Free consultation on treatment in Moscow. Call or fill out the form below:
Cancer of the oral mucosa is a malignant tumor that develops from the epithelium lining the cavity from the inside. Squamous cell carcinoma predominates, but there are pathologies originating from the minor salivary glands of the palate, oral floor, and cheeks. It occurs three times more often in men, but recently its detection in women has also been increasing.
Epidemiology has revealed significant differences in population morbidity in different regions of the globe. The highest rates are in India, Pakistan, Sri Lanka, Tajikistan, Uzbekistan, Kyrgyzstan and some neighboring countries of Russia. The predisposition is associated with the traditional use of betel nut.
If you or your loved ones need medical assistance, contact us. The site’s specialists will recommend a clinic where you can get effective treatment:
Risk factors for developing oral cancer
One of the main risk factors for developing oral cancer is tobacco use. This includes smoking cigarettes, cigars and pipes, and chewing tobacco.
People who drink large amounts of alcohol and use tobacco are at even greater risk, especially when both products are used on a regular basis.
Here are other risk factors for developing oral cancer:
- human papillomavirus (HPV)
- chronic exposure to sunlight on the face
- previous diagnosis of oral cancer
- family history of oral or other cancers
- weakened immune system
- poor nutrition
- genetic diseases
- male
Men are twice as likely to develop oral cancer as women.
Causes
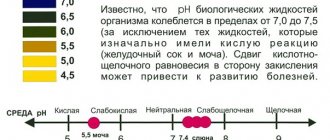
The exact cause leading to the appearance of tumors in the mouth has not been established. Researchers have only identified a number of factors that significantly increase the likelihood of developing this disease. The key among them are bad habits - smoking, chewing nasvay or betel, as well as alcohol abuse.
Additional factors are:
- Chronic mechanical injuries of the oral cavity.
- Using low-quality or ill-fitting dentures.
- Poor treatment of fillings and dental injuries - sharp edges of fillings and broken teeth cause constant injury to the mucous membranes of the cheeks and tongue.
- Injuries to gums from dental instruments.
- Poor hygiene.
- The use of metal prostheses made of different metals in dental prosthetics - galvanic voltage can arise between different metals, which leads to cell damage and malignancy.
According to recent research in virology and medicine, human papillomaviruses, which can be transmitted through kissing, play a certain role in the development of oral cancer.
An increased incidence of this pathology has been noted in people working in difficult and harmful conditions: in constant contact with harmful substances, in conditions with high or extremely low temperatures and high humidity.
Exposure to spicy and hot foods also contributes to the formation of tumors on the oral mucosa. The situation is aggravated by a deficiency of vitamin A in food and the presence of inflammation or precancerous disease in the oral cavity.
Precancerous diseases that can develop into cancer of the oral mucosa
- Leukoplakia . It looks like a whitish spot on the mucous membrane in any area of the oral cavity: on the palate, on the cheeks near the lips on the inside. Characterized by areas of keratinization of the epithelium.
- Erythroplakia. It is characterized by the appearance of red lesions, abundantly penetrated by blood vessels. Up to half of the cases of erythroplakia transform into oncology.
- Dysplasia is actually a precancer. Examination of dysplastic lesions under a microscope shows that some of the cells have already acquired malignant features. If this pathology is ignored, in 99% of cases oral cancer develops within a few months.
What are the signs and symptoms of oral cancer?
Here are the signs and symptoms of oral cancer:
- a sore on the lip or mouth that does not heal
- growth anywhere in the mouth
- bleeding from the mouth
- tooth loss
- pain or difficulty swallowing
- problems wearing dentures
- lump in throat
- ear pain that doesn't go away
- severe weight loss
- numbness of the lower lip, face, neck, or chin
- white, red, and white or red patches on the lips or mouth
- a sore throat
- pain or stiffness in the jaw
- tongue pain
Some of these symptoms, such as a sore throat or earache, may indicate other conditions. However, if you notice any of these symptoms, especially if they do not go away or you have more than one, contact your dentist or doctor as soon as possible.
Diagnostics
The diagnosis is made based on the patient's complaints and after examining the oral mucosa. A tumor biopsy helps confirm the diagnosis. Technological diagnostic methods, such as ultrasound or tomography, are not very informative for these tumors. To identify damage to the bone tissue of the lower and upper jaws, the patient is prescribed an x-ray of the facial skeleton.
To identify metastatic foci, doctors usually prescribe an ultrasound of the abdominal organs and a chest x-ray. It is also possible to prescribe computed tomography or magnetic resonance imaging.
More often, dentists are the first to notice neoplasms in the oral cavity due to the peculiarities of their profession. When the first signs of cancer are detected in the mouth, the patient must be referred for a consultation with an oncologist.
How is oral cancer diagnosed?
First, your doctor or dentist will perform a physical examination. It involves a thorough examination of the top and bottom of the mouth, the back of the throat, the tongue and cheeks, and the lymph nodes in the neck. If your doctor can't determine the cause of your symptoms, you may be referred to an ear, nose, and throat specialist.
If your doctor finds any tumors, growths, or suspicious lesions, he will perform a biopsy.
In addition, your doctor may perform one or more of the following tests:
- X-ray . To see if cancer cells have spread to the jaw, chest or lungs.
- CT scan . To detect any tumors of the mouth, throat, neck, lungs or other parts of the body.
- PET scan . To determine whether the cancer has spread to the lymph nodes or other organs.
- MRI . To obtain a more accurate image of the head and neck and determine the extent or stage of cancer.
- Endoscopy . For examination of the nasal passages, sinuses, inner throat, respiratory tract and trachea.
Photo
In photographs of cancer of the oral mucosa, neoplasms are clearly visible, which are the main symptoms of the disease. Neoplasms can differ both in appearance and in the nature of pain.
Most often, the inner surfaces of the cheeks are affected, especially at the level of the mouth line
Leukoplakia of the oral cavity is one of the causes of cancer development
Cancer of the oral mucosa: photo of a benign tumor
Stages of oral cancer
There are four stages of oral cancer.
- Stage 1 : The tumor is 2 cm or smaller and the cancer has not spread to the lymph nodes.
- Stage 2 : The tumor is 2–4 cm and the cancer cells have not spread to the lymph nodes.
- Stage 3 : The tumor is either larger than 4 cm and has not spread to the lymph nodes, or is any size and has spread to one lymph node but not to other parts of the body.
- Stage 4 : Tumors are any size and cancer cells have spread to nearby tissue, lymph nodes, or other parts of the body.
According to the National Cancer Institute, five-year survival rates for oral and pharynx cancer are as follows:
- 83% for localized cancer (that has not spread)
- 64% for cancer that has spread to nearby lymph nodes
- 38% for cancer that has spread to other parts of the body
Overall, 60% of all people with oral cancer will survive for five years or more. The earlier the diagnosis is made, the higher the chance of survival after treatment. In fact, the five-year overall survival rate for patients with stage 1 and 2 oral cancer is typically between 70 and 90 percent. This makes timely diagnosis and treatment all the more important.
Signs
The first symptoms of oral cancer, oddly enough, are very similar to ordinary inflammation. But at the very beginning without pain.
- The appearance of redness, ulcers, nodules on the surface of the mucous membranes.
- Various strange spots of white and red.
- Burning, tingling and numbness of the affected area.
- A small bump is visible. You can feel it on your tongue or cheek by slightly pressing on the sore spot.
- The pain radiates to the temples and ears.
- Severe inflammation, pus, bad breath.
- Long-lasting sores inside the mouth.
- It is difficult to swallow, move the tongue, or the cheek with a significant size of the tumor.
- The appearance of a lisp when speaking.
- Headaches, weight loss, drowsiness, fatigue, dizziness.
- Metallic taste of blood.
As the disease progresses and the tumor becomes larger, it will release more waste products, plus pathogenic bacteria will enter the ulcer. Subsequently, the neoplasm will grow and germinate into neighboring tissues, organs, and later metastasize.
NOTE! If you suspect oral cancer or have any strange symptoms, you should immediately contact your dentist. You should not postpone your visit and try to treat yourself.
Treatment of oral cancer
Treatment for oral cancer will vary depending on the type, location, and stage of cancer at diagnosis.
Surgery
Treatment in the early stages usually involves surgery to remove the tumor and cancerous lymph nodes. In addition, other tissue in the mouth and neck area may also be removed.
Radiotherapy (radiation therapy)
Radiation therapy is another option. The doctor shines the beams on the tumor once or twice a day, five days a week, for two to eight weeks. Treatment for advanced stages usually involves a combination of chemotherapy and radiation therapy.
Chemotherapy
Chemotherapy is treatment with drugs that kill cancer cells. The medicine is given to you either orally or intravenously. Most people receive chemotherapy as an outpatient, although some require hospitalization.
Targeted therapy
Targeted therapy is another form of treatment. It can be effective in both early and late stages of cancer. Targeted drugs will bind to specific proteins on cancer cells and interfere with their growth.
Nutrition
Nutrition is also an important part of your oral cancer treatment. Many treatments make eating and swallowing difficult or painful, and poor appetite and weight loss are common. Be sure to discuss your diet with your doctor.
Getting advice from a nutritionist can help you create a menu that suits your mouth and throat and provides your body with the calories, vitamins and minerals it needs to heal.
Maintaining oral health
Finally, keeping your mouth healthy during cancer treatment is an important part of treatment. Make sure your mouth is moist and your teeth and gums are clean.
Classification of malignant tumor of the mouth
Malignant tumors of the mouth can be classified in several ways.
Depending on the location of the tumor process in the oral cavity, the following types of cancer are distinguished:
- floor of mouth;
- mucous membrane of the tongue, with the exception of its root;
- cheeks;
- hard palate or soft palate;
- gums;
- alveolar process of the lower jaw or upper.
Based on their appearance, tumors are divided into:
- ulcerative - a defect appears in the oral cavity in the form of a long-term non-healing, often bleeding, constantly growing ulcer. The bottom of the ulcer is often lumpy and covered with a grayish-dirty coating. The edges of the ulcer rise above itself and the surrounding surface of the mucous membrane;
- nodular - expressed by the appearance of thickening of the mucous membrane, which is clearly limited from still healthy tissues. The surface of such neoplasms may be covered with a whitish coating or may not change at all;
- papillary - formations that seem to “hang” from the area of the mucous membrane from where they begin to grow. The mucous membrane has virtually no changes.
