Second degree of purity
In this case, leukocytes in the smear (the norm for women is 1-3 per field of view) may be completely absent.
Sometimes the laboratory technician notes the presence of single white bodies. This suggests that there is no inflammatory process in the examined areas. In addition to leukocytes, lactobacilli and other microorganisms are present in the vagina. The following indicators fall into this category. The laboratory technician detects leukocytes in the smear (the norm in women is exceeded, there are up to 15 of them in the field of view). In addition, beneficial microorganisms and bacteria are present. In some cases, the number of the latter may be reduced. Most often, such indicators are considered normal.
In this subspecies, leukocytes are also detected in the smear. The norm for women before or after menstruation (with the third degree of vaginal cleanliness) is exceeded (up to 50 units). At the same time, additional indicators can also often be overestimated or underestimated.
In this case, the woman requires treatment. Since such a large number of white cells indicates the presence of an inflammatory process.
This subgroup is the last. When examining the material, leukocytes are determined in the smear. The norm in women after menstruation or before them with vaginitis is exceeded (more than 50 units). Pathological indicators of additional cells are also noted. Most often, bacteria and fungi are present in this case.
A woman with fourth degree purity always needs treatment. Most often, the pathology is caused by a sexually transmitted infection.
A smear on the flora in women (the norm in the table above is used as an international standard) is the basis for determining the degree of vaginal cleanliness. There are 4 degrees in total.
| Purity level | Characteristics of the smear | Meaning | |||
| leukocytes | epithelium | slime | microflora | ||
| 1 | single | 5-10 in sight | moderate amount | pH – sour, Doderlein sticks – no less than 95% | ideal state of microflora |
| 2 | up to 10 in view | 5-10 in sight | moderate amount | pH – acidic, presence of a small number of gram-positive cocci, Doderlein rods – predominate | normal state of microflora, found in the vast majority of women of reproductive age who are sexually active |
| 3 | 10-30 in sight | more than 10 in sight | moderate to large amount | pH - neutral or slightly alkaline, presence of gram-negative and gram-positive cocci, Doderlein rods - in small quantities or absent | inflammatory process in the vagina (colpitis), requires treatment even if it is asymptomatic |
| 4 | more than 30 in the field of view, or entirely | completely | a large number of | pH – alkaline, a large number of opportunistic and pathogenic bacteria, no Doderlein bacilli | severe inflammatory process requiring immediate treatment |
Thus, a woman need not worry about her health only if the degree of cleanliness of her vagina is 1 or 2. Grades 3 and 4 are signs of pathology and require treatment.
0-10 in the field of view - Normally, the presence of single leukocytes in the vagina and on the surface of the cervix is allowed.
Leukocytes more than 15 in the field of view, epithelium more than 10 - an increase in the number of leukocytes, a large amount of epithelium indicates the presence of an inflammatory process in the vagina.
Decoding the results of men
In the results of a smear for flora in men, the number of leukocytes should normally be from 0 to 5 in the field of view, epithelium from 5 to 10 in the field of view , cocci are present in a single amount , mucus in a moderate amount, and trichomanadas, gonococci, and fungi are absent.
Deviations from the above norms indicate a pathological process or inflammation. Leukocytes are one of the main indicators that indicate to the doctor the degree of inflammation and pathology of the organs of the urogenital tract. They may be elevated in the following diseases:
- specific or nonspecific urethritis;
- prostatitis;
- urolithiasis disease;
- the presence of benign and malignant neoplasms;
- stricture (narrowing) of the urethra.
An increase in the epithelium also indicates an inflammatory process or urolithiasis, and the detection of cocci approximately higher than 4-5 in the field of view means the presence of acute or chronic nonspecific urethritis caused by opportunistic bacteria. of mucus also indirectly indicate inflammation, but with normal other indicators it can indicate sluggish urethritis or prostatitis.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
of gonococci, trichomands, and Candida fungi in the analysis indicates specific urethritis and, accordingly, the diseases of gonorrhea, trichomoniasis, and candidiasis . In any case, the doctor must take into account all the indicators of the smear for the purpose of further diagnosis and treatment.
Flat epithelium
No more than 10 were found in the field of view - Normally, squamous epithelium is present in the smear, since these cells are constantly renewed and exfoliated.
Found in large numbers, more than 10 in the field of view - An increase in the number of epithelial cells in the smear is a sign of an inflammatory process in the vagina.
Not detected - In the absence of epithelium in the smear of the vagina and cervix, it can be assumed that the woman’s hormonal levels are disrupted, and there is an insufficient amount of estrogen. This is also an indirect sign of atrophy of the vaginal mucosa.
Staphylococcus aureus, cocci
Not detected – Normally, the absence of foreign flora is a sign of a high degree of vaginal cleanliness.
Less than 10 were found in the field of view - a single number of extraneous opportunistic microorganisms is normal, if there are no signs of inflammation.
More than 15 were found in the field of view, the entire field of view, leukocytes above 15 in the field of view - The presence of a large number of cocci, leukocytes, inflammatory cells (key cells) is a laboratory indicator of purulent inflammation in the vagina or cervical canal.
Not detected - normal
Detected - Gonococci detected in a smear in any quantity are laboratory confirmation of gonorrhea. Treatment with antibacterial drugs is necessary, including for the sexual partner.
Leukocytes in a smear for flora during pregnancy
When registering a pregnant woman, this test is always taken. The study is also carried out before childbirth. Leukocytes must be detected in the smear. The norm for women during pregnancy corresponds to the indicator of the first degree of vaginal cleanliness. Thus, during pregnancy, white cells should not exceed 1-3 in the field of view.
Some doctors allow normal values within 15 units. In this case, the woman’s microflora corresponds to the second degree. However, there are doctors who, in this case, insist on conducting additional research.
Large amount during pregnancy
Registration during pregnancy is accompanied by an examination by a gynecologist and a mandatory smear. In pregnant women, leukocytes are slightly elevated, so the norm will be 20 units for scraping from the cervix and 15 for taking material from the vaginal walls.
The main reasons for pregnant women, due to which the leukocyte count is moderately increased: decreased immunity caused by hormonal changes in the body and exacerbation of hidden gynecological diseases. If a woman’s leukocytes are elevated beyond the acceptable norms for pregnant women, this indicates pathological abnormalities.
Why are they increased?
White cells may be slightly elevated due to the fact that hormonal changes in a woman slightly disrupt the immune response and the activity of opportunistic microorganisms slightly increases. A relative increase in the leukocyte count is necessary to maintain the “purity” of the vaginal contents and suppress the activity of pathogenic and opportunistic microflora.
If there are a lot of leukocytes in a smear during pregnancy, then the reasons are the same as in non-pregnant women:
- inflammation of the reproductive system;
- allergic reactions;
- sexually transmitted diseases (gonorrhea, syphilis, ureaplasma);
- tumors (benign and malignant);
- candidiasis (thrush caused by a fungus of the genus Candida).
But you shouldn’t immediately suspect a terrible pathology. During pregnancy, a woman may experience slight leukocytosis in a vaginal smear under the influence of external factors:
- rubbing the perineum with tight, uncomfortable underwear;
- rough sex accompanied by vaginal microtraumas;
- frequent douching;
- nervous tension and fatigue.
In a pregnant woman, if leukocytes are elevated in a smear, what this means can only be determined after analyzing her lifestyle and additional examination. If the pathology is confirmed, then the drugs for the pregnant woman are selected so as not to harm the fetus and suppress the pathological process.
What is the threat?
A vaginal infection is relatively harmless for a woman’s life, but pathogens can enter the pregnant uterus and infect the fetus. This will lead to a number of complications:
- infectious processes will disrupt the full development of the child;
- pathogenic microorganisms will cause intrauterine fetal death.
In the first case, a baby is born with abnormalities, the severity of which depends on the degree of developmental disorder in the mother’s womb. And in the second case, the pregnancy either freezes (the dead fetus remains in the uterus) or a stillborn child is born.
Elevated white blood cells in a smear can disrupt the full development of the child
Sticks (Doderlein)
Not found, cocci, gonococci, trichomonas, fungi, leukocytes more than 15 - the absence of bacilli is a sign of a severe disorder of the vagina, severe inflammation, with the displacement of vaginal lactobacilli by the pathogenic flora.
Found in small quantities, cocci, gonococci, trichomonas, fungi, leukocytes more than 15 - An insufficient number of bacilli is a sign of a severe disorder of the vagina, severe inflammation, with the displacement of vaginal lactobacilli by the pathogenic flora.
95% of all bacteria – The natural microflora of the vagina is normally 95% or more bacteria.
Not detected - there should normally be no E. coli in the vagina
Detected, leukocytes more than 15 in the cell. – Escherichia coli in the vagina can be a component of opportunistic flora, and enter the vagina from the intestines. In the presence of a large number of leukocytes, and the absence of other infections, E. coli in the smear is considered the causative agent of the inflammatory process.
Found in single quantities - E. coli in the vagina can be a component of opportunistic flora, and enter the vagina from the intestines. If there are no complaints, no treatment is required
Normal indicators during pregnancy, menopause, after cesarean section
When researching, pay attention to such indicators as:
- slime;
- epithelial cells;
- key cells;
- microflora;
- yeast fungi;
- Trichomonas;
- gonococci.
For the vagina, cervix and urethra, the indicators will be different. An ideal analysis is one in which there are sufficient quantities (++++) of gram-positive rods (only in the vagina, neither in the cervix, nor in the urethra). Mucus may be present in the cervix and vagina, but in small quantities.
White cell norm:
- in the vagina – 0-10;
- in the cervix – 0-30;
- in the urethra – 0-5.
Epithelial cells may be present everywhere, but no more than 10 units per field of view. All other indicators must be negative. During pregnancy, elevated white blood cells may be a consequence of changes in the body, therefore, if this indicator was detected in an amount of up to 20 units, there is no need to worry.
During menopause, a woman’s body undergoes significant changes, therefore, for this age, the usual interpretation of the analysis is no longer relevant, and the norms will differ slightly from the generally accepted ones.
Changes in the level of leukocytes are affected by changes in vaginal acidity. If the acidity is below the permissible norm - 4.4, then pathogenic microbes begin to become active and, accordingly, the level of leukocytes increases. Sometimes a poor analysis may be due to an infection or disease that has entered the body, such as vaginitis (nonspecific), vaginosis (bacterial), gonorrhea, candidiasis.
In a healthy woman who has recently given birth, the material taken from the genital organs should not contain more than 10 units of leukocytes, and from the cervical canal - 30 units. The method of delivery, natural or by cesarean section, also affects laboratory parameters.
If after a natural birth the indicators are significantly higher than normal, this may indicate infection during childbirth or pieces of the placenta remaining in the uterus. After a cesarean section, an increase in the number of white blood cells in the tests is considered normal. But if, after a week, they have not returned to normal, then anti-inflammatory therapy is prescribed.
Reasons for deviation of smear results from the norm
Biomaterial samples for analysis are taken from various tissues - the vaginal mucosa, urethral and cervical (cervix) canals. Even in the absence of pathological symptoms, such a control diagnosis should be carried out in women who are sexually active - annually. In addition, the following factors are indications for taking a smear in women:
- changes in the color, odor and structure of vaginal discharge;
- discomfort when urinating;
- manifestation of itchy symptoms in the groin area;
- burning sensation and soreness in the urethra and vagina;
- pain in close intimate relationships;
- causeless abdominal pain
- disruptions in the cyclicity of menstruation.
It should be remembered that a long course of antibiotic therapy leads to the death of many beneficial microorganisms, which are quickly replaced by “aggressive inhabitants” (pathogenic flora). This may distort the analysis results. Therefore, it is advisable to carry out this diagnostic procedure after finishing taking antibiotics.
To avoid distortion of data in smear analysis, the procedure for collecting biomaterial should be taken seriously. Because many factors can provoke the detection of leukocyte cells in smears, in the complete absence of pathological processes, or, on the contrary, exclude their presence in the tests, in the pronounced presence of pathology. Preparatory measures include:
- Avoid intimate relationships for 3 days before collecting biomaterial.
- Seven days before the test, you should avoid taking various medications (suppositories, tablets and external medications, solutions for washing the vagina and injections).
- Before taking smears, in the next two days, it is not recommended to use soap or gels for intimate hygiene, using only slightly warmed water for this purpose. The last wash should be done on the eve of the upcoming day of the procedure.
- The last act of urination should be 3 hours before the procedure.
The test is not done during menstruation unless there are urgent circumstances. A good period for taking samples is 7 days before the start or 2-3 days after the end of your period.
An important criterion for a diagnostic indicator is the number of leukocytes in a smear. It can suggest the development of various inflammatory reactions in the body. Because it is precisely in the inflammatory foci that a large number of white cells tend to get into, creating a protective barrier for the body.
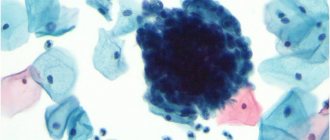
However, during the process of phagocytosis, white cells are destroyed and their morphological composition changes. Such cells are called neutrophils. The greater the number of them found in the samples, the more pronounced the inflammatory reaction. Along with leukocytosis, the quantitative composition of other elements changes - beneficial and pathogenic microorganisms, mucus, epithelial and formed elements, the level of vaginal acidity.
It is the collection of leukocytes with additional inclusions in smears that makes it possible to accurately diagnose the pathological process. For example: fungal flora will be present in samples for vaginal candidiasis, coccal flora - for purulent-inflammatory pathologies (gonorrhea or vaginosis). With uterine endometrium or colpitis, tests show staphylococcus and decrease vaginal acidity.
The fact that during menstrual flow the concentration of leukocytes may change due to hormonal influences is also taken into account. And in the absence of large changes in the level of leukocytes, this is considered a physiological process and not a pathology. The final diagnostic verdict is based on the presence of all additional criteria.
Normally, leukocytes are constantly present in women’s smears, and the leukocyte smear norm itself is a rather arbitrary concept. Because in different intimate areas of the female body their level of permissibility varies. Most leukocytes are found in the cervical canal (uterine cervix) - up to 30 cell units in the visual field of the microscope. And the smallest amount is in the urethra, up to 5 units.
In a healthy body, in the absence of pathological processes, the table of norms of leukocytes in smears in women will show that the cervical and urethral canals are sterile and do not “carry” pathological flora. As for the vagina, small fluctuations in the standard parameters are acceptable. Its sterility - the degree of purity, depends on the introduction of different flora.
No woman can have a completely flawless smear, without leukocytes and bacteria in the vagina. Often, smears of vaginal discharge may contain up to 10 leukocyte units, a few epithelial cells and various bacterial microorganisms. Such indicators are not considered a manifestation of pathology and are counted as the normal limit. But sterility in this case has the 2nd degree of vaginal purity.
If coccal, yeast or anaerobic flora is detected in the vaginal discharge, and a quantitative decrease in lactobacilli and bifidobacteria is noted, this is an indication for a more in-depth diagnostic study. At the same time, the number of leukocytes in the smears significantly exceeds the norm, and large quantities of mucus are detected - this indicates the development of a strong inflammatory reaction.
With such indicators, the sterility of the vagina has the 3rd degree of purity.
The last degree of sterility - 4th - includes conditions in which a very slight presence or complete absence of lactobacilli is noted in the test smear. And the level of leukocyte cells is so high that they fill the entire field of view, and the amount of epithelium and mucus increases.
Table of leukocyte norms in a woman’s smear
| Indicators | V | C | U |
| Leukocytes | 0 — 10 | 0 — 30 | 0 — 5 |
| Flat epithelium | 5 — 10 | 5 — 10 | 5 — 10 |
| Slime | Moderately | Moderately |
When an excess of leukocyte cells is detected in a smear in women, the cause is always associated with inflammatory reactions in the body. By their concentration one can judge the clinical severity of the inflammatory process. But an assessment of the reason for the presence of leukocytes in a smear is always carried out in conjunction with other diagnostic aspects.
Eg:
- An increase in the amount of mucus in the discharge is evidence of the development of an infectious process. In this way, the body tries to get rid of pathogenic flora.
- An increased concentration of epithelium, as well as leukocytes, indicates the presence of inflammatory diseases.
- The key indicator in diagnosis is bacterial sand - epithelium covered with gardnerella. Its detection in smears is a sure sign of the development of vaginal gardnerellosis.
- An indicator of a reduced number of lactobacilli appears against the background of antibiotic therapy or infectious diseases. A decrease in their concentration in the body leads to a decrease in vaginal acidity and creates conditions for the development and growth of bacterial flora, manifestations of gonorrhea, thrush, trichomoniasis.
Infectious and inflammatory processes in women are always accompanied by leukocytosis in the examined smear. The reasons for elevated white blood cells in smears are due to many factors:
- various inflammatory pathologies such as andexitis and endometritis, urethritis and cervicitis or colpitis;
- tumor neoplasms;
- vaginal and intestinal bacterial imbalance;
- autoimmune disorders;
- hormonal disorders;
- stress and chronic fatigue;
- too aggressive sex.
Deviations from normal parameters also occur in the other direction, when leukocytes are not detected in smears at all, or they are present in very small quantities. With such a diagnosis they don’t talk about good health.
As a rule, such deviations are typical for women in menopause or who have “consigned their intimate life to oblivion.” They are fraught with dangerous consequences. Regular medical monitoring and restoration of intimate relationships are desirable. Simply put, the root of all problems is lack of sex.
Leukocytosis in smears during pregnancy is caused by a purely physiological factor - hormonal changes that give impetus to large hormonal secretion. Under the influence of hormones, active reproduction of lactobacilli begins, affecting the acidity of the vagina. In particular, it increases it, which prevents the proliferation of pathogenic microorganisms, but promotes the accumulation of leukocyte cells.
At the same time, their number in smears will be increased to 20 units. In this condition, this level of white cells is considered the physiological norm. Another reason for leukocytosis in pregnant women in smears is due to a decrease in immune functions, which is inherent in the female body at the genetic level. To avoid activation of phagocytosis against the fetus, which can cause its rejection.
But this property opens up the possibility of activating latent, asymptomatic infectious diseases and the penetration of pathogenic flora into the body, manifested in smears by an increased level of leukocyte cells. In such cases during pregnancy, a thorough examination of the woman and immediate treatment are required. The infection, having penetrated upward into the uterus, can infect the fetal fluid and the baby itself, which can lead to miscarriage or early birth.
If the number of leukocyte cells in the smear is no more than 20, all other indicators correspond to the standard, and the expectant mother does not show pathological signs, there is no reason to worry. But it is important to note that at the same time, the leukocyte norm for the urethral and cervical canals should not change.
Changes in the normal concentration of leukocytes in the test smear are not a disease or even a symptom, as many believe. This is only an indicator for further detailed and in-depth diagnostics (bacteriological, serological or immunological) to identify the true cause.
Tags: analysis women's health
So, now you know the quantity of leukocytes in a smear (the norm in women). The norm is not always absolute. It is worth noting that the third and fourth degrees of vaginal cleanliness are a deviation from generally accepted values. Treatment in this case must be carried out after additional research. There are several reasons why there is an increase in white blood cells in the vagina, cervical canal or urethra.
The role of cells in the body
Not detected – Normal
Detected leukocytes above 15 in p.z. – Atypical cells, key cells, are cells of the epithelium and small rods – gardnerella – glued together. The presence of these cells indicates hardrenellosis - bacterial vaginosis. Typically, the presence of a large number of gardnerella is manifested by an unpleasant odor from the vagina, similar to the smell of spoiled fish.
The process of destruction of foreign and dangerous elements by leukocytes is called phagocytosis. They capture and absorb “enemies”, then die themselves.
What are leukocytes in a smear in women?
Their main functions:
- Production of antibodies to fight external and internal “enemies”.
- Normalization of metabolic processes and supply of tissues with necessary enzymes and substances.
- Cleansing the body - eliminating pathogens and dead leukocytes.
Candida
Not detected – Yeasts should not be present in the normal vaginal microflora.
Candida was detected above 104 CFU/ml, leukocytes more than 15 in the field of view, squamous epithelium more than 10 in the field of view. – The presence of yeast-like fungi is a manifestation of candidiasis (thrush), or a concomitant laboratory indicator for inflammatory processes in the vagina. Candida is found as an opportunistic flora, and often accompanies viral infections of the cervix and vagina, STDs.
Drug treatment
Treatment is prescribed depending on the nature of the disease detected - inflammatory or infectious.
Inflammatory processes are treated according to the following scheme:
- Antiseptics for douching - “Potassium Permanganate”, “Miramistin”, “Chlorhexidine”;
- Antibiotics - “Pimafucin”, “Genferon”, “Viferon”, “Terzhinan”.
If the patient’s poor health is due to the presence of thrush, then “Flucostat” or “Fluconazole” is prescribed for its treatment.
Infectious processes are treated according to the following scheme:
- Antibiotics (intravenously) - “Ciprinol”, “Ornidazole”, “Metronidazole”;
- Prebiotics (prevention of dysbacteriosis) - “Laktovit”, “Bifidumbacterin”, “Linex”, “Lactofiltrum”, “Yoghurt”.
Doctors, as a rule, prescribe drugs not only for treatment, but also to increase immunity:
- "Immunal";
- Echinacea tincture;
- Eleutherococcus;
- Ginseng tincture.
Why is a flora smear prescribed in gynecology?
A smear on the flora in women (the norm is given in the table below) is prescribed to diagnose infectious and inflammatory processes and changes in hormonal levels.
Clear indications for conducting a microflora study are:
- pathological leucorrhoea;
- the presence of itching and burning;
- the appearance of an unpleasant odor;
- feeling of dryness and discomfort;
- pain and bleeding during intimate relationships;
- pain and pain when urinating.
It is mandatory to examine the microflora of the genital organs several times during pregnancy and upon admission to the maternity hospital. The analysis is also indicated before any gynecological operations and manipulations (colposcopy, IVF and others).
In addition, a smear on the flora is the simplest method to detect the presence of sexually transmitted diseases. Therefore, for the purpose of early diagnosis of STDs in the case of unprotected sex with an unfamiliar partner, it is also recommended to conduct an analysis, even in the absence of symptoms.
If a woman has no complaints or special indications, it is performed 1-2 times a year as part of routine gynecological screening.
When to see a doctor
Symptoms for which you should definitely consult a doctor are:
- Discomfort and pain when urinating;
- Itching, burning;
- Weakness, lethargy;
- Loss of appetite;
- Redness of the genitals;
- Discomfort or pain during sexual intercourse;
- Nagging pain in the lower abdomen;
- Discharge (sometimes with an unpleasant odor).
The presence of certain symptoms depends on what bacteria are detected.
Preparation for delivery
Preparation for microflora analysis involves some restrictions a few days before the examination. All types of douching and the use of any vaginal products: suppositories, creams and intimate deodorants are prohibited.
Taking sitz and lying baths, as well as intimate hygiene using soap or special gels, is not allowed. In addition, you should refrain from intimate relations, including using a condom.
1-2 hours before the test, you should thoroughly wash yourself with warm boiled water without soap and dry your genitals with a clean towel. After this, do not urinate until a smear is taken.
The analysis is taken no earlier than 2 days after the end of menstruation, and no later than 2 days before the start of the next one, ideally from 10 to 20 days of the cycle.
Preparation for flora analysis
A smear to study the flora is the fastest and most accessible way to determine infectious diseases and inflammatory processes for both sexes. In this regard, it makes sense to understand the terms in more detail in order to understand the entries in the form.
- do not have sexual intercourse for several days before the study, and also avoid douching, vaginal suppositories and other local interventions;
- the analysis cannot be carried out during menstruation, since the blood will not allow sufficient viewing of the material;
- calculate your fluid intake on the day of the test so that you go to the toilet for the last time to urinate 3 hours before the test;
- do not take any medications (tablets, injections, etc.) 10 days before the test;
- Do not use hygiene products on the day of analysis. It is advisable to use warm boiled water in the morning on the day of the test for women, and for men in the evening before the test.
Men should be prepared for the fact that the collection of the analysis itself is not a pleasant procedure and may be accompanied by uncomfortable sensations even a couple of hours after it is carried out.
In the smear itself from the male urethra, if the subject is healthy, everything is much simpler than in women. And let this moment bring a little peace to men who have undergone such an unpleasant procedure.
- leukocytes – up to five cells in the field of view;
- flora – the presence of single rods;
- urethral epithelium - diluted with a general background of a transitional nature, from five to ten cells in view;
- small amounts of mucus;
- conditionally pathogenic flora in the smear – single microorganisms (staphylococci, streptococci, etc.). If there is a need to differentiate the flora, a Gram smear is used.
READ MORE: The result of cervical cytology is inflammation.
If there is an inflammatory process, the smear changes its picture:
- leukocytes – a rich picture;
- rod flora is replaced by cocci or cocco-bacillary flora;
- the presence of microbes (yeast, Trichomonas, etc.);
- for correct diagnosis and accurate determination of the type of pathogen, additional research is carried out using a culture or PCR method (under a microscope it is practically impossible to detect chlamydia, mycoplasma and ureaplasma, and also to distinguish diplococci that cause gonorrhea from enterococci, streptococci);
- Rarely, it is possible to detect E. coli in a smear from the urethra of men. This indicates a complete lack of hygiene. E. coli, which is useful in the intestines, can cause cystitis, prostatitis, urethritis and other diseases if it enters the male urethra. More research is also needed to distinguish E. coli.
You should prepare for the procedure, since some factors lead to false test results - detection of leukocytes in the absence of diseases, or vice versa.
Preparation for taking a smear is as follows:
- Refusal of sexual intercourse 3 days before visiting the doctor;
- Stop taking medications of any form (tablets, suppositories, douching, injections, ointments) a week before the study;
- For 2 days before the analysis, neither soap nor gel should be used for hygiene of the external genitalia - only warm water, and the last intimate toilet is carried out the night before;
- 3 hours before the test you should not urinate.
The analysis is taken in the first days after the end of menstruation or before its onset, however, in emergency cases, scraping is done at any time. What rules must be followed when preparing? A woman should:
- refuse intimate contacts three days before taking a sample;
- stop taking any medications a week before the tests - including diuretics;
- stop using hygiene products for washing the genitals two days in advance - you should wash only with warm water;
- refrain from urinating for three hours before taking the sample.
You should also not douche a couple of days before taking a smear. When visiting a doctor, you need to wear fresh, pure cotton underwear; your genitals should be washed with warm water without hygiene products.
The tests are ready in about 2-3 days. In paid clinics, results can be obtained within a few hours. If tests reveal an increased number of white blood cells, a diagnosis for a hidden disease is prescribed.
It is necessary to prepare correctly for taking the analysis. There are some preparation rules, it is important to follow them so that the results are correct.
If you are menstruating, you should postpone your visit to the doctor. During menstruation, smears are not taken, since no pathological abnormalities will be visible among the red blood cells; blood has an antimicrobial effect.
Before taking the test, you do not need to thoroughly wash your genitals; it is important that the flora remains natural. You are only allowed to wash with soap; you cannot use gels, shampoos or special products.
It is worth refraining from urinating for several hours before going to the gynecologist. Before taking a smear on the eve of the test, you should not use suppositories, ointments or tablets. You should not take a bath or douche before the test.
By following all the recommendations for preparing for the test, you will be able to see the correct results and will not have to take the smear again.
In order for the analysis results to be as reliable as possible, the woman must prepare for the study. She should refrain from sexual intercourse the day before the visit to the gynecologist, not use vaginal suppositories and pills, and not douche.
The smear reflects the composition of the microflora of three anatomical areas: vagina, cervix, urethra. To collect biological material, only sterile instruments are used:
- bacteriological loop;
- gauze swab;
- putty knife.
The scrapings are placed on slides, which are dried, stained and examined under a microscope.
The number of leukocytes is determined primarily by simple counting. Normally, their content should be small, directly in the cervical canal from 0 to 30.
It is optimal to do a smear for cytology after the end of menstruation and before the middle of the next menstrual cycle.
— Refrain from sexual contact. — Do not use vaginal products (suppositories, creams, gels, etc.). — Do not douche.
- Biomaterial is collected using sterile disposable instruments.
1. The patient undresses to the waist and lies down in the gynecological chair.
2. To visualize the cervix, the doctor uses a Speculum speculum.
It is rational to take scrapings for histology under colposcopy control.
3. The doctor inserts a cervical brush into the cervical canal to a depth of 1.5-2 cm, takes a sample of endocervix tissue and places (imprints) it on a prepared glass slide with appropriate markings.
4. Then, using an Eyre spatula, scrape from the junction (from the transformation zone) of the epithelium and place it on the designated part of the first slide or on the second glass.
5. If necessary, with another spatula, the doctor makes a targeted scraping from the suspicious area of the ectocervix and places the taken biomaterial on another glass with the appropriate marking.
6. Smears are immediately treated with a fixative, dried and sent for examination.
7. In the laboratory, first of all, the adequacy of the cytological smear is assessed: - are there enough cells on the glass for analysis; — is the biomaterial applied too thin/thick;
- Satisfactory quality of the biomaterial (adequacy of the smear) is a key factor in the effectiveness of smear analysis for cytology for decoding.
If your doctor asks you to retake the PAP test, don’t be alarmed. Practice shows that up to 20% of smears are not performed adequately and must be repeated.
READ MORE: Cervical cytology - what is it, explanation
The procedure for taking a smear is short-term, low-traumatic, safe and in most cases painless. Sometimes the patient may feel mild, transient discomfort.
How to behave after the procedure: - Refrain from sexual contact for 1-2 days. — Otherwise, lead a normal life. — If necessary, the doctor gives individual recommendations.
Contraindications to cytology: - Acute genital infection (itching, profuse, purulent, with a strong odor, foamy vaginal discharge). - Pregnancy. - Virginity. - Menstruation.
For minor patients who are sexually active, cervical scraping is done in the presence of their parents (guardian).
How is it surrendered?
A smear on the flora in women, the norm in the table for which will be presented later in the article, is taken strictly before a manual examination, colposcopy and ultrasound with an intravaginal sensor.
The patient is positioned on a gynecological chair. The doctor inserts a special speculum into the woman’s vagina and then, using a sterile Volkmann spoon, takes material from the surface of the cervix and the posterolateral vault of the vagina.
After this, a sample is taken from the external opening of the urethra for analysis using a sterile loop. The gynecologist applies the resulting materials onto separate glass slides and sends them for examination to the laboratory. A smear is taken from virgins without the use of a dilator through an opening in the hymen.
The test collection procedure takes a few minutes and is absolutely painless. The exception is situations in the presence of a strong inflammatory process, but even in these cases the discomfort when taking smears is minimal.
Diagnostics and medical assistance
Despite the high information content of microflora analysis, it does not allow diagnosing:
- Pregnancy. To diagnose it, it is necessary to take a blood test for hCG (human chorionic gonadotropin) and perform an ultrasound of the pelvic organs.
- Viral infections (HIV, papillomavirus, herpes, chlamydia, ureaplasmosis, mycoplasmosis). An HIV test is performed using venous blood ELISA; other infections are performed using a urogenital smear using the PCR method.
- Cancerous and precancerous conditions of the studied tissues. Assessment of the presence of atypical or cancer cells is carried out through a cytological examination (oncocytology or PAP (PAP) test), as well as examination using a colposcope.
If an increased level of leukocytes is detected in the smear, you should consult a doctor:
- Gynecologist.
- Dermatovenerologist.
- Infectious disease specialist.
The doctor chooses the treatment method based on laboratory tests. To establish an accurate diagnosis, additional diagnostics are prescribed.
https://www.youtube.com/watch?v=o94ikVJc6L0
The following types of diagnostic procedures are most often prescribed:
- sowing on flora;
- flora smear;
- ELISA (enzyme-linked immunosorbent assay);
- test for antibodies in the blood;
- biopsy;
- PCR (polymerase chain reaction);
- CBC (complete blood count);
- OAM (general urinalysis);
- Ultrasound of the abdominal cavity.
Treatment for pathology in microflora
According to laboratory tests, a diagnosis is made and treatment is prescribed.
One smear will not be enough to diagnose the patient. She will have to donate blood, urine, and have a pelvic ultrasound. Only after the collected tests will the doctor be able to make a diagnosis. Depending on the severity of the infection and the disease itself, antibiotics, anti-inflammatory and antibacterial drugs may be prescribed. If the norm of leukocytes has been disturbed by dysbiosis or sexually transmitted infection, then the course of treatment always lasts two to three weeks.
In some cases, longer therapy may be required. Inflammatory processes in a woman’s genital organs can lead to infertility and ectopic pregnancy.
Doctors often prescribe not only drug therapy, but may also recommend folk remedies. They also contribute to the rapid normalization of leukocytes:
- Douching is carried out with a decoction of herbs (chamomile, calendula, nettle), you can choose any of the herbs given.
- Garlic cloves (6 pieces) are poured with boiling water and left overnight. Strain before use.
In addition, they are prescribed to take vitamins and medications to strengthen the immune system. But if the disease is cured, and the leukocyte count does not stabilize, they can conclude that the patient is experiencing frequent stress. She is recommended to go on vacation, to a resort, to the sea, where the woman’s emotional state will be restored.
Chronic stress depletes the entire body, its immune system is in very poor condition and cannot protect the body. The sea, high mountain nature, excess ultraviolet radiation will help restore the nervous system, strengthen the immune system and normalize the woman’s flora.
Reasons for deviation of smear results from the norm
The decoding of the received data should be carried out exclusively by a doctor. Self-diagnosis leads to a delay in adequate treatment, which can significantly worsen the patient’s condition and the severity of the disease, including death.
Normal (reference) values of leukocytes in the vagina and cervical canal are presented in the table.
| Criterion | Normal values | ||
| Vagina (V) | Cervix (C) | Urethra (U) | |
| Leukocytes | 0 — 10 | 0 — 30 | 0 — 5 |
| Flat epithelium | 5 — 10 | ||
| Slime | Slightly | Little or no | |
| Lactic acid bacteria (Lactobacillus ssp.) | Significant amount | None | |
| Yeast (Candida) | Single cells or absent | ||
| Pathogenic flora: Trichomonas vaginalis Neisseria gonorrhoeae Escherichia coli | None | ||
Viral infection
If a woman has caught a cold or caught a viral infection, then a slight increase in the number of white cells may be present on all mucous membranes. That is why it is worth warning the doctor about your illness or even rescheduling the test.
Sexually transmitted diseases
In the presence of gonorrhea, syphilis, trichomoniasis and other ailments, an increase in the level of leukocytes in the smear is observed. In this case, the number of white bodies will be large in all sources of material collection. In this case, it is worth taking additional tests and finding out what is the cause of the pathology.
Inflammation of the urinary system
In some cases, urinary tract infections can cause an increase in white blood cells in the smear. It is worth noting that the number of white bodies is increased only in the urethra. A normal number of white blood cells is determined in the vagina and cervix.
Inflammation of the uterus and appendages
Diseases such as endometritis, adnexitis, salpingitis and metritis can increase the level of leukocytes. Most often, pathology is detected in the cervix and vagina. A urethral smear gives a normal white blood cell count.
It is worth noting that the more acute the inflammatory process, the greater the number of white cells will be detected. When the disease becomes chronic, the level of leukocytes decreases to normal values.
Poor hygiene
A pathological number of white cells can be detected when improper preparation for the test is carried out. If the genitals have not been washed, the number of bacteria may be higher. This is why it is so important to properly prepare for a visit to a gynecologist and undergo such tests.
| V | C | U | |
| Leukocytes | 0-10 in the field of view (during pregnancy up to 20) | 0-30 in sight | 0-5 in sight |
| Epithelial cells | 5-10 in sight | 5-10 in sight | 5-10 in sight |
| Slime | moderately | moderately | absent |
| Red blood cells | 0-3 in sight | 0-3 in sight | 0-3 in sight |
| Gonococcus | absent | absent | absent |
| Trichomonas | absent | absent | absent |
| Candida | absent | absent | absent |
| Key cells | absent | absent | absent |
| Microflora | Doderlein sticks in large quantities | absent | absent |
Minor deviations from these standards may be the result of improper preparation for the examination. But a significant increase in the content of leukocyte cells, especially in combination with an increased amount of squamous epithelium, red blood cells and mucus, indicates the presence of an inflammatory process.
If gonococci, trichomonas, yeasts and gardnerella are detected, the pathogen is identified, and the doctor will prescribe treatment immediately. But in cases of an inflammatory smear and a negative test for these infections, further examination is necessary to identify the pathogen.
1. In the vagina:
- femoflor screening (allows you to evaluate the bacterial composition of microflora using the PCR method);
- bacterial culture of a smear to determine the sensitivity of pathogens to antibiotics;
- smear for hidden infections (syphilis, mobiluncus, ureaplasma, chlamydia).
2. On the cervix:
- Papanicolaou smear (PAP test) or oncocytology of the cervix;
- colposcopic examination of the cervix
3. In the urethra:
- consultation with a urologist;
- general urine analysis;
- bacterial culture of urine.
An increase in white blood cells in a smear in women is a sign of an inflammatory process in the body.
You can find out their level by taking tests:
- flora smear;
- blood analysis;
- Analysis of urine.
Women are most often prescribed a smear test for flora.
This study allows you to identify diseases of the urinary canal, kidneys or bladder; recognize the inflammatory process in the urogenital area.
Material for research is taken:
- from the vaginal wall;
- from the mucous surface of the cervix;
- from the mucous membrane of the urethra.
Normal levels of immune cells in a smear:
- from the vagina - no more than 10;
- from the urethra - no more than 5;
- from the uterine cervix - no more than 15.
During the study, it is necessary to take into account the following features:
- The number of white blood cells (leukocytes) increases after sexual intercourse; elevated levels last for 24 hours after the act.
- Increased levels are observed during the installation of an intrauterine contraceptive device.
- Microtraumas of the vaginal walls also increase the indicators.
The main reasons for an increase in the number of leukocytes in a smear in women are:
- Sexual infections transmitted directly during sexual intercourse (STIs):
- Gonorrhea.
- Chlamydia.
- Ureaplasma.
- Syphilis.
- Trichomoniasis.
- Mycoplasma.
- Papillomaviruses.
- HIV.
- Candidiasis.
- Cytomegalovirus.
- Actinomycetes.
- Genital herpes.
- Bacterial vaginosis. This disease is better known as vaginal dysbiosis. Occurs when the number of pathogenic microorganisms in the vaginal flora increases.
Prerequisites for the development of the disease are hormonal disorders, decreased local immunity, or the use of vaginal suppositories.
- Allergic reaction to gels and lubricants for intimate hygiene or douching products.
- Oncological diseases of the reproductive system.
An increased content of white immune cells in a smear indicates the presence of the following diseases:
- Colpitis is an inflammatory process of the vaginal mucous tissues.
- Cervicitis is an inflammatory process of the cervical canal.
- Endometritis is an inflammatory process of the mucous surface of the uterus.
- Adnexitis is an inflammatory process of the ovaries and fallopian tubes.
- Urethritis is an inflammatory process of the urethra.
- Dysbacteriosis of the intestines or vagina.
- Oncology of the reproductive system.
Note: the reasons for an increased level of leukocytes in a smear in women are prolonged stress or depression.
Why is a smear taken and what does it show?
A gynecological smear for cytology or flora is a type of laboratory test that allows one to determine the bacterial components of the vaginal environment. Thanks to bacteriological research, the doctor finds out which pathogenic agents provoked the female disease and makes a diagnosis.
A smear at a gynecologist is prescribed for the purpose of:
- determining the state of the vaginal environment;
- identifying pathogens that cause sexually transmitted infections;
- determining what stage the inflammatory process is in;
- assessing the cleanliness of intimate places before undergoing the next diagnostic test or gynecological surgery;
- studying the condition of the expectant mother during pregnancy.
Using a gynecological smear, a doctor diagnoses many pathologies such as:
- Infections transmitted through sexual contact. The analysis shows the presence of increased levels of pathogens in the biological sample. We are talking about ureaplasma, mycoplasma, gardenella, gonococci, trichomonas and other microorganisms that cause illnesses.
- Inflammatory processes in the reproductive organs. We are talking about vaginitis, colpitis, cervicitis, endocervicitis. Pathology is indicated by the presence in the smear of an increased number of white blood cells called leukocytes.
- Vaginal dysbiosis caused by an imbalance of the vaginal microflora. With this problem, there is a decrease in the number of lactobacilli and an increase in the number of other microorganisms.
- Candidiasis, also called thrush. The analysis shows a sharp increase in the number of Candida fungi. In a biological sample taken from the vagina, the presence of pseudomycelium is observed. This indicates a fungal infection.
https://youtu.be/6684_AbF64I