Home » Tuberculosis » Types »
The closed form of tuberculosis is a serious infectious disease caused by rod-shaped bacteria. Its main difference from the open form of the disease is that the infection can remain in the human body for a long time and not cause acute reactions. Infection does not always mean illness. At least nine out of ten patients do not develop symptoms or physical signs of active disease. They are not contagious, but they can get sick later and then spread TB to others.
Closed tuberculosis is an insidious disease, this is primarily due to the fact that it can persist in the body and wait for favorable conditions to transform into an open form. A decrease in the immune system is the favorable conditions under which the infection begins to intensify. An infected person may not even be aware of the presence of this disease. How dangerous is it and is closed tuberculosis dangerous for others?
Open form of tuberculosis
Active tuberculosis is a condition in which the body's immune system is unable to fight tuberculosis bacteria, so bacteria are released into the external or internal environment. Microorganisms spread through the air and usually affect the lungs, although they can involve other organs and parts of the body in the pathological process.
If the body's resistance is low, for example due to aging, malnutrition, infections such as HIV, or other reasons, the bacteria become active and cause overt tuberculosis.
The World Health Organization estimates that every year, 8 million people worldwide develop active disease and nearly two of them die. One in ten people infected with pathogens may develop open tuberculosis. The risk of development is greatest in the first year after infection, but the form often develops many years later.
It is impossible to immediately infect an open form of the disease, since it is necessary to go through its first phase. When TB germs enter the body, they are inactive.
Dormant germs do not damage the body or cause symptoms of illness. This is called latent TB infection.
It may last for a short time or many years. When microbes become active, begin to grow and damage the body, then specific signs of pathology appear. This is called active or open tuberculosis.
www.tuberculosis.emedtv.com
www.health.state.mn.us
Routes of infection with tuberculosis
Infection with tuberculosis occurs from carriers of the disease in an open form. The causative agent of the disease is a bacterium called Koch's bacillus. Here's how closed-form tuberculosis is transmitted:
- Airborne route of infection. The pathogen is concentrated in the exhaled air, and is also actively released with microdrops of saliva when the patient coughs, sneezes, or laughs. A healthy person inhales air with bacteria in it and becomes infected. This is the most common cause of the disease;
- Nutritional path. Bacteria enter the body through the digestive tract. This happens when patients fail to comply with hygiene rules and use shared utensils;
- Contact path. This is quite a rare occurrence. Bacteria are not transmitted sexually even with complications such as tuberculosis of the reproductive system. The medical literature describes cases of infection of young children through the conjunctiva from adult carriers of the infection. Unlikely, although infection through skin contact is theoretically expected;
- Intrauterine path. Tuberculosis is transmitted from a mother infected with Koch bacilli in two ways:
- when the placenta is infected;
- during the period of gestation;
- when the fetus is infected;
- when passing through the birth canal. Cases of intrauterine infection have been described, but are considered extremely rare.
Popular Signs of manifestation of the early and first stages of tuberculosis
The closed form of infection is almost always asymptomatic at first. But in the absence of proper treatment, the form may change to open.
Currently, there are two most significant problems in the prevention of tuberculosis:
- The first is due to the fact that patients with different forms of tuberculosis are not admitted separately. This leads to the fact that generally accepted safety measures are effective for patients with a closed type, but practically do not work for people with an open type. Both healthy people and patients with a closed form suffer from this. The health status of the latter may worsen due to additional infection;
- The second consists of a high influx of labor migrants into the country from states where the level of medical care is low. Vaccinations of the population against tuberculosis are carried out haphazardly, and diagnostic tests for the disease are not mandatory. Migrant workers can be infected with tuberculosis and other dangerous diseases and not even know it. Once in a team, such an employee is capable of infecting others with various infectious diseases within a short time, and this form of tuberculosis is no exception.
Main symptoms of pathology
Manifestations of active tuberculosis depend on the individual characteristics of the organism.
The open form of tuberculosis can cause symptoms such as:
- a productive cough that lasts 3 weeks or longer;
- chest pain;
- secretion of sputum mixed with blood.
Nonspecific signs may include:
- weakness or fatigue;
- weight loss;
- anorexia;
- chills;
- fever;
- night sweats.
These possible symptoms of tuberculosis are not reliable signs of the disease. Other health problems can also cause these signs. Anyone with possible symptoms of the disease should consult a doctor as soon as possible so that the problem can be diagnosed and treated in a timely manner.
www.tuberculosis.emedtv.com
Other factors causing the disease
The awakening of mycobacteria is facilitated by weakened immunity, which occurs for reasons such as:
- Prolonged stress;
- Poor nutrition;
- Chronic long-term lack of sleep;
- Alcohol abuse;
- Smoking;
- Concomitant chronic or acute diseases;
- Lack of ventilation and penetration of direct sunlight in the place where the sick and healthy are located.
