Psoriatic arthritis is an inflammatory pathology that affects the joints. Its leading clinical manifestations are arthralgia, pain in the spine and muscles, the formation of plaques on the skin, subsequent deformation of the vertebral bodies, bone, cartilage joint structures. Treatment of psoriatic arthritis is conservative with the use of drugs from various clinical and pharmacological groups, physiotherapeutic measures, and exercise therapy.
Psoriatic arthropathy: what is it?
Psoriatic arthritis is a chronic disease that affects peripheral and, in some cases, larger joints.
The disease develops against the background of psoriasis, and sometimes is a harbinger of the appearance of a skin rash. People of all age categories are susceptible to the disease. The number of sick women does not significantly exceed the representatives of the stronger sex affected by the disease.
Patients often confuse the symptoms of psoriatic arthritis with signs of rheumatoid arthritis. In fact, the diseases listed above manifest themselves slightly differently. The symptoms of psoriatic arthritis, unlike the second disease, appear quite quickly.
It affects the interphalangeal joints, and then the metacarpophalangeal joints. Tissue lesions caused by psoriasis are more severe than those caused by rheumatoid arthritis.
Due to the similarity of symptoms, you should not make a diagnosis and choose a treatment option on your own. For this purpose, it is better to consult a doctor.
Treatment methods
To the question of whether psoriatic arthritis is curable, it is more correct to answer in the negative. However, modern advances in medicine help doctors prevent further progression of the process. In some cases, even partial restoration of joint function is possible.
How to treat psoriatic arthritis in a particular patient should be decided by the doctor after a full examination and medical history.
Drug therapy
For joint damage and psoriasis, treatment is not specific, it is aimed at:
- slowing down the progression of the disease;
- elimination of acute symptoms;
- normalization of the function of the musculoskeletal system;
- reduction of inflammatory and immune reactions.
The use of medications is the leading method of treating psoriatic arthritis. For this purpose, various groups of active substances are used.
Anti-inflammatory
Non-steroidal drugs (ibuprofen, diclofenac) are taken to reduce the manifestations of inflammation, as well as pain and associated mobility limitations. At the same time, the swelling in the area of the changes decreases.
Glucocorticosteroids
Hormonal medications can quickly eliminate the main symptoms of psoriatic arthritis. Since their systemic use poses a risk of developing negative reactions, they can be injected directly into the joint cavity.
Methotrexate
Methotrexate for psoriatic arthritis is the most commonly prescribed systemic drug. Despite this, there are still no definitive studies proving its effectiveness. The standard dose is 15-20 mg over a week. However, patients receiving such therapy should constantly monitor liver and kidney function. If significant deviations are detected, it is necessary to reduce the dose or completely discontinue the drug. When the spine is involved in the process and ankylosing spondylitis develops, methotrexate has low effectiveness.
Sulfasalazine
Sulfasalazine has anti-inflammatory and antibacterial effects and is often prescribed for rheumatoid arthritis. However, after recent clinical trials, this drug was approved for use in psoriasis. Sulfasalazine for psoriatic arthritis is usually prescribed in a dose of 2 g. It must be taken for a long time. But due to the presence of a large number of side effects, in particular from the intestines, as well as the lack of effectiveness in cases of damage to the spine, the question of prescribing this medicine should be decided on an individual basis.
Tumor necrosis factor inhibitors
In the treatment of psoriatic arthritis with drugs, the most effective drugs have been those that inhibit tumor growth (adalimumab, etanercept, infliximab). This therapy affects pathogenetic mechanisms, that is, it not only eliminates the symptoms of the disease, but also counters its main causes. The main inconvenience of this technique is the injection of the drug, but most patients are okay with this, as they feel a clear improvement in their condition.
Cyclosporine
Cyclosporine for psoriatic lesions is taken 3 mg per day. This drug slows down the changes that occur in bone and cartilage tissue, which is confirmed by x-rays.
Leflunomide
Leflunomide has a positive effect on the course of the disease, reducing arthralgia and swelling in the joints, and also slows down bone destruction. This undoubtedly improves the patient's quality of life. Take it at a dose of 100-20 mg per day.
Physiotherapy
Against the background of psoriasis, treatment of arthritis using physiotherapeutic procedures in some cases can be very effective. The most commonly used methods are:
- laser irradiation of blood;
- PUVA therapy;
- magnetic therapy;
- electrophoresis using glucocorticosteroids;
- phonophoresis;
- physical therapy.
