What is hypoglycemia?
Glucose is considered one of the main sources of energy in the body. When its content in the blood is low, a life-threatening condition develops - hypoglycemia. Most often, its manifestations are experienced by people suffering from type 1 diabetes, but it can also appear in type 2 of the disease. In some cases, this condition may signal other diseases and health problems.
The concentration of glucose in the blood during hypoglycemia is up to 3.3 mmol/l. At such moments, brain cells begin to lack sugar and, in the absence of the necessary measures to replenish its reserves, may die.
Lack of glucose negatively affects the functions of neurons, which leads to impaired coordination of movement, loss of the ability to think clearly and independently control one’s own actions.
With such symptoms, it is important to begin treatment immediately. Otherwise, a hypoglycemic coma may develop, which can even lead to death.
Hypoglycemia: When should you see a doctor?
On the other hand, for milder, low-sugar forms, simple measures that patients or their relatives can do on their own are often sufficient. These include drinking sweetened tea or taking a small dose of glucose.
In contrast, severe hypoglycemia is a potentially life-threatening condition that should always be treated by a doctor. Because if it goes further, low sugar will eventually lead to what is called hypoglycemic shock. Victims then lose consciousness and may fall into a coma. Therefore, you should always call an ambulance if you suspect you have hyperglycemia.
Reasons for the development of a hypoglycemic state
People with diabetes must adhere to all the rules of behavior within the framework of their disease, namely:
- follow a diet, nutrition regimen;
- take synthetic drugs appropriate for the type of diabetes or inject insulin subcutaneously;
- control sugar.
Ignoring these recommendations may result in dangerous consequences for the patient, including hypoglycemia.
Factors provoking a hypoglycemic state:
- Excess insulin in the body. Most often this occurs in patients with insulin-dependent diabetes when the wrong dose of the drug is administered.
- Long intervals between snacks, or lack of meals necessary for the body due to the nature of work or being in public places. In this case, a person may either unintentionally ignore the first signs of hypoglycemia or be embarrassed to have a snack in the environment, making a serious mistake.
- Consumption of alcoholic beverages. After drinking strong drinks, glucose levels may drop sharply after some time if drinking is not accompanied by a snack that includes a sufficient amount of carbohydrates.
- Physical activity was not taken into account. Any workout is accompanied by increased consumption of glucose by muscle tissue, so the lack of snacks before or after exercise leads to a drop in sugar levels.
- Taking certain medications that can impair sensitivity to hypoglycemia.
- The presence of severe diabetic polyneuropathy, as a result of which nerve cells are affected and sensitivity to hypoglycemia is lost. A person has to check his sugar more often with a glucometer to avoid a sharp drop.
- Insufficient drinking regime. In this case, the body begins to intensively use up glucose reserves, causing a decrease in its level in the blood.
Hypoglycemia in diabetes mellitus
Most often, this condition occurs if a person has insulin-dependent diabetes. Hypoglycemia develops when a patient injects himself with a larger dose of insulin than is required to process the glucose present in the blood. After all, diabetics do not have large glycogen reserves; they are forced to control the level of carbohydrates entering the body. With this disease, you need to follow a strict diet, calculating how much glucose you need to consume (it is calculated in XE - bread units) depending on physical activity. But errors are possible in the initial stages of the disease, as well as in case of violation of the daily routine or diet. In diabetes, an attack of hypoglycemia is caused by the following reasons:
- incorrect insulin dosage;
- consumption of alcoholic beverages;
- prolonged fasting, often even skipping one meal leads to a decrease in glucose levels;
- great physical activity;
- low level of carbohydrates in food;
- the use of drugs that enhance the effect of insulin, for example, Aspirin, Warfarin, Glinase and others.
In addition to a pathological decrease in glucose levels, symptomatic hypoglycemia occurs in diabetes mellitus. The patient feels all the signs of pathology when sugar drops sharply from high to normal levels. To avoid problems, people with diabetes need to follow a strict diet, follow all doctor's recommendations and check their blood for sugar several times a day.
Classification and symptoms of the disease
The hypoglycemic state is classified into types based on clinical manifestations, severity, mechanism of development and origin.
Main forms of hypoglycemia:
- Transient (neonatal). This condition often accompanies newborns and is explained by the lack of glucogenesis while in the womb. Infants born prematurely, with developmental defects, or born to mothers with diabetes are more susceptible to neonatal hypoglycemia.
- Reactive . It occurs in obese people when large amounts of insulin are produced in response to excessive carbohydrate consumption.
- Alcoholic . Occurs in people who abuse alcohol and have insufficient nutrition.
- Night . Hypoglycemia appears during sleep from 2 to 4 hours, when the body least needs insulin. The cause of its development is considered to be an overdose of the hormone administered subcutaneously at night.
- Nutritional . It appears after surgery on the gastrointestinal tract (gastrointestinal tract) due to impaired absorption of glucose in the blood.
From the moment of the first manifestations until loss of consciousness, a person experiences 3 degrees of hypoglycemia, each of which is accompanied by characteristic symptoms.
Table of symptoms and degrees of hypoglycemia:
| Degree | Common reasons | Symptoms |
| Lightweight | The occurrence of this stage of hypoglycemia is most often provoked by various stresses, fear or very serious experiences | The patient at this stage may feel weakness, anxiety and restlessness for reasons unknown to him, a slight feeling of hunger, tachycardia, an attack of nausea or dizziness |
| Average | Lack of a snack or scheduled main meal | A person develops cold sweat, weakness, trembling in the knees and hands, headaches, and ringing in the ears. The patient's consciousness begins to gradually become cloudy. Speech disturbances, loss of control over one’s actions, and pale skin become noticeable to people around. |
| Heavy | Ignoring symptoms characteristic of a moderate degree of the syndrome, as well as refusing to eat carbohydrates | The person loses control over the situation and faints. He may experience convulsions, which indicates the onset of a coma. The patient's body temperature decreases and glucose levels drop below 2.2 mmol/l |
With uncompensated diabetes mellitus, patients are often in a state of hyperglycemia, when the blood sugar level consistently exceeds acceptable values (more than 10 mmol/l). Bringing the indicator back to normal can cause symptoms of “false” hypoglycemia in these people.
In this case, the body takes the glucose level usual for healthy people, which is within 5 mmol/l, as a critically low value. The patient begins to consume carbohydrates and thereby again provokes an increase in glycemia.
It is important for people with diabetes to be able to distinguish the symptoms of real hypoglycemia from false manifestations and control their sugar levels to avoid dangerous health consequences due to sudden drops and spikes in glucose.
Blood Sugar Level
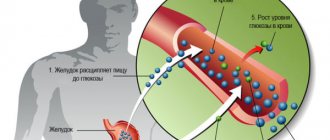
The vital functions of the body are maintained through metabolic processes. This is a metabolism that ensures that all necessary microelements and energy enter the cells, as well as the removal of cell waste products. For the functioning of the brain and all organs, glucose is primarily needed. It is supplied to the body only with food. But not only sugars are a source of glucose. It is also produced from any carbohydrates. They are all processed at different rates.
In order for glucose to be absorbed by cells, insulin is a special hormone. As soon as sugar enters the blood from the gastrointestinal tract, this substance begins to be intensively produced by the pancreas. Insulin helps cells use incoming sugar, converting it into energy. In healthy people, it is produced exactly as much as is needed to absorb the glucose received from food. In addition, there are reserves of glucose in the body in the form of glycogen, which is located in the liver. And excess carbohydrates are also stored in fat.
Therefore, it is very important to maintain normal blood glucose levels at all times. Increasing it can lead to obesity or diabetes, and with low sugar levels hypoglycemia develops. Insulin processes glucose from the blood, so this condition often occurs when diabetics take the wrong dosage of the drug. But it can also develop in healthy people with an unbalanced diet.
First aid
First aid to eliminate the symptoms of hypoglycemia includes 2 stages:
- Carbohydrate intake.
- Control glycemia until its values normalize.
It is possible to relieve the symptoms of hypoglycemia at home only in the first two stages of its manifestation. To do this, it is enough to consume a few bread units (XE).
Each bread unit contains 12 g of carbohydrates. When glycemia is less than 3.5 mmol/l, it is best to drink sweet juice or tea. Chocolate or cake are not suitable in this case, as they contain fat, which is digested more slowly.
After a quarter of an hour, you should measure your sugar using a glucometer. If the glucose level is below 3.9 mmol/l, then you need to consume another 1.5 XE, measuring the sugar after 15 minutes.
If there is no increase in the indicator, the snack should be repeated with a mandatory check of the blood glucose level. You should alternate snacks with control sugar measurements until the value obtained on the glucometer exceeds 3.9 mmol/l.
If a person is no longer able to consume carbohydrates on his own and is unconscious, then you need to lay him on his side and call an ambulance. Giving drink or food to people in this condition is dangerous as they may suffocate. Before the medical team arrives, the patient’s relatives can inject him with a subcutaneous glucagon solution, which is sold in a special kit in pharmacies. This will help save lives.
Hypoglycemia: symptoms, causes, treatment methods
Image from lori.ru
Hypoglycemia is a condition in which the blood glucose level drops below the limit of 3.3 mmoll. This is the level below which disturbances in the normal functioning of organs and tissues occur, since glucose is the main nutrient for cells. Hypolycemia can occur suddenly or gradually.
Causes of hypoglycemia
The main causes of hypoglycemia are identified - these are, first of all, diabetes and its incorrect correction, an overdose of insulin against the background of limited food intake, prolonged fasting while taking long-acting insulin, stress, heavy physical activity or mental work. Drinking alcohol with metabolic problems can lead to a special glycemia, it is called alcoholic (hangover syndrome in the morning). Hypoglycemia, so-called transient or reactive, can also occur in ordinary people during fasting, dieting, or taking medications.
Hypoglycemia in children is highlighted separately. It usually occurs at the birth of a baby from a mother with diabetes due to a sharp activation of the baby's pancreas in utero. In newborns, immediately after birth, insulin transfers glucose into the cells, and due to nutritional deficiency, severe hypoglycemia can quickly occur. Hypoglycemic syndrome is distinguished separately against the background of a hormone-producing tumor - insulinoma.
Hypoglycemia can occur while taking antihyperglycemic drugs for type 2 diabetes mellitus. Often manifestations of hypoglycemia force the patient to consult a doctor.
Development mechanism
Insulin is synthesized by special islets of the pancreas. In type 1 diabetes, there is no or very little insulin, so it requires external administration. In type 2 diabetes, there is insulin, but it is defective or does not work, then it is necessary to introduce special drugs that will reduce blood glucose. Most cells need insulin in order to absorb glucose; they feed on it. But not all cells metabolize glucose with insulin (for example, the brain and muscles “eat” glucose without it). During stress, heavy workload or mental work, glucose is actively consumed by those cells that do not need insulin, and the insulin you injected becomes too much for the rest of the glucose. To maintain the brain and muscles in working condition, there must always be a certain amount of glucose in the blood, at least 3.3 mmol; below this threshold, symptoms of hypoglycemia begin. With a sharp decrease in glucose below 2.7 mmoll, consciousness can be impaired; with figures of 2.3-2.5 mmoll, death can occur.
Symptoms
The main symptoms of hypoglycemia appear gradually or abruptly, it all depends on the rate of decrease in blood glucose. Characteristic signs of hypoglycemia are:
- severe hunger;
- severe weakness;
- heavy sweating and sticky cold sweat;
- trembling in the arms and legs;
- tachycardia;
- severe headache;
- vision problems with blurry objects, spots, and double vision;
- dizziness;
- irritability and agitation, aggression;
- numbness in the lips and tongue.
Not all symptoms necessarily appear at once; only a few of them may be present.
It is more difficult to recognize hypoglycemia in children, especially newborns and toddlers. The following signs indicate hypoglycemia:
- mother had diabetes before or during pregnancy;
- the child is excited or sharply inhibited;
- he has tremor of the limbs (trembling);
- he is very pale, cold and sweaty;
- he has a sharp tachycardia and increased breathing;
- he experiences a disturbance of consciousness.
People who have had diabetes for a long time may not feel the onset of hypoglycemia. Then the first symptoms of hypoglycemia can be noted by others - this is inappropriate behavior similar to intoxication, strange behavior, aggression, and excessive sweating. In this case, movements are poorly coordinated, speech is impaired.
If first aid is not provided in a timely manner, then the attack can turn into a state of hypoglycemic coma in literally 20-30 minutes. The patient loses consciousness, experiences severe muscle hypotension, pallor, the skin becomes moist, and there may be convulsions. Sharp fluctuations in blood glucose levels cause negative consequences in the form of damage to blood vessels in tissues and the brain, which adversely affects the course of diabetes.
Treatment
All treatment of hypoglycemia can be divided into emergency at the time of the attack and prophylactic, preventing its onset.
At the first signs of hypoglycemia, you need to eat any product rich in light carbohydrates - sugar, candy, jam, honey, wash it down with warm tea, which will enhance the absorption of carbohydrates. If it is difficult for the patient to do this, it is necessary for someone to help. It is important that you have a strict diet with regular meals and a set amount of carbohydrates. In the treatment of diabetes, short-acting insulin is used (it is injected before meals) and long-acting insulin (it is injected in the morning or during the day with the expectation of a long-term effect). It is important that the peak breakdown of complex carbohydrates occurs during the action of long-acting insulin, and the absorption of fast carbohydrates during short-acting insulin. In order to prevent hypoglycemia, nutrition for diabetes should be regular and fractional, counting bread units.
If a person loses consciousness, you should not give him sugar or sweet tea, you must lay him on his side, put a piece of solid sugar on his cheek and immediately call an ambulance. Doctors will immediately administer intravenous glucose to him and continue administering it in the hospital together with insulin.
Prevention
In order to prevent and immediately eliminate hypoglycemia, it is necessary to stop drinking alcohol and accurately calculate the dose of insulin and glucose-lowering drugs with your doctor, and not skip meals, especially after insulin injections.
You should always carry a sugar cube or glucose tablets in your pocket. At the first sign of hypoglycemia, you need to eat them. Always carry information about yourself and that you have diabetes in your clothing pocket. This will help you get the right help.
Author: Alena Paretskaya, pediatrician
Treatment in a hospital setting
Emergency care for a patient who is unconscious or in a coma consists of drug therapy in a hospital setting according to the following scheme:
- A glucose solution (40%) in a volume of 40-60 ml is administered intravenously together with the drug Glucagon. If the glucose level still remains below normal, then connect an IV with a 5% solution of the same drug until the patient regains consciousness.
- An injection of Adrenaline is used to restore breathing and heartbeat.
- To prevent cerebral edema, a Magnesia injection is performed.
- When a deep coma occurs, the patient is given 150 mg of hydrocortisone intramuscularly.
If a person does not return to consciousness 4 hours after the measures taken, this indicates a high chance of cerebral edema, which can lead not only to disability, but also death.
Hypoglycemia - description, causes, symptoms (signs), diagnosis, treatment.
Short description
Hypoglycemia is a decrease in blood glucose levels less than 3.33 mmol/l. Hypoglycemia can occur in healthy individuals after several days of fasting or several hours after a glucose load, resulting in increased insulin levels and decreased glucose levels in the absence of symptoms of hypoglycemia. Clinically, hypoglycemia manifests itself when glucose levels decrease below 2.4–3.0 mmol/l. The key to diagnosis is Whipple's triad: • nervous - mental manifestations during fasting; • blood glucose less than 2.78 mmol/l; • relief of an attack by oral or intravenous administration of r-radextrose. The extreme manifestation of hypoglycemia is hypoglycemic coma.
Causes
Risk factors • Insulin therapy • Long-term experience of diabetes (more than 5 years) • Old age • Kidney disease • Liver disease • Cardiovascular failure • Hypothyroidism • Gastroenteritis • Fasting • Alcoholism.
Genetic aspects. Hypoglycemia is a leading symptom of a number of hereditary enzymopathies, for example: • Hypoglycemia due to glucagon deficiency (231530, r) - congenital hypoglycemia with high insulin levels and glucagon deficiency • Hypoglycemia with liver glycogen synthetase deficiency (#240600, r). Clinically: congenital hypoglycemia, hypoglycemia and hyperketonemia during fasting, hyperglycemia and hyperlactatemia during feeding, convulsive syndrome. Laboratory: glycogen synthetase deficiency • Fructose - 1,6 - phosphatase deficiency (229700, r) • Leucine - induced hypoglycemia (240800, r) - several types of congenital hypoglycemia • Hypoketotic hypoglycemia (#255120, carnitine palmitoyl transferase I deficiency [*600528, 11q, CPT1 gene defect], r).
Etiology and pathogenesis
• Fasting hypoglycemia •• Insulinoma •• Artificial hypoglycemia is caused by the use of insulin or taking oral hypoglycemic drugs (less commonly caused by taking salicylates, beta-blockers or quinine) •• Extrapancreatic tumors can cause hypoglycemia. These are usually large, abdominal tumors, most often of mesenchymal origin (eg, fibrosarcoma), although liver carcinomas and other tumors have been observed. The mechanism of hypoglycemia is poorly understood; report intensive uptake of glucose by some tumors with the formation of insulin-like substances •• Ethanol-induced hypoglycemia - in individuals with a significant reduction in glycogen stores due to alcoholism, usually 12-24 hours after binge drinking. Mortality is more than 10%, so rapid diagnosis and administration of p-radextrose are necessary (with the oxidation of ethanol to acetaldehyde and acetate, NADP accumulates and the availability of NAD, necessary for gluconeogenesis, decreases). Impairment of glycogenolysis and gluconeogenesis, necessary for the formation of glucose in the liver during fasting, leads to hypoglycemia •• Liver disease leads to deterioration of glycogenolysis and gluconeogenesis sufficient to cause fasting hypoglycemia. Similar conditions are observed in fulminant viral hepatitis or acute toxic liver damage, but not in less severe cases of cirrhosis or hepatitis •• Other causes of fasting hypoglycemia: deficiency of cortisol and/or growth hormone (for example, in adrenal insufficiency or hypopituitarism). Renal and heart failure are sometimes accompanied by hypoglycemia, but the causes of its occurrence are poorly understood.
• Reactive hypoglycemia occurs several hours after consuming carbohydrates •• Nutritional hypoglycemia occurs in patients after gastrectomy or other surgical intervention, leading to an abnormally rapid flow of food into the small intestine. Rapid absorption of carbohydrates stimulates excess insulin secretion, causing hypoglycemia some time after eating •• Reactive hypoglycemia in diabetes. In some cases, patients in the early stages of diabetes experience a later but excessive release of insulin. After eating, the plasma glucose concentration increases after 2 hours, but then decreases to the level of hypoglycemia (3–5 hours after eating) •• Functional hypoglycemia is diagnosed in patients with neuropsychiatric disorders (for example, chronic fatigue syndrome).
Symptoms (signs)
The clinical picture is determined by a feeling of hunger in combination with neurological and adrenergic symptoms.
• Neurological symptoms predominate as glucose levels gradually decrease •• Dizziness •• Headache •• Confusion •• Visual disturbances (eg, diplopia) •• Paresthesia •• Seizures •• Hypoglycemic coma (often develops suddenly).
• Adrenergic symptoms predominate with an acute decrease in glucose levels •• Hyperhidrosis •• Anxiety •• Tremor of the limbs •• Tachycardia and a feeling of interruptions in the heart •• Increased blood pressure •• Attacks of angina.
Age characteristics • Children: transient hypoglycemia of the neonatal period, hypoglycemia of younger and older children • Elderly: in most cases, hypoglycemia is associated with concomitant diseases or the use of hypoglycemic drugs.
Pregnancy often causes transient hypoglycemia.
Diagnostics
Laboratory studies • Determination of plasma glucose levels and glucose tolerance testing • Determination of C-peptide allows identifying the source of insulin secretion •• Low glucose and high insulin levels, pathognomonic for insulinoma, are accompanied by increased levels of C-peptide • Low levels of C peptide indicates an exogenous source of high insulin concentration • Liver function tests, determination of serum insulin, cortisol.
The influence of drugs. Sulfonylurea stimulates the production of endogenous insulin and C-peptide, therefore, to exclude artificial hypoglycemia, a blood or urine test is performed for sulfonylurea drugs.
Special studies • Plasma glucose after a 72-hour fast is less than 45 mg% (less than 2.5 mmol/l) in women and less than 55 mg% (3.05 mmol/l) in men • Test with tolbutamide: with intravenous administration, glucose level after 20–30 minutes it decreases by less than 50% • Radioimmune determination of insulin levels • CT or ultrasound of the abdominal cavity to exclude a tumor.
Differential diagnosis. Psychogenic hypoglycemia, or pseudohypoglycemia. Many patients (most often women aged 20–45 years) are diagnosed with reactive hypoglycemia, but such a complex of symptoms is usually associated with severe fatigue or autonomic-vascular dysfunction (stress also plays a significant role in the genesis of these symptoms). Such patients are difficult to treat. A consultation with a psychotherapist is advisable.
Treatment
Management tactics • Diet high in protein (in patients with dumping syndrome - low in digestible carbohydrates). Frequent and small meals • When the first signs of hypoglycemia occur - oral intake of easily digestible carbohydrates (2-3 tablespoons of sugar in a glass of water or fruit juice, 1-2 cups of milk, cookies, crackers) • If the patient cannot eat, glucagon is administered intramuscularly or subcutaneously (in our country glucagon is rarely used) • In case of hypoglycemia caused by drugs, avoid taking it or carefully monitor the dose of the drug • Avoid significant physical activity and stress.
Drugs of choice
• Emergency medical care •• If it is impossible to take glucose orally, administer 40-60 ml of 40% r-radextrose intravenously over 3-5 minutes, followed by a continuous infusion of 5 or 10% r-radextrose •• For neurological symptoms in children treatment begins with an infusion of 10% r-radextrose at a rate of 3-5 mg/kg/min or higher •• For hypoglycemia caused by oral hypoglycemic drugs (for example, sulfonylureas), continued dextrose infusion and observation of the patient for 24 –48 hours due to the likelihood of coma relapse.
• It is possible to administer intramuscular or subcutaneous glucagon to the patient in the upper third of the shoulder or thigh (rarely used in our country). Glucagon usually reverses the neurological manifestations of hypoglycemia within 10–25 minutes; If there is no effect, repeated injections are not recommended. Doses of glucagon: children under 5 years old - 0.25-0.50 mg, children from 5 to 10 years old - 0.5-1 mg, children over 10 years old and adults - 1 mg.
Complications • Brain edema • Persistent neurological impairment.
ICD-10 • E15 Non-diabetic hypoglycemic coma • E16 Other disorders of pancreatic endocrine system • P70 Transient disorders of carbohydrate metabolism specific to the fetus and newborn • T38.3 Poisoning with insulin and oral hypoglycemic [antidiabetic] drugs
Notes • Attaching undue importance (overinterpretation) to a glucose tolerance test may lead to overdiagnosis of hypoglycemia. It must be remembered that in more than 1/3 of healthy people, symptomatic or asymptomatic hypoglycemia is observed within 4 hours after this test • b - Adrenergic blockers mask the symptoms of hypoglycemia.
Consequences for the body
Frequent attacks of hypoglycemia negatively affect the functioning of all internal organs.
Main consequences:
- development of vascular angiopathy;
- the risk of heart pathologies increases;
- brain function is disrupted;
- stroke and cerebral edema may develop;
- the patient's diabetic complications progress;
- coma sets in.
Prolonged coma causes brain cells to die and can lead to death.
Prevention of low sugar
In healthy people, hypoglycemia develops only under extreme conditions. To avoid this, it is necessary to dose physical activity, avoid long periods of fasting, and eat right. It is very important that your diet contains as few fast carbohydrates as possible, but you should definitely eat cereals, whole grain bread, legumes, vegetables and fruits every day. If you experience frequent attacks of hypoglycemia, you should always have a chocolate bar, juice or cookies with you. But you shouldn’t get carried away with this; it’s better to undergo an examination and find out the causes of this condition.
It is especially important to follow all doctor’s recommendations for patients with diabetes. Hypoglycemia can be prevented by following several rules:
- do not exceed the insulin dosage;
- measure your sugar level several times a day;
- avoid periods of prolonged fasting;
- do not drink alcohol;
- maintain a diet;
- Take any medications only after consulting your doctor.
Hypoglycemia is a condition that is often ignored by healthy people. But not only patients with diabetes, but also every person should know about its signs and possible consequences.
How to prevent a dangerous condition?
You can reduce the risk of a pathological condition using preventive measures, including the following recommendations:
- know methods for relieving this condition and eliminating its symptoms;
- be able to select the dosage of insulin in accordance with the amount of XE planned for administration;
- do not exceed the dose of the administered hormone;
- monitor your diet and follow the injection schedule;
- do not skip main meals, as well as planned snacks;
- monitor morning glycemia, as well as changes in glucose levels after each meal using a glucometer;
- do not drink alcoholic beverages;
- always have lumps of sugar, glucose tablets or simple carbohydrates with you to stop hypoglycemia at the first manifestations;
- be sure to read the instructions for the medications you take to know how their components affect your glucose level;
- Have extra snacks before starting physical work or sports.
Why does blood sugar drop sharply:
A timely snack at the first signs of hypoglycemia will help prevent the onset of a severe form of its manifestation, when carbohydrate intake is no longer possible.
It is difficult to help a person who is fainting, especially if the people around him do not know about his illness. It is important to understand that avoiding the onset of hypoglycemia is much easier than eliminating its symptoms.
Chronic hyperglycemia
As the disease progresses, in which hyperglycemia plays a leading role, beta cells lose their function and are destroyed, the pulse pattern of insulin release is disrupted, and this further increases glycemia.
As a result of these pathological changes, complications quickly develop. The following are involved in the appearance of diabetic angiopathy:
- Oxidative stress.
- Non-enzymatic glycation of proteins.
- Autoxidation of glucose.
The main function in the mechanisms of occurrence of these processes is assumed by hyperglycemia. It has been proven that even before high fasting hyperglycemia is diagnosed, 75% of beta cells lose their function. Fortunately, this process is reversible.
Scientists have found that the beta cells of the pancreas are in a dynamic state, that is, they are regularly renewed and the mass of beta cells adapts to the body’s needs for the hormone insulin.
But with persistent chronic hyperglycemia, the ability of surviving beta cells to adequately respond with insulin to acute stimulation with glucose is greatly reduced. The absence of this response to a glucose load is fraught with disruption of phases 1 and 2 of insulin secretion. At the same time, chronic hyperglycemia potentiates the effect of amino acids on beta cells.
Stages of the disease
Medicine considers four stages of hypoglycemia, including coma.
First degree, mild
Decreased performance, lethargy, hand tremors. Determined by the patient himself, it is relieved by taking easily digestible sugars - candy, cookies, sweet tea.
Preschool children cannot assess their condition themselves; adult supervision is required.
Mild hypoglycemia causes them to become lethargic and want to eat “something sweet,” after which the child’s activity is restored.
Second degree, moderate
The patient can observe his condition, communicate with others and turn to them for help, but he can no longer provide help to himself - the state is semi-fainting.
Possible irritability, tremors, sticky cold sweat. Moves with the help of others, but can drink sweet drinks and eat foods with fast carbohydrates.
It may be necessary to use insulin-lowering drugs. It is recommended to consult a specialist.
Third degree, severe
We recommend you find out: Why is hyperandrogenism syndrome dangerous in women?
The patient is on the verge of a coma, consciousness is confused or absent, convulsions, low temperature with hypoglycemia are a common occurrence.
Medical intervention is necessary and urgent therapy is required to prevent hypoglycemic coma.
Fourth degree, coma
The patient is unconscious, there may be a lack of breathing, muscle hypertonicity, and a near-death state. Risk of cardiac and brain arrest, urgent medical attention required!
Hypoglycemic coma develops rapidly within minutes, less often hours. Be sure to call qualified doctors and take the patient to a medical facility.
Symptoms of hypoglycemic syndrome
Depending on how hypoglycemic syndrome manifests itself in a person’s condition, its symptoms are divided into two groups.
Read: Why is liver fluke dangerous for humans?
We advise you to find out the signs of giardiasis in adults.
Neuroglycemic
In this case, the body’s reaction is due to the fact that the nervous system is deprived of its only source of “feeding” - glucose. She reacts to forced starvation with real rebellion:
- headache, increased fatigue, drowsiness during the day and insomnia at night;
- deterioration in vision clarity;
- depression, irritability, attention deficit;
- inappropriate behavior - causeless anxiety, incoherent speech, lack of interest in others and even hallucinations.
Vegetative
These manifestations of hypoglycemic syndrome are due to the fact that a lack of glucose provokes the body’s release of a group of hormones - catecholamines. Symptoms are characteristic of a situation when the sympathoadrenal system is in an excited state:
- the skin turns pale and suddenly breaks out in sweat;
- the heart beats at an increased frequency;
- tingling sensation in fingertips and lips;
- hands tremble slightly, muscle weakness overcomes, knees give way;
- I really want to eat.
Typical clinical picture
The above symptoms do not necessarily appear simultaneously during hypoglycemic syndrome. It all depends on the degree of hypoglycemia, the conditions of its development and the presence of adaptation of the body.
Most often, the signs of excitation of the sympathoadrenal system are the first to appear on the scene; they can be considered harbingers of an acute attack. However, if glucose deficiency develops slowly, the syndrome may immediately manifest itself in neurological signs.
Important: the most characteristic symptom of acute glucose deficiency is considered to be a depressed state of the cerebral cortex with increasing signs - from simple drowsiness to loss of consciousness (coma) through intermediate states.
What can cause hypoglycemic syndrome?
First of all, hypoglycemic syndrome is dangerous at the stage when a person can no longer help himself on his own. The severity of hypoglycemia in this case is considered to be high, regardless of whether the attack is accompanied by loss of consciousness or not. The development of events will depend on the situation: whether anyone will be nearby, and how quickly those around them will be able to determine the cause of the illness.
Protracted long-term hypoglycemic syndrome threatens with serious disorders of the central nervous system without hope of improvement. In young patients they manifest themselves in a decrease in intellectual abilities, in adults – in personality defects (altered consciousness). This pathological condition is also dangerous for elderly people with a history of heart, vascular and brain diseases. During attacks, they may develop a stroke, heart attack or encephalopathy.
Find out how to take Fitogastrol.
We advise you to find out what a liver fibroscan is.
Read: what to do if you feel a lump in the esophagus.
Treatment of glycemia
Glycemia requires drug treatment. It is prescribed by a doctor on a case-by-case basis based on the patient’s sugar level, age and weight, as well as a number of other factors. However, treatment may be ineffective if a person does not change his habits and adjust his lifestyle.
A special place in the treatment of glycemia is given to diet. Every patient with high glucose levels in the body should consume carbohydrates with a low glycemic index.
For both hyperglycemia and hypoglycemia, meals should be taken in small portions 5-6 times a day. The diet should mainly consist of proteins and complex carbons. It is these products that can fill the body with energy for a long time.
When treating glycemia, people should not forget about moderate physical activity. This could be cycling, running or walking.
Glycemia may not manifest itself for a long time, but if it is detected, it is necessary to immediately begin its treatment.
Diagnostics
Detection of hypoglycemic syndrome is carried out according to the scheme given below.
Severe neuropsychiatric disorders often lead to patients being misdiagnosed. This is observed in 75% of patients with insulinoma who are mistakenly treated for epilepsy, vegetative-vascular dystonia, and neurasthenia.
Patients with hypoglycemic syndrome, as well as patients with diabetes, require regular self-monitoring using glucometers.
Etiology
- dehydration;
- poor nutrition with abuse of refined carbohydrates, with a pronounced deficiency of fiber, vitamins, and mineral salts;
- treatment of diabetes mellitus with insulin, oral hypoglycemic drugs in case of overdose;
- insufficient or late meals;
- unusual physical activity;
- illness;
- menstruation in women;
- alcohol abuse;
- critical organ failure: renal, hepatic or cardiac, sepsis, exhaustion;
- hormonal deficiency: cortisol, growth hormone or both, glucagon + adrenaline;
- not a p-cell tumor;
- tumor (insulinoma) or congenital anomalies - 5-cell hypersecretion, autoimmune hypoglycemia, 7-ectopic insulin secretion;
- hypoglycemia in newborns and children;
- intravenous administration of saline by dropper.
Signs
Symptoms of hypoglycemic syndrome are:
- painful feeling of hunger;
- abdominal pain, nausea, vomiting;
- general weakness;
- trembling in the limbs;
- sweating;
- feeling of heat, redness or paleness of the face;
- palpitations, tachycardia, drop in blood pressure.
The following symptoms are noted from the central nervous system:
- dizziness;
- drowsiness;
- burning sensation, crawling;
- headache;
- darkening of the eyes;
- visual impairment (double objects);
- mental retardation;
- convulsions;
- amnesia;
- loss of consciousness, coma.
The degree of manifestation of these signs can vary - from mild, in which the attack lasts several minutes and the patient’s general condition is satisfactory, to severe, when patients completely lose their ability to work. For those people who have insulinoma, the only complaint may be frequent sudden loss of consciousness between meals, at night, or after exercise.