The following categories of people are at risk:
- Patients suffering from diabetes, stomach or duodenal ulcers.
- Patients taking glucocorticoid drugs. Hormonal drugs suppress the immune system, which contributes to the development of tuberculosis upon contact with the patient.
- Patients infected with the human immunodeficiency virus.
- Social group of people. This category includes people suffering from alcoholism, taking drugs, serving time in prison, refugees, etc.
- Group of people in contact with tuberculosis patients: medical staff, social workers, relatives of patients.
- Patients with reduced immunity as a result of other diseases or as a result of treatment.
- Persons who have once had pulmonary or extrapulmonary tuberculosis.
Children and pensioners are also at risk, to whom the disease is transmitted especially easily. This is explained by the fact that their body, the lung area and the endocrine system have not fully formed, and therefore they are weakened and cannot fully resist viral and tuberculosis lesions. In addition, closed tuberculosis is transmitted more quickly in stuffy rooms. The first symptoms of tuberculosis in children are described here.
Under unfavorable circumstances, mycobacteria are activated. From this moment, the closed form of tuberculosis becomes open, and the infection can be easily transmitted even with short-term contact.
Despite the fact that tuberculosis in its closed form is not contagious, it is important to understand that this disease can develop into an open form without any symptoms. Symptoms of open tuberculosis will begin to appear only after some time, when the patient still does not know that he poses a threat to others.
Thus, there are often no signs at an early stage, so it is quite difficult to determine it, which in most cases becomes the reason for untimely treatment of the disease.
In 80% of cases, the primary stage of tuberculosis development, taking a closed form and not showing any symptoms, is transmitted genetically. For most of them, the closed variety of tuberculosis remains in its infancy throughout their entire life. A huge role in this process is given to timely diagnosis and early treatment.
Risk of infection - how you can become infected with a pathology
How can you become infected with open tuberculosis? Anyone can contract a dangerous disorder. When someone with pulmonary tuberculosis coughs, sneezes or talks, germs can be sprayed into the air. People nearby may inhale the agents. It is impossible to contract the disease from a handshake or from food, dishes, bedding and other items. People with weak immune systems are more susceptible to infection.
How can you become infected:
- abusing alcohol or drugs;
- having diabetes;
- with silicosis;
- having head or neck cancer;
- if you have leukemia or Hodgkin's disease;
- when diagnosing severe kidney disease;
- having low body weight;
- during certain types of treatment (eg, corticosteroids or organ transplantation);
- during specialized therapy for rheumatoid arthritis or Crohn's disease.
If pathogens are in the lungs, you must be careful to protect other people from germs, as the risk of infection increases severalfold with open TB. Ask your doctor or nurse, they will tell you what you need to do to prevent the transmission of germs to loved ones and how you can become infected yourself.
www.tuberculosis.emedtv.com
www.health.state.mn.us
What you need to know about the disease
Focal pulmonary tuberculosis
Pulmonary tuberculosis is a dangerous infectious disease, which in pulmonology is included in a separate group of pathologies of the respiratory system. The causative agent is a microscopic mycobacterium called Koch's bacillus, in honor of the scientist who first described it.
The peculiarity of this pathogen is that its cell has the characteristics of bacteria and microscopic fungi and can infect not only the lungs, but also other organs, and also infect various animals.
The human body can be infected by two types of pathogenic microorganisms that cause tuberculosis - the aforementioned Koch bacillus and the bovine tuberculosis bacterium. All other strains are not dangerous for a healthy person, and invasions can only occur with critically low immunity, for example, HIV patients are at risk.
The fight against a dangerous disease is complicated by the fact that pathogenic microorganisms have high eco-plasticity, and therefore easily adapt to changing conditions. In addition, their genome is rearranged quite quickly, which allows the bacteria to develop stable resistance to the drugs used, which makes it quite difficult for the doctor to select drug treatment.
Note. Tuberculosis pathogens have an increased survival rate in unfavorable conditions. For example, when treated with various antiseptics containing chlorine, Koch's bacillus can remain viable for up to five hours.
Ultraviolet radiation is lethal for microorganisms of this series. But the greatest efficiency is achieved only from artificial sources.
Direct sunlight can destroy pathogenic strains only if exposed continuously for 1.5 hours. If bacteria are in a favorable environment without exposure to harmful factors, then they remain viable for 5–7 years outside a living host organism.
The high degree of resistance is explained by the ability of bacteria to form cysts in unsuitable conditions for life and reproduction - special formations that help them remain viable for a long period of time. In this case, microorganisms are in a state of suspended animation, i.e. in their cells all processes stop until favorable conditions occur. And as soon as the microorganism enters the animal body, it wakes up, grows and begins to actively reproduce.
How long do people live with this disease?
Pathology does not always lead to death. Without treatment, life expectancy can range from 5 to 30 years; how long people live with open tuberculosis depends on many external and internal factors.
First of all, the immune resistance of the body is influenced, as well as age and the presence of concomitant diseases.
You can expect to keep your job, stay with your family, and lead a normal life if you get TB. However, you should take the medicine regularly to ensure positive results and prevent infection of other people.
After therapy, the chance of complete recovery is very high, but not 100% guaranteed. There are particularly severe forms of the disorder that are practically resistant to most antibacterial drugs.
Therefore, the importance of following the prescribed exposure regimen cannot be underestimated. Without treatment, the disease will progress and can lead to disability and even death.
Smoking more than 20 cigarettes a day creates a poor prognosis for life and a high risk. This increases the chance of pathology and dangerous complications by two to four times. Diabetes also worsens the prognosis of the disease.
Other painful conditions that reduce the chances of recovery:
- alcoholism;
- end stage kidney disease;
- malnutrition;
- Hodgkin's lymphoma;
- chronic lung diseases.
www.emedicinehealth.com
www.news-medical.net
How are extrapulmonary forms of the disease transmitted?
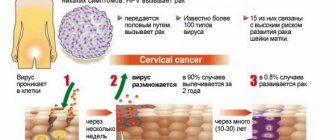
Tuberculosis can affect not only the human lungs; other organs are also susceptible to the penetration of bacteria and the spread of infection. The disease can develop:
- In the intestines. Characterized by significant disturbances in the functioning of the digestive organs. The intestinal walls, where the pathogen enters with food, are highly susceptible to infection. The complexity of the diagnosis lies in the similarity of the symptoms of gastrointestinal tuberculosis with other pathologies, such as intestinal infection, duodenal ulcer.
- In bones and joints. This is a common form of tuberculosis that affects the bones of the thighs, legs, and in some cases the vertebrae. Treatment of such a disease is complex and long-term, with constant examination of surrounding areas and organs. This is due to the fact that often the disease in hard tissues is formed from a closed form of infection of the lungs. It’s easy to find out how bone tuberculosis is transmitted, but protecting yourself from it is a difficult task.
- In the genitourinary system. The destructive effects of Koch bacilli are often experienced by the kidneys, ureters and bladder. Untimely treatment will lead to deformation of organs, which can lead to serious complications. The disease spreads through the genitourinary system in all possible ways.
- In the lymph nodes. The disease also affects the biological filter system. Many people ask doctors - what is lymph node tuberculosis, how is this disease transmitted? Professionals note that it is possible to fall victim to this particular disease by any of the above types of infection. At the first stage, tuberculosis of the lymph nodes is not contagious, but in the future it develops into a full-fledged open form and destroys the immune system.
In addition to the organs described above, tuberculosis less often affects the testicles, uterus, prostate gland, nerve endings, meninges, and skin. All these forms of the disease are dangerous to health, so doctors, if there is any suspicion, advise you to urgently visit a medical facility for diagnosis and a comprehensive examination of the body. Delayed treatment in most cases leads to death.
Open and closed form - comparison
People with latent infection do not get sick or have any symptoms. They are infected with the mycobacterium M. tuberculosis (Koch's bacillus), but do not show signs of disease.
The only confirmation is a positive reaction to a tuberculin skin test or a blood test for tuberculosis. Persons with the latent form are not contagious to others.
Overall, without treatment, 5-10% of infected people develop the full-blown form of the disease at some point in their lives. For half of them, this will happen within the first two years after infection.
In people whose immune systems are weak, especially in HIV-infected people, the risk of developing an active form of the disease is much higher than in patients with normal body defenses.
In a person with latent tuberculosis infection:
- usually a skin test or blood test result indicates an infection;
- normal chest x-ray and negative sputum test;
- tuberculosis bacteria in the body are alive but inactive;
- no symptoms;
- microorganisms do not spread to others.
In some people, bacteria overcome the defenses of the immune system and begin to multiply, which leads to progression from a closed to an open form of pathology. Some people get sick soon after infection, while others get sick later when their body's response becomes weaker.
People are considered infectious to the surrounding community. If suspected, patients should be referred for a full medical examination.
Open tuberculosis is a very serious disease and can lead to death if left untreated. The closed form is always dangerous because a person cannot start drug therapy in a timely manner.
