
- rejection or destruction of a biological implant;
- infective endocarditis;
- postoperative restenosis (re-narrowing)
Operated mitral stenosis is a good reason for regular examinations and monitoring by a cardiologist for the rest of your life.
Danger and complications
If the pathology is not detected in time and not treated, complications in the form of progression of heart failure and pulmonary hypertension are inevitable.
In this case, the main danger is inevitable death due to symptoms of pulmonary embolism, acute heart failure or pulmonary edema.
Adequate treatment can significantly reduce the risk of all these complications and reduce the likelihood of tragic events by 90-95%.
In rare cases, the following postoperative complications occur:
- infective endocarditis – 1-4%;
- thromboembolism – 1%;
- restenosis or repeated narrowing after surgical correction – in 20% of patients within 10 years after surgery.
Stages of disease development
In total, clinicians distinguish five stages of development of mitral stenosis:
- The first is full compensation. There are no signs of cardiac dysfunction;
- the second is a violation of blood circulation in the pulmonary circle. Symptoms can only be observed with increased physical activity;
- third – stagnation of blood in the pulmonary circulation and disturbances in the systemic circulation;
- fourth – pronounced indicators of circulatory disorders in the cardiovascular system, symptoms of initial failure, are clearly audible through auscultation;
- fifth – dystrophic stage. Signs of acute heart failure are observed.
It is worth noting that complications can occur at any stage of the disease. In this case, everything depends on the general condition of the patient, his age and the clinical picture of the disease.
Diagnosis of the mitral orifice
Examination for stenosis
The characteristic appearance of a patient with a developed picture of the disease (i.e., in the presence of severe pulmonary hypertension) is a “mitral face” (fades mitralis), which is characterized by bluish lips and bright flushed cheeks. These manifestations result from low cardiac output, vasoconstriction of the systemic circulation, and severe pulmonary hypertension. With severe pulmonary hypertension, you can see pulsation in the III-GU intercostal space to the left of the sternum (pulsation of the outflow tracts of the right ventricle), as well as pulsation in the epigastric region, which intensifies at the height of inspiration (which is also due to pronounced hypertrophy of the right ventricle). With decompensation, signs of chronic right ventricular failure are observed. When stenosis occurs in childhood, a lag in physical development and the development of a cardiac hump are noted.
Palpation
Palpation of the peripheral pulse on the radial arteries can reveal irregular heart rhythm (extrasystole, atrial fibrillation).
The Savelyev-Popov symptom (discovered extremely rarely) is characterized by pulse asymmetry in the radial arteries: the amplitude of the pulse wave in the left radial artery decreases compared to the right due to compression of the left subclavian artery by the enlarged left atrium.
In the position of the patient on the left side (especially when holding the breath in the breathing phase), diastolic tremor in the area of the apex impulse can be detected (previously this sign was called the “cat purring” symptom).
With severe pulmonary hypertension, an accent of the second tone in the second intercostal space to the left of the sternum is palpated. Also, at the apex of the heart, palpation can reveal an increase in the first tone (with sufficient elasticity of the mitral valve leaflets).
With mitral stenosis, a symptom of “two hammers” is also observed - an intensified 1st sound at the apex of the heart is felt by the base of the palm (the first “hammer”), an intensified 2nd tone in the 2nd intercostal space to the left of the sternum - felt by the terminal phalanges of the fingers (the second “hammer”). When there is stagnation in the systemic circulation (right ventricular failure), an enlarged liver is palpable.
Auscultation of the heart
1.
A characteristic sign of mitral stenosis is an intensified (“popping”) first sound. It occurs due to vibrations of the elastic (compacted) cusps of the mitral valve at the moment of their closure. However, with pronounced fibrous changes, calcification of the valves, and their deformation, the enhancement of the first tone may disappear as a result of limited mobility of the valves.
2.
The “click” (tone) of the opening of the mitral valve is easier to listen to using a phonendoscope, also in the projection of the mitral orifice. It should be remembered that the earlier in diastole the opening tone of the mitral valve appears, the more pronounced the stenosis of the mitral orifice. The opening tone of the mitral valve is absent in cases of severe fibrosis and calcification of the mitral valve leaflets.
3.
In the presence of pulmonary hypertension, an accent of the second tone is heard over the pulmonary artery.
4.
An intensified 1st sound, an intensified 2nd tone and the opening tone of the mitral valve form ri - a pathognomonic auscultatory sign.
5.
Diastolic murmur in the projection of the mitral valve and at the apex of the heart can be better heard using a stethoscope with the patient positioned on the left side while holding the breath in the expiratory phase. The noise is low-frequency and has a decreasing character. It should be remembered that:
- diastolic murmur increases after exercise;
- the longer it is, the more pronounced the disease. However, the murmur may become shorter or even absent when cardiac output is low.
6.
Minor mitral stenosis may also be characterized by the absence of this noise (which is extremely rare). Diastolic murmur occurs immediately after the opening tone of the mitral valve (in protodiastole) and usually indicates a significant pressure gradient, while presystolic murmur, detected during sinus rhythm, is usually characteristic of less severe disease.
7.
The diastolic murmur of pulmonary valve insufficiency (Graham Still murmur) has a high-frequency decreasing character, is heard in the second intercostal space to the left of the sternum and occurs due to expansion of the fibrous ring only with the development of severe pulmonary hypertension. The noise is made in the II-III intercostal space to the left of the sternum. It can disappear (in whole or in part) with a decrease in pulmonary hypertension (due to the development of tricuspid valve insufficiency) and elimination of the mitral orifice disease by surgery.
8.
A systolic “click” (short high-frequency sound) in the second intercostal space to the left of the sternum is sometimes heard with severe pulmonary hypertension and dilation of the pulmonary artery trunk.
9.
Systolic murmur heard at the apex of the heart when the mitral orifice is damaged may indicate mitral (concomitant) or tricuspid valve insufficiency (as a complication or with organic damage to the tricuspid valve). Increased systolic murmur at the height of inspiration and its weakening during forced exhalation are characteristic of tricuspid valve insufficiency (Rivero-Carvallo symptom). With the so-called aphonic stenosis of the mitral orifice, there are no auscultatory signs of narrowing of the mitral orifice due to pronounced changes in the mitral valve leaflets (for example, calcification), a sharp limitation of the mobility of the leaflets.
10.
Difficulties in identifying auscultatory signs of mitral stenosis may also be associated with tachycardia (sinus tachycardia, atrial fibrillation), severe tricuspid valve insufficiency, significant dilatation of the right ventricle (clockwise rotation of the heart by the right ventricle forward and displacement of the left ventricle backward), reduced cardiac output. When eliminating severe heart failure, auscultatory signs of mitral stenosis may appear more clearly.
Carrying out an ECG
In sinus rhythm, hypertrophy and dilatation of the left atrium are reflected in the “mitral” P wave - it is wide (more than 0.12 s), double-humped in leads I, II, aVL, V5, V6. In addition, a deep negative phase in lead Vi is characteristic (although such ECG changes are more indicative of a slowdown in impulse transmission through the left atrium than of its hypertrophy and dilatation). The classic P-mitral wave may be absent with severe pulmonary hypertension, tricuspid valve insufficiency and right atrium dilatation, as well as with atrial fibrillation. When mitral orifice stenosis is complicated by atrial fibrillation, its signs are revealed on the ECG. In case of severe pulmonary hypertension, the ECG records a deviation of the electrical axis of the heart to the right and signs of right ventricular hypertrophy in the form of the appearance of complexes of type R, Rs, qR in the right precordial leads and complexes of type RS, rS in the left precordial leads.
X-ray examination for stenosis
When changes occur in the lungs, they are characterized by the appearance of radiological signs of venous pulmonary hypertension (increased pulmonary pattern, expansion of the roots of the lungs, general opacification of the pulmonary fields, expansion of the veins of the upper lobe of the lungs), the presence of Kerley lines type B (horizontal linear shadows in the lower parts of the lungs 1-2 thick mm and 10-30 mm long, caused by thickening of the interlobular septa due to fluid accumulation; a sign of pulmonary hypertension). In arterial pulmonary hypertension, a symptom of “amputation” of sharply expanded pulmonary roots with depletion of the pulmonary pattern is noted. In the direct (antero-posterior) projection from the side of the heart, bulging of the left atrium appendage and the trunk of the pulmonary artery (third and second arches of the heart) is detected. Sometimes mitral valve calcification is detected. In the right oblique projection, the enlarged left atrium pushes the contrasted esophagus posteriorly (usually along a small radius arc).
Echocardiography
The study is considered the most sensitive and specific non-invasive method for diagnosing mitral stenosis. Echocardiography is of particular importance in the diagnosis of “aphonic” disease.
In two-dimensional mode, thickened leaflets (cusp) are detected in case of mitral deviation. In diastole, the anterior leaflet of the mitral valve takes the shape of a dome, a sail, inflated towards the left ventricle due to high pressure from the left atrium. When recording a short-axis echocardiogram, the area of the mitral opening can be calculated using the planimetric method. An area of less than 1 cm2 is considered a sign of critical mitral stenosis. In the same mode, dilation of the left atrium and the presence of blood clots are determined.
In one-dimensional mode, indirect signs of mitral deviation are revealed: U-shaped oscillation curve of the anterior leaflet of the mitral valve, concordant displacement of the posterior leaflet. In Doppler mode, turbulent diastolic flow is recorded in the projection of the mitral valve. Using a special method, you can also calculate the area of the mitral orifice.
Clinical picture
Symptoms of mitral stenosis, starting from childhood, are manifested by shortness of breath. The child does not participate in fast games and often gets tired.
- Heart pain occurs during a rheumatic attack and possible involvement of the coronary vessels or as a result of compression of the left coronary artery by the atrium.
- Hemoptysis appears at first only after physical exertion due to rupture of connections between the venous capillaries of the lungs and bronchioles. A mechanism similar to a hypertensive crisis is formed, but in the vessels of the lungs.
- Patients with mitral valve stenosis suffer from frequent prolonged bronchitis and pneumonia.
The first and second phases of the development of the compensatory mechanism do not manifest severe symptoms.
With decompensation, the patient complains of:
- severe shortness of breath at rest;
- cough with foamy sputum containing blood;
- inability to lie down due to increased shortness of breath in a horizontal position;
- increasing pain in the heart area;
- arrhythmia with frequent heart contractions.