Diet
Diet for psoriatic arthritis of the joints plays an important role in the treatment of the disease, as it helps to consolidate the results achieved through medication. A fairly significant condition for normalizing the condition is maintaining an alkaline environment in the body, since otherwise there is a high probability of developing an exacerbation of the disease.
Nutrition for psoriatic arthritis must be carried out according to the following rules:
- refusal of alcoholic products;
- exclusion of possible allergens, which is carried out on an individual basis;
- eating small portions;
- refusal of smoked foods, preservatives, spicy and salty foods;
- It is forbidden to eat citrus fruits;
- limited intake of easily digestible carbohydrates;
- increasing the volume of fermented milk products, cereals, vegetables, legumes;
- replace butter with vegetable oil.
At the same time, the diet for psoriatic arthritis should be low-calorie, since excess weight increases the load on the joints. This leads to increased pain, as well as deformation and the appearance of other symptoms. Since most physical activity is contraindicated in case of serious intra-articular changes, patients’ only chance to eliminate excess weight is proper nutrition.
Classification
Psoriatic arthritis can manifest itself in different ways, affecting the joints of different areas. For this reason, to simplify diagnosis and select prescriptions, experts have developed a separate classification, including possible variants of the disease.
Among the variants of the disease, the following types of illness are distinguished:
- arthritis of the distal interphalangeal joints . In this case, damage occurs to the joints located precisely in this zone;
- oligoarthritis and polyarthritis . In the first case, inflammation of one joint occurs, and in the second, the disease simultaneously affects more than five joints;
- spondyloarthritis (spondylitis) . With this type of disease, inflammation and decreased mobility of the spine occur;
- mutilating articular psoriasis . This disease is accompanied by the destruction of bone tissue, resulting in a decrease in the length of the fingers;
- symmetrical polyarthritis . The symptoms of this type of disease are very similar to those of rheumatoid arthritis.
In addition to the types of disease listed above, based on the characteristics of the development of the disease, three forms of the disease are distinguished: mild, moderate, severe.
Healthy hand and psoriatic arthritis
Experts also distinguish 4 stages of psoriatic arthritis:
- Stage 1 (the patient’s ability to work is maintained);
- Stage 2 (loss of performance occurs);
- Stage 3 (the patient’s mobility is impaired, as a result of which he cannot care for himself);
- Stage 4 (almost complete loss of mobility, which is accompanied by the death of muscle tissue).
Due to such a variety of variants of the disease, only a specialist can give the patient an accurate diagnosis.
Diagnosis of the disease
To make an accurate diagnosis if psoriatic arthritis is suspected, the doctor interviews and examines the patient, and also prescribes the following diagnostics:
- general and biochemical blood test;
- radiography;
- blood test for rheumatoid factor.
To make sure that the disease has not had a negative effect on the heart, an electrocardiogram is performed. If necessary, the doctor may prescribe arthroscopy and puncture. It is imperative to carry out differential diagnosis with Reiter's disease and ankylosing spondylitis, gout, infectious-allergic and rheumatoid joint damage.
Causes of joint damage in psoriasis
Psoriasis is an autoimmune disease in which the nervous system and immune system malfunction. In essence, the immune system acts as a protective shield that can provide a person with a reliable barrier against all kinds of harmful agents.
Ideally, the immune system destroys cells that are dangerous to the body, thereby maintaining health. With psoriasis, this system malfunctions, causing the body to attack and destroy its own cells.
The result is not only lesions on the skin, but also destroyed joints.
The described process may be aggravated by the following circumstances:
- excessive physical activity;
- constant feeling of stress (causes malfunctions of the immune system);
- trauma at an early stage of the disease;
- genetic predisposition;
- transferred infections of various nature.
In order to prevent the development of the disease, it is better to avoid negative factors or keep them under complete control.
Disease prevention
The primary prevention of psoriatic arthritis is only regular examination by a doctor if there is a history of cases of familial psoriasis. But you can prevent the exacerbation of inflammatory pathology in various ways.
Maintaining skin hygiene
Often, to prevent exacerbation of arthritis, it is enough to prevent skin clinical manifestations of psoriasis. To do this, you should use hygiene products without fragrances, preservatives, or stabilizers. Doctors recommend that patients with psoriasis use gel, soap, and foam intended for children when carrying out water procedures. They moisturize the skin well and do not cause irritation.