In an infected person with open form:
- a positive skin test or blood test result indicating infection;
- an abnormal chest x-ray or positive sputum smear and culture;
- there are active tuberculosis bacteria in the body;
- multiple symptoms appear, such as cough for 3 weeks or longer, coughing up blood, chest pain, unexplained loss of weight and appetite, night sweats, fever, fatigue and chills;
- spread of bacteria to others may occur;
- treatment is mandatory.
www.cdc.gov
Treatment of closed tuberculosis
Is it possible to cure closed tuberculosis? Treatment of the closed form of tuberculosis is based primarily on the use of medications. TB drugs are taken regularly and usually for 6-12 months. The prescribed medications are combined and used in strict accordance with the doctor’s recommendations. Due to the fact that this form of the disease is not active, treatment is carried out without isolating the patient.
For a detailed answer to the question, we recommend reading the article: Is pulmonary tuberculosis completely curable or not? on our website.
The way to prevent the disease is vaccination, which is currently performed on newborns immediately after birth. Also among the main methods of prevention, early detection of the disease and implementation of immediate treatment are considered effective. Improving living conditions, namely sanitary conditions. It is necessary to get rid of alcohol and drug abuse, as well as smoking cigarettes.
First signs of illness
Manifestations of tuberculosis usually develop slowly, over several months and years, and are often masked by other conditions. Bacteria reproduce very slowly, so symptoms of the disease also appear slowly, usually from several months to many years. Many symptoms are vague and may have other causes.
Classic manifestations of active tuberculosis are:
- malaise;
- night sweats;
- generalized body pain;
- periodic fever;
- weight loss and appetite;
- fatigue.
Among the specific symptoms, the first signs of an open form of tuberculosis are a persistent cough, which in the morning may be with yellow or green sputum. Over time, traces of blood appear, although a large amount of it is unusual.
Cough is often thought to be related to smoking, asthma or a recent illness, but tuberculosis is often forgotten. The pathology causes increased night sweats, with the person waking up drenched in sweat.
As the disease progresses, fatigue and malaise increase, and weight loss and loss of appetite progress. Other common early symptoms are chest pain and shortness of breath. They may result from the formation of pleural effusion, a buildup of fluid between the thin membranes that line the lungs and the inside of the chest wall.
www.everydayhealth.com
How to determine the presence of a disease
The symptoms of tuberculosis are varied, which sometimes complicates the diagnostic search. Lethargy, apathy, loss of appetite and body weight, persistent low-grade fever (37-38), decreased performance, irritability are signs of the onset of the disease.
People infected with tuberculosis may complain of increased sweating, especially in the head and chest area. But a person usually associates such general symptoms with emotional stress or increased physical activity, which can delay a trip to a TB doctor.
The cough comes with the height of the disease. In the initial stage, sputum production is usually not observed.
The amount of exudate increases as bacteria increasingly disseminate into the lung tissue. In the uncomplicated form, the sputum is usually colorless, impurity-free and odorless. Further progression of inflammation causes increased coughing and the appearance of large amounts of sputum.
Dyspnea most often accompanies acute and chronic disseminated, fibrous-cavernous and cirrhotic tuberculosis. Severe lung damage leads to a decrease in the area of tissue contact with oxygen, due to which the body experiences hypoxia.
The impact of pathogenic bacterial toxins on the respiratory center in the medulla oblongata also plays a significant role in the development of shortness of breath. Hemoptysis is more often observed in infiltrative, cirrhotic and fibrous-cavernous pulmonary tuberculosis.
https://youtu.be/N-DwZnCQBLI
The focal form of the disease is usually asymptomatic with moderate fever and malaise.
Sometimes the clinical picture of respiratory tuberculosis is similar to the course of pneumonia and ARVI.
Treatment with antibiotics may slightly improve the patient's condition.
Extrapulmonary forms are accompanied by both general and local symptoms, depending on the location of the pathogen.
With intestinal tuberculosis – stool disturbance, bleeding; with bone – pain in the spine or joints; with tuberculous brain damage - dizziness, headache; with tuberculosis of the ovaries and uterus - infertility, irregular menstruation. When the male genital organs are infected, the epididymis and testicle are first affected, then the prostate is involved in the process. Ulcers appear on the genitals, which open over time, bringing improvement to the patient’s well-being.
Against the background of tuberculosis, severe complications can develop, for example, generalized sepsis, pulmonary hemorrhage, cardiac and respiratory failure, which can result in death.
Tuberculosis and incubation period
The microbacterium Mycobacterium tuberculosis has an incredibly low infectious dose - less than 10 microorganisms to initiate disease. The bacteria have a long incubation period, ranging from two to twelve weeks with a range from fourteen days to several decades.
They have the ability to both hide and initiate an active form of the disease. Mycobacteria inhaled by the host infect the lungs and are ingested by alveolar macrophages. After this, they can remain inactive for a long time or begin to multiply inside these cells, which causes an open infection.
The duration of tuberculosis incubation varies depending on individual risk factors.
According to the data, within six weeks of infection, an infected person develops a primary infection in the lungs, which does not cause any symptoms.
The disorder then enters an inactive phase, which can last from several weeks to several years. The incubation period can be protracted. Therefore, everyone who comes into contact with a potentially infected person has a risk of becoming infected.
www.microbewiki.kenyon.edu
www.healthyliving.azcentral.com
Kinds
With tuberculosis, the patient's status changes depending on the stage of development of the disease and the effectiveness of treatment. It can be open or closed.
In the open form, a sick person releases mycobacteria into the environment. The open form is characteristic of pulmonary tuberculosis, when microbes are released during coughing and expectoration of sputum. It is also called BC+. This means that during a microscopic examination of a sputum smear, the bacteria that cause tuberculosis were detected.
The closed form of tuberculosis is diagnosed much more often. It is designated as BK-. This means that the patient does not release Koch bacilli into the air. The disease destroys cells quite slowly, while remaining almost motionless. The infection constantly changes from active to inactive and back, so it is difficult to treat the closed form of tuberculosis.
Tuberculosis can be primary and secondary. With primary tuberculosis, which usually occurs in childhood, symptoms do not appear for several days or even weeks.
Secondary tuberculosis is a more common form of lung disease. It occurs due to the fact that in old lesions there is still an infection. When favorable conditions are created for pathogens, they become activated and aggravate the disease. Secondary tuberculosis can develop at any age.
Treatment of secondary tuberculosis should be long-term. This is the only way to prevent serious irreversible damage occurring in the lungs.
Secondary tuberculosis has several form-stages:
- Focal pulmonary tuberculosis.
- Infiltrative.
- Tuberculoma.
- Caseous pneumonia.
- Cavernous.
- Cirrhotic.
Other types of tuberculosis:
- Tuberculosis of intrathoracic lymph nodes. This is one of the most common forms of primary tuberculosis. When the lymph nodes enlarge, the tracheobronchial tree is compressed and local changes develop.
- Disseminated pulmonary tuberculosis. It occurs rarely. Typically, disseminated tuberculosis occurs in acute or subacute forms. The disease develops due to extensive hematogenous spread of tuberculosis infection.
- Tuberculosis of the genitourinary system. This disease is the most common type of extrapulmonary tuberculosis. In this case, kidney damage occurs.
- Tuberculosis of joints, bones. It develops mainly in children in the first three years after infection, and in most cases the middle parts of the spine are affected.
- Tuberculous meningitis. This form is rare and has a poor prognosis. Without qualified treatment, tuberculous meningitis can result in death.
- Miliary tuberculosis. In this form of the disease, the pathogen spreads through the blood. Because of this, small lesions called granulomas form in different organs and tissues.
Forecast
With timely detection and treatment, the prognosis for the disease is quite favorable. Foci of infection gradually fade, decrease in size and are replaced by connective tissue. Metatuberculous changes are formed in these areas, which nevertheless do not make themselves felt.
It is important to remember that a closed type of infection is a disease that turns into an open form. With such an unfavorable course of the disease, the patient develops various serious complications, including death.
Often, almost everyone around him becomes infected with tuberculosis. That is why you should immediately respond to any alarming symptoms and strictly follow the recommendations of TB specialists.
Danger level
As already mentioned, the closed type of the disease does not pose a danger to healthy people. Those people who are extremely concerned about the question of whether it is possible to become infected with tuberculosis from patients with a closed form of the disease should know that such patients are not dangerous, since the Koch bacillus is not excreted. It is impossible to become infected with tuberculosis from them, and that is why such people are not even admitted to dispensaries. Their treatment is carried out on an outpatient basis, under the supervision of a TB doctor.
However, a disease that develops into an open form is already dangerous. The sputum and other secretions of patients will infect others, primarily immunocompromised individuals and children. An experienced specialist will help prevent the transition from one form to another, and, if necessary, he will refer the patient to the hospital.
Causes
For closed tuberculosis to develop, there must be predisposing factors that weaken the immune system. These include:
- smoking;
- failure to maintain personal hygiene;
- alcohol abuse;
- living in areas with unfavorable environmental conditions;
- frequent illnesses;
- other situations that can worsen immunity.
As a result of a decrease in local resistance forces, mycobacteria reach the lung tissue and remain dormant for an indefinite period of time, causing no harm. Often the infection remains inactive for the rest of life.
Complications of pneumonia in the absence of treatment
Active prevention of tuberculosis in developed countries is carried out at the state level. In Russia (with the consent of the parents), in the first few days after birth, every child in the maternity hospital is vaccinated with the BCG vaccine. It contains a weakened strain of bovine tubercle bacilli that does not cause infection but is active enough to trigger an immune response.
Active prevention also includes the following measures:
- For children - annual Mantoux test;
- For adults - fluorography at least once every 2 years.
Passive preventive measures are those aimed at strengthening the immune system. The main ones are:
- Taking multivitamins;
- Proper nutrition;
- Healthy lifestyle;
- Sports activities;
- Hardening;
- Frequent ventilation of enclosed spaces.
If pulmonary tuberculosis is not treated, it will undoubtedly lead to death sooner or later. Untimely treatment of the disease can lead to the following complications:
- Spread of the disease to other organs. Tuberculosis spreads to other vital organs, affecting them. If, for example, it is the liver, then its diseases lead to serious consequences for the body;
- Joint damage. With the development of skeletal tuberculosis, severe joint pain, swelling, and abscess formation begin;
- Pulmonary hemorrhage. It opens when a vessel in the lungs is destroyed as a result of advanced tuberculosis. Often the bleeding cannot be stopped and this ends in the death of the patient;
- Respiratory failure. With extensive damage to the lungs, the efficiency of their work is greatly reduced. This leads to oxygen starvation and attacks of suffocation;
- Heart failure. Appears along with respiratory failure;
- Pneumotrax. When an alveoli or bronchiole ruptures, the air that accumulates in the pleural cavity begins to compress the lung, which leads to attacks of suffocation.
Methods of therapy
Early diagnosis of tuberculosis guarantees the effectiveness of treatment. And although the closed type of tuberculosis infection is a non-transmissible disease and does not provoke serious pathological changes in the respiratory organs, it is necessary to undergo a therapeutic course. In very rare cases, such a patient is treated in a hospital, but usually such measures are unnecessary. As a rule, the patient takes a course of medications at home. However, any therapeutic measures should be carried out under the supervision of a specialist. Only he can identify the degree of infection and prescribe adequate treatment. Self-medication in this case can be fatal.
Medication
Koch's bacillus can be neutralized through long-term use of anti-tuberculosis antibiotics. In the case of a closed type of infection, there is no active development of it, so first-line anti-inflammatory drugs are used:
- Isoniazid,
- Ethambutol,
- Rifampicin,
- Pyrazinamide,
- Streptomycin.
The decision as to whether the patient can take one drug or whether they should be taken in combination is made only by the attending physician. Often at least 3 medications are prescribed, as bacteria may be resistant to certain medications.
The duration of the therapeutic course will depend entirely on how affected the body is by the infection. Most often it lasts from six months to a year, but visible relief is observed after 4 months. Radical measures, for example, surgery, are not used for closed forms of tuberculosis.
In addition to antibiotics, the doctor may prescribe immune-strengthening drugs, vitamin complexes, physiotherapeutic procedures and breathing exercises. The patient’s diet is also scrupulously reviewed and a special diet No. 11 is often prescribed. It is quite possible to include alternative medicine.
Traditional methods
If the attending physician does not object, then the main therapy can be supplemented with treatment with traditional medicine. An infusion of birch buds is often used. To prepare such a remedy, you need to pour 2 glasses of vodka over birch buds collected according to all the rules. Next, the product is allowed to brew until the liquid acquires the color of cognac. After this, the infusion is filtered and taken 1 tbsp. l. three times a day before meals.
Definition of the disease, how it manifests itself - symptoms and first signs in adults
Tuberculosis has been known since ancient times.
Hippocrates and Aristotle also warned about the increased contagiousness of this disease. Even some ancient Egyptian mummies have bones affected by tuberculosis. Tuberculosis is an infectious-inflammatory disease caused by mycobacteria of the M. tuberculosis group, called Koch bacilli (named after the scientist who discovered them, Robert Koch). Among all cases of diagnosed tuberculosis, only 10% are the open form of the disease. In most patients, tuberculosis occurs in a closed form, which is less dangerous, but also requires treatment with antibiotics under the constant supervision of a phthisiatrician.
Infection with Koch's bacillus occurs as follows: mycobacteria that enter the body spread throughout the body. Individual or multiple tubercles appear in the patient’s lungs. These are the foci of infection.
Stages of development
The tuberculosis bacillus, located inside the tubercle, does not escape beyond its boundaries. In this case, the lesion gradually begins to heal, but a seal appears on the tissue. This is the first stage of the disease. If the infection enters the patient’s blood, then multiple lesions are already formed. In this case, we talk about the second stage of the disease. Whether focal tuberculosis is contagious or not is described in this material.
At any stage of the closed form, the infected patient does not release mycobacteria into the outside world. The infection inside a person is as if in a closed jar, the walls of which do not allow it to get out.
The following features are characteristic of patients with the closed form of tuberculosis:
- The patient does not feel unwell;
- A special diagnostic test (tuberculin test) shows a positive result;
- A chest x-ray does not show any problems in the lungs;
- Sputum test for tuberculosis is negative;
- Bacteria living in the body are not active;
- In rare cases, infected people experience a persistent feeling of weakness and pain when breathing.
Pathogens
As already mentioned, tuberculosis goes through several stages in its development. The first of these is infection. This stage begins from the moment the first Koch bacillus is transmitted from a carrier to a healthy person, and lasts until the body’s immune response is formed.
Having settled on internal organs, Koch's bacillus creates an inflammatory focus, which is covered with protective connective tissue - a fibrous capsule. The formations tend to grow and, if left untreated, affect large areas of organs, causing their collapse. In this case, bacteria are spread beyond the affected area; they can be found in all physiological secretions of the patient - saliva, sputum, urine, feces, etc. This form of tuberculosis is called open.
Tuberculosis is an infectious disease caused by fairly common microorganisms - mycobacteria (Koch bacilli). Caused mainly by human and bovine bacteria. Before the twentieth century, it was better known among people as phthisis (to waste away). Since there were no effective medicines for this disease, people who fell ill with it gradually withered away and faded away.
Only in the twentieth century did they find ways to fight the disease. But still, the mortality rate among the population is quite high, especially if they seek help too late. It cannot be said that only vulnerable sections of the population get sick. In prosperous families, one of the household members may also develop this disease.
Mycobacteria differ from all other organisms harmful to humans in that they are very resistant to various external factors: acids and alkalis. They easily survive treatment with alcohol and do not die when exposed to direct sunlight. They are contagious for a long time in sputum, on objects, in dust.
Another negative feature that is difficult to combat is that they mimic and adapt to tuberculostatic drugs. And this can persist for quite a long time. Clinical manifestations are determined not only through the pathogen. The state of a person’s immunity and its resistance play a very important role.
However, a decrease in the body's resistance can occur under unfavorable living or working conditions. A person has managed to adapt to mycobacteria and his body successfully resists their harmful effects, but over time, immunity may weaken, so in this case revaccination will be required.
Tuberculosis most often affects the lungs, and in order to protect yourself from the development of the disease in the body and stop it at the earliest stages, you should know at least partial signs of the disease:
- Fatigue. A person feels overwhelmed even after a small amount of work.
- Irritability.
- The temperature is slightly increased, as if there was inflammation.
- Sleep is disturbed and appetite disappears.
- Sweating most often at night.
- Enlarged cervical lymph nodes (but not in all cases).
Does everyone infected with tuberculosis get sick?
The widespread distribution of Mycobacterium tuberculosis in the environment creates conditions for infection of a large number of people. But infection is not a disease. The human immune system is designed to attack viruses and bacteria, and good immunity suppresses the activity of tubercle bacilli. Mycobacteria simply live in the human body, waiting for an opportunity to attack.
The insidiousness of the Koch stick lies in its ability to develop resistance to drugs, after which it is extremely difficult to destroy it.
Any factor that leads to a weakening of the immune system’s defenses triggers the mechanism for the proliferation of mycobacteria, namely:
- Chronic stress;
- chronic diseases;
- metabolic diseases;
- oncological diseases;
- immunodeficiency syndrome;
- drug addiction and alcoholism.
Is treatment possible?
Nowadays, the closed form is successfully treated. Like many diseases, recovery depends on how early the patient sees a doctor. Treatment lasts a long time and must be supervised by a phthisiatrician. The prescribed medications will initially relieve general symptoms quite quickly, but complete recovery will not occur. The patient can stop taking medications only with the permission of the attending physician.
The key to success is a combination of several measures. Treatment is not limited to medication. The doctor prescribes, in addition to the course of pills, physiotherapeutic procedures and breathing exercises. It is better to take a course in a specialized sanatorium.
Under no circumstances should you engage in self-medication or treatment with traditional methods. In extreme cases, folk remedies can only act as an addition to real treatment.
Along with medical procedures, the patient is prescribed to lead a healthy lifestyle: no alcohol and nicotine. Good nutrition also promotes recovery. The patient's diet must include meat and fish dishes, vegetables and fruits.
Modern methods of prevention (vaccination and drugs)
In order to prevent the Russian Federation, children are vaccinated with the anti-tuberculosis vaccine (BCG), but this is possible only with the informed consent of the parents. Until the age of 18, all children undergo the Mantoux test annually; after reaching this age, it is no longer performed. In adults, prevention comes down to early diagnosis of the disease and its timely treatment. To detect the disease, a fluorography method is used, which every person must undergo once a year.
To prevent the disease at home, you should regularly ventilate and hang blankets, pillows and cotton products in the sun, as sunlight neutralizes Koch's bacillus within an hour. It is also important to systematically ventilate living spaces and combat dampness, since this is an ideal environment for the proliferation of Koch bacilli.
You should have a chest exam every year. Adults should undergo fluorography, children a Mantoux test. Prevention of tuberculosis in children is vaccination. It is carried out on the third to seventh day of the baby’s life with the BCG vaccine. The baby is vaccinated provided that he is absolutely healthy and there are no contraindications.
Diagnostics
Metamorphoses in the lungs caused by tuberculosis are detected through mandatory annual radiography. The condition of the lungs can be better studied using CT and MRI. Another diagnostic method is to analyze sputum for the presence of the pathogen in it. The person will also be asked to donate blood to determine the level of white blood cells and hemoglobin.
MRI is a method for diagnosing the closed form of tuberculosis
It has already been mentioned that for people with a closed form of the disease, such methods are not informative and it is better for them to resort to a tuberculin skin test. The most common of them is the Mantoux test. Monitoring the reaction to the introduction of a small amount of weakened bacteria is systematically carried out in all children's institutions, which helps to timely diagnose the presence of Koch's bacillus in the body.
Effective treatment of the disease
It is important to promptly begin treatment for people with a closed form of the disease who are in the following groups.
Persons with a positive test for the expression of gamma interferon, or with a Mantoux reaction of more than 5 mm:
- HIV-infected patients;
- upon contact with a confirmed patient;
- in the presence of fibrous changes on the radiograph associated with old cases of tuberculosis;
- organ transplant recipients;
- with reduced immunity (for example, when taking 15 mg of prednisolone per day for a month, or TNF antagonists).
Persons with a positive test for the expression of gamma interferon, or with a Mantoux reaction of more than 10 mm:
- immigrants who arrived less than 5 years ago from countries with high incidence rates;
- patients taking medications by injection;
- workers in places with a high risk of infection (correctional institutions, nursing homes, homeless shelters, hospitals and other healthcare structures).
- bacteriological laboratory workers;
- children under 4 years of age, or all minors in contact with adults from high-risk groups.
Closed tuberculosis is treated only after active infection has been ruled out. If there is doubt about the presence of an open form of the disease, the doctor prescribes several medications until results appear confirming or excluding the disease.
This regimen is considered highly effective for patients with HIV infection taking antiretroviral drugs, as well as children from 2 to 11 years of age.
The combined use of Isoniazid and Rifampicin for 12 weeks is an effective regimen for healthy patients over 12 years of age who are at high risk of developing the disease, namely:
- persons who have recently been in contact with a sick person;
- when a positive result appears on one of the diagnostic tests (for example, the Mantoux test or interferon gamma expression analysis);
- with changes on the radiograph after tuberculosis.
This mode is not recommended:
- children under 2 years old;
- people with HIV/AIDS taking antiretroviral medications;
- infected with drug-resistant bacilli;
- pregnant women or planning pregnancy in the next 12 weeks.
www.cdc.gov
Outcome for the patient
Treatment of the closed form is indicated for all carriers of the infection, as it can significantly reduce the risk of developing the disease in the future. Regular testing of high-risk populations is recommended.
If a diagnosis of “closed form of tuberculosis” is made, it is necessary to immediately begin treatment with the most effective and appropriate drugs, as prescribed by the attending physician. To get a favorable outcome, it is important to follow the entire course of treatment without interrupting it. Inpatient treatment will be more effective.
www.cdc.gov
www.who.int
Treatment options
Is it possible to cure open tuberculosis? Timely treatment and the use of effective medications gives many patients a great chance of recovery. Modern treatments are governed by three principles:
- Reduce bacteria counts as quickly as possible. This measure minimizes the severity of symptoms and the risk of disease transmission.
- Preventing the development of drug resistance. Regular use of drugs causes bacteria to become resistant to them.
- Long-term monitoring of the patient and the use of appropriate therapy to prevent relapses.
The disease is treated with strong antibiotics for six months to two years. Because some strains of the disease are unusually resistant to drugs, drugs are being tested on bacteria that infect humans to determine effective treatments. In severe cases, the person may undergo surgery to remove the infected areas.
Attention! Under no circumstances should treatment be interrupted without consulting a doctor! This is unsafe for the health of not only the patient, but also the people who are in contact with him.
How long does it take to treat the pathology?
When treating with isoniazid, two regimens are usually prescribed, which last 6 or 9 months. The 9-month regimen is preferred due to its higher effectiveness.
Treatment for 6 months is less expensive for patients and therefore has a wider response. Taking this fact into account, the attending physician may prescribe 6-month therapy, since the main thing is that a person with a closed form of tuberculosis takes medication for at least 6 months.
The use of Rifampicin for 4 months can be considered for people who cannot tolerate or are not susceptible to isoniazid. This regimen should not be used in patients with HIV infection who are taking antiretroviral drugs.
The combined use of isoniazid and rifampicin for 12 weeks, one dose per week, is recommended as an alternative to a 9-month course of isoniazid in healthy people at high risk of developing the disease. The duration of the course may change depending on the test results.
www.cdc.gov