Periodically, there are attacks of cardiac asthma at night.
This is what patients with the defect look like
During the decompensation phase, the doctor, upon examination, pays attention to an unusual bluish blush against the background of a pale face, cyanosis of the lips, tip of the nose, and fingers.
By placing your hand on the heart area, you can feel a trembling; it is compared to a “cat’s purr.” It is formed by the passage of blood through vibrating valves, intensifies in a position on the left side.
In the epigastric region, powerful cardiac impulses are detected, especially during inspiration, due to the increased work of the right ventricle. A dense, enlarged liver is palpable.
Typical heart murmurs are heard on auscultation.
Swelling is detected on the legs. With severe decompensation, the abdomen enlarges due to fluid effusion and compression of the portal vein by the dense liver.
In the terminal stage, swelling of the entire body (anasarca) occurs and blood pressure drops. The patient dies from general oxygen deficiency in the body.
DETAILS: Treatment of hyperglycemic coma
Classification methods
There are 4 stages of mitral stenosis:
- 1 – area greater than 3 cm2. The stenosis is slightly expressed;
- 2 – the hole gradually narrows to 2.9-2.3 cm2;
- 3 – pronounced narrowing of the lumen, up to 2.2-1.7 cm2;
- 4 – with minimal lumen, they speak of critical mitral stenosis.
Important! Critical MV stenosis is accompanied by cardiac pathology that is life-threatening.
Tricuspid valve defects
Mitral valve stenosis is an acquired type of defect; congenital abnormal thinning of the orifice is recorded very rarely, and then only in combination with other abnormalities of the cardiac structure. Mitral stenosis is often the result of acute rheumatic fever. Rheumatism of cardiac tissues and muscles can progress against the background of advanced tonsillitis, tonsillitis and laryngitis, as well as purulent infections. The provocateur of all these ailments is hemolytic streptococcus.
Rheumatic fever begins to progress when the infection, untreated or incorrectly treated, spreads throughout the body. In response to infection, the body begins to produce antibodies that act against its own tissues of the heart, brain and joints. Rheumatic carditis causes the progression of autoimmune inflammatory processes in the mitral valve region, provoking its calcification and narrowing.
Mitral valve stenosis can also be caused by the presence of infective endocarditis, which often evolves against the background of a reduction in human immunity due to serious autoimmune diseases. The stimulants of the disease are the same harmful microorganisms that penetrate the systemic blood channels.
Several factors can provoke fusion of the MV valves with each other, among which are the following:
- Rheumatism. It develops as a complication after a sore throat caused by streptococcal infection in the respiratory tract. Symptoms of rheumatism may appear several weeks after the patient has had a sore throat.
Rheumatism has the ability to affect the valve leaflets in two directions: thickening of the walls of the valve leaflets or their fusion. In any case, as a result of the impact of a rheumatic attack, the mitral valve ceases to perform its functions, losing its elasticity.
Rheumatism leads to disruption of the process of blood movement from the left ventricle to the atrium.
- Congenital heart defect. Mitral stenosis is rarely congenital. Such patients require surgical intervention.
- Other factors. This list includes reasons such as the development of blood clots or tumors that form on the walls of the mitral valve, thereby reducing the opening between its leaflets.
There are also frequent cases when, in mature patients, calcium layers are deposited on the halves of the MV, which can also provoke the development of a diagnosis of mitral valve stenosis.
It is also worth highlighting among the factors that can lead to the development of anomalies, the negative effects of certain medications or exposure to ionizing radiation.
If one or more of the above factors affects the human body, it can automatically be classified as a risk group.
In order to avoid the development of a diagnosis such as mitral stenosis, such patients should periodically undergo medical examination in a hospital.
The use of medications in the treatment of mitral stenosis does not provide complete relief from the disease. The main purpose for which a course of drug therapy is prescribed is to alleviate the patient’s general condition by alleviating the symptomatic picture.
Among the medicines, the following groups can be distinguished: diuretics, anticoagulants, antibiotics, antiarrhythmics.
Surgical treatment of mitral valve stenosis is used if the disease is at an advanced stage of its development. In the practice of modern medicine, both traditional and minimally invasive methods of surgical therapy are equally successfully used.
Treatment of mitral stenosis with traditional methods consists of the following processes:
- Valvuloplasty. It is performed using an open incision in the chest. Treatment of mitral valve stenosis using this method has a high likelihood of recurrent stenosis some time after surgery.
- Replacing MK. Many patients diagnosed with mitral stenosis require MV replacement surgery. For this purpose, valves of mechanical or biological origin can be used.
Minimally invasive methods of treating stenosis are safer and simpler, unlike traditional ones. Among them, valvotomy can be distinguished.
To treat using this technique means to partially replace one of the mitral valve leaflets. After such an operation, the patient can leave the hospital within a day or two.
It is important to remember that it is not always possible to determine the presence of MV stenosis at an early stage of development as a result of auscultation. Therefore, it is extremely important not to neglect an annual medical examination. It can keep you healthy!
Among the defects of the tricuspid (tricuspid) valve, valve insufficiency is diagnosed most often, but in isolated form it is extremely rare: usually tricuspid valve insufficiency is combined with defects of the mitral or aortic valve.
Coronary heart disease (CHD) is an acute or chronic heart disease caused by a decrease or cessation of blood and oxygen delivery to the heart muscle, resulting from pathological processes in the coronary artery system. This term was proposed by the WHO Expert Group for the Study of Atherosclerosis in 1957 and adopted as the definition of CAD in 1962.
• atherosclerosis of the coronary arteries;
• spasm of (unchanged or slightly changed) coronary arteries;
• coronary artery embolism;
• anemia;
• AG;
• arterial hypotension;
• tachycardia or bradyarrhythmias.
IHD is widespread in many countries of the world, it affects mainly men aged 40-60 years; in women after 60 years of age, IHD occurs with the same frequency as in men of this age. Of all causes of death from cardiovascular diseases, IHD accounts for more than 50%.
Classification
• sudden coronary death (primary cardiac arrest);
• angina pectoris (first-time exertional angina, stable exertional angina of various (I-IV) functional classes, progressive exertional angina, rest angina, spontaneous (special) angina);
• MI (with a Q-wave (previously called “transmural”, “large-focal”) and without a Q-wave (formerly called “small-focal”, “subendocardial”);
• post-infarction cardiosclerosis (old, previous MI);
• heart rhythm disturbances (meaning only those associated with myocardial ischemia);
• heart failure (associated with myocardial damage due to ischemic heart disease).
It should be noted that over the past 30 years since the creation of the classification of IHD, proposed by WHO experts in 1979, significant changes have occurred in the understanding of the pathogenesis and treatment options for many clinical forms of IHD. In this regard, in recent years, a number of new terms have appeared (for example, “acute coronary syndrome”, “unstable angina”) and a number of new classifications of certain forms of coronary artery disease (for example, “universal definition of MI”, 2007 classification of MI). They are not reflected in the 1979 WHO classification and will be presented in the appropriate sections of this textbook.
• non-modifiable, which include male gender, age and hereditary predisposition;
— dyslipidemia (high concentration of total cholesterol in the blood ({amp}gt;240 mg/dl) and LDL {amp}gt;160 mg/dl, decreased HDL concentration, increased triglyceride levels);
- AG;
- smoking;
— physical inactivity (physical detraining);
- excess body weight and high-calorie diet;
- diabetes mellitus or impaired glucose tolerance.
The sequence of palpation of the heart area:
- characteristics of the apex beat;
- identification of systolic or diastolic tremor of the “cat’s purr”;
- pulse and its properties.
https://www.youtube.com/watch?v=VvYKjma1tnk
The main properties of the apical impulse are:
- localization;
- square;
- force;
- height.
By localization it can be:
- normal (in the 5th intercostal space 1-1.5 cm medially from the midclavicular line);
- move left, right, up and down.
By area it can be:
- normal (2 cm²);
- spilled;
- limited.
The symptom of “cat purring” occurs when blood passes through a narrow opening, causing it to swirl.
Depending on the phase of cardiac activity, there are:
- systolic “cat purr”;
- diastolic "cat purr".
The pulse is a periodic oscillation of the vascular wall synchronous with the activity of the heart.
1) synchronicity on both hands.
If the filling is different, the pulse is different (p.differents).
Surgical method
It has a large number of indications and contraindications. In the initial stages of mitral valve stenosis, classical therapy is carried out, and only when the narrowing becomes less than 3 cm, then a decision is made about possible surgery.
Surgical treatment methods are resorted to if the danger to life is higher than the risk of surgery.
- Balloon valvuloplasty - sedatives are administered, after which a probe with a balloon is inserted through the femoral artery, reaching the place of narrowing of the ring, the catheter is inflated and causes the destruction of the fused valve leaflets, after which it is removed back;
- Open commissurotomy - performed in case of impossibility of balloon plasty, and is performed by cutting the site of narrowing of the valve with a scalpel and enlarging the opening of the ring on the open heart;
- Valve prosthetics (replacement) - transplantation of a valve of foreign or artificial origin is used, the method is used if the valve disorder is so severe that it is impossible to restore it using previous methods.
Open valve surgery
Contraindications for surgery
There are a number of strict contraindications for such an operation:
- Infectious lesions;
- Damages of the cardiovascular system (stroke, myocardial infarction, etc.);
- Terminal heart failure and severe deadaptation (reduction in blood output to the level of 20 percent);
- General diseases that exhaust the vital forces of the body, such as diabetes, bronchial asthma, etc.
Postoperative complications
- Infectious foci on the valves of the mitral ring;
- The occurrence of thrombus formation at the site of mechanical intervention;
- Rejection of the artificial prosthesis by the body and a further increase in mitral insufficiency.
Mitral valve replacement surgery can be performed in any large city in the country. At the same time, by submitting an appearance with the necessary documentary evidence, you can receive it according to the quota. Otherwise, it will cost you from 100 to 300 thousand rubles.
Image of the valve apparatus
Complications without surgery
Some patients are skeptical about surgery. But the lack of timely and effective compensation for mitral valve stenosis can lead to extremely negative consequences.
These include:
- Increased level of hemodynamics;
- Progression of congestion in the pulmonary vessels, and later in all organs;
- Fatal pulmonary edema;
- AHF – when the heart can no longer cope with contractile function.
Etiology
The most common cause of the development of the pathological process is rheumatism. It is noteworthy that the disease can begin to develop asymptomatically. The first signs of mitral stenosis may appear after 10–15 years from the onset of the disease. Naturally, this circumstance significantly complicates the treatment process.
In addition, mitral stenosis can form due to the following factors:
- heart or chest injuries;
- infective endocarditis;
- atherosclerosis;
- ailments caused by infection;
- intracardiac thrombi.
In more rare clinical cases, mitral valve stenosis may be caused by congenital pathologies. But, as medical practice shows, in 80% of cases, patients are diagnosed with acquired mitral valve stenosis.
Against the background of such a defect, other ailments may develop. The most common is aortic insufficiency.
Surgery
Not in all cases, with the help of medications, it is possible to restore the condition of a patient diagnosed with mitral stenosis.
Treatment in some cases will not give the desired effect. As a rule, starting from the third stage of the disease, cardiologists recommend not to refuse surgical treatment. It can be performed using traditional or minimally invasive methods. The latter are, of course, preferable. They are less traumatic and better tolerated.
Traditional methods include valvuloplasty. This method requires an open incision around the heart. During the operation, the surgeon dissects the fused valves. But in the future they may connect again, and the operation will have to be repeated.
The most effective method is to replace the valve. For this procedure, neither hemodynamics in mitral stenosis nor the severity of the disease is important. It can be carried out even in advanced conditions. Mechanical or biological valves can be used as a replacement. True, the use of the former is fraught with risks of developing thrombosis. And the latter have a limited service life.
Prognosis and prevention
A favorable prognostic conclusion applies to asymptomatic acquired heart defects, as well as timely corrected conservative or surgical treatment.
An unfavorable prognosis is made in the presence of serious hemodynamic changes that significantly affect the functioning of the heart and the body as a whole. During the decompensation stage, physical activity may also be significantly impaired, which is why the patient is considered temporarily or permanently disabled.
Prevention of PPS is as follows:
- Infectious and inflammatory diseases should be promptly eliminated with appropriate therapy.
- The immune system needs to be strengthened with suitable medications prescribed by a doctor.
- It is important to stop smoking and drinking caffeine-containing and alcoholic drinks in increased quantities.
- Body weight should be within normal limits.
- Physical activity should be maintained at an acceptable level.
Therapeutic methods
To treat stenosis, only surgical treatment methods can be used. This is due to the fact that the drugs are not able to widen the opening between the ventricle and the atrium.
If the defect occurs without pronounced symptoms, then medications are not needed. If clear manifestations of disorders appear, then before performing the operation and to eliminate the cause of the pathology, you need to undergo treatment:
- diuretics;
- blockers of adrenaline receptors and calcium channels.
In the case of atrial fibrillation and an increased likelihood of blood clots forming in the cavity of the left atrium, direct anticoagulants like Warfarin cannot be avoided. If thromboembolism occurs, they resort to Heparin, which can be combined with Acetylsalicylic acid.
Mitral stenosis is a disease that is most often caused by rheumatism. Therefore, in order to avoid re-development of disorders, measures must be taken to prevent infectious damage to the endocardium and rheumatism.
To do this, they resort to antibacterial drugs, salicylates, and pyrazoline agents. After completing this therapy for several years, the patient should take Bicillin-5 once a month.
The patient is advised to lead a healthy lifestyle and choose an occupation that would not worsen the condition.
But, if there are no signs of decompensation and the hole is not narrower than 1.6 centimeters, then women are allowed to become pregnant and bear a child. If the situation is much worse, but the woman becomes pregnant, then an abortion is recommended. In rare cases, balloon valvuloplasty or mitral commissurotomy is resorted to.
If the hole has narrowed to one centimeter, blood clots are constantly forming, or pulmonary hypertension is severe, then surgical treatment is resorted to.
In some cases, surgical procedures may involve valve replacement. A prosthesis is installed in its place.
Forms of the disease
In official medicine, three stages of the development of the disease are distinguished. They are diagnosed depending on the area of the mitral orifice:
- light form - hole no less than 2 and no more than 4 square centimeters;
- moderate - hole from 1 to 2 square centimeters;
- heavy - the hole is less than 1 square centimeter.
As a rule, a mild form of mitral stenosis occurs without any symptoms. The disease can be diagnosed accidentally - during research for other diseases.
- avoid excessive physical activity, hypothermia;
- visit your doctor at least once a year to monitor symptoms of the disease and conduct echocardiography;
- carry out prevention of relapse of the disease with penicillin drugs once every 4 weeks for 10 years after the last episode of rheumatic fever or at least until the age of 40;
- follow all recommendations of the attending physician;
- limit the consumption of table salt and liquid;
- consult with your doctor about the need for antibacterial prophylaxis of infective endocarditis in case of planned operations in the oral cavity, gastrointestinal and urogenital tracts;
- Consult a doctor immediately if you experience shortness of breath, hemoptysis, swelling in the legs, fever, unexplained weakness and fatigue.
Etiological factors
There are acquired and congenital mitral stenosis. In the latter case, the child is born with already changed valve structures. Its presence can be diagnosed at the prenatal stage - during pregnancy. In addition, modern capabilities make it possible to correct this defect, if necessary, at the same time, before the birth of the fetus.
It is difficult to speak definitely about what specific reasons lead to the development of the defect. After all, there are a lot of theories that have not been definitively proven.
However, there are a number of factors that could potentially influence the risk of developing congenital heart disease:
- genetic predisposition, which occurs within the framework of connective tissue dysplasia syndrome;
- the influence of factors such as alcohol, tobacco smoking, as well as inhalation of other components containing tars;
- infection of a woman during pregnancy with viruses (for example, rubella);
- irradiation;
- taking medications.
For the purpose of early diagnosis of this pathology, prenatal screening, carried out at the stage of antenatal consultation, can be considered.
Valvotomy
Balloon valvuloplasty aims to repair the mitral valve without direct heart surgery. It works as follows. The surgeon inserts a thin catheter into the femoral artery. A special canister is placed at the end of it. The catheter is guided through the artery to the mitral valve. When it is in place, the balloon inflates and due to this, the fused valve flaps diverge. After this, it is deflated and removed from the heart cavity.
The procedure is carried out under X-ray control. But there are a number of contraindications for its implementation. So, if mitral valve stenosis is combined with its insufficiency or there are blood clots in the heart cavity, then valvotomy cannot be performed. There is also a risk of complications. As a result of such intervention, the valve may change its shape. This may cause it to stop closing the hole. It is also impossible to exclude the development of embolism of the pulmonary artery or cerebral vessels due to blood clots or fragments of valve tissue.
In most cases, re-intervention is required after approximately 10 years.
Causes of heart disease
The main cause of mitral stenosis is a rheumatic process maintained by the continuous circulation of hemolytic streptococcus in the blood.
The disease begins in childhood, often after a sore throat. The latent period (without clinical manifestations) can last up to 20 years. Signs of rheumatic disease appear already in adulthood of the patient.
Girls have been found to be more susceptible to infection.
In 30% of cases, rheumatic attacks cause the formation of mitral insufficiency. They are more often observed in boys.
Most cases of pathology develop after rheumatism. The problem also occurs:
- if a person has suffered myocarditis of infectious origin;
- after syphilis;
- due to atherosclerotic changes;
- after chest injuries;
- for autoimmune disorders;
- with genetic predisposition;
- in case of malignant processes in the body;
- under the influence of poisoning with certain drugs.
With the development of stenosis, changes occur in the functioning of the heart, depending on which the stages of development of the disease are distinguished:
- Mitral insufficiency of the 1st degree is a condition in which the disturbances are fully compensated, the opening narrows to four centimeters.
- The second stage is determined when signs of increased pressure in the veins appear in the small circle. But so far there are no clearly visible symptoms of circulatory disorders. The left atrium begins to enlarge.
- At the third stage, symptoms of heart failure appear, the organ sharply increases in size, pressure in the veins increases, the liver enlarges, the mitral opening becomes narrower and reaches 1.5 cm. The dimensions of the left atrium exceed five centimeters.
- In the fourth stage, the condition worsens. Blood begins to stagnate in the vessels, this leads to an enlargement and thickening of the liver, narrowing the opening to one centimeter.
- The fifth stage is terminal. In this case, almost complete closure of the mitral orifice and pronounced hypertrophy of the left atrium are observed.
Depending on how much the structure of the mitral valve has changed, the following is observed:
- The first degree, in which calcium salts settle on the valve flaps.
- Mitral valve insufficiency of the 2nd degree is manifested by the coating of all valves with calcium salts.
- The third degree is characterized by calcification of all valve structures.
The onset of the disease often goes unnoticed and is mistaken for a common cold. The symptoms of rheumatic fever are no different from acute respiratory disease: fever for a short period of time, bone aches, dizziness and weakness. Fever lasts no more than 5–7 days and in the vast majority of cases is relieved by the body on its own.
- Infectious diseases transmitted by ticks cause damage to cartilage and connective tissue. As a result, autoantibodies enter the blood, causing mitral stenosis.
- According to recent studies, the tendency to heart disease also has hereditary roots: the gene is passed on through the maternal line. However, this factor is predisposing and is not the cause of the disease.
Classification of the disease and corresponding symptoms
The thermal stage of disease progression is diagnosed when the mitral valve area is from one to 1.6 centimeters. Such a decrease in the area of the hole is critical for the patient, since irreversible deformations occur in all internal organs due to a deficiency of nutritional components and oxygen, tissue death progresses, followed by the biological death of a person.
Characteristic signs of the thermal stage: swelling of the whole body, muscle deformation, heart failure, epigastric pulsation, decreased blood pressure, arrhythmia, tachycardia. Without serious and long-term treatment, a patient with this type of disease has poor prognostic assessments by doctors.
General symptoms
At the initial stage, the disease may not show symptoms at all. As the disease progresses, the following symptoms may occur:
- increased fatigue;
- shortness of breath, even with minor exertion;
- cough with blood;
- arrhythmia or tachycardia;
- asthma attacks at night.
At later stages of the disease, signs of mitral stenosis may be more pronounced. Especially the doctor can detect interruptions in the functioning of the heart using auscultation. At a late stage, a person experiences shortness of breath even at rest. Asthma symptoms become more frequent, and not just at night.
A symptom such as shortness of breath is the first and most sure sign of an illness. But, at the same time, such a symptom, as well as hemodynamics, may indicate other diseases. Therefore, you should consult a cardiologist for an accurate diagnosis.
The patient's appearance gradually changes. Cyanosis of the lips and even fingertips is observed. An unhealthy blush may appear on your cheeks. These are also characteristic symptoms of the disease.
Mitral stenosis can be fatal if not treated promptly. According to statistics, this disease leads to death in 40% of cases.
The compensatory mechanisms involved in heart disease complicate both diagnosis and treatment, and the absence of pain syndromes in the first two stages becomes a common reason for ignoring the disease.
The following symptoms may be a serious reason to seek medical help:
- dizziness, sudden short-term loss of strength, pre-fainting states that appear against the background of rest, and not physical activity;
- progressive weakness, rapid fatigue, impaired thermoregulation: on the one hand, the patient is constantly chilly, his hands and feet are cold, but he also does not tolerate heat well;
- a bluish coloration of the nose, lips, fingertips is observed - cyanosis, a limited purple blush appears - a doll's blush;
- disturbances in the functioning of the heart; when listening, characteristic systolic murmurs, presystolic trembling, and the tone of valve opening are observed;
- the appearance of shortness of breath during physical exertion, and in the later stages - at rest. It is impossible to identify the disease by this symptom alone, but increased shortness of breath in a horizontal position is very indicative;
- mitral stenosis is often accompanied by persistent bronchitis and various forms of pneumonia;
- wet cough with bleeding;
- dull unpleasant pain that is localized on the back between the shoulder blades on the left side of the body.
DETAILS: Treatment of hemorrhoids in Moscow: affordable prices
The most dangerous feature of heart disease is the discrepancy between the signs and the severity of the lesion. The disease develops so slowly that most sufferers do not notice how they reduce physical activity.
A little anatomy and physiology
The mitral valve (MV) in our heart looks like a dense muscle ring. It is located on the left side of the heart and separates the ventricle from the atrium. The valve consists of two leaflets and does not allow blood to flow back. If it functions normally, blood does not flow back into the left atrium and moves on through the vessels. With pathology of the valves of the heart valve, regurgitation occurs: backflow of blood and impaired circulation inside the cavities of the heart.
As a rule, this disease occurs due to rheumatic pathologies. The formation of the defect is observed in young people, often females. Dysfunction of the MV opening can take different forms:
- mitral valve insufficiency;
- narrowing (stenosis) of its ring.
If the MV is insufficient, its valve flaps weaken and poorly cover the valve opening. With mitral stenosis, the valve ring becomes smaller as its leaflets begin to fuse together. There is a gradual narrowing of the gap that connects the left atrium to the ventricle.
This is interesting!
The main symptoms of mitral stenosis were first described by the French physician Raymond Viessin in 1715.
Why does the disease occur?
Congenital narrowing of the valve ring is rarely detected. If such a diagnosis is made, it is accompanied by other heart defects. They are very severe and are not difficult for an experienced cardiologist to detect.
Acquired narrowing of the MV ring often occurs due to rheumatism. Rheumatism is a serious chronic disease. It occurs after colds and pustular infections caused by beta-hemolytic streptococcus. This dangerous microorganism provokes a specific fever in rheumatic patients. During a fever, the patient's body produces cells against its organs and tissues. This phenomenon is called an autoimmune reaction. Autoimmune pathologies include:
- arthritis;
- minor chorea;
- erythema;
- rheumatic carditis.
It is with rheumatic carditis that the inflammatory process seizes the valves of the mitral valve. Rough scars made of connective tissue appear on them. The valves are gradually soldered together, and the hole between them narrows. Thus, rheumatic stenosis of the mitral valve occurs.
In addition to rheumatism, the disease provokes endocarditis of infectious origin. It is caused by beta-hemolytic streptococcus or another microorganism. It enters the bloodstream of patients with low immunity or drug addicts who inject themselves with drugs through a vein.
Also, MV stenosis can be caused by a number of diseases:
- atherosclerosis;
- high levels of calcium in organs and tissues (they become hard);
- syphilis;
- benign cardiomyxoma;
- aortic valve insufficiency;
- blood clots inside the heart;
- congenital heart defect with Lutembashe syndrome.
Information!
MV stenosis causes poisoning with drugs that contain wormwood.
Preventive methods
The main question in the strategy for patients with valve stenosis is how to prevent relapses. People who have suffered a primary attack of stenosis or surgery must take special medications throughout their lives. For example, benzathine benzylpenicillin, which is suitable for both adults and children. It is administered intramuscularly.
It is also necessary to prevent infected endocarditis and rheumatic fever. If there are no clinical manifestations, then you need to take medications only for rheumatic fever.
Work activities associated with physical activity and psycho-emotional stress, as well as cooling, a patient diagnosed with valve stenosis should be abandoned. If complications develop, then a disability group is assigned, because people become unable to work.
As for pregnancy, pregnancy is allowed if the valve area is at least 1.5 cm² and there is no heart failure. If the area is significantly smaller and health deteriorates, doctors advise terminating the pregnancy.
Causes
In most cases, acquired heart defects develop against the background of infectious processes, while 50% of patients with PPS become so due to rheumatism. This disease in almost 90% of cases leads to the formation of mitral valve stenosis or insufficiency; the aortic and tricuspid valves can also be affected.
Other causes of PPS of infectious origin include syphilis and bacterial endocarditis, which affect the aortic valve, and less commonly, the tricuspid valve.
The clinical picture of atherosclerosis and coronary heart disease is also often supplemented by acquired heart defects. Against the background of atherosclerosis, the aortic valve is mainly affected, and with ischemic heart disease, mitral insufficiency often occurs.
In rare cases, PPS are formed due to a tumor process, heart injury, or due to the accumulation of parasites.
The formation of acquired defects occurs in several ways:
- Formation of stenosis due to scarring of the affected valve leaflets. Cicatricial rigidity of the leaflets is also formed along with the subvalvular structures.
- Valve insufficiency occurs as a result of the formation of scars, deformations on it, and its destruction or damage can also occur.
Valve stenosis leads to the formation of anatomical obstacles to the flow of blood in the cardiac cavities, and insufficiency leads to dynamic obstacles that contribute to the return of part of the blood through the damaged valve. Therefore, heart defects are dangerous for the development of various serious complications.
Reasons for the development of the problem
Factors in the development of a pathological process are always pathogenic in nature. Heart defects do not form naturally.
Among the highlights:
- Oversupply of medications. Especially glycosides. The greatest danger comes from tincture of wormwood and lily of the valley. You need to be careful with them. Especially during long-term use as prescribed by a doctor.
- Rheumatism, arthritis of autoimmune origin. It is considered the main cause of the formation of mitral stenosis. The approximate frequency is about 60%. Therapy is a priority. Lifetime. During exacerbations it is intense.
- Another 20% is due to inflammatory pathologies of cardiac structures. The main one among them is myocarditis. Accompanied by destruction of the atria. Requires urgent prosthetics as part of high-tech care.
- Exposure to radiation. Submariners, workers of nuclear power plants, and liquidators of accidents of this kind are susceptible to this factor. Specific assistance is aimed at eliminating the valve obstruction.
- Calcinosis. Deposition of inorganic salts in the structures of the heart. Usually of metabolic origin. A whole range of manifestations is observed, including from the musculoskeletal system.
- Previous chest injuries affecting cardiac structures. Scarring becomes a natural outcome.
- Syphilis without proper treatment. This is an insidious disease that destroys a person inside and out.
- Thromboembolism.
- Benign and less commonly cancerous tumors of the heart and its formations.
- Congenital and acquired malformations of the organ, against which the opening is formed.
- Aortic insufficiency.
- Long-term arterial hypertension of any origin.
- Cholesterolemia.
The reasons need to be sought urgently. Especially if symptoms appear. The days are counting.
Stages of the pathological process
Normally, the area of the mitral orifice in humans is from 4 to 6 cm2. There are five stages of development of the defect. Initially, it is completely compensated by the left atrium. The patient does not feel discomfort and does not complain, but there are already auscultatory signs of the disease.
In the second stage of stenosis, pulmonary circulation is disrupted. The patient feels discomfort during physical effort and stress. At rest, symptoms may not be observed. The third stage is characterized by obvious symptoms of impaired blood flow. Their first signs are expressed in a small circle, and subsequently appear in a large one.
At the fourth stage of mitral stenosis, clear symptoms of impaired blood flow are observed in both circles. The stage is always accompanied by the development of atrial fibrillation. Atrial fibrillation is a disorder of the atria. It is manifested by their frequent contraction and severe heart rhythm disturbances.
Important! At the fifth stage of the disease, doctors talk about the development of heart failure of the 3rd degree.
Symptoms of MV stenosis
You can detect the symptoms of MV stenosis if you know about the peculiarities of the development of this insidious disease. If the patient has been diagnosed with rheumatic fever, the incubation period for the development of the defect can be 5 years or more.
At the onset of the disease, shortness of breath and tingling in the chest appear. Also, the first stage is characterized by palpitations, which are accompanied by a feeling of fear and discomfort. Symptoms occur with physical exertion, prolonged walking and walking up stairs.
As the pathology progresses, these symptoms bother the patient even at rest and with minimal exertion. In the second stage, congestion is observed in the pulmonary vessels and internal organs. In a lying position, shortness of breath and a dry cough occur, the legs and feet look swollen. Due to overload of the hepatic veins, abdominal pain appears.
At the third stage of the disease, it is difficult for the patient to perform ordinary household tasks: prepare dinner, tie shoelaces, move. Fluid accumulates in the abdomen (ascites), and the abdomen appears large and distended. The limbs and face look swollen and pale, and the skin becomes bluish in color. As the fluid constantly presses on the lungs, shortness of breath gets worse.
On a note! With severe stenosis of the mitral valve, a “mitral blush” can be seen on the patient’s cheeks. The cheeks become blue-red.
Severe stage 4 of MV stenosis is called terminal by cardiologists. All symptoms occur with complete rest. The heart cannot act as a pump that pumps blood. Organs and systems lack nutrition and oxygen. This is fraught with the development of dystrophic processes. Anasarca appears - a condition in which the entire body swells. If left untreated, death occurs very quickly.
The first two stages of the disease proceed slowly, from 10 to 20 years. Chronic heart failure occurs when blood stagnates in both circulation circles.