An important place among all divisions is given to the international classification of malignant tumors of the oral cavity according to histological principles.
So, depending on which cells the tumor grows from, cancer is usually divided into:
- tumors growing from soft tissues : fibro-, rhabdo-, lipo-, chondro-, leiomyosarcoma, as well as the following malignant types: angiosarcoma, schwannoma, lymphosarcoma, hemangiopericytoma;
- tumors growing from stratified squamous epithelium : squamous cell carcinoma, carcinomas - intraepithelial, spindle cell, verrucous, as well as lymphoepithelioma;
- melanogenic tumors: melanoma (malignant);
- tumors of unspecified or controversial origin - such types of sarcomas as: Kaposi, alveolar soft tissue, as well as granular cell tumor of a malignant type.
Recovery after oral cancer treatment
Recovery from each type of treatment will vary.
Postoperative symptoms may include pain and swelling, but removing small tumors usually does not have long-term problems.
Removing large tumors may affect your ability to chew, swallow, or speak. You may also need reconstructive surgery to restore bone and tissue in your face that was removed during surgery.
Radiation therapy can have negative effects on the body. Here are some of the side effects you may experience:
- sore throat or mouth
- dry mouth and loss of salivary gland function
- tooth decay
- nausea and vomiting
- sore or bleeding gums
- skin and mouth infections
- stiffness and pain in the jaw
- problems with prosthetics
- fatigue
- changes in your ability to taste and smell
- changes in your skin, including dryness and burning
- weight loss
- thyroid changes
Chemotherapy drugs can be toxic to fast-growing, non-cancerous cells. This type of treatment may cause side effects such as:
- hair loss
- pain in the mouth and gums
- bleeding in the mouth
- severe anemia
- weakness
- poor appetite
- nausea
- vomit
- diarrhea
- sores in the mouth and lips
- numbness in the arms and legs
Recovery from targeted therapy is usually minimal. Here are the side effects of this type of treatment:
- fever
- headache
- vomit
- diarrhea
- allergic reaction
- rash
Although these treatments have side effects, they are often necessary in the fight against cancer. Your doctor will discuss side effects and help you weigh the pros and cons of your treatment options.
Prevention
Since the most common cause of oral cancer is smoking or tobacco use, it is necessary to completely abandon these bad habits. In general, prevention comes down to following the following recommendations:
- Do not stay in the sun for a long time.
- Eat properly.
- Visit the dentist in a timely manner.
- Brush your teeth regularly.
- Treat wounds and erosions on the mucous membrane in a timely manner.
- Limit your intake of spicy and hot foods.
Reconstruction and rehabilitation after treatment for oral cancer
People diagnosed with advanced oral cancer will likely need reconstructive surgery and some rehabilitation to help with eating and speaking during recovery.
Reconstruction may include dental implants or grafts to replace missing bone and tissue in the mouth or face. An artificial palate is used to replace missing tissue or teeth.
Rehabilitation is also necessary for cases of advanced cancer. Speech therapy may be provided from the time of exit from surgery until the maximum level of improvement is achieved.
Diagnosis of cancer
Since the oral mucosa is examined daily by a person during hygiene procedures, the slightest changes on it are visible to the naked eye. This speeds up the diagnosis - during the examination, the specialist can also note areas of tissue thickening, cracks, and ulcers.
To confirm or refute the diagnosis, modern examination methods will be recommended:
- collection of mucosal cells from a suspicious area for examination under a microscope - biopsy;
- Ultrasound – examination of nearby internal organs and tissues for the presence of secondary tumors and foci of cancer;
- X-ray – examination of the bone structures of the skull, lungs;
- if necessary – CT, MRI are performed;
- laboratory tests - to clarify the general state of human health.
Only after receiving all the information from the above diagnostic procedures will a specialist be able to make a full diagnosis - whether a person really has a cancer focus in the oral cavity.
Forecast
The prognosis for oral cancer depends on the specific type and stage of cancer at diagnosis. It also depends on your general health, your age, tolerance and response to treatment. Early diagnosis is critical because treatment for stage 1 and 2 cancers can be less destructive and have a higher chance of successful treatment.
After treatment, your doctor will ask you to have regular checkups to make sure you are improving. Your examinations usually consist of physical examinations, blood tests, x-rays and CT scans. Be sure to check with your dentist or oncologist if you notice anything unusual.
Forms of mucosal cancer
The disease has several forms:
- Knotty shape. It is characterized by the appearance of a compaction with clear edges. The mucous membrane around it does not change, and the compaction itself quickly increases in diameter.
- Ulcerative form. During the ulcerative form of the disease, the mucous membrane is affected by numerous ulcers. The ulcerative form of the disease occurs most often in patients.
- Papillary form. It is a hanging tumor.
When diagnosing, you should be extremely careful, because the initial stages of cancer often try to disguise themselves as other, harmless diseases. Therefore, before making a final diagnosis, it is necessary to undergo the following examinations: magnetic resonance imaging (MRI), biopsy, radiography.
Timely treatment – quick recovery without consequences
When the first signs appear, you need to consult a doctor and choose the right treatment, which will be aimed at eliminating the root cause of the disease and its consequences.
This approach will help stop the development of further inflammatory process, avoid complications and get rid of painful sensations. Remember, your health is only in your hands, so remember it every day and spend time visiting competent specialists. This article is for informational purposes only, please consult your doctor for details! Ask your doctor about contraindications and side effects.
Diagnosis of cancer
To diagnose cancer in a timely manner, you will need to conduct a self-examination. However, some areas are difficult to inspect. Therefore, it is recommended to undergo a dental examination once a year. If alarming sensations or neoplasms appear, such an examination should be unscheduled.
Diagnosis of oral cancer
The doctor will carefully examine, especially the sublingual area. A hospital visit will be required for additional examination and consultation. The oral cavity is examined using a lamp and a small mirror. To carefully examine its posterior sections, use an endoscope (a thin long tube equipped with a light bulb at the end).
To make a diagnosis, a biopsy is required, which involves removing a tiny piece of tissue from the oral area for microscopic examination. Typically, general anesthesia is used for this procedure, so a short hospital stay will be required. The patient's general health is assessed through blood tests and chest x-rays. A tumor can also be diagnosed using other examination methods.
The most common diseases of teeth and gums:
- Caries.
This is a common problem that affects almost every person at different ages. At the first stage of development, spots appear on the enamel, and as a result of development, hard tissues are destroyed;
- Gingivitis.
An inflammatory process that causes swelling and tenderness of the soft tissues. If treatment is not treated in a timely manner, the problem worsens and becomes chronic;
- Periodontitis.
A popular problem in which the initial stage is asymptomatic. Pain and discomfort appears after damage to bone and soft tissue;
- Periodontal disease
is expressed in periodontal damage, which can lead to tooth loss. Therefore, it is important to start treatment in a timely manner.
Cancer of the mucous membrane of the alveolar processes of the upper and lower jaws
Almost always has the structure of squamous cell carcinoma. It manifests itself quite early, because the teeth are involved in the process, and toothache occurs. This can lead the doctor down the wrong path. In the initial period, the tumor is local and bleeds with easy penetration. Infiltration of the underlying bone tissue occurs after several months and is considered a late manifestation of the disease. The extent of spread to the bone is determined radiographically. Regional metastasis is observed in a third of patients.
Features of regional metastasis of malignant tumors of the oral cavity. Oral cancer usually metastasizes to the superficial and deep lymph nodes of the neck. The frequency of metastasis is high and, according to various sources, ranges from 40 to 70%. The frequency and localization of regional metastases depends on many factors: histological identity, localization, size of the tumor, features of lymph circulation in the affected organ. Thus, with cancer of the mid-lateral surfaces and the tip of the tongue, metastasis occurs in the submandibular, middle and deep cervical lymph nodes of the neck. Cancer of the distal parts of the tongue metastasizes early and 2 times more often than the proximal parts (35 and 75%, respectively). When the mucous membrane of the cheeks, floor of the mouth and alveolar processes of the lower jaw are affected, metastases are found in the submandibular lymph nodes. Mental lymph nodes are rarely affected by metastases when tumors are localized in the anterior sections of these organs.
Cancerous tumors of the distal parts of the oral cavity often metastasize to the middle and upper jugular lymph nodes. When the mucous membrane of the oral surface of the alveolar processes of the upper jaw is damaged, metastasis occurs in the retropharyngeal lymph nodes, which are inaccessible to palpation and surgical removal. In general, oral cancer can affect any lymph nodes in the neck. Supraclavicular lymph nodes are extremely rarely affected.
Distant metastases from oral cancer are rare. According to US oncologists, they are diagnosed in 1-5% of patients. Distant metastases can affect the lungs, heart, liver, brain, and skeletal bones. Their diagnosis can be very difficult and in some patients they are detected only at autopsy.
When regional metastases are detected, regardless of the size of the primary tumor, the prognosis worsens. In general, the prognosis for oral cancer is very serious. In comparative terms, cancer of the distal parts of the oral cavity has a poor prognosis, while cancer of the proximal parts is somewhat worse. The presence of distant metastases, regardless of their number, location, or size of the primary tumor, indicates the patient’s incurable condition (only symptomatic treatment is indicated).
Diagnostics, mandatory use of all methods of clinical examination of patients, and the main task of the morphological research method at the present stage is not only to determine the tumor identity and histo- and cytological picture, but also to identify signs characterizing the structural features of squamous cell carcinoma: the degree of differentiation, cellular and nuclear polymorphism , mitotic activity. Analysis of tumor invasion into surrounding organs and tissues is also necessary.
The Clinic of Dental Surgery at SamSMU has developed a method for diagnosing the extent of primary tumors of the tongue using electromyography. For this purpose, aluminum electrodes were used, fixed on the tongue with MK-1 glue. Biopotentials were recorded on a Medicor electromyograph. Biopotentials were recorded on the healthy and affected sides of the organs. Normally, the value of the biopotential of the tongue muscles depended on the area of study and was 180 μV at the tip, 200 μV in the middle third, and 240 μV at the lateral surface of the middle third. In case of a malignant tumor, fluctuations in biopotential depended on the stage of the tumor process. At T1 – 190 µV on the healthy side and 170 µV on the affected side, at T2, 160 and 140 µV, respectively, at T3 – 100 and 85 µV, at T4, due to the large spread of the tumor, the total bioelectrical activity of the muscles was only 40 µV. Thus, the electromyographic method can be used to objectify the extent of the tumor process.
Differential diagnosis of malignant tumors of the oral cavity is often carried out with precancerous diseases, tumors from the minor salivary glands, specific and nonspecific inflammatory processes. Tumors from the minor salivary glands (polymorphic adenoma, mucoepidermal tumor) are usually localized in the posterior parts of the tongue and hard palate. They grow slowly, lateral to the midline, have a rounded shape, and are covered with a normal mucous membrane. Their consistency is dense. The final diagnosis is possible after a morphological examination. Inflammatory processes usually occur after injury by a foreign body and are painful, with the formation of a large infiltrate. Anti-inflammatory treatment leads to rapid relief of the process. Syphilis and tuberculosis of the oral mucosa are rare and are usually secondary. Specific reactions and biopsy help in diagnosis.
Differential diagnosis of malignant tumors of the oral cavity is often carried out with precancerous diseases, tumors from the minor salivary glands, specific and nonspecific inflammatory processes. Tumors from the minor salivary glands (polymorphic adenoma, mucoepidermal tumor) are usually localized in the posterior parts of the tongue and hard palate. They grow slowly, lateral to the midline, have a rounded shape, and are covered with a normal mucous membrane. Their consistency is dense. The final diagnosis is possible after a morphological examination. Inflammatory processes usually occur after injury by a foreign body and are painful, with the formation of a large infiltrate. Anti-inflammatory treatment leads to rapid relief of the process. Syphilis and tuberculosis of the oral mucosa are rare and are usually secondary. Specific reactions and biopsy help in diagnosis.
In recent years, radiologists have been searching for ways to make radiation therapy more effective (irradiation using particle accelerators, HBOT, contact neutron therapy). Great hopes are placed on the use of cell cycle synchronizer drugs (metronidazole) in clinical practice. There are reports of improved results of radiation therapy when combined with hyperthermia.
Isolated radiation therapy is still the main treatment method for cancer of the distal oral cavity. The reason is good short-term results due to the high radiosensitivity of tumors in this location and inaccessibility for surgical treatment. In general, the commitment of many researchers to isolated radiation therapy for malignant tumors of the oral cavity is understandable, because it is better tolerated by patients and eliminates the appearance of cosmetic and functional disorders. However, data from the specialized literature and our research allow us to conclude that in most cases, isolated radiation treatment does not provide a lasting effect in distal tumor localizations, as well as in the most common T3-4 cancer that the clinician deals with.
The use of chemotherapy, especially a complex of chemotherapy drugs, made it possible to ensure regression of tumors in some cases by more than 50% of the initial value. It turned out that squamous cell carcinoma of the oral cavity is sensitive mainly to two drugs: methotrexate and bleomycin. However, despite the good immediate results of chemotherapy, the life expectancy of patients could not be increased. The combination of chemotherapy with radiation therapy improved results by only 10% with an increase in the number of local and general complications. Based on the above, the renewed interest of surgeons and oncologists in the possibilities of the surgical method becomes clear.
The surgical method of treating malignant tumors of the oral cavity is performed according to all the rules accepted in oncology: i.e. resection of the affected organ should be carried out within healthy tissues, departing from the visible and palpable boundaries of the tumor by 2.5-3.0 cm. An isolated surgical method for this localization of tumors is practically not used due to their particular malignancy. In most cases, a combined treatment method is prescribed according to the following scheme: preoperative irradiation in the SOD - 45-50 Gy, a three-week break, then radical surgery. Since more than half of malignant tumors of the oral cavity occur on the tongue, we will dwell in more detail on the methods of surgical treatment of malignant tumors of this location. The most common method of surgical intervention for tongue cancer to date is hemiglossectomy (half resection). This operation was first performed by Pimperhell in 1916. Pirogov's development of a technique for ligating the lingual arteries significantly reduced the risk of surgery associated with the possibility of heavy bleeding. Hemiglossectomy is performed for T1-2 tongue cancer affecting the lateral surface of the tongue. The operation is performed under endotracheal anesthesia. The tongue is mobilized by cutting the frenulum. The tip of the tongue is fixed with a silk ligature, with the help of which the tongue is removed from the oral cavity as much as possible. A scalpel is used to dissect the tissue from the root to the tip of the tongue, adhering to the midline. The tongue stump is sutured (on itself) after hemostasis. The five-year survival rate of patients after half resection of the tongue is, without specifying stages and locations, about 40%.
Unsatisfactory treatment results for this group of patients force us to look for more rational methods of surgical interventions. In recent years, there has been a noticeable tendency to expand the scope of surgical interventions for tongue cancer. Thus, Tsybarne (1983) suggests retreating from the tumor boundaries by 4.0-5.0 cm. V.L. Lyubaev, A.I. Paches, G.V. Falileev expands the scope of the operation to resection of half of the tongue with the root, lateral wall of the pharynx and tissues of the floor of the mouth. In this regard, the work of Yu.A. is very interesting. Shelomentsev, who studied the features of the microvasculature of the tongue and the floor of the mouth. He established a close relationship between the lymphatic and bloodstream of the tongue, the floor of the mouth, and the submandibular salivary glands. Without taking these features into account, it is impossible to perform radical surgery. Taking the data of Yu.A. Shelomentsev as a basis, the Department of Surgical Dentistry of SamSMU proposed a new method of surgical treatment of locally advanced malignant tumors of the tongue (T2-3), for which an author’s certificate was received (Olshansky V.O., Fedyaev I.M., Belova L.P.). The method consists in the fact that under endotracheal anesthesia, the tongue affected by the tumor, the tissues of the floor of the mouth and the regional lymphatic system in an appropriate volume are simultaneously removed in a single block. The operation is performed via extraoral access and ends with plastic surgery of the floor of the mouth defect using a skin-fat flap of the neck and the tumor-free oral mucosa. Maximum life expectancy is 10 years. Relapse was observed in only one patient due to abnormal ablastics. There is no need to talk about a solution to the problem of treating patients with tongue cancer. Surgical interventions of this kind have a number of disadvantages. First of all, they are traumatic. Having a large volume, they cannot always be performed in patients with concomitant diseases of the respiratory and cardiovascular systems. In addition, large-scale operations inevitably entail severe disturbances in vital functions: speech, eating, and traumatize the psyche of patients, so patients do not always consent to the operation. Our clinical material allows us to draw the following conclusion: for tongue cancer, the greatest effect is achieved by combined treatment: radiation therapy + surgery. The extent of surgical intervention depends on the extent of the tumor: T1, hemiglossectomy is indicated, for T2-3 - surgery in the above volume, for T4 - palliative or symptomatic treatment.
Treatment with folk remedies
Ointments
Ointment forms of drug release for stomatitis are not effective, since the ointment “rolls off” from the oral mucosa without providing a therapeutic effect. Acyclovir is used for herpes stomatitis, but only in the form of a gel, not an ointment.
Vinylin
Another name for the drug is Shostakovsky balm. Vinilin has an antiseptic and wound-healing effect and is suitable for the treatment of aphthous stomatitis. Given its low toxicity, it can be used in children. Choose an aerosol dosage form.
Solcoseryl
For ulcerative lesions of the mucous membrane, the use of Solcoseryl-gel and Actovegin-gel is justified as an additional means to accelerate tissue regeneration. For the same purposes, dentists use Methyluracil, but this drug has contraindications, so it is better to consult a doctor.
Holisal
Dentists often prescribe this particular remedy for stomatitis. Cholisal gel has pronounced antimicrobial and anti-inflammatory activity, is well absorbed by the mucous membrane and has an analgesic effect. The disadvantage of the gel is the taste of anise oil, which increases salivation.
For minor forms, you can use home remedies to treat stomatitis. But if the condition does not improve, seek professional medical help from the best dentists in the city - rating on our website.
Language
The anatomy of the human oral cavity also provides the formation of taste sensations. They occur when various chemicals interact with specialized receptors. Agree, the perception of taste is purely individual. But scientists distinguish its main varieties. These include sour, bitter, sweet and salty.
Taste receptors are called chemoreceptors. They are located in taste buds, each of which connects to the mouth opening at a time. Despite the general plan of the structure, they are all specialized. So, at the tip of the tongue there are receptors that perceive sweet, at the edges - sour, at the root - bitter. The larger area is capable of perceiving salty taste. It is located at the tip and along the edges. The tongue is also involved in the formation of sounds, wetting, mixing and swallowing food.
Metastasis
Cancer pathology is characterized by a high rate of germination into the surrounding tissue layers. The degree of activity of compaction development is determined by its shape and location.
The development of pathology occurs in the flow of mutant cells into the lymphatic ducts and nodal connections.
- With oncology of the cheeks and alveoli, the disease metastasizes to the mandibular zone.
- Anomalies that develop in the distal zones metastasize to the jugular vein.
- When parts of the tongue are affected, metastasis processes work in the area of the submandibular lymph nodes and cervical joints.
Distant metastases destroy the bone tissue of the skull, liver, pulmonary system, and heart.
Types of pathologies
Depending on the type of microorganisms that caused the appearance of the abnormal condition, all diseases detected in the oral cavity are conditionally differentiated into infectious and fungal . Additionally, dental problems, allergic reactions and cancer are identified, the etiology of which has not been clinically confirmed.
Infectious diseases of the oral cavity and their symptoms
The infectious group of diseases combines diseases that arise as a result of the growth and development of bacterial and viral colonies in the affected tissues. The list of the most common diseases includes stomatitis, gingivitis, glossitis, pharyngitis. The main reasons for their appearance are poor-quality procedures for caring for the gums, tongue and teeth, as well as the progression of pathologies of internal organs, mainly gastrointestinal disorders - peptic ulcer, gastritis, enterocolitis.
To avoid the occurrence of infectious diseases, you should undergo regular preventive medical examinations and visit the dentist.
Stomatitis
Stomatitis is one of the anomalies that develops in patients of different ages. There are several types of disease. The list of common stomatitis includes:
- Aphthous. Caused by the herpes simplex virus. The primary symptoms of the oral infection in question are swelling of the mucous membrane, tissue hyperemia. As it develops, painful erosions (aphthae) appear, covered with a fibrinous coating. The second name for the lesion is herpetic stomatitis.
- Vesicular. The signs are similar to the symptoms described above. It is detected by the presence of small vesicular eruptions that transform into erosions. The pathology is of herpetic nature.
- Catarrhal. When an infection enters the oral cavity, swelling of the mucous membranes develops, and a light yellow coating appears.
It is impossible to determine the type of stomatitis on your own. At the first signs of illness, you should immediately consult a doctor.
Gingivitis
Inflammation of the gums is provoked by chemical, mechanical, and infectious factors. Gingivitis, activated as a result of the activity of pathogenic agents, occurs mainly in children and young people and either manifests itself as independent pathologies or signals the development of other ailments, including periodontal disease.
Signs of gingivitis:
- swelling;
- inflammation of the mucous membrane of the gum line;
- bad breath;
- tissue bleeding.
Dentists distinguish between acute and chronic forms of gingivitis. The latter is characterized by the duration of its course and the weakness of its symptoms.
Glossitis
Glossitis is a large group of pathologies that cause disruption of the structure and change in color of the tongue. The risk group includes people who refuse regular hygiene procedures. The infection penetrates into the tissues of the tongue in the presence of injuries, inflammation in the oral cavity or the gastrointestinal tract.
You can prevent the occurrence of glossitis through the daily use of floss, hygienic rinses, and high-quality toothpastes.
Diseases of the larynx
Chronic and acute forms of pharyngitis, tonsillitis (tonsillitis), laryngitis are accompanied by a deterioration in the general condition of the patient, the appearance of dry mouth, discomfort and sore throat. Children and people with weakened immune systems are most susceptible to developing these pathologies. Hardening, playing sports, and taking vitamins will help to avoid the appearance of anomalies.
Other anomalies of viral etiology
Unprotected oral-genital contacts are the cause of oral infection with sexually transmitted infections. With this type of intimate relationship, the following are transmitted from a patient to a healthy partner:
- gonorrhea;
- syphilis;
- cytomegalovirus;
- chlamydia;
- human papillomavirus;
- HIV.
The presence of the disease is indicated by plaque on the tonsils and enlarged lymph nodes. When swallowing, the root of the tongue and throat hurt. If left untreated, the pathogen spreads quickly and the disease becomes chronic.
Fungal infections
The causative agents of fungal diseases of the mucous membranes of the oral cavity are yeast-like microorganisms Candida, penicillium, and aspergillus. Infectious agents belong to the group of saprophytes that acquire pathogenic properties and cause a mycotic process only under certain conditions. Among the factors that activate their vital functions are weakened immunity, treatment with corticosteroids and antibiotics, and the presence of diseases.
Infection with mold fungi occurs in 2% of cases of the total number of examined patients. The most common disease localized on the mucous membranes is candidiasis.
Candidiasis
According to the nature of the course, the disease is differentiated into 3 forms:
- Pseudomembranous or acute. The main signs of its development include dryness of the inner surfaces of the palate, lips, cheeks, tongue and the formation of a white cheesy coating in these areas. The patient feels itching and burning.
- Hyperplastic or chronic. It is distinguished by the appearance of plaques tightly fused to the tissues. Attempts to remove plaque cause bleeding of the mucous membranes.
- Atrophic. Identified in patients using removable orthopedic structures. The list of symptoms includes dryness and inflammation of the surface of the oral mucosa.
Yeast-like microorganisms can cause fungal glossitis, sore throat, and angular infectious cheilitis. The last of these ailments affects the red border of the lips. When opening the mouth, patients experience severe discomfort. Superficial erosions, detected at the onset of the disease, spread to the skin of the chin as cheilitis progresses.
To avoid the development of fungal pathologies, experts recommend strengthening the immune system and avoiding stress and hypothermia.
Dental problems
Diseases in the oral cavity are also detected in patients who refuse regular visits to the dentist. If left untreated, periodontitis and periodontal disease worsen the condition of the gums, expose the necks of the teeth, and disrupt the structure of the jaw. The list of additional signs of the presence of diseases includes swelling and bleeding of tissues. If you constantly postpone a visit to the doctor, you can lose teeth located at the site of inflammation.
The development of carious processes is accompanied by a change in the composition of the microflora of the oral cavity. Dental plaque forms in carious holes, which plays a significant role in the activation of the previously listed diseases. The only way to avoid the progression of the problem is by visiting a clinic.
Diseases of unknown etiology
Among the diseases observed in the oral cavity is lichen planus, an anomaly whose causes are not clear. The clinical picture of the disease has a number of features:
- In the initial stage, rashes appear on the mucous membranes of the oral cavity - small papules.
- The progression of pathology leads to an increase in affected areas and their merging.
- Stripes and plaques with a keratinized grayish-white surface form on the tissues, protruding above the level of the mucous membranes.
Treatment regimens for lichen are selected individually, taking into account the patient’s condition.
Other pathologies
Among the ailments that change the structure of the oral mucosa are diseases resulting from allergic reactions. These include Reiter's syndrome, Lyell's syndrome, and exudative erythema. Provoking factors that cause abnormal conditions are microbial, contact and drug allergies. Treatment regimens for diseases include studying the allergological status and eliminating the source of negative impact.
The incidence rate of oral cancer varies from 2 to 4% of the total number of cancer pathologies detected in Russia. At an early stage, the disease proceeds hidden. Its further development is accompanied by the appearance of local pain, bleeding, and ulcers. In a later period, the discomfort intensifies and begins to radiate to the cheekbones, temples, and forehead. The outcome of oncological pathologies depends on the stage of the identified process and the general condition of the patient.
Treatment regimens for diseases of the oral cavity and tongue
Treatment of infections in the mouth involves the use of a complex of drugs. Health workers recommend treating emerging foci of inflammation with antiseptics (Miramistin, Chlorhexidine, Furacilin, Hexoral) and infusions of raw medicinal plants (calendula, chamomile, sage).
The development of viral diseases in the oral cavity is suppressed by the use of Famvir, Valacyclovir, Acyclovir. When chronic pathology is detected, antibiotics are used - Ciprofloxacin, Augmentin, Amoxiclav. For the treatment of mycotic diseases of the oral cavity and tongue, the drugs Nystatin and Levorin are used.
To speed up the regeneration process, doctors include rosehip and sea buckthorn oils, propolis ointment, and the drug Solcoseryl in treatment regimens. Itching, burning and swelling are minimized with the help of antihistamines (Tavegil, Cetirizine), pain - with analgesics and NSAIDs (Nise, Aspirin, Ibuprofen).
Dental pathologies should be treated when their first signs are detected. Teeth affected by caries are filled, and units of the dentition that cannot be restored are removed.
Additional measures
Following a special diet helps stop the development of pathologies. The patient's menu should not consist of excessively hot dishes, hot sauces, or sour dressings. Alcoholic beverages are prohibited.
The list of permitted products includes milk, vegetables (boiled), and cereals in the form of porridges. Multivitamin complexes and herbal medicine will help to consolidate the achieved effect.
Phases of development
Neoplasms, even of benign origin, after some time degenerate into a malignant tumor, which, as it progresses, goes through three stages of development:
- The initial form is characterized by unusual phenomena for the patient in the form of pain, ulcers, and lumps in the oral cavity.
- A developed form of the disease - the ulcers take on the appearance of cracks, pain appears, radiating from the mouth to different parts of the head. There are cases when the patient does not feel pain at this stage.
- An advanced form is the active phase of cancer, when lesions spread quickly. Associated symptoms are also noted: pain in the mouth, difficulty swallowing food, a sharp decrease in body weight, and a change in voice.
Etiology
So far, the root causes that could affect the formation of tumors on the oral mucosa have not been identified, but doctors suggest that people who suffer from bad habits, drink alcohol, and smoke are susceptible to the development of pathology. The disease can also occur in a person who does not watch their diet, eats spicy food, does not visit the dentist on time, suffers from chronic pathologies of the gastrointestinal tract, or has had a viral infection such as herpes.
If tumors form on the oral mucosa of a child, the cause may be intrauterine pathologies that are associated with genetic abnormalities. Neoplasms of this etiology appear in the first year of a baby’s life, and if parents notice a suspicious growth in the baby’s mouth, it is worth visiting a doctor and consulting about treating the problem.
Classification
According to its microscopic structure, cancer of the oral mucosa is of the squamous cell type. There are several of its forms:
- Keratinizing squamous cell carcinoma. It looks like a cluster of keratinized epithelium (“cancer pearls”). Accounts for up to 95% of cases of development of pathology of this localization.
- Non-keratinizing squamous cell. It is manifested by the proliferation of epithelial cancer cells without areas of keratinization.
- Poorly differentiated (carcinoma). This is the most malignant and difficult to diagnose form.
- Cancer of the oral mucosa in situ. The rarest form.
Depending on the characteristics of tumor growth, the following forms are distinguished:
- An ulcer is one or more ulcers that gradually grow and tend to grow and merge. Usually the bottom of the ulcers is covered with an unpleasant-looking coating.
- Nodular - characterized by the appearance on the mucous membrane of a dense growth in the form of a node, covered with whitish spots.
- Papillary - manifests itself as fast-growing, dense growths resembling warts. The growths are usually accompanied by swelling of the underlying tissues.
Certain forms of cancer of the oral mucosa
- Tongue cancer. The typical location of the pathology is the lateral surface of the tongue; less often, the tumor is found on the root of the tongue, the back or the lower surface. A malignant tumor already in the early stages leads to chewing and swallowing disorders, which facilitates diagnosis.
Photo: initial stage of cheek cancer
Cancer of the buccal mucosa. This tumor often masquerades as aphthous ulcers located along the line of the mouth on the cheeks. An increase in the diameter of the ulcer and its growth into the masticatory muscles leads to restrictions in opening the mouth, which is a typical symptom of cheek cancer.
- Cancer of the palate and gums of the upper jaw. A rapidly growing nodule with a tendency to ulceration forms on the palate. Early onset of pain may occur, especially in situations where deeper tissues are affected.
- Cancer of the mucous membrane of the floor of the mouth. The first signs of the disease almost always go unnoticed. The tumor grows early into the surrounding tissues, including bone. The oncological process is often accompanied by increased salivation (salivation), and the development of bleeding is dangerous. The growth of a tumor affecting the bone tissue of the lower jaw is accompanied by facial deformation.
- Cancer of the mucous membrane of the alveolar processes. At an early stage, it is accompanied by problems with teeth - patients are bothered by toothache, teeth become loose and fall out, and gums become swollen. A typical phenomenon is bleeding from the socket of a fallen tooth.