Lichen sclerosus is a chronic skin disease that mainly affects areas of the genitals and perianal area. Lesions may also occur on the chest, upper torso, and arms. Most often, the disease occurs in postmenopausal women. Lichen sclerosus is rare in men and children. Externally, it is manifested by the formation of light spots on which the skin is thinner than normal.
The ratio of sick women to men is 6-10:1. Pathology occurs in every 60th woman in the population (1.7%). After 70 years, unlike many diseases of the genital organs, remission of lichen sclerosus does not occur.
What is lichen sclerosus?
Lichen sclerosus in girls is a slowly progressive chronic disease in which dystrophic damage to the mucocutaneous tissue occurs. Most often it is observed on the external genitalia, but there may also be extragenital manifestations.
One of the most common and characteristic symptoms is whitish spots. Until recently, this pathology was detected mainly in middle-aged and elderly women during menopause. In recent years, there has been an increase in incidence among children, both in Russia and in other countries.
In medicine, other names are used for this deviation:
- white spot disease;
- white lichen of Tsumbusha;
- kraurosis of the vulva;
- drop morphine;
- lichenoid scleroderma;
- atrophic punctate leukoderma.
The disease also occurs in men, but 4-10 times less frequently than in women. A combination of scleroatrophic changes with lichen planus and systemic scleroderma (about 9% of patients) is often diagnosed - an autoimmune disease that damages the skin, blood vessels and internal organs.
Forecast
When treated with glucocorticoids, remission occurs in 72% of women under the age of 50 years. In patients aged 50-70 years, the remission rate decreases to 23%. After 70 years, the disease never progresses to this stage. Also, skin scleroatrophy cannot be cured if it lasts 15 years after menopause or more.
Most women experience a relapse of the pathology over time. Thus, in half of the patients with remission, signs of the disease reappear within the first 8 months. The longest duration of remission reaches 4 years.
9.6% of women with recurrent lichen sclerosus subsequently develop invasive squamous cell carcinoma of the skin. Sometimes a tumor appears very quickly, even with constant medical supervision.
Although topical steroids have been used to treat the disease since 1988, the optimal duration of treatment to improve the prognosis of the disease is still unknown. One of the most detailed studies in this area showed that even long-term use of strong topical corticosteroids cannot cure the disease in women over 70 years of age.
Complete remission in young women is also temporary and does not guarantee the absence of vulvar cancer in the future. Although this malignant tumor often develops in untreated patients or patients receiving inadequate therapy.
Causes
Lichen sclerosus in girls and its exact etiology have not yet been sufficiently studied in modern medicine.
The influence of the following factors that can lead to its occurrence is noted:
- Genetic inheritance. In 78% of patients, a relationship with the HLA-DQ7 and HLA-DQ8 genes is detected. In 17% of cases, this disease is familial in nature, that is, it is also present in other members of the same family - mothers, sisters, grandmothers.
- Autoimmune dysfunctions. The presence of atrophic skin changes outside the genital area is often combined with scleroderma, so these pathologies presumably proceed through a similar mechanism. 67% of patients have low titers of some types of autoantibodies. 5-20% of patients have other hereditary diseases of an autoimmune nature - vitiligo, celiac disease, gastritis, Hashimoto's thyroiditis, pernicious anemia, alopecia.
- Hormonal changes in the pituitary-adrenal-ovarian system. Most often, the disease occurs in girls before menarche, with low estrogen levels. Such patients are characterized by later puberty and menstrual irregularities. When the first menstruation occurs, some girls experience subsidence of symptoms of the disease. In older women, with aging and loss of reproductive functions, this phenomenon is also observed.
The triggers for the development of lichen sclerosus may be the following:
- local damage to the skin, especially where there are old scars; If we talk about the genital area, then such irritating factors are masturbation, helminthic infestations and allergies, accompanied by itching;
- radiation therapy;
- constant rubbing of the skin with clothes;
- chronic urinary irritation in patients with diabetes;
- infectious and inflammatory pathologies of the pelvic organs
Causes of the disease
Lichen sclerosus or white spot disease is a pathology of unknown origin. Therefore, it is impossible to accurately determine the cause of the disease. There are several factors influencing the manifestation of the disease:
- genetic predisposition - more than 12 percent of cases of pathology in the family;
- skin injuries, especially in the genital area;
- disruption of the metabolic process in the body;
- changes in the functioning of the immune defense;
- constant exposure to various allergens.
Sometimes the manifestation of lichen sclerosus is associated with the presence of autoantibodies in the body, thyroid disease and genetic changes in the body. But the etiology of the disease has not been fully determined.
Stages and forms of SAL
The dystrophic process develops gradually and consists of the following successive stages:
- Thickening of the skin, an increase in the number of keratin cells in the stratum corneum.
- Formation of horny plugs at the mouths of hair follicles.
- The appearance of lesions is first bright pink and then whitish in color, with a waxy sheen.
- The occurrence of asymmetry of the labia, the formation of an edematous zone under the epidermis, swelling of the clitoris.
- Gradually, the skin becomes thinner and wrinkles, loses its natural color and becomes like tissue paper.
- Atrophy at the final stage may be accompanied by complications in the form of cracks, erosions, and hemorrhages.
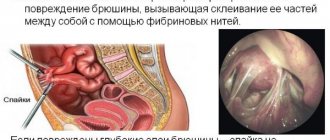
- Synechiae (fusion) of the labia minora or majora are formed, the entrance to the vagina narrows, and the perineum and anal area are deformed.
Skin lesions in the genital area have a wide variety of manifestations.
The following forms of the disease are distinguished:
- Erythematous. Redness and swelling of the skin are noted, and on the inner surface of the labia majora there is superficial atrophy in the form of whitish areas. Often a red or discolored rim runs along their border line. This form of the disease occurs with inflammation of the vulva and vaginal mucosa.
- Papular. On the inner surface of the labia majora, flat papules are formed - cavityless nodules. After their resolution, areas of atrophy with a whitish tint remain. The perianal area is usually not affected, and discomfort in girls and women is mild.
- Erosive. Against the background of inflamed and atrophic areas, bleeding erosions or small ulcers occur. In this case, severe pain is felt.
- Vitiligo, manifested in the formation of foci of depigmented skin and the appearance of cracks.
- Bullous. This form is characterized by the formation in the edematous zone of blisters filled with serous fluid (may be mixed with blood). Patients experience itching and burning. Lichen bullosa is one of the most difficult to treat forms of this disease.
Forms of the disease
This type of lichen can be located on various areas of the skin. Depending on this, there are two main forms of the disease.
Extragenital
This type of lichen sclerosus occurs in almost 20 percent of patients. Skin lesions are mainly observed in the neck and torso area - on the back, in the navel area or on the skin of the armpits. Pathology can also appear on the bends of the wrists, palms and soles of the feet. Sometimes the rash affects the oral mucosa.
Genital
This form of white spot disease is divided into two types:
- Lichen sclerosus of the vulva. A fairly common disease that affects the skin of the female genital organs. Ringworm can often form in the perineal and vulvar areas. In this case, the focus is observed in the area of the labia and in older women there is a risk of degeneration of the disease into squamous cell carcinoma.
- Lichen sclerosus of the penis. White spots form on the skin of the foreskin and glans. Pathology is observed in uncircumcised men. The acute form of the disease sometimes leads to a narrowing of the urethra or foreskin.
Lichen sclerosus occurs more frequently in females.
The disease affects people under 70 years of age. In old age, pathological remission is not observed.
Localization in girls, women
Most often, the lesion is located in the genital area and anus. However, in some patients (about 20% of cases), lesions may occur in other places.
The article discusses in detail the symptoms and causes of lichen sclerosus in girls and women.
The following areas are most often subject to atrophic changes:
- breast;
- back;
- neck;
- forearm;
- shins;
- stomach;
- area under the mammary glands;
- axillary area.
In such cases, small flat papules 3-12 mm in size, white or grayish-whitish in color with a pearlescent sheen, appear on the skin. They can be located singly or in groups, forming plaques with irregular contours and a depression in the center.
On their surface there are follicular elements in the form of comedones. There is usually no pain, but slight itching may be felt. This rash often goes away on its own, leaving depigmented spots in its place.
It won't go away on its own
Remember, if lichen sclerosus has been diagnosed, treatment is mandatory. You should not hope that the disease will go away on its own. As soon as you suspect you have it, immediately visit a dermatologist to identify an accurate diagnosis and determine which medical methods are applicable in a particular case.
Often the disease develops over years. People pay little attention to it, since the rashes do not cause concern and do not provoke pain or itching. Without qualified help, the disease becomes advanced and the affected area gradually increases.
The disease is characterized by “waves”, when the affected areas become larger or smaller. In some cases, papules degenerate into cancer cells. Then squamous cell carcinoma is diagnosed. You can avoid cancer only by being attentive to your health and visiting a doctor at the first sign of lichen.
Symptoms
Lichen sclerosus, in addition to the above signs of the disease, may also be accompanied by the following symptoms in girls and adult women:
- discomfort when walking, mild itching at the initial stage of development of the disease;
- gradually the itching becomes unbearable, a burning sensation occurs in the genital area (mainly at night);
- pain during urination, defecation and sexual intercourse;
- a feeling of tightness, numbness or tightness in the genital area;
- minor hemorrhages, dilation of blood vessels under the skin;
- “figure-of-eight” lesion in the vulva and anus;
- sometimes the surface of the plaques can be rough and resemble parchment in structure.
About a quarter of patients do not complain, that is, the disease proceeds without subjective symptoms, however, even in this case, complications can develop.
Folk remedies
Alternative therapy for lichen sclerosus is aimed at eliminating the symptoms of the disease. Traditional methods are used in combination with basic drug treatment.
Celandine tincture is a folk remedy for lichen sclerosus
Among the most effective alternative medicine recipes are:
- Herbal decoction. Place a herbal mixture in a container, consisting of burdock root, nettle, string, yarrow, black currant leaves, as well as horsetail, tricolor violet and strawberry leaves. All components are added in equal parts - one tablespoon at a time. Pour the herbal mixture with 500 milligrams of hot water and boil for three minutes over low heat. After this, the container is covered with a lid so that the broth infuses for half an hour. The strained mixture should be taken three times a day, 150 milligrams. The course of treatment consists of three months.
- Baths. Pour 250 grams of string, chamomile and calendula with three liters of boiling water and leave covered for twenty minutes. Use warm, strained herbal liquid for baths. This treatment should be carried out daily for three months.
- Lotions. Pour 100 grams of dry crushed celandine with the same amount of vodka. The mixture is hermetically sealed in a container and left to infuse in a shaded place for fourteen days. Moisten the affected areas with the prepared liquid once a day. The procedure should be carried out carefully, since the alcohol tincture causes a burning sensation in the area of the sore spots.
To relieve itching and irritation, washing with a solution of tar soap and soda is often used. Cold compresses also help relieve unpleasant symptoms.
After therapeutic water procedures, the affected skin is treated with Vaseline, baby cream or sea buckthorn oil. All products must be of high quality and not contain additional irritants.
Traditional medicine recipes have good anti-inflammatory, soothing and wound-healing properties. You can get the desired result from such products only with long-term and regular use. All therapeutic actions must be agreed upon with the attending physician.
Features of the course of lichen sclerosus in girls
In 70% of cases in girls, this disease is detected at the age of 5-10 years. Most often this happens by accident, during routine examinations. Thus, compared to adult women, girls have 3 times fewer complaints about itching of the genital organs. The most common clinical sign in childhood is thinning of the vulvar mucosa and dryness.
As medical studies show, the following abnormalities are detected in early-age patients:
- hormonal imbalance – decreased levels of estradiol, progesterone and increased FSH, testosterone; activation of the hormones bradykinin and kalidin, which are responsible for the regulation of vascular tone and adaptation of the body to environmental conditions;
- frequent episodes of acute respiratory viral infections, herpetic rashes (including in the oral cavity, stomatitis), inflammation of the vulva, the development of allergic dermatitis, rhinitis, warts on the palms and soles;
- pathological discharge from the genital tract.