Diet
It is necessary to exclude nightshades, citrus fruits, legumes, sorrel, and fatty meats from the diet. You should avoid processed foods, fast food, coffee, and carbonated drinks, especially sweet ones. The daily menu of a patient with psoriasis should consist of lactic acid products, permitted fresh vegetables and fruits, lean meat, fish, and cereal porridges.
Rejection of bad habits
Ethyl alcohol, nicotine, and tobacco tar negatively affect not only all internal organs, but also the musculoskeletal system. When smoking and alcohol abuse, blood vessels, including coronary ones, are especially affected. Poor circulation further complicates the course of psoriatic arthritis.
Maintaining a daily routine
Adequate sleep, exercise therapy and gymnastics, and daily walks in the fresh air become an excellent prevention of joint pathology. Exercise therapy doctors also recommend that patients do swimming, yoga, water aerobics, and Pilates several times a week.
Adequate assessment of stressful situations
In group sessions with a psychotherapist, patients are taught to respond adequately to conflict situations in order to prevent stress or depression. They are the ones that most often act as factors that provoke relapses of psoriasis.
Symptoms of arthropathy
As a rule, symptoms of arthritis appear already when inflamed spots have formed on the skin. However, in about a fifth of patients, psoriasis begins with inflamed joints. The disease can manifest itself acutely or develop gradually.
Regardless of the nature of the disease, pathological processes are accompanied by the following signs:
- changes in the contours of joints and their deformation;
- the appearance of pain in the joints, which manifest themselves mainly not during movement, but at night, when the patient is sleeping;
- stiffness of diseased joints in the morning;
- staining of the skin at the site of inflammation in a burgundy color;
- the appearance of multidirectional dislocations (due to impaired elasticity and density of the ligaments);
- crunching knees;
- shortening of fingers.
For a more accurate diagnosis, it is better to consult a specialist.
It is quite difficult to recognize psoriatic arthritis and not confuse it with similar ailments without a medical education. But in most cases, the affected areas look the same.
The joint has an inflamed appearance, the skin in this area takes on a burgundy or rich pink hue, and the temperature of the skin in the affected area rises.
Symptoms and diagnosis of psoriatic arthritis
Psoriatic arthritis can occur at any age (even in children). It most often appears between the ages of 30-50 years. This disease affects both men and women equally.
Diagnosis and treatment of the disease in the early stages is very important for psoriatic arthritis. Many symptoms mimic other conditions or types of arthritis, so psoriatic arthritis can be misdiagnosed.
Changes in joints in psoriatic arthritis
Diagnosis of psoriatic arthropathy
To diagnose psoriatic arthritis, you need to see a rheumatologist. Typically, the following steps are performed to establish a diagnosis:
- Taking a blood test for rheumatoid factor
- X-rays of the joints, as well as the spine, if necessary, are necessary
- You also need to be examined by a dermatologist to diagnose psoriasis and prescribe treatment.
- You may need to undergo other tests, which will be prescribed by your rheumatologist.
PA symptoms and risk factors
Scaly skin (psoriasis)
If you suffer from psoriasis, an autoimmune disease that causes scaly patches of skin, then you are at risk. 30% of people with psoriasis develop psoriatic arthritis.
Psoriasis
For most people, psoriasis symptoms begin about 5 to 10 years before arthritis develops. In some cases, arthritis appears first. 10% of people are diagnosed with psoriasis and arthritis at the same time.
The severity of psoriasis does not determine the development of psoriatic arthritis. Some psoriasis symptoms are so mild that people may be misdiagnosed as osteoarthritis or other types of arthritis.
Periodic joint pain
People with psoriatic arthritis may experience stiff, painful joints that are red and warm to the touch. Morning stiffness can be a particular problem. Such complex symptoms may be mistaken for rheumatoid arthritis, which is also caused by an autoimmune attack.
Like other autoimmune conditions, symptoms tend to flare and wane before flaring up again.
Psoriatic arthritis is not completely curable, but symptoms can be relieved. Symptoms can be moderate to severe and can lead to joint destruction, which may require joint replacement surgery.
Asymmetrical pain
Although this is not always the case, psoriatic arthritis tends to affect the large joints in the legs, such as the knees and ankles, or the tips of the fingers.
The pain is often asymmetrical, i.e. One knee may hurt, but the other may not. In contrast, rheumatoid arthritis is often symmetrical, for example affecting both wrists at the same time.