Lichen sclerosus in girls is recurrent until puberty, after which spontaneous self-healing can occur.
What is it about?
Lichens are commonly referred to as a whole group of health disorders characteristic of humans. All diseases in this group are skin diseases, but have different origins.
The name came to us from the Greek language, where it meant infection, lichen. In the 19th century, scientists of the Herb included lichen among skin ailments, thereby medicine was finally able to resolve the issue of classifying the disease, which had been the subject of several centuries of discussion.
Nowadays, it is customary to divide lichen sclerosus into:
- brilliant;
- forming spines;
- tropical;
- linear;
- sclerotic atrophic.
Diagnostics
Diagnosis of this disease is carried out mainly on the basis of the characteristic external signs and complaints of the patient.
The set of diagnostic procedures includes:
- collection of anamnesis data (survey);
- examination of the genital organs in a gynecological chair or on a couch;
- general blood test (a decrease in the number of neutrophils, platelets, and an increase in the number of lymphocytes is noted);
- smear for microflora (to determine the pathogen in vulvovaginitis);
- cytological and histological examination of scrapings from a damaged area of skin;
- Serum ELISA to detect herpes viruses, cytomegalovirus, Epstein-Barr virus;
- study of hormone levels, cytological analysis of vaginal smear;
- Ultrasound of the pelvic organs (if indicated).
Consultations with an allergist, immunologist, otolaryngologist, dermatologist and pediatrician (therapist) may also be required. Similar symptoms are observed in other diseases.
During the examination, differential diagnosis is carried out with such pathologies as:
- Vitiligo is a skin disease in which the melanin pigment disappears in certain areas of the skin and they become discolored. With vitiligo, there are no inflammatory manifestations, itching or swelling of the tissues, and the spots have clear boundaries, along the edge of which you can see a halo with hyperpigmentation.
- Milian's white atrophy , which occurs due to damage to small capillaries in the skin. As a rule, this disorder occurs on the legs and appears as whitish foci of atrophy with a dark rim. Spider veins and spider veins may be present in the center of the formations. Often this manifestation occurs in patients with diabetes.
- An undifferentiated type of leprosy (leprosy), in which discolored spots of different sizes appear, in which there is no sensitivity and sweating.
- Lichen planus (atrophic form). With this disease, pink spots are present on the skin. For its diagnosis, histological examination of tissue is crucial.
Buy online
Differential diagnosis
Differential diagnosis in the early stages should be carried out with the following diseases [1, 2, 13-15]:
- with neurodermatitis - the epithelium is thickened, compacted, dry, the skin pattern is enhanced with inflammatory papules of a brownish-pink color, the skin is hyperemic, shagreen-like, itching appears and on other parts of the body;
— vitiligo is characterized by a lack of pigmentation, sometimes mild itching, and no atrophic changes;
- for lichen planus - multiple grouped papular rashes with atrophic changes or sclerosis with the formation of keloid-like scars;
- with diabetes mellitus - severe itching of the vulva, the tissues of the external genital organs are swollen, have a “doughy” consistency, and are sharply hyperemic.
As a chronic inflammatory dermatosis with a long course of cycles of “itching-scratching-itching” and the formation of scars, SALV is a triggering factor for carcinogenesis or contributes to it. Apparently, dysregulation of immune processes also predisposes to the development of vulvar malignancy.
Treatment
One of the initial measures is the elimination of irritating factors, careful care of the vulva, treatment of secondary infections, local use of estrogens, which prevents atrophy of the vulva and vagina. This consists of following a diet (excluding spicy, salty, sweet foods, caffeine-containing products, alcohol) and intimate hygiene rules (limiting/excluding soap-containing products, deodorants, synthetic underwear, pads, tampons). For severe manifestations of itching, desensitizing therapy and sedatives are recommended [2].
The most widely accepted and recommended gold standard treatment for PALS is topical application of ultrapotent corticosteroid ointments [16], especially clobetasol propionate 0.05% ointment. The anti-inflammatory properties of clobetasol are most effective in the treatment of SALV, which is reflected in the reduction of inflammation and the prevention of progression of the condition and subsequent scarring. Topical ultrapotent corticosteroids are first-line therapy in the treatment of SALV (mometasone furoate, clobetasol proprionate (Ib, A). Clinical guidelines published in 2019 by the American Association of Child and Adolescent Gynecologists suggest the use of highly active glucocorticoid drugs in the long term as first-line drugs mode.They have the following effects:
- anti-inflammatory effect;
- antihyperplastic effect on the proliferating superficial layers of the skin;
- antiallergic, local analgesic and antipruritic properties;
- inhibitory effect on the functions of cellular and humoral immunity.
Summarizing recommendations for the treatment of SALV in children, taking into account the level of evidence, American colleagues presented them as follows:
1. Therapy in patients with SALV should begin with the use of highly active glucocorticoid drugs. Level II-2 B
.
2. There is limited data justifying the possibility of using immunomodulators both when treatment is ineffective and when patients refuse medications with glucocorticoids. Level II-3 B.
3. SALV should be suspected in children if there are complaints of various disorders of urination and defecation, including dysuria and dyschezia. Level C
.
In patients with SALV, it is necessary to exclude autoimmune diseases. It should also be noted that the diagnosis of SALV in children and adolescents does not necessarily require a vulvar biopsy. A biopsy of the skin of the vulva can be performed only if there are areas of the skin of the vulva and perianal area suspicious for atypia and/or with persistent resistance to therapy.
Patients with SALV require mandatory monitoring every 6-12 months to assess complaints, exclude changes in the architecture of the vulva and perianal area, and also to prevent the possible risk of malignancy [6].
As already noted, in the treatment of SALV, super-potent corticosteroids clobetasol or halobetasol in the form of 0.05% ointments are used. Because relapses can be frequent, prolonged, and can lead to atrophy and scarring, long-term maintenance therapy is recommended and is considered safer. Since there are no randomized controlled studies comparing the potency of steroids, the frequency of use and duration of treatment for each patient is selected on an individual basis. According to the results of a study by M. Gurumurthy et al. [17] reported that in a trial of clobetasol propionate ointment, complete remission was achieved in 66% of patients and a partial response to treatment was obtained in 30%. The scars did not progress. Conversely, there was no improvement in 75% of patients without treatment, and progression of scars was observed in 35% of women [17].
Depending on the severity of the clinical effect, modern topical corticosteroids (TCS) are divided into four groups [3, 18, 19] (Table 1):
Table 1. Current topical corticosteroids
- weakly active drugs (hydrocortisone 1%, prednisolone 0.5%, fluorocinolone acetonide 0.0025%);
- drugs of moderate action (alclomethasone dipropionate 0.05%, betamethasone valerate 0.025%, clobetasol butyrate 0.05%, deoxymethasone 0.05%, flumethasone pivalate 0.02 and 2%);
- potent drugs (betamethasone valerate 0.1%, betamethasone dipropionate 0.025 and 0.5%, butesonide 0.25%, fluorolorolone acetonide 0.025%, fluorcinoid 0.05%, fluorcinolone acetonide 0.025%, triamcinolone acetonide 0.02, 0 .1% and 2%, methylprednisolone aceponate 0.1%, hydrocortisone 17-butyrate 0.1%, mometasone fluorate 0.1%);
- drugs with very strong activity (clobetasol propionate 0.05%, difluorocortolone valerate 0.05%, galcinonide 0.1%).
Corticosteroids include halogenated (fluorinated) and non-halogenated ones [18-20]. Fluorinated corticosteroids (dexamethasone, betamethasone, flumethasone, triamcinolone, clobetasol, fluticasone, fluocinolone, flumethasone), as a rule, have greater anti-inflammatory activity, but more often lead to side effects. Non-halogenated corticosteroids include prednisolone derivatives (mometasone fuorate, methylprednisolone aceponate, hydrocortisone acetate and hydrocortisone 17-butyrate) [3, 20].
The mucous membranes of the vulva are relatively resistant to steroids, which suggests using ointments with maximum steroid potency to achieve a good effect. For 2-3 months they are applied daily, then 3 times a week in a thin layer on the vulva. In the circumference of the anus, where the skin is thinner, the ointment is applied daily for 4 weeks, followed by a transition to three times a week, and later - once or twice a week. The effectiveness of treatment is evidenced by a significant reduction in the number of cracks, erosions, hemorrhages and thickened white lesions. Even with effective treatment, they do not always disappear completely.
Various dosing regimens can be used. One of the most common is the daily use of high and maximum potency steroids: once a day for 3 months. In children, to avoid skin atrophy, TCS is used weekly for 3 months.
The use of TCS twice daily has additional benefit in the onset of lichen sclerosus. Proactive maintenance therapy with twice-daily mometasone furoate ointment 0.1% is effective and safe in maintaining remission and may help prevent the occurrence of malignant changes (Ib, A). The use of 30 g of the maximum potency steroid should continue for 3 months.
In postmenopause, long-term, for 6 months, use of corticosteroids of maximum activity is necessary. Within 12 weeks, in 77-90% of observations, it is possible to achieve significant improvement and disappearance of complaints, and in 23% of observations, complete disappearance of skin changes. Long-term treatment allows you to maintain remission of the disease for a long time. The patient should be monitored throughout her life. For thickened, hypertrophied, treatment-resistant lesions, administration of triamcinolone into them can be effective [1]. The use of TCS in combination with antibacterial and antifungal agents, such as gentamicin or fusidic acid and nystatin or azole antifungals, may be advisable when a secondary infection occurs. They can be used for a short period of time to eliminate infection (IV, C).
An allergic reaction to any corticosteroid ointment may occur after prolonged use. It should be taken into account that TCS can change the manifestations of some skin diseases, which can complicate the diagnosis. In addition, the use of TCS may delay wound healing [21].
When carrying out long-term local corticosteroid therapy in the anogenital area, serious side effects are detected:
- skin thinning;
- “rebound” reaction, which occurs when therapy is suddenly stopped and manifests itself in the form of dermatitis with intense redness of the skin and a burning sensation;
- formation of striae;
— development of fungal infections;
- suppression of adrenal function as a result of systemic absorption.
According to research results [2], it has been proven that all side effects resolve quickly as the activity of topical corticosteroids decreases and the frequency of their use.
The selection of treatment tactics for SALV is based on theoretical assumptions. Therapy for patients suffering from SALV is associated with polypharmacy, as it should help simultaneously eliminate the phenomena of atrophy, hyperkeratosis, reduce microcirculatory disorders, inflammation, and improve the healing of erosions on the skin of the vulva and perineum. However, the inappropriate use of antiseptics, antibiotics, antiviral and other groups of drugs often increases the activity of the pathological process and the spread of SALV. In case of lichen sclerosus, long-term observation is necessary to prevent increasing scarring and early detection of malignant neoplasm, the risk of which is not great, but real. As a rule, treatment leads to long-term remission. Its absence is a reason to doubt the diagnosis. A possible complication is contact dermatitis as a reaction to local treatment or excessively careful hygiene, infection, or the development of vulvar cancer. The ineffectiveness of local corticosteroid therapy is often associated with a violation of the patient's regimen, including due to misunderstanding or the inability to fully apply the ointment due to obesity or arthritis. Scars can be painful.
According to the European guideline for the management of vulval conditions 2019, patients with SALV require treatment [21]. About 10% of patients are not pruritic but have clinical signs of lichen sclerosus and should also be treated (IV, C).
In recent years, there has been a debate among specialists about the need to continue further treatment while relieving the initial symptoms. This is due to the fact that there is no data on disease activity at that time. However, it is indicated that SALV can progress further and lead to scarring, despite the lack of symptoms after prophylactic treatment, patients are indicated for continuous therapy for many years to prevent progression (IV, C).
A 5-year follow-up period showed that continuous treatment with an individually selected corticosteroid prevented the progression of symptoms, further scarring and the development of carcinoma, respectively, in 58% of cases versus 93.3%, 40% versus 3.4%, and 0% versus 4. 7% [21].
One of the representatives of the modern generation of TCS is the domestic combination drug for external use - tetraderm (Table 2).
Table 2. Composition of tetraderma cream for external use According to its pharmacological action, it has anti-inflammatory, antibacterial, wound-healing, antifungal, and glucocorticoid effects.
Pharmacodynamics
The activity of the drug is due to the pharmacological properties of the components included in its composition.
Gentamicin is a broad-spectrum antibiotic from the aminoglycoside group. Has a bactericidal effect, active against gram-negative microorganisms: Pseudomonas aeruginosa, Aerobacter aerogenes, Escherichia coli, Proteus vulgaris, Klebsiella pneumoniae
;
gram-positive microorganisms: Staphylococcus aureus
(coagulase-positive, coagulase-negative and some strains producing penicillinase).
Dexpanthenol is a derivative of pantothenic acid. Stimulates skin regeneration, normalizes cellular metabolism, accelerates mitosis and increases the strength of collagen fibers. Penetrates into all layers of the skin. It has a weak anti-inflammatory effect.
Mometasone is a synthetic CS that has a local anti-inflammatory, antipruritic and anti-exudative effect, induces the release of proteins that inhibit phospholipase A2 and lipocortins, which control the biosynthesis of inflammatory mediators (prostaglandins and leukotrienes, cellular inflammatory mediators) by inhibiting the release of their common precursor - arachidonic acid.
Econazole is a synthetic imidazole derivative. It has an antifungal and antibacterial effect, inhibits the biosynthesis of ergosterol, which regulates the permeability of the cell wall of microorganisms. It is easily soluble in lipids and penetrates well into tissues; it is active against dermatophytes Trichophyton, Microsporum, Epidermophyton,
yeast-like fungi of the genus
Candida, Corynebacterium minutissimum,
as well as
Malassezia furfur (Pityrosporum orbiculare)
, which causes pityriasis versicolor, and some gram-positive bacteria (streptococci, staphylococci).
Indications for use of the drug Tetraderm
Treatment of dermatoses of inflammatory origin with concomitant bacterial and mycotic infection or a high probability of secondary infection (simple and allergic dermatitis, atopic dermatitis (including diffuse neurodermatitis), limited neurodermatitis, eczema, dermatomycosis (dermatophytosis, candidiasis, pityriasis versicolor), especially when localized in the groin area and large folds of skin; simple chronic lichen (limited neurodermatitis).
Directions for use and doses
Externally.
The cream is applied to the affected areas of the skin in a thin layer, gently rubbing, 2 times a day until a positive clinical result is achieved. The duration of treatment is individual, depends on the size, location of the lesion and the severity of the disease and is usually 1-2 weeks. It is not recommended to use Tetraderm for more than 4 weeks.
Second-line therapy for SALV
Topical calcineurin inhibitors (TCIs) - pimecrolimus, tacrolimus - have a dermatotropic, immunosuppressive, anti-inflammatory local effect, specifically bind to the cytosolic receptor macrophilin-12 of T-lymphocytes and inhibit calcium-dependent phosphatase - calcineurin. Currently, TICs are recommended as second-line therapy for SALV. Pimecrolimus cream 1% is an immunosuppressant that inhibits T cell activation by blocking the transcription of early cytokines, and thus significantly reduces the itching, burning and inflammation associated with SALV. In addition, it prevents the release of pro-inflammatory cytokines, mediators of inflammation from mast cells in vitro
in response to stimulation by IgE antigen, does not affect keratinocytes, fibroblasts and endothelial cells.
Although TCIs can provide effective symptomatic relief, topical clobetasol is superior to pimecrolimus in reducing inflammation and improving clinical symptoms. However, pimecrolimus cream has a more acceptable safety profile and does not cause skin atrophy, although its use is associated with an increased risk of complications due to suppression of local immunity. As a result, TCI should be administered under the supervision of a specialist who can monitor the potential risk of malignancy of SALV. Given the proven effectiveness and safety of topical corticosteroids, experts agree that TICs should be reserved for cases of SALV not responding to topical corticosteroids [2].
TIC is used externally 2 times a day, applied in a thin layer to the affected areas of the skin and gently rubbed until completely absorbed. Treatment is continued until symptoms disappear completely. At the first signs of relapse, therapy should be resumed. If symptoms persist for 6 weeks, the patient's condition should be re-evaluated.
The most famous forms of TEC:
1. Tacrolimus - Protopic ointment 0.03 and 0.1%. Undesirable effects of this drug include: burning and itching sensation, redness, pain, irritation, rash at the application site, development of folliculitis and acne. Isolated cases of malignancy (skin and other types of lymphomas, skin cancer) have been recorded.
2. Pimecrolimus - Elidel cream 1%. Side effects include a burning sensation at the site of application of the cream, the development of impetigo and skin infections, rhinitis, and urticaria.
The most relevant seems to be 0.03% tacrolimus ointment for the effective treatment of children with anogenital lichen sclerosus 2 times a week, while reducing relapses is possible (IIIA, B). A comparison of pimecrolimus (1% cream) and clobetasol propionate (0.05%) cream showed an improvement in the symptoms of itching, burning, pain 12 weeks after the onset of vulvar lichen sclerosus, while clobetasol was used to quickly relieve the inflammatory process (Ib, A) . Other studies of pimecrolimus showed that 42% of patients were in “complete remission” after 6 months of use (IIb, B). Local irritation was the most common side effect with tacrolimus and pimecrolimus. The long-term risks of TIC use still need to be studied, as there are concerns about the possibility of an increased risk of malignancy due to local immunosuppression with long-term SALV therapy [21].
Emollients
One of the important components of SALV therapy are emollients ( eng.
. emollient - emollient) softening and moisturizing agents. These products do not contain potential allergens such as propylene glycol and lanolin, can minimize local inflammation, increase the moisture content of the stratum corneum of the skin, strengthen weakened skin barrier function and reduce subclinical inflammation [2].
According to the results of a study conducted by T. Simonart et al. [22], it was found that more than 50% of women who used a daily moisturizer along with topical corticosteroids maintained remission for 58 months. And more than 2/3 of women stopped using topical corticosteroids while remaining on emollients for a long time.
Based on their source of origin, emollients are divided into plant (natural), chemical and synthetic. Plant emollients are, first of all, natural oils. They soften the skin and protect it, making it elastic. They are absolutely harmless. These include popular cosmetic oils: peach, olive, jojoba. Chemical emollients include paraffin, petroleum jelly and ointments based on it (“Propolisnaya”, “Calendula”), and mineral oils. Synthetic emollients are produced industrially by carrying out various reactions and mixing fatty acids, esters and other components. These are cyclomethicones, dimethicones and synthetic oils. The most well-known and studied are the products from the Emolium, Locobase Ripea, and Lipikar line.
Effects of emollients:
— begin to act immediately after application to the skin, reducing moisture evaporation due to the occlusion effect;
— with further penetration into the stratum corneum, the lipids replace the missing lipids of the epidermis and maintain skin moisture for several hours (medium-term effect);
- lipids reach the deeper layers of the skin and enter the empty “storage areas” - lamellar bodies; if necessary, they are released to maintain the water-lipid balance of the skin (long-term effects).
Estrogen-containing drugs
This group of funds
has a proliferative effect without having a systemic effect on the endometrium and mammary glands [23, 24]. Orniona cream is one of the most modern domestic preparations that contains estriol, an analogue of the natural female hormone. Estriol is used to correct estrogen deficiency in pre- and postmenopausal women. Effective in the treatment of urogenital disorders. In the case of atrophy of the epithelium of the vagina and cervix, which occurs with SALV, estriol stops these disorders, helps restore normal microflora and physiological pH of the vagina, thereby increasing the resistance of the vaginal epithelium to infectious and inflammatory processes. Unlike other estrogens, estriol interacts with the nuclei of endometrial cells for a short period of time, so that with daily use of the recommended daily dose, endometrial proliferation does not occur. Thus, there is no need for cyclic additional administration of progestogens, and “withdrawal” bleeding is not observed in the postmenopausal period.
Indications for use:
- hormone replacement therapy (HRT) for the treatment of atrophy of the mucous membrane of the lower urinary and genital tract associated with estrogen deficiency in postmenopausal women;
— pre- and postoperative therapy in postmenopausal women who are about to undergo or have already undergone surgery via vaginal access;
- for diagnostic purposes in case of unclear results of cytological examination of the cervical epithelium against the background of atrophic changes (as an adjuvant).
Contraindications for use:
- established hypersensitivity to the active substance or to any of the excipients of the drug;
- untreated endometrial hyperplasia;
- established, known or suspected breast cancer;
- diagnosed or suspected estrogen-dependent tumors (for example, endometrial cancer);
- bleeding from the vagina of unknown etiology;
- thrombosis (venous and arterial) and thromboembolism currently or in history (including deep vein thrombosis, pulmonary embolism, myocardial infarction, stroke), cerebrovascular disorders;
- conditions preceding thrombosis (including transient ischemic attacks, angina) currently or in history;
- congenital or acquired predisposition to the development of arterial or venous thrombosis, for example deficiency of protein C, protein S or antithrombin III;
- liver disease in the acute stage or a history of liver disease, after which liver function tests have not returned to normal;
- porphyria;
- pregnancy and breastfeeding.
Directions for use and doses
Ornion cream should be inserted into the vagina before bed using a calibration applicator. One dose (when filling the applicator to the ring mark) contains 0.5 g of Ornion cream, which corresponds to 0.5 mg of estriol. The course of treatment consists of prescribing estriol at a dose of 500 mcg per day for 2-3 weeks daily, then switching to a maintenance dose 1-2 times a week. A small part of a single dose is applied directly to the vulva, and the rest into the vagina with a dispenser. With the detachment of hyperplastic plaques, there is increased pain that passes quickly.
Ornion cream can be used both in women with a history of hysterectomy and in women with an intact uterus. When carrying out HRT for the treatment of atrophy of the mucous membrane of the lower urinary and genital tract associated with estrogen deficiency in postmenopausal women, one intravaginal cream is administered daily for no more than two weeks until symptoms alleviate. Then the dose is gradually reduced to a maintenance dose depending on the clinical picture (for example, one injection 2 times a week).
For pre- and postoperative therapy in postmenopausal women who are about to undergo or have already undergone surgery via vaginal access, one intravaginal injection of cream is performed daily for 2 weeks before surgery, one injection 2 times a week for 2 weeks after surgery. For diagnostic purposes, if the results of a cytological examination of the cervical epithelium against the background of atrophic changes are unclear, one intravaginal administration of the cream is performed every other day for 1 week before taking the next smear.
If the next dose of the drug has been missed, you should continue to use the drug according to the usual regimen, without making up for the previously missed dose. You cannot administer 2 doses of the drug in 1 day. When initiating or continuing treatment for postmenopausal symptoms, use the lowest effective dose for the shortest possible duration.
In women not receiving drugs intended for HRT, or women who are switching from continuous use of oral combination drugs for HRT, treatment with Orniona can be started on any day.
Women who are switching from a cyclic regimen of oral HRT medications should begin treatment with Orniona 1 week after stopping these medications.
Side effect
Like any drug applied to the mucous membrane, Ornion cream may cause local irritation or itching. Acyclic bleeding, breakthrough bleeding, and metrorrhagia are possible. In rare cases, breast tenderness, tenderness, tenderness, or enlargement may occur. As a rule, these side effects disappear after the first weeks of treatment, in addition, they may indicate that the dose of the drug was prescribed too high. With long-term treatment with hormones, you should pay attention to the pigmentation of the vulva. If pigment spots appear during treatment, completion of the course of treatment is indicated.
Topical hormonal therapy (progesterone or testosterone) has failed to demonstrate effectiveness in controlled studies (IIa, B)
Treatment of lichen sclerosus using photodynamic laser
One of the modern and gentle methods of treating SALV is photodynamic therapy (Ib, A). It has been used in Russia for more than 20 years. It is based on the activation of a photosensitizer applied to the affected area of the skin by laser radiation energy with the subsequent formation of singlet (atomic) oxygen, which has a selective cytotoxic effect on damaged tissues [25-27].
The photodynamic therapy method is based on the ability of a drug to selectively accumulate in a tumor or affected skin cells and generate singlet oxygen, which has a toxic effect on tumor cells and a modifying effect on their membranes when exposed to light with a wavelength corresponding to one of the absorption peaks of the drug (406, 506, 536, 608 or 662 nm). Due to the low penetrating power of radiation and minor tissue damage, rough scars and stenoses do not form, swelling is reduced, and healing time is shortened, which is facilitated by the biostimulating properties of laser radiation.
The differences between photodynamic therapy and other laser treatment methods [26, 28] are as follows:
— non-contact (impossibility of infecting the patient);
- painless and bloodless treatment procedure;
— rapid healing, preservation of tissue structure;
— absence of postoperative scars;
— significant reduction in the observation period;
- rapid restoration of full performance.
Fractional photothermolysis with a CO2 laser for scleroatrophic changes in the vulva
Microablative fractional CO2 laser is commonly used as an effective method for skin rejuvenation and restoration of skin quality. Recently, this technique has been used for symptomatic vulvovaginal atrophy and genitourinary syndrome during menopause to treat the skin of the vulva and vagina, as well as for the treatment of vestibulodynia and vulvar lichen sclerosus associated with changes in vaginal microbiocenosis [29, 30]. According to clinical studies, a significant reduction in pain, burning and dyspareunia, and a significant improvement in the condition of the vaginal vestibule in general were revealed in women who underwent three sessions of fractional CO2 laser treatment for lesions of the vaginal vestibule. The majority (92.6%) of patients reported significant improvement or that their condition was somewhat improved by the laser procedure. In addition, encouraging treatment results have been obtained for lesions of the vaginal vestibule in women with SALV using a simple fractional CO2 laser. To further confirm the obtained results, further studies with a longer observation period and in accordance with all GSP rules and standards are needed [31].
Analysis of the effectiveness of radio wave treatment and laser destruction for dystrophic diseases of the vulva
Extensive experience has been accumulated in the treatment of patients with SALV using radio wave and laser methods. However, with laser therapy there are problems of a high frequency of recurrence, the formation of extensive foci of deformation of the vulva, and often complete ineffectiveness. All this highlighted the need to search for new approaches using alternative types of surgical energies [32–34]. Radio wave therapy rightfully occupies a leading position in the treatment of cervical pathology, having a number of advantages over laser. Since 2013, a method of treating patients with lichen sclerosus using the Surgitron radio wave apparatus has been introduced, which has a number of advantages over a laser, which is explained by the peculiarities of the impact of high-frequency radio waves on living tissue. Some of the clear advantages are the following: a minimal area of lateral coagulation necrosis, a significant reduction in epithelialization time, a good cosmetic effect, and the absence of scar deformities and stenoses. Thus, the zone of altered epithelium caused by the action of high-frequency radio waves at the excision site is 0.04 mm, the laser causes tissue disintegration at a distance of 1.20 mm, ultrasound - 1.13 mm. A very important point at the stage of diagnosing a pathological process is the adequate taking of biopsies by obtaining high-quality material for histological examination.
According to the results of a study with a comparative analysis of almost 100 cases of treatment of lichen sclerosus over a period of 3 years [35], it was proven that laser destructive methods are highly traumatic, have low effectiveness in the treatment of lichen sclerosus, and are characterized by a high incidence of complications. 37% of women who underwent laser destruction experienced impaired sexual function, and 42% of patients expressed dissatisfaction with the cosmetic results. The use of laser destruction for lichen sclerosus leads to aggravation of the course of degenerative processes, the formation of rough scars and the development of relapse in 62% of cases within 1 year after treatment. The recurrence rate after radio wave excision of foci of dystrophy is much lower and is only 26%. The use of radio waves in the treatment of lichen sclerosus has shown good results. The method has a number of advantages: rapid epithelization, shortening of the rehabilitation period, good cosmetic effect and low recurrence rate.
Thus, the polyetiology and pathogenetic features of lichen sclerosus of the vulva cause certain diagnostic and therapeutic difficulties. The clinician’s task is to identify several main ways to improve treatment outcomes, implying primary and secondary prevention of the disease. Primary prevention includes: prevention and adequate treatment of urogenital infections, normalization of immunodeficiency states, metabolic and endocrine disorders, restoration of vaginal microbiocenosis.
Secondary prevention consists of timely and adequate treatment of benign degenerative processes of the vulva. Therapy for these conditions of the vulva should not be carried out without histological clarification of the diagnosis. Conservative drug treatment of dystrophic diseases of the vulva in the absence of effect should last no more than 6 months. If treatment is ineffective, it is necessary to promptly raise the issue of using modern and gentle treatment methods, such as photodynamic therapy.
The material was prepared with the support of. The company had no influence on the collection and analysis of literature data, writing and editing the text of the article.
The authors declare no conflict of interest.
*e-mail; https://orcid.org/0000-0001-6155-788X
Treatment of girls, women
Lichen sclerosus in girls and women is treated using the following groups of drugs:
- antiviral and antifungal agents;
- antihistamines (to reduce itching and inflammation);
- vitamin complexes and enzymes to eliminate metabolic disorders;
- regenerative medicines to improve blood microcirculation, cellular nutrition and tissue restoration;
- immunostimulants.
The treatment tactics are similar to those used for focal scleroderma. There are no specialized drugs to treat this disease.
Medicines
Among the antibacterial agents, the drugs indicated in the table below are prescribed.
| Name | Dosage | Contraindications | Average price, rub. |
| Benzylpenicillin, intramuscular injections | Children over 1 year – 50 thousand units per 1 kg of weight, adults – 250 thousand units 4 times a day for 2 weeks | Increased sensitivity | 7 (1 bottle 1 million units) |
| Amoxicillin, tablets | Children over 5 years old and adults – 1 tablet 250 mg 2 times a day, course of treatment – 7-10 days | Bronchial asthma, hay fever, ARVI, mononucleosis, lymphocytic leukemia, intestinal infections accompanied by diarrhea and vomiting | 60 |
| Ampicillin, powder for suspension (oral administration) | Children weighing up to 20 kg - 20 mg per 1 kg of weight, adults - 250 mg 2 times a day | Mononucleosis, lymphocytic leukemia, liver pathologies | 30 |
Among angioprotectors (medicines that strengthen the walls of blood vessels), the drugs described in the table below are prescribed.
| Name | Dosage | Contraindications | Average price, rub. |
| Pentoxifylline injection | Intramuscularly 100-200 mg | Myocardial infarction, hemorrhage, stroke, pregnancy, breastfeeding, arrhythmia, low blood pressure | 130 |
| Trental, concentrate for infusion | Children – 100 mg 3 times a day, adults – 250 mg | 150 | |
| Xanthinolanicotinate, solution for IM and IV administration | The same as the previous drug, as well as acute or chronic cardiac, renal failure, ulcerative lesions of the gastrointestinal tract, glaucoma | 140 |
The following are prescribed as enzyme agents:
| Name | Dosage | Contraindications | Average price, rub. |
| Lidaza, solution for injection | 64 IU | Malignant and acute infectious and inflammatory processes, lung pathologies accompanied by bleeding, tuberculosis, hemorrhages in the eyes, estrogen intake, hypersensitivity | 190 |
| Mezim forte, tablets | Children – 500 units per 1 kg of weight during each meal, adults – 2 tablets | Children under 3 years of age, acute pancreatitis, hypersensitivity, hereditary galactose intolerance, lactase deficiency, malabsorption | 160 |
| Longidaza | Solution 3000IU for intramuscular injections, for adult women - vaginal suppositories (1 pc. 10 days) | Same as Lidaza's | 1830 |
For external therapy, the medications listed in the table below are used.
| Name | Dosage | Contraindications | Average price, rub. |
| Solcoseryl ointment | 2 times a day, 14 days | Increased sensitivity | 850 |
| Gel Troxerutin | 45 | ||
| Methyluracil ointment 10% | 45 | ||
| Hydrocortisone ointment 1% | Skin ulcers, infections, tuberculosis, syphilis, acne, tumors, children under 2 years of age, pregnancy, hypersensitivity | 33 |
As vitamin therapy, Aevit or other complex products are prescribed, which contain A, E, B, D2, and nicotinic acid.
Non-drug therapy
Lichen sclerosus in girls and women, after stopping the acute stage of the disease, can be treated using the following types of physiotherapeutic procedures:
- phonophoresis (ultrasonic influence) on the affected areas with Lidaza and Madecassol (an ointment containing tiger grass extract, which is used for chronic skin diseases);
- paraffin therapy and mud therapy;
- balneotherapy (therapeutic baths);
- short-term exposure to low-intensity laser radiation for 3 minutes (has an analgesic, vasodilator and anti-inflammatory effect);
- magnetic therapy on affected areas.
Surgical intervention
With late diagnosis of the disease and lack of treatment, girls develop synechiae - fusion of the labia, which can lead to complete closure of the vaginal opening and blockage of the urethra. At the initial stage, this process can be stopped using estrogen-containing external agents.
The duration of such treatment is on average 2 months.
In advanced cases, surgery is required to separate the labia. It is done under local anesthesia. Complications of the operation may include scarring of the skin and recurrence of fibrous fusion.
ethnoscience
In folk medicine, the following recipes are used to treat this disease:
- Sitz baths with herbs that have an anti-inflammatory effect - chamomile, string, calendula, St. John's wort. To prepare them, pour 3 liters of water into a large saucepan, bring to a boil, then add 1 tbsp. dry raw materials, stir well. Turn off the heat and leave for 30 minutes. Baths are taken daily for 15-20 minutes. The water temperature should be around 38°C.
- Lubricate the affected areas with sea buckthorn oil. This procedure is an analogue of medicinal regeneration agents (Actovegin, Solcoseryl). The oil helps reduce inflammation and promotes healing of minor wounds and ulcers.
- Aloe cream. Its action is similar to the previous recipe. To prepare it, you need to grind the pulp of the leaves of the plant so that you get a paste. 4 tbsp. l. stir in ½ tbsp. olive oil and lubricate the affected areas with this product 2 times a day.
- If the first 3 recipes are applicable for both children and adults, then this one can only be used by mature women whose vulvar kraurosis is caused by a low concentration of estrogen. Mix oregano flowers, wormwood, and hogweed in equal proportions. 1 tbsp. l. mixture pour 1 tbsp. boiling water, leave for 1 hour. This amount should be drunk in 2-3 doses during the day. The course of treatment is 2-3 months.
Treatment
The appearance of spots on the skin outside the genital organs does not require intensive care. Rashes in the arm and chest area often go away quickly on their own. Deprivation of the genitals requires special attention.
With pathologies of the genital organs, scars often remain, which cause urinary dysfunction and decreased sexual activity. Therefore, even with minor symptoms of the genital form of lichen sclerosus, you should undergo examinations and begin treatment immediately.
Dermovate - glucocorticoid ointment for lichen
When women become ill, drug therapy is carried out. During the treatment process, various glucocorticoid ointments are used:
- "Klovate";
- "Powercourt";
- "Dermovate."
Treatment with drugs is prescribed for four months. For the first thirty days, the ointment is used twice a day. The rest of the time, the products are applied to the affected areas once a day. To avoid relapse after eliminating the lesion, treatment with such drugs continues at intervals of three to four days.
Treatment of lichen in women should be accompanied by a visit to a dermatologist. The need to examine the skin is caused by the duration of use of potent ointments. Sometimes the following side effects occur:
- redness of the skin;
- fungal infections;
- stretch marks of the skin on the affected areas.
Allergic reactions are occasionally observed. If treatment with hormonal drugs does not give the desired result, then additional drugs are prescribed:
- sedative medicinal substances that relieve irritation;
- calcineurin inhibitors;
- preparations with retinoids.
In most cases, young girls with pathology are not prescribed treatment, since the disease disappears during puberty. But still, sometimes lichen sclerosus leaves traces - darkening of the skin or scars.
For diseases of the male genital organs, surgical procedures are performed. Mostly circumcision of the foreskin is practiced. With this treatment, the likelihood of relapse is reduced to zero.
Treatment of lichen sclerosus is carried out only in specialized centers, and all drugs are prescribed only by a doctor. Self-medication of pathology is unacceptable, as it can lead to irreparable consequences, the most dangerous of which is cancer.
Prognosis and complications
Medical research shows that in most cases, girls under 12 years of age have a favorable prognosis for the disease. By the time the first menstruation arrives, regression of pathological processes may occur. Cases of self-healing are also often observed, especially with skin lesions outside the genital area. At a later age, the disease becomes chronic and difficult to treat.
To prevent exacerbations, you should adhere to the following recommendations:
- wear only cotton underwear that does not restrict movement;
- avoid the use of detergents and hygiene products (soap, gel, pads) that cause skin irritation;
- try not to scratch the skin, despite itching;
- use moisturizers with lanolin (if there are no allergic reactions to it).
Lichen sclerosus can lead to the following complications:
- Development of squamous cell carcinoma. In this regard, patients must undergo mandatory examination at least once a year.
- Formation of scars, blisters, subcutaneous hemorrhages, extensive hematomas.
- Atrophy (reduction) of the labia, synechia, narrowing of the vaginal opening.
- Painful sexual intercourse, inability to have sex and conceive a child.
Lichen sclerosus can cause serious complications in childhood and adulthood. One of the measures to prevent its occurrence in girls is a routine examination by a pediatric gynecologist, which parents should not neglect. Early diagnosis and treatment will avoid degenerative changes in tissues, as well as surgical intervention.
Therapy
If the spots are located only on the arms or chest, they do not require special treatment and disappear over time. Treatment of lichen sclerosus is necessary when the lesion is localized in the genital area. Even if the patient does not feel itching or pain, over time the spots can turn into scars that interfere with urination or impair sexual function. In addition, there is a small risk of developing skin cancer in these areas.
In men, therapy is often performed surgically. The most common method is removal of the foreskin, that is, circumcision. There are no relapses of the disease with this method of treatment.
In women, lichen sclerosus is treated primarily with medication. Even if the lesions are removed, relapses of the disease often occur.
Highly active ointments with glucocorticoids are used for therapy. They must be applied to the affected area 2 times a day every day for a month, then 1 time a day for 3 months. After the symptoms disappear, the prescribed drug should be used twice a week to prevent relapse. It is preferable to use hormonal ointment, since creams often contain fragrances or other irritants, such as propylene glycol. If symptoms reappear, the frequency of use of the drug should be increased.
The main remedy for the treatment of pathology is an ointment containing clobetasol (Dermovate, Cloveit) or a cream with this substance (Powercourt). Apply the medicine only to the affected areas, being careful not to touch healthy skin.
Elderly patients often do not understand the need for long-term use of ointments and creams, especially in the genital area. Their adherence to treatment is low. Therefore, it is important to explain the danger of malignant degeneration of the pathology. In addition, it must be explained that the disease never recedes in postmenopausal age.
With long-term use of hormonal ointments, regular monitoring by a dermatologist is necessary. These medicines may cause the following side effects:
- thinning and redness of the skin;
- stretch marks at the application sites;
- fungal infections (thrush) of the genitals.
If hormones from topical products begin to be absorbed into the blood, they can cause weight gain, frequent infections or allergic reactions. However, such adverse effects occur very rarely, so topical (external, local) glucocorticoids are the basis for long-term treatment of lichen sclerosus.
If glucocorticoid ointments are ineffective, doctors prescribe:
- retinoids (Roaccutane) – for the appearance of scars or excessive keratinization (hyperkeratosis) of the skin;
- topical calcineurin inhibitors - Pimecrolimus cream or Tacrolimus ointment (with caution);
- ultraviolet irradiation (not used for skin lesions of the genital organs);
- sedatives for severe itching at night, which causes uncontrolled scratching of tissues.
Although there are positive results from treatment with Tacrolimus, it must be used with caution. This drug inhibits the activity of the immune system, therefore increasing the likelihood of developing a malignant tumor, which has been proven in animal experiments. Pimecrolimus and Tacrolimus are immunosuppressants that effectively relieve itching, inflammation, pain and burning in skin scleroatrophy.
When symptoms of the disease appear in young girls, treatment is often not carried out. Sometimes the pathology disappears spontaneously during puberty, but in some cases scarring and hyperpigmentation of the skin remain.
Once a diagnosis has been established, you should visit a dermatologist 1-2 times a year.
If an elderly patient does not want to regularly use hormonal ointment, she should visit the gynecologist more often - up to 3-4 times a year.
Non-drug treatment and home care
Patients should avoid contact with various irritants, in particular those containing lanolin or propylene glycol, and should not wash themselves with soap. You should avoid sanitary pads and tight underwear that rub your skin.
In addition to hormonal ointment, it is necessary to use emollients - softening preparations, for example, based on Vaseline. Applying cold compresses and cool sitz baths can reduce the intensity of itching.
Women should examine their external genitalia monthly with a mirror and report them to their doctor if new symptoms appear. Patients also need to be taught how to properly apply hormonal ointment. First of all, this concerns thorough hand washing before and after the procedure, as well as avoiding contact of the ointment with sensitive areas of the mucous membrane, for example, with the eyes.
If depression or sexual dysfunction develops, patients are advised to consult a psychotherapist and sexologist. The conversation should be conducted as tactfully as possible, since patients with such pathology tend to be embarrassed and hide it.
How to treat lichen sclerosus
Treatment is prescribed taking into account the patient’s age and the degree of damage to the skin and mucous membranes. Usually prescribed:
General strengthening agents, for example, Resorquin or Delagil.
Hormonal ointments . External therapy containing corticosteroids is used in short courses, not forgetting that steroids provoke thinning of the skin.
Injections . Improvements in skin condition are noted after a course of injections of triamcialone acetonide.
Pills. In advanced cases of the disease, it is advisable to use Acitretin (systemic retinoid).
External agents that improve blood circulation and increase tissue elasticity. A good effect is observed from the use of ointment with tacrolimus (0.1%), which, due to its non-hormonal composition, can be used for a relatively long time.
Supportive therapy . There is a beneficial effect on the condition of the skin of laser and ultrasound therapy, as well as selective photocoagulation and acupuncture.
Surgery. Used in rare cases, mainly in men.
Why is lichen sclerosus dangerous?
The prognosis of the disease is relatively favorable for patients under 50 years of age. With appropriate treatment, they experience remission in 70% of cases. At the age of 50-70 years, the probability of recovery decreases to 25%. After 70 years, a cure is unlikely.
The addition of concomitant infections of bacterial or viral origin significantly complicates the course of sclerosing dermatosis. Relapses are fraught with the formation of adhesions, erosions, and cracks in the genital area.
Severe symptoms lead to problems in sexual relations. Sexual intercourse is difficult for women due to itching, pain and cicatricial narrowing of the vagina. Men may have problems with erection and urination as a result of scarring of the foreskin. Patients experience physical suffering and emotional discomfort, which leads to prolonged depression.
Skin changes in lichen sclerosus are of great danger. The volume of the skin and the elasticity of its fibers decrease. Untreated atrophy provokes the development of skin and vulvar cancer in 9% of women over the age of 60-70 years.
To avoid frequent relapses and malignant complications of lichen sclerosus, patients should visit a dermatologist or oncologist at least 4-5 times a year.
Alternative names for SL
The name lichen sclerosus has a number of synonyms. Typically, the names of the diagnosis depend on the affected area and the doctor's specialty. In gynecology, for example, this disease is usually called kraurosis of the vulva, in urology xerotic balanitis obliterans, in dermatology - lichen sclerosus. Such terms as lichen sclerosis and lichen sclerosus are known.
At the end of the 70s. The ISSVD, an international society dedicated to the study of diseases of the vulva and vagina, has recommended using the term lichen sclerosus to refer to this disease. At the end of the 90s. this recommendation is supported by the American Academy of Dermatology.
To date, professionals in the field of urology have not been able to agree on the use of the term lichen sclerosus.
What to apply?
Most often, progesterone is prescribed in the form of a cream. It is used for up to four weeks twice a day, after which they undergo a new examination by a doctor. The drug is not very effective against itching, which is different from androgen creams.
The practice of using testosterone propionate is widespread. It is also used twice daily for up to three weeks. The drug fights itching and tones the body tissues.
Local glucocortcoids are well suited for external therapy. These products have a complex effect, since the perception of histamine and serotonin by skin receptors changes, histaminase A2 is blocked, and hyaluronidase becomes more active. Vascular walls become less permeable, cell membranes are stabilized, and itching goes away.
Main causes of the disease
The exact reasons for the appearance and development of the disease are unclear. What is known is that the disease can appear as a consequence of a disruption in the functioning of the human nervous, endocrine or immune systems. It can be caused by various infections. Some people have a genetic predisposition to this disease. One of the main causes of the disease are infectious diseases and viruses that affect the human genitourinary system, and previous diseases:
- cystitis accompanied by problems with the genitourinary system;
- vulvovaginitis, vulvitis, other gynecological pathologies;
- papillomas, herpes virus and other fungal and viral diseases;
- pyelonephritis, nephritis and other kidney problems, cysts, polycystic diseases, problems with the ovaries;
- gastroduodenitis, tuberculosis, hormonal disorders;
- uterine hypoplasia, estrogen deficiency, allergies, atopic dermatitis, hay fever;
- diabetes, juvenile rheumatoid arthritis, lesions of other skin areas, focal scleroderma, psoriasis;
- Down syndrome;
- mitral valve problems;
- individual characteristics of the heart, dilation of the artery in the lungs.
Due to these diseases, the organs are weakened. People living in polluted industrial areas are more likely to develop lichen sclerosus.
Vulvovaginitis can cause the development of the disease
Prognosis and prevention
The presence of risks of degeneration of the pathology into a cancerous state, the lack of understanding of the causes of the formation of the disease allows doctors to classify lichen sclerosus as a disease with an unfavorable prognosis. The treatment undertaken does not help everyone; in advanced cases, complications arise that significantly worsen the quality of life of the sick person. Therefore, anyone who has been diagnosed with this should visit a dermatologist and oncologist every two months in order to identify the development of undesirable consequences and their timely treatment.
Treatment of lichen sclerosus
Considering that the cause of the development of lichen on the genitals is not yet known, therapy is symptomatic. Tsumbusha lichen cannot be cured. Doctors' efforts are aimed at slowing the spread of the disease and restoring tissue functionality. For this, all available methods are used.
Drugs
In the early stages, it is recommended to treat lichen sclerosus with medications. Complex therapy is prescribed, which includes:
- Corticosteroid creams and ointments based on clobetasol (Dermovate, Powercourt, Cloveit, Etrivex) are applied to dry, intact areas of the skin. Another option is corticosteroid injections.
- If hormonal therapy is ineffective, calcineurin inhibitors (tacrolimus ointment or pimecrolimus cream) are prescribed. But these drugs suppress local immunity, which increases the risk of genital cancer.
- Antimalarial drugs (Delagil, Resorcinol), according to observations, delay the further spread of lichen.
- Injections into the lower leg with anti-scarring drugs Lidase and Heparin.
Additionally, antihistamines and emollients may be prescribed to reduce itching and burning. Skin condition also improves after taking vitamins A and D.
Your doctor may prescribe a course of medications containing the sex hormones testosterone and progesterone. But such treatment was ineffective and is currently not recommended for lichen.
Folk remedies
Alternative medicine recipes are used as an aid after consultation with your doctor. Their action is aimed at softening tissues, combating itching and preventing secondary infection of damaged skin. For this you can use:
- Baths. Add 3-4 tbsp to 5 liters of hot water. l. calendula and infuse for 6 hours. Then the infusion is heated and poured into a basin. You need to sit in it for 15 minutes before going to bed for a week.
- Decoctions. Add 2 tbsp to 1 liter of water. chamomile and boil for 20 minutes. The liquid is then wrapped up and cooled. After straining, the broth is used for washing once daily.
- Alcohol tinctures. 50 g of celandine is poured into 0.5 liters of vodka. Infuse in a glass container away from the sun for 14 days. The tincture is shaken every day. The finished product is diluted by half with vodka and used for wiping. Before this, undamaged skin is lubricated with a rich cream.
You can also reduce itching with tar soap, using it during daily hygiene procedures.
Other methods
Physiotherapeutic treatments are often recommended by dermatologists as an adjunct to drug therapy. These include:
- photodynamic therapy;
- ultraviolet phototherapy;
- laser vaporization;
- cryotherapy.
These methods help to achieve temporary improvements in well-being. But, according to researchers, there is also a side effect - accelerated development of lichen.
In advanced cases, when the disease interferes with the normal functioning of organs or there is a risk of degeneration into cancer, surgical intervention is used.
The affected tissue is excised or removed. In the future, patients are recommended to undergo genital or anal plastic surgery.
Treatment for lichen sclerosus in men often involves circumcision of the foreskin on the penis, even in the early stages of the disease. This helps to slow down the development of guttate scleroderma as much as possible.
Manifestations of the disease
Symptoms of lichen sclerosus depend on the location and form of the lesion. In men and women, the clinical picture has distinctive characteristics. With a mild stage of lesions, the disease proceeds without any special symptoms
Among women
Light-colored spots called plaques form on the skin of the vulva, in the perineal area, in the perianal area, as well as on the inguinal folds. Each mark has fairly clear boundaries. Such plaques can occur in the abdomen, neck, thighs, shoulders and chest.
As the disease develops, women often experience the following symptoms:
- severe swelling of the mucous membrane of organs;
- reducing the level of tissue elasticity;
- expansion of the capillary network.
Patients have blisters filled with hemorrhagic fluid and erosion. After healing of the mucous areas, scars often form on the tissue, which can lead to fusion of the labia minora.
The disease is also accompanied by other symptoms:
- itching;
- pain;
- dysfunction of urination;
- bleeding.
As the disease progresses, sometimes there is a change in the shape of the genital organs and atrophy of the skin tissue. When skin cells are severely damaged, scratches, cracks and scratching may occur. Rarely, the development of lichen sclerosus causes squamous cell carcinoma.
In men
Pathology in males is observed much less frequently. Basically, the focus of the disease occurs in the genital area. In this case, the following symptoms are observed:
- formation of white spots;
- the formation of dryness and decreased elasticity of tissues in the affected areas;
- narrowing of the foreskin;
- Clots similar to comedones form on the hairy skin.
In the future, the disease is accompanied by problems with urination, pain, cracking, itching and atrophy of the skin. Due to tissue scarring, men may have erection problems in the future.
When the first signs of scleroatrophic type lichen appear, you must contact the specialized department of the medical center to establish an accurate diagnosis. At the initial consultation, the doctor conducts a visual examination of the affected areas.
Depending on the extent of tissue damage, a biopsy may be prescribed. This analysis is carried out to exclude cancer.
What should the treatment be?
Therapy can be prescribed only after the doctor confirms the diagnosis of lichen sclerosus. Treatment must be comprehensive. It includes drugs to improve blood microcirculation (Dipyridamole, Retinol Acetate), application ointments (Solcoseryl, Actovegin).
All patients, without exception, are prescribed a course of lymphotropic therapy with subcutaneous injection of Lidase with Heparin into the lower leg area.
Lichen sclerosus of the penis is treated with medication only in the early stages. Patients are prescribed general restorative therapy and antimalarial drugs (Delagil, Resorquin). In case of low effectiveness of conservative therapy, circumcision is indicated. When the pathological process spreads to the genitourinary canal, penile plastic surgery is usually necessary.
For representatives of the fair sex, the affected tissue is excised; in addition, plastic surgery of the vulva and anus may be required.
All patients are advised to follow a special diet and bed rest. It is advisable to isolate the patient for some time from healthy family members, since the etiology of the disease has been little studied to date. Such measures are necessary to prevent possible infection of third parties. It is not recommended to try to overcome lichen sclerosus on your own - it is quite dangerous. The pathology will actively progress, which entails the development of rather unpleasant consequences, including those of an oncological nature.
Clinical picture
Lichen sclerosus affecting the penis can last for years without causing concern to the patient. Sometimes scleroatrophic kraurosis is discovered by chance at a routine appointment with a therapist or urologist.
Lichen sclerosus manifests itself by the appearance of spots and papules. The elements of the rash are whitish in color and have clearly defined boundaries. Papules with kraurosis often merge, resulting in the formation of rather large plaques.
At the first stage of lichen sclerosus, the elements of the rash are located at the same level as the intact mucosa, but as lichen progresses, they become concave. A small depression can be seen in the center of the papules and plaques.
The openings of the sweat glands are dilated and filled with horny masses; outwardly, these formations resemble comedones. If a lot of horny plugs form in the affected area, then the lichen lesion looks warty.
With lichen sclerosus of the genital organs in men, the head of the penis and the inner surface of the foreskin are affected. Most often, the first symptoms of the disease are decreased elasticity and dryness of the foreskin. Connective tissue gradually grows in the affected areas. Complications of lichen sclerosus are:
- The development of phimosis is a narrowing and thickening of the foreskin, which leads to the inability to expose the head.
- Narrowing of the urethral opening;
- The appearance of painful cracks along the outer edge of the foreskin. Cracks often appear after sexual intercourse.
The head in lichen sclerosus is usually affected diffusely, however, in some patients the process becomes focal. The affected area becomes gray-white, sometimes with a bluish tint.
As scleroatrophic lesions develop, atrophy phenomena are observed on the tissues, the skin wrinkles, telangiectasia and peeling appear on its surface. The skin in areas of kraurosis becomes excessively thin and can easily be gathered into small folds.
With the development of kraurosis, the foreskin becomes stiffer and denser, the skin color is noticeably paler in healthy areas. In rare cases, a scleroatrophic hoop is formed that pinches the penis around its circumference.
Stages of disease development
There are four stages of the course of lichen sclerosus:
- At the first stage of lichen formation, only the foreskin is affected;
- At the next stage, the scleroatrophic process spreads to the head;
- The third stage of development of kraurosis is characterized by damage to the head, foreskin and the outer part of the urethra.
- The last, fourth stage of development of lichen sclerosus is a precancerous condition, so patients should be referred for examination to exclude the malignant nature of the disease. As a rule, a biopsy of the affected tissue is performed, followed by examination of the material to exclude the presence of atypical cells.
The causes of her illness
To date, the causes of this disease have not been fully studied. It is believed that pathologies in the endocrine, immune and nervous systems, as well as infections, play an important role in its formation. Experts suggest associations of lichen sclerosus with genetic causes, autoimmune diseases and reduced levels of endogenous hormones. Doctors have found that approximately 1/5 of women with lichen sclerosus also suffer from autoimmune disorders:
- alopecia areata;
- vitiligo;
- disorders of the thyroid gland.
In addition, scientific research shows that more than half of women with this disease have circulating autoantibodies. The prevalence of LS in close relatives supports the theory of the presence of a genetic component. Patients often have low endogenous levels of female steroid hormones. No changes in symptoms were observed during menstruation, pregnancy, hormone therapy, or oral contraception use.
Thus, we can identify certain factors involved in the formation of the disease:
- autoimmune (sometimes the manifestations of tissue damage that lichen sclerosus provokes are similar to those characteristic of autoimmune connective tissue diseases);
- genetic (research data indicate a relationship between development and expression level with the transmission of certain genes);
- hormonal (disturbances in the absorption of male sex hormones can give impetus to the development of LS);
- infectious (infectious and viral agents, such as spirochetes and human papillomavirus, can affect the appearance of LS);
- local (periodically lichen sclerosus may be associated with local trauma to the skin, for example, radiation exposure, trauma to old scars, chronic irritation of the dermis, abrasions).
Danger of skin disease
Lichen on the genitals may seem like a harmless disease. For most people, the symptoms of the disease in the initial stages do not cause discomfort. But after a few years complications appear. The most dangerous:
- Sexual dysfunction. When the tissue of the foreskin becomes sclerotized, men develop cicatricial phimosis—the inability to expose the head of the penis. Women have a similar problem due to overgrowth of the vaginal opening. Sexual intercourse becomes painful at first and then impossible.
- Secondary infection. Microorganisms affect not only areas of the skin of the penis and vulva damaged by lichen, but also the urinary tract and kidneys. The reason is inflammation that develops against the background of difficulty in the outflow of urine.
- Oncology. In 3-5% of cases, lichen degenerates into a malignant tumor. At the same time, vulvar cancer in women develops much more often than a similar lesion of the glans penis in men.
The disease is also accompanied by psychological problems associated with a feeling of constant discomfort and a drop in self-esteem due to a feeling of inferiority in the sexual sphere. Such complications can be avoided only with regular examination and timely treatment of lichen sclerosus.
What can be the prevention of genital LS?
Unfortunately, there are no effective preventive measures that could prevent LS disease. However, if you notice the first signs of LS, you should immediately consult a urologist (men) or gynecologist (women). After all, as mentioned above, if LS is not treated in a timely manner, quite serious consequences can occur.
Early removal of the affected skin tissue of the genital organs, followed by observation and, if necessary, treatment with ointments can stop the disease and prevent it from causing such dangerous complications. Before consulting a doctor, it is important to make sure (by studying his reputation based on patient reviews) that he is quite knowledgeable in the diagnosis and treatment of LS and other diseases of the genital organs.
The Andros Clinic provides treatment for all forms of lichen sclerosis of the genital organs. If necessary, all operations necessary to get rid of this disease can be performed, from circumcision to complex reconstructive operations on the urethra. If there are lesions suspicious for penile cancer, a biopsy and careful histological examination are performed.
Materials used in preparing the publication: Lazzieri M, Barbagli G, Palmintieri E, Turini D. Lichen sclerosus of the male genitalia. Contemporary Urology 2001; 3.
Otherwise, the disease is called kraurosis. In this case, the head of the genital organ is involved in the pathological process. As a rule, the disease develops in adult patients, but is relatively rare.
With kraurosis in men, not only the head of the penis is affected, but also the inner part of the foreskin. Initially, the disease manifests itself as a decrease in elasticity and the appearance of dryness in this area. In the affected areas, the so-called connective tissue grows. Complications of lichen include the following:
- Phimosis (narrowing of the foreskin, which entails the inability to fully expose the head).
- Reduction of the urethral opening.
- The appearance of cracks in this area.
With lichen sclerosus, the head is usually diffusely affected. It becomes white with a bluish tint.
As the disease progresses, atrophy of the skin areas is observed, and so-called telangiectasias appear on its surface. In total, there are four stages of development of the disease:
- At the first stage, only the foreskin is affected.
- Then the pathological process spreads to the head.
- The third stage involves damage to the entire genital organ, foreskin and outer urethra.
- The last stage of the disease is also considered precancerous. All patients are prescribed a full diagnostic examination to exclude the malignant nature of the disease.
What is lichen sclerosus (LS)?
LS is a chronic inflammatory skin disease, usually of the genital organs in men and women, the causes of which are still far from fully understood and known. However, it is now clear that if LS is not treated, this disease leads to scarring of the genital organs, which can cause serious problems. Men, in particular, may develop a narrowing of the foreskin (phimosis) and difficulty opening the glans penis. In more severe cases, a narrowing (stricture) of the external opening of the urethra and the scaphoid fossa (the part of the urethra closest to the external opening) may form, which leads to urination disorders and impaired urine outflow. Such changes can cause a decrease in quality of life, and sometimes lead to complications such as urinary tract infection (pyelonephritis, cystitis), dilation of the renal cavity system (hydronephrosis), and urolithiasis. In addition, severe forms of LS are considered predisposing conditions for the development of penile cancer.
What synonyms for disease can your doctor use when referring to LS?
Several synonyms can be used to describe SL. As a rule, the names of the diagnosis of LS may vary depending on the specialty of the doctor and the location of the skin lesion. For example, gynecologists often use the term “vulvar kraurosis”, dermatologists - “lichen sclerosus”, urologists - “xerotic balanitis obliterans”. In 1976, the International Society for the Study of Vulvar and Vaginal Diseases (ISSVD) recommended using the term lichen sclerosus to describe this disease. The American Academy of Dermatology (AAD) joined this recommendation of gynecologists in 1995.
To date, unfortunately, none of the professional urological associations have come to unity in the use of the term “lichen sclerosus” (Latin: lichen sclerosus). In Russia, in most educational institutions, LS is not taught at all to urology students as an independent form of inflammation of the glans and foreskin of the penis. In this regard, many urologists simply do not know either the symptoms of this disease or its treatment methods. Very often we have to deal with situations where patients with LS were treated with antibiotics in the form of systemic and local therapy for “banal balanoposthitis”, “fungal balanoposthitis”, “herpes”, “chlamydia”, “acquired phimosis”, etc. However, since antibiotics and antifungals are often not effective for LS, and surgical removal of phimosis (circumcision or circumcision of the foreskin) was not accompanied by further treatment, patients never received adequate care.
What else you need to know about lichen sclerosus
- It is almost impossible to prevent the development of the disease , since the causes of the disease have not been established.
- Affected skin should be carefully cared for using neutral detergents and formulations containing moisturizing and softening ingredients.
- Make sure that covers do not come into contact with synthetic fabrics, and also avoid natural, but too brightly and unstablely colored linen and clothing.
- Be careful when choosing sanitary pads ; definitely avoid scented products, which often cause irritation and allergies.
- In most cases, lichen sclerosus can be cured; it is only important to contact a specialist in time , who will prescribe adequate treatment.
Treatment of atrophic changes
Most often, lichen sclerosus can be managed using conservative therapy methods:
- Use of hormonal medications.
- Compliance with doctor's recommendations for changing lifestyle and hygiene habits.
- Use of emollients.
However, if the vagina or labia are fused, as well as if there is a significant narrowing of the urethra or foreskin, surgical intervention may be necessary to correct these conditions.
Medicines
The drugs of choice for the treatment of lichen sclerosus are medications for topical application (ointments and creams) with corticosteroid hormones. When treating scleroatrophic changes in the genital organs, preference is usually given to ointments with clobetasol propionate; it is believed that they effectively suppress the inflammatory process and prevent the progression of the disease, and also help to avoid further scarring.
It is better to use ointments on mucous membranes, since they contain slightly fewer additives than creams and, accordingly, are less likely to provoke reactions of individual intolerance and irritation.
To achieve a therapeutic effect, it is usually recommended:
- Use the ointment exclusively on the spot for a month, twice a day. Subsequently, application is carried out once a day for another three months. Further, low-dose non-daily use is possible - maintenance therapy.
- Use the ointment sparingly, applying only to the affected areas, drying them thoroughly.
- Increase the frequency of application in accordance with the doctor’s recommendations (in particular, if symptoms increase after reducing the frequency of lubrication).
Long-term maintenance therapy is considered safer than the potential risk of relapse of the disease, which can cause scarring and atrophy.
In parallel with hormonal treatment, patients may also be advised to:
- Use creams with retinoids that have pronounced emollient properties.
- Use ointments or creams that accelerate regeneration processes. Solcoseryl, Bepanten, Actovegin, etc. give this effect.
- Take sedatives and antihistamines to relieve severe itching.
Sometimes doctors may decide to inject corticosteroids into the affected areas.
Non-drug therapy
Patients diagnosed with lichen sclerosus are strongly advised to:
- Prevent exposure of the skin and mucous membranes to all kinds of irritants. Do not use soap or sanitary pads with chemical additives (fragrances).
- Switch to loose clothing made from natural fabrics. It is important to avoid pressure on the affected areas from rough seams and tight wardrobe parts.
- Use emollient moisturizers that can increase the moisture content of the skin and minimize local inflammation.
- Refuse sexual activity until the condition stabilizes.
- Avoid scratching affected areas.
Non-pharmacological methods of intervention will help reduce negative symptoms and avoid complications. They will also contribute to a noticeable improvement in the quality of life.
Folk remedies
To date, there is no confirmed evidence that folk remedies can help in the treatment of lichen sclerosus. Nevertheless, there are recommendations online for the treatment of this disease using:
- Sitz baths with medicinal herbs. In particular, the use of string, calendula flowers, and chamomile is recommended. The selected raw material should be used in the amount of 1 tbsp. Brew it with 3 liters of boiling water and cover with a lid. After the infusion has cooled to a pleasant temperature, strain and use as intended. The duration of one procedure is up to half an hour. It is worth repeating such baths every day.
- A healing decoction from a collection of herbs. To create such a medicine, it is necessary to combine equal shares of nettle and strawberry leaves, as well as black currant, tricolor violet, crushed burdock roots, horsetail grass and string. 2 tbsp. l. Brew the resulting mixture with 0.5 liters of boiling water and simmer for 3-5 minutes. The finished medicine needs to be left to steep for about 30 minutes, then strain and drink half a glass 3 times a day. per day. The duration of therapy with this decoction is 3 months.
- Tincture of celandine. Fill a glass jar halfway with dried herbs and fill it to the top with vodka. Leave for 2 weeks. in a fairly warm and dark place, then strain. The resulting infusion should be diluted with vodka in a ratio of 1:2 and used to wipe the affected areas. Of course, such a remedy cannot be used on mucous membranes.
- To neutralize the unbearable itching, you can wash yourself with chamomile-colored decoctions or a string. But it is worth noting that such procedures have a drying effect, so after them you need to lubricate the skin with emollients.
The advisability of using folk remedies in each specific case of lichen sclerosus must be agreed with the attending physician. All medicinal herbs can cause reactions of individual intolerance and provoke other side effects.
Introduction
Lichen sclerosus (LS) is a chronic autoimmune dermatosis that occurs with focal skin atrophy and tissue damage in the anogenital area [1–3].
According to the general clinical classification developed by S. Peterson, LS is one of the clinical variants of limited plaque scleroderma (OS) [4]. A feature of the clinical course of LS is lesions of both the skin and tissues of the anogenital area, which can be isolated or combined [5]. Anogenital localization of LS occurs more often in women than in men, in a ratio of 3:1 [6, 7], in addition, dermatosis can develop at any age, but the peak incidence occurs in prepubertal age (9–11 years) and in menopause and /or postmenopausal period (45–55 years). In men, the disease usually develops after 40 years of age [6–8].
The issues of etiology and pathogenesis of LS have not been fully studied, however, it is known that the following important roles are played in the pathogenesis of the disease: genetic predisposition; inhibition of the activity of the pituitary-adrenal system; dysfunction of the thyroid and gonads; vaccination; injuries; acute and chronic infections (ixodid tick-borne borreliosis ( Borrelia burgdorferi
), scarlet fever, diphtheria, erysipelas, sexually transmitted infections (STIs)); human papillomavirus (HPV); herpes simplex virus (HSV); hepatitis B and C, etc., paraneoplastic genesis is also possible [9–14]. In recent decades, the development of LS of anogenital localization has been associated with the participation of estrogens and progesterone and their relationship with disturbances in the reaction of synthesis of collagen and connective tissue components [13, 14]. Literature data report that the free fraction of testosterone and androstenedione is significantly reduced in patients with genital LS, and abnormal activity of the 5α-reductase enzyme is also noted [14]. In a number of studies, the role of the leading factor is given to hypoestrogenism, since after the age of 30, the activity of steroidogenesis steadily decreases (by 1–3% per year) and by the age of 50 it decreases by almost 20% [14, 15]. The development of LS in the prepubertal period is in most cases associated with low estrogen levels and estrogen saturation of target organs [15]. However, with the development of LS in children, in rare cases, regression of pathological foci is possible, since the level of estradiol increases with age [15, 16]. A special role in the pathogenesis of LS is given to the pathological autoimmune process that develops in the walls of small vessels (capillaritis) and the interstitial substance of connective tissue, due to the high level of antigenic “collagen” stimulation [15–17].
A decrease in the activity of the hyaluronidase enzyme, the accumulation of mucopolysaccharides and progressive fibrinoid degeneration of connective tissue elements in combination with vasospasm due to the accumulation of serotonin lead to edematous-indurative changes [2, 10, 15]. The launch of a whole cascade of autoimmune, vascular and metabolic disorders leads to increased synthesis of collagen (types I, III, IV and VII) and other components of the extracellular matrix, obliteration of small vessels, which is clinically manifested by a progressive atrophic process of tissues [15–17].
In a number of cases, damage to the genital organs in LS can develop almost asymptomatically, especially at the onset of the disease [15]. The main complaints presented by patients with the steady progression of the process are soreness, paresthesia, tingling and “crawling” sensations, moderate itching, and then hardening of tissue in the genital area, hair loss and the appearance of cracks. As the disease progresses, along with increasing subjective sensations, patients develop a number of other qualitative symptoms. These include urinary syndrome, including persistent urinary tract infections, cystourethritis [16], gastrointestinal syndrome, manifested by pain during defecation, chronic constipation [17], and vulvovaginal syndrome, including dyspareunia and a whole range of dysfunctional sexual disorders [16, 17].
The typical clinical picture of LS consists of many small (3 to 5 mm in diameter), clearly contoured areas of atrophy that tend to merge. Elements of rashes can be scattered or grouped. Gradually, their number and size increase, they merge and form vast fields of thinned epidermis and atrophy, leading to partial tissue reduction. The color of the affected skin is whitish, with a pearlescent or liquid tint. The skin is difficult to fold, there is no hair on it, and apocrine and sweat glands are also absent [15–18]. The progression of scleroatrophic changes in the anogenital area in men, when localized on the skin of the penis and anus, leads to thinning of the foreskin, narrowing and stricture of the urethra. Paraphimosis and phimosis often develop [18, 19]. A serious complication of penile LS is squamous cell carcinoma, which accounts for up to 50% of cancer cases in the corresponding localization [19, 20]. In women, the progression of scleroatrophic changes in the anogenital area leads to loss of vulvar structure and its reduction. The vulva is easily injured and dyspareunia occurs. The folds of the labia are flattened and smoothed, the clitoris and labia minora are practically impossible to determine (like Hart’s line), due to severe tissue sclerosis, the entrance to the vagina narrows, the size of its vestibule and the external opening of the urethra decrease. Vulvar LS with chronic hyperkeratosis and erosions can be complicated by squamous cell carcinoma [19–21].
All these phenomena, in addition to unpleasant subjective sensations, cause patients significant moral suffering and significantly reduce the quality of life, since they are a serious cosmetic defect.
It is also important to note that patients with LS of anogenital localization are observed in obstetrics and gynecology clinics, where this disease is perceived only as an isolated lesion of the genitals, and not as a form of OS that requires a comprehensive examination and a systematic approach to treatment.
Purpose of the study:
to identify the frequency of damage to the anogenital area in the main clinical variants of OS, to establish differential diagnostic clinical criteria for damage to the anogenital area during OS, to improve the treatment method taking into account the anogenital localization and to evaluate the clinical effectiveness of the developed treatment method.
Drug treatment
As a rule, medication is the main treatment for the disease. Based on the results of histological examination, one of several ointments known to modern medicine is selected. This will definitely be a corticosteroid drug. You will have to use the ointment twice a day, the course duration is about three months.
If complete recovery has not occurred within a quarter of a year, a new histological examination is performed and the same drug continues to be used. A biopsy is required to rule out the presence of malignant cells in the affected area.
Medicines used locally are common, not least hormonal.
Possible complications
Even with proper treatment, lichen sclerosus can provoke unpleasant complications. And in the absence of timely correction, the risk of their development is especially high. In particular, the disease can cause:
- Decreased quality of life, especially sexual. Incorrect or inadequate treatment can lead to the development of irreversible structural changes that cause sexual dysfunction and greatly complicate relationships.
- Erectile dysfunction in men, as well as problems with proper urination.
- Attachment of secondary infection. The appearance of erosions, cracks and scratches contributes to the active proliferation of bacteria at the site of the lesion.
- Development of squamous cell carcinoma. Regardless of the location of lichen sclerosus and the speed of recovery from this disease, patients with this disease fall into the lifelong risk group for this cancer. Degeneration into cancer occurs infrequently - in approximately 3-5% of cases. The risk of malignancy in women is slightly higher than in men.
Fortunately, lichen sclerosus rarely causes complications in children. And adequate therapy and medical supervision reduces the risk of developing such unpleasant consequences to a minimum.
Establishing diagnosis
If primary symptoms appear, it is recommended to seek help from a specialized center (for example, the Institute of Dermatology and Cosmetology in Moscow). During the consultation, a specialist can confirm the diagnosis based on the patient’s complaints and studying the clinical manifestations of the disease. In some cases, a biopsy of the affected tissue may be additionally prescribed, followed by examination of the material under a microscope.
Why is it developing?
Lichen sclerosus is being studied by scientists from many countries. However, the clear causes of the pathogenesis have not yet been established. There are several recorded factors:
- Hereditary gene pool. A gene connection has been proven for manifestations in parents and children. The complexity of the problem depends on the genetic characteristics.
- Presence of autoimmune diseases. There is a connection between diseases such as vitiligo, diabetes mellitus and lichen sclerosus.
- Infections. Infections are assigned a significant role in influencing the development of the disease.
- Influence of local factor. The development of lichen sclerosus is quite rarely associated with injuries.
- Chronic nature of irritation of the foreskin by the urine of patients with diabetes mellitus.
- Hormonal imbalance. The function of the cells accepting male hormones is impaired.
Is it possible to cure Tsumbusha lichen?
Indeed, it is often possible to get rid of all manifestations of lichen sclerosus only in pediatric patients. In them, the disease can disappear on its own and without a trace, never recurring. In other cases, doctors do not give very favorable prognoses, because:
- The pathology has an unknown origin; it is impossible to predict the features of its development in the future.
- Despite the therapy, patients may still have atrophic areas of varying sizes on their body.
- There is always a risk of complications.
Patients with lichen sclerosus need to be observed at intervals of two to three months by a dermatologist-oncologist, urologist or gynecologist. This will help to promptly identify possible complications or prevent them.
Prevention
The factors that provoke lichen sclerosus have not been established, so preventive measures are of a general nature. For prevention purposes, it is recommended:
- carefully care for the affected areas;
- wear cotton underwear that does not cause pressure;
- regularly moisturize damaged areas;
- stop using pads;
- wash yourself without using strong intimate products.
Lichen sclerosis and atrophic are prone to progression, which leads to the appearance of cancer. Seeing a doctor in the early stages of the disease will help avoid negative consequences. Treatment gives positive dynamics, but examinations are recommended to be carried out during the period of remission - 2 times a year.
Research results
Patients with the clinical variant in the form of plaque scleroderma amounted to 78 people (75%), linear scleroderma - 1 person (0.9%), Pasini-Pierini atrophoderma - 2 people (1.9%), LS - 23 people (22.2 %).
Scleroatrophic lesions of anogenital localization were observed in 40 patients with plaque scleroderma (64.5%), in 21 patients with LS (33.8%), in 1 patient with linear scleroderma (1.7%).
LS of anogenital localization was observed more often in women - 82.9% (51 patients) than in men - 17.1% (11 patients). The main group of patients with lesions of the genital organs occurs in the age median from 41 to 50 and from 61 to 70 years, which corresponds to the period of pre- and postmenopause. Age and gender characteristics of patients with LS are given in Table 1.
When analyzing the clinical features of the prevalence of scleroatrophic lesions of the skin and mucous membrane of the genital organs, we found that in 32.3% of cases the scleroatrophic process was localized only in the anogenital zone, and in 67.7% of cases the process was combined.
Thus, according to our data, in 32.3% of cases (n=20) an isolated lesion of the anogenital localization was observed in the scleroatrophic variant of OS. When analyzing combined lesions of the skin and anogenital zone, in 46.7% of cases (n=29), we identified a combination of two forms of OS: the plaque form on the skin and LS of the anogenital zone. In 19.4% of cases (n=12), we identified combined lesions of the skin and anogenital zone. In 1.7% of cases (n=1), lesions of the LS type in the anogenital zone were combined with lesions of the linear scleroderma type on the skin of the trunk.
When conducting a detailed analysis of the localization features of scleroatrophic lesions of the anogenital zone in women (n=51), it was found that lesions of the vulva occurred in 41 cases (80.4%), lesions of the clitoris - in 36 (70.5%), lesions of the perineal tissue - in 38 (74.5%), lesions of the perianal area in 24 (47%) (Fig. 1, 2).
Analysis of the characteristics of scleroatrophic lesions in men (n=11) showed scleroatrophic lesions of the glans penis in 8 cases (72.7%), lesions of the frenulum tissue - in 6 (54.5%), lesions of the skin of the shaft of the penis - in 3 (27 .3%), damage to the perianal area - in 4 cases (36.4%) (Fig. 3).
When analyzing concomitant chronic pathology in the studied patients (n=62), we found that in 71% of cases (44 patients) STIs and pelvic inflammatory diseases were detected, in 86.4% of cases (in 38 women) and in 17.1% cases (in 6 men). In 33.9% (21 patients) of cases, the following were found: HPV of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) and HSV types I and II - in 16 women (25.8%) and 5 men (8.1%) (Table 2).
Scleroatrophic lesions of anogenital localization were combined with bacterial vaginosis - in 27.4% of cases (17 patients), chlamydia ( Chlamydia trachomatis
) - in 24.2% of cases (15 patients), trichomoniasis (
Trichomonas vaginalis
) - in 17.7% of cases (11 patients), gonorrhea (
Neisseria gonorrhoeae
) - in 3.2% of cases (2 patients).
Scleroatrophic lesions of anogenital localization were combined with chronic persistent viral infection: HSV type II - in 16.1% of cases (11 patients), HSV type I - in 6.4% of cases (3 patients) (see Table 2).
It is also important to note that the presence of chronic persistent viral infection with HPV with a high oncogenic potential (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) in patients with scleroatrophic lesions of the genital organs causes significant interest due to the high risks of developing malignant transformation (see Table 2).
We analyzed concomitant chronic pathology in a group of patients (n=62) with lesions of anogenital localization. Of great interest are diseases of the pelvic organs, which were identified in 40.3% of cases (n=25): uterine fibroids - in 12 women, salpingoophoritis - in 5 women, salpingitis - in 3 women, cystitis - in 2 women; Prostatitis was detected in 2 men, prostate adenoma - in 1.
In addition, chronic focal infection of various localization was detected in 27.4% of cases (n=17): in women - rhinitis in 5, chronic tonsillitis - in 3, chronic pharyngitis - in 3; in men: rhinitis - in 3, chronic tonsillitis - in 2, chronic pharyngitis - in 1. Diseases of the cardiovascular system were detected in 19.4% of cases (n=12): in women - arterial hypertension in 7, arrhythmia in 1; in men - arterial hypertension in 3, heart failure - in 1. Pathology of the gastrointestinal tract and hepatobiliary system occurred in 3.2% of cases (n=2): in women - gastritis in 1, dyskinesia of the gallbladder - in 1. Pathology not detected in 9.7% of cases (n=6).
The effectiveness of the course of therapy was assessed by the positive dynamics of the skin process: a decrease in the density of lesions, the disappearance or blanching of the corolla of hyperemia, the absence of growth of old lesions and the appearance of new ones, a decrease in the size of old lesions, and a decrease in subjective sensations.
After the first course of complex therapy there was a break of 1.5–2.0 months, after which the next course of complex therapy was carried out. In the absence and/or insignificance of changes after a course of therapy, patients were prescribed a second course (the maximum number of courses did not exceed 5).
Thus, out of 62 patients with OS and damage to the anogenital zone, the majority of patients - 56.5% (35 people) required 3 courses of complex therapy, 16.1% (10 people) - 4 courses, 11.3% (7 people) - 2 courses, 6.4% (4 people) - 1 course and 8.1% (5 people) - 5 courses to completely stabilize the process.
Against the background of complex therapy, a decrease in the density of lesions was observed in 48 (77.4%) patients, blanching of the corolla of hyperemia - in 28 (45.1%) patients. The absence of growth of old lesions and the appearance of new ones was noted in 62 (100%) patients, a decrease in the size of lesions was observed in 39 (72.6%) patients (Table 3).
Analysis of the dynamics of subjective sensations showed a positive trend towards their decrease. Thus, before treatment, itching of the anogenital area occurred in 77.4% of cases, after complex treatment - in 24.2% of cases. Painful sensations in the lesions were observed in 59.7% of cases before treatment, and in 17.7% after treatment. Paresthesia before treatment was observed in 75.8% of cases, after treatment - only in 19.4% of cases. A feeling of tightness and dryness before treatment was observed in 80.6% of cases, after treatment - in 37.1%. Sleep disturbances were detected in 77.4% of cases before treatment, and in only 8.1% after treatment. Sexual dysfunction occurred in 51.6% of cases before treatment, and in 22.6% of cases after treatment (Table 4).
All patients (n=62) were asked to assess the degree of negative impact of the skin disease on various aspects of their life (family relationships with relatives, friends, work colleagues, sports, sex, social activity, etc.). quality of life index (QOL) before and after treatment. After a complex course of treatment, a significant increase in DIGI was noted in all patients with scleroatrophic lesions of the anogenital area (Table 5).
What treatments are there for lichen sclerosus?
The extent of treatment depends on the extent of the spread of the LS process.
It is important to note that circumcision (circular excision of the foreskin in LS has its own characteristics. The main task of circumcision in LS is the complete excision of the affected tissue. However, too much of the foreskin should not be removed, as it may be needed in the future for plastic surgery reconstruction of narrowings (strictures) of the urethra (primarily the scaphoid fossa), which can be caused by LS. The following figures show the stages of treatment of LS of the penis stage I-II (the appearance before surgery is shown in Fig. 3).
Rice. 5. Circumcision for LS using the double-incision technique. The skin incision is marked in such a way as to excise the affected part of the foreskin of the penis, which is clearly visible.
Rice. 6. Condition of the penis after surgery. The affected skin is excised, but it is sufficient for possible subsequent reconstructive operations.