There are five subtypes of psoriatic arthritis. Four of them are asymmetrical, and they account for about 80% of cases.
Swollen fingers
Swelling in the arms and legs is observed in approximately 40% of patients with psoriatic arthritis. Because this symptom is much less common in other types of arthritis, it can help doctors differentiate between psoriatic arthritis and other conditions such as rheumatoid arthritis.
Dactylitis (swollen fingers) is caused by inflammation of the entire tendon that runs along the fingers or toes. Such finger problems may appear before other symptoms.
Leg pain
Psoriatic arthritis can cause pain and swelling outside the joints. Enthesitis is inflammation of the area where a tendon or ligament connects to a bone.
If it occurs in the foot, it may be misdiagnosed as plantar fasciitis or heel spur, which are typically caused by overuse or injury. People with rheumatoid arthritis may also have leg pain, as can people with lupus and other autoimmune diseases. Psoriatic arthritis can be similar to gout or arthritis, which also cause joint pain.
Pitting on toes and fingers
Pitting corrosion on fingers
Psoriatic arthritis can cause toenails and fingernails to become discolored or pitted, pitting, and nails that may even fall off.
This can happen with distal interphalangeal arthropathy, one of the five types of psoriatic arthritis. This type mainly affects the joints at the end of the fingers and toes.
It occurs in only 5% of patients and is more common in men than women.
Because nail changes are specific to psoriatic arthritis (and psoriasis), it can help doctors diagnose the condition.
Back problems
People with psoriatic arthritis often experience back problems along with other symptoms. Pain may occur along with inflammation and stiffness in the spine, neck and pelvis, or in the tendons and ligaments that attach to the spine. About 1 in 5 people with psoriatic arthritis have a type called psoriatic spondylitis, in which the bones of the vertebrae fuse.
Back problems are the only manifestation of psoriatic arthritis in 5% of patients.
Fatigue
Like other autoimmune diseases, psoriatic arthropathy can cause fatigue. Fatigue is a result of inflammation caused by arthritis.
Vision problems
People with psoriatic arthritis may suffer from eye inflammation known as conjunctivitis or iritis. This can cause blurred vision, and the eyes may become sore, red, and sensitive to light.
However, other autoimmune diseases such as rheumatoid arthritis and multiple sclerosis can also cause vision problems.
Finger deformity
Psoriatic arthritis can sometimes cause a flexion deformity in which the fingers deviate from their normal position.
About 5% of people with psoriatic arthritis develop the most severe form of the disease, called arthritis mutilans, a severe type of arthritis that primarily affects the fingers and toes. Left untreated, it can lead to destruction of multiple joints, often in the arms, legs, neck and lower back. When the disease affects the hands, it can cause the characteristic “telescoping fingers” - where the bones of the fingers retract, causing tissue destruction.
Psoriatic arthritis photo
Photo of hands with psoriatic arthropathy
Photo of legs with psoriatic arthropathy
Why the disease is terrible: consequences and complications
Psoriatic arthritis is an insidious disease because it can cause a lot of unpleasant consequences and complications.
Sometimes they develop even with intensive treatment. However, this only happens in particularly severe cases. So, in addition to the fact that the disease destroys joints and provokes severe pain, some of its types can also create additional difficulties for the patient.
Complications may include dactylitis (painful swelling of the fingers and toes), pain in the foot due to inflammation of the tendons, and spondylitis (inflammation of the joints of the spinal column).
In order not to aggravate an already difficult condition, it is recommended to constantly support your body by undergoing regular courses of preventive therapy.
Causes
Psoriatic arthritis is currently considered as a clinical manifestation of systemic psoriatic disease . Despite the fact that the cause of the development of psoriatic arthritis is still not clear, etiopathogenetic heterogeneity is noted. Researchers consider the etiology to be multifactorial and identify a number of factors contributing to the occurrence and manifestation of the disease:
- genetic;
- immunological;
- ecological (environmental).
Diagnostics
There is no separate analysis, the result of which can reliably confirm the diagnosis of psoriatic arthritis. Therefore, the specialist prescribes a series of tests for patients, and after evaluating the results of which, we can say with confidence that the patient has this particular illness.
Typically, patients suffering from characteristic symptoms are referred for the following types of examination:
- - ray Allows you to check the tissues of the joints for the presence of destruction characteristic only of this disease;
- ESR (erythrocyte sedimentation rate);
- rheumatoid factor (RF) . This is an antibody (protein formation) present in the blood in the presence of psoriatic arthritis.
- analysis of synovial fluid . The liquid is taken from the knee joint using a long needle, after which its composition is studied in the laboratory. If it contains uric acid, the patient is developing gout, not arthritis.
Also, during the examination, in order to maximize the accuracy of the diagnosis, the specialist uses the CASPAR criteria table, developed and approved by doctors in 2006. In this case, the doctor will evaluate some external criteria (5 points in total): the presence of psoriasis at the time of examination, dactylitis and others.
For compliance with each item, the patient receives 1 point. In order for a patient to receive an appropriate diagnosis, he needs to score from 3 to 5 points.
Treatment of the disease
An integrated approach to the treatment of psoriatic arthritis is practiced. Its treatment is aimed at reducing the severity of symptoms, preventing the spread of the inflammatory process to healthy tissues, vertebrae, and joints. During relapses, patients are advised to use a gentle regimen, wearing orthopedic devices - bandages, orthoses of varying degrees of fixation.
Medications
To relieve acute pain and eliminate stiffness, intra-articular administration of glucocorticosteroids is practiced. They are used only when non-selective (Diclofenac, Indomethacin, Ibuprofen) or selective (Meloxicam, Nimesulide, Celecoxib) non-steroidal anti-inflammatory drugs are ineffective. The following drugs can be used in the treatment of psoriatic arthritis:
- basic agents - Methotrexate, Leflunomide, Sulfasalazine, Colchicine;
- immunosuppressants - Azathioprine, Cyclosporine.
In severe cases of the disease, monoclonal antibodies to tumor necrosis factor, for example, Etanercept or Infliximab, are included in therapeutic regimens.
Physiotherapy
Photochemotherapy is the most effective physiotherapeutic measure in the treatment of psoriatic arthritis. During the procedure, the patient takes a photosensitizing drug, and then is exposed to external irradiation with UV rays. Patients are also prescribed several sessions of laser therapy, magnetic therapy, UHF therapy, shock wave therapy, ultraphonophoresis or electrophoresis with chondroprotectors, Dimexide, and hormonal agents.
ethnoscience
After carrying out the main therapy, achieving stable remission by reducing inflammation, the doctor may allow the use of folk remedies. It is not advisable to use rubs, compresses, and homemade ointments due to the high likelihood of skin irritation and relapse of psoriasis. Only teas and infusions made from rose hips, chamomile, and elecampane are allowed. To prepare them, pour a teaspoon of dry crushed raw materials with a glass of boiling water, leave for an hour, take 100 ml up to 3 times a day.
Treatment of arthropathic psoriasis
Unfortunately, this disease is quite difficult to treat, and there is no special therapy that can permanently relieve the patient of pain and other inconveniences. Therefore, the main goal pursued by specialists is to eliminate pain. To achieve maximum effect, it is recommended to use an integrated approach to treatment.
Drug therapy
During treatment, the patient may be prescribed:
- immunosuppressive drugs;
- glucocorticoids;
- NSAIDs;
- basic drugs.
The choice of medications should be made only by the attending physician, taking into account the characteristics of the course of the disease, the presence of side effects and concomitant diseases.
In especially severe cases, when medications do not have the desired effect, they resort to the help of surgeons.
Diet therapy
A properly structured diet is a necessity for patients with psoriatic arthritis. A well-organized menu can significantly reduce the manifestations of the disease.
During an exacerbation of arthritis, the following should be included in the diet:
- dairy products;
- vegetables, fruits, berries, herbs;
- dietary meat (turkey, rabbit, chicken);
- eggs (chicken and quail).
It is better to exclude fatty, spicy, salty foods, as well as alcoholic beverages, tobacco products, legumes, spices and other types of harmful foods from the diet.
How to treat the disorder with folk remedies?
To enhance the therapeutic effect, you can use folk remedies. Quite effective in the fight against the disease are compresses from dandelion leaves, a decoction of dandelion flowers, lingonberry tea, St. John's wort tincture, a decoction of spruce branches and many other recipes.
A decoction of dandelion leaves and flowers helps with arthritis.
The key to the successful application of folk advice is the regular use of medicines.
How to eat with psoriatic arthritis
Patients should be aware of certain dietary habits that will help them “keep the disease under control.”
Limiting the consumption of fatty, fried, spicy foods, sweets, coffee, strong tea, and a complete absence of alcohol will allow you to stay in remission for a longer period and avoid deterioration of your health, even without maintenance courses of drug therapy.
It is advisable, both during the acute phase and during the lull of the disease, to consume foods enriched with protein, unsaturated fatty acids, and fiber. And consume carbohydrates and fats in limited quantities.
You should say “yes” to fermented milk products, vegetables, both raw and boiled, lean sea fish, boiled dietary meat, fruits, soybeans, buckwheat, rice and chicken porridge.
Svetlana Ognevaya, a famous Russian dermatologist-phytotherapist, is of the opinion that in order to create optimal long-term remission for psoriatic arthritis, it is necessary to eat foods that create an alkaline environment in the body.
Alkaline-forming foods should make up 80% of the patient’s diet. Such products include vegetables and juices from vegetables, most fruits, with the exception of citrus fruits, pomegranates, white meat, seafood, milk, alkaline mineral waters.
Don't miss: Instructions for using the drug Metformin, as well as reviews and prices
It is important to avoid overeating, to eat small meals, but often (at least 5-6 times a day). Alcohol is not recommended to be consumed even in minimal quantities, as are sweets. If you really want something sweet, let it be a banana or a baked apple with honey.
How to live with psoriatic arthritis: prognosis and recommendations
In most cases, the disease develops gradually and is sluggish, with irregular exacerbations.
However, in severe clinical cases, the disease develops rapidly and is acute. The prognosis for such patients is disappointing, and it takes a lot of time to eliminate the symptoms.
If you already have psoriasis, in order to prevent the disease, be sure to try:
- avoid hypothermia and colds;
- regularly provide the body with feasible physical activity;
- do not deviate one step from the therapeutic recommendations prescribed by the doctor.
Apitherapy in the treatment of psoriatic arthritis
Treatment with bees and bee products (royal jelly, propolis, beebread, honey) is extremely popular and has a beneficial effect on the body for many ailments, including psoriatic joint changes.
The most desperate patients decide to conduct sessions where bees directly sting the skin over the inflamed area. A single release of up to 10 bees per medium-sized joint area is allowed. Bee venom has an anti-inflammatory, antioxidant, immunosuppressive effect, and improves blood circulation in the affected area.
Alcohol tinctures or water infusions are made from propolis. Patients use them internally or externally in the form of rubs and poultices.
Bee bread, royal jelly, beeswax, and propolis are included in many cosmetic creams produced by industry and sold through the pharmacy chain.
Apilak is a biogenic stimulant based on bee products that strengthens the immune system and is used for many conditions accompanied by immunodeficiency and immune disorders, including various manifestations of the psoriatic process.
Psoriasis arthritis and treatment with folk remedies
When treating the disease, specialists pay great attention to treatment and prophylactic complexes (therapeutic complexes). Gymnastics is often used during the patient’s rehabilitation period or during remission after the inflammatory process has reduced. Like massage, these complexes are contraindicated during an exacerbation.
The main goal of exercise therapy is to strengthen the muscular-ligamentous system and improve joint mobility. They are carried out under the supervision of a specialist with a permissible range of motion and should not cause severe pain.
Physiotherapy
These physiotherapeutic methods are used, as a rule, to treat the skin symptoms of psoriasis and affect the soft periarticular tissues.
Methods include the following types:
- electromagnetic therapy - UV irradiation with or without the use of photosensitizers;
- laser therapy;
- magnetic therapy.
These procedures help improve blood microcirculation in the affected areas, accelerate recovery processes and mobilize the body's protective properties. Procedures are contraindicated during the period of active inflammatory process.
Treatment with folk remedies
Like many other diseases, psoriasis arthritis is treated with folk remedies. Although it is quite difficult to call this a full-fledged treatment.
Rather, these techniques can be an addition to the main therapy. It consists of using decoctions and infusions based on St. John's wort, calendula, chamomile, echinacea and other medicinal plants. These drugs have anti-inflammatory and immunostimulating effects and have a beneficial effect on the body's condition. Before use, you should consult your doctor.
Compresses using plants that have anti-inflammatory properties have proven themselves quite well: white cabbage, nettle leaves, coltsfoot. These compresses will help reduce pain symptoms and swelling of the limbs. However, they should be used with caution in cases of severe skin manifestations of psoriasis and the presence of ulcerative peeling on the skin.
Diet
As you know, psoriasis arthritis can be of autoimmune origin, and 70% of the body’s immune defense, one way or another, depends on the functioning of the gastrointestinal tract (GIT). Thus, a proper diet is the key to a healthy body.
With this pathology, you should limit the use of:
- alcoholic drinks;
- spicy, salty and fatty foods;
- citrus fruits;
- products to which you are allergic are considered individually.
Eat more vegetables, fruits, fish, dairy products, and foods high in fiber. Monitor your body weight. Excess body weight increases the load on sore joints.
Complications
Psoriatic arthritis is chronic. It occurs cyclically and periods of remission are replaced by stages of exacerbation. Existing treatment methods can improve the patient’s quality of life, but cannot eliminate the disease as a whole. In the absence of timely and adequate medical treatment, the disease leads to loss of ability to work and disability. And other pathologies developing against the background of severe arthritis can lead to death.
Reasons for the development of the disease
Psoriatic arthritis
The development of the disease is formed against the background of changes in epidermal cells. These changes, in turn, are triggered by changes in chemical and biological processes. The same factors cause the appearance of foci of inflammation in the joint cavity and bone tissue.
The exact causes of psoriatic arthritis are not fully understood, but medical researchers believe that the main factors influencing the development of the disease are disruptions in the nervous system . Various nervous shocks, disorders, stress, mood swings - all this over time causes symptoms of a serious illness. But this is not the only reason, because one should not exclude a hereditary predisposition , as a result of which psoriatic arthritis may occur in the offspring.
In addition, there are a number of factors that directly lead to the development of a pathological abnormality in the form of psoriatic arthritis.
- When the body is infected with various types of bacteria or viruses . These bacteria are able to live in the human body for a long time, thereby becoming pathogens.
- If the joints had characteristic features of damage or bruises . In this case, a minor injury can cause serious consequences.
- In case of metabolic disorders . If the metabolic process is disrupted, the body and all organs experience heavy loads, which leads to their failures. In this case, the development of arthritis is observed in the joints, this is especially typical for the spine.
- If surgery was performed , during which an infection could enter the body.
- For connective tissue ailments , as a result of which a person develops psoriasis, causing the development of arthritis.
- Nervous disorders, stress, mood swings . Any psycho-emotional disorders lead to malfunctions of certain organs, which causes the development of the disease.
- Bad habits . Alcohol and tobacco products lead to a decrease in the human immune system, which makes it possible for bacteria to actively spread and develop.
- Presence of hormonal levels . These reasons are typical for the fair sex, as a result of which the body needs to constantly readjust due to menstrual cycles, pregnancy and menopause. During pregnancy, symptoms of the disease can be unpredictable. In some pregnant patients, there was an increase in the symptoms of the disease, while in others, on the contrary, the symptoms of the disease partially faded away for a while. During menopause or the menstrual cycle, the signs of arthritis intensify.
- When using medications, the possibility of developing the disease cannot be excluded. These drugs include anti-inflammatory non-steroidal drugs: Diclofenac, Ibuprofen.
- Disorders of the endocrine glands.
- Increased activity of T lymphocytes , which affect the functioning of the immune system.
As you can see, there are more than enough reasons for the development of the disease, so anyone, even a healthy person, can develop psoriatic arthritis. The next section will tell you how to find out if a person has signs of a disease.
Forecast and preventive measures
Timely drug therapy can achieve stable remission of psoriatic arthritis. Pathology usually occurs unpredictably. The prognosis of psoriatic arthritis will depend on the severity of the disease, the frequency of relapses, the timeliness and correctness of treatment.
To avoid joint damage, people with psoriasis are advised to:
- stop smoking;
- eat rationally;
- eliminate alcohol consumption;
- avoid stressful situations;
- timely treatment of infectious diseases.
It is important to control your weight so that the load on your joints does not increase and do exercises to develop them.
Psoriatic arthritis is considered a dangerous disease. Very often the disease ends in disability for the patient. Proper complex therapy will help restore the affected joint to its functionality.
Diagnostic criteria for PA
Psoriatic arthritis - develops in approximately 7% of people with psoriasis. PA is difficult to diagnose because the symptoms are similar to inflammatory joint lesions.
The main symptoms are expressed as:
- skin inflammations of a psoriatic nature and destruction of nails - clouding, furrows, grooves on them;
- destructive conditions of the distal interphalangeal joints of the fingers;
- painful sensations in the heels;
- swelling of the fingers, simultaneous damage to the metatarsophalangeal (metacarpophalangeal) and distal (proximal) interphalangeal joints;
- negative reaction to autoantibodies;
- purplish-blue coloration of the skin over the affected joints;
- multi-axial displacement of bones during osteolysis, periosteal overlays (periostitis);
- early damage to the joint of the big toe;
- radiological and clinical signs of inflammation of the sacroiliac joints;
- morning stiffness and pain in the spine;
- X-ray symptoms of psoriatic spondylopathy (pathological changes in the intervertebral discs).
The diagnosis of PsA is usually made when skin manifestations and multi-axial bone displacements are detected, against the background of psoriatic heredity.
Possible complications
In severe cases, there is a risk of damage to internal organs and other complications. The most likely consequences of the disease include:
- The occurrence of multiple arthritis with severe swelling;
- Curvature of joints;
- The appearance of excruciating pain;
- Weight loss;
- Weakening of the immune system;
- Trophic ulcers;
- Hair loss;
- Iridocyclitis;
- Hepatitis;
- Heart diseases;
- Disturbances in brain function;
- Glomerulonephritis.
Advanced forms of the disease can cause disability and even lead to death.
Causes and predisposing factors
The real causes of the disease are unknown; official medicine adheres to the theory of the multicomponent influence of various factors:
- Genetic predisposition (40–45% of patients had immediate relatives with psoriasis or psoriatic arthritis).
- Autoimmune and toxic-allergic reaction (to an increase in inflammatory, anti-inflammatory substances and products of cellular necrosis in the blood).
- Injuries (in 25%).
- Metabolic problems (diabetes mellitus).
- Infections.
- Long-term use of medications (non-steroidal anti-inflammatory drugs, beta blockers).
- Nervous and physical exhaustion, excessive stress.
- Hormonal imbalance (physiological changes, disease).
- Bad habits (tobacco smoking, alcoholism).
Among the factors that can trigger the appearance of psoriatic arthritis are sun exposure (sunburn), age (usually from 30 to 50 years) and the presence of diagnosed psoriasis.
Click on photo to enlarge
Symptoms
The key symptom of psoriatic arthritis is pain. It can be localized in different joints. However, there are a number of symptoms that are characteristic of this particular disease:
- Swelling of the joint. The swelling spreads to nearby tissues.
- Pain upon palpation.
- Blue skin color. Sometimes it turns purple.
- Damage to the nail plates.
- Thickening of fingers. This occurs symmetrically on the arms and legs.
- Shortening of fingers.
- Dislocations of different directions. They are caused by a violation of the density and decrease in the elasticity of the ligaments.
- Formation of ossifications. This problem occurs when intervertebral joints are damaged, which is observed in 40% of cases. This causes pain and stiffness in motor activity.
- Increased skin temperature in the affected area.
Experts also identify malignant psoriatic arthritis. Typically, this anomaly develops in young men - under 35 years of age.
In this case, specific symptoms of psoriatic arthritis occur:
- Damage to the joints of the spine and skin;
- Fever;
- General weakness, exhaustion of the body;
- Impaired motor activity of joints, polyarthritis, which is accompanied by severe pain;
- Increased size of lymph nodes;
- Damage to most organs - eyes, liver, kidneys, nervous system, heart.
Treatment and prevention of PA development
Smirnov Alexander Viktorovich
Leading Researcher, Doctor of Medical Sciences State Institute of Rheumatology of the Russian Academy of Medical Sciences
The main radiological symptoms of pathological changes in small joints of the hands in rheumatic diseases
Rheumatoid arthritis (RA)
Psoriatic arthropathy (PsA).
Systemic scleroderma (SSc)
Systemic lupus erythematosus (SLE).
Primary osteoarthritis (OA)
Initial manifestations (correspond to stages 1-2 of arthrosis according to Kellgren):
Pronounced changes (correspond to 3-4 stages of arthrosis according to Kellgren):
Features of the pathology
Joint damage in psoriasis is observed in 50% of patients. The disease most often develops between 20 and 50 years of age. Sometimes it is observed in children. Inflammatory joint damage usually occurs with skin lesions. This means that both symptoms are present at the same time.
In 25% of cases, changes in bone tissue occur several months or even years before plaques appear. The course of the disease resembles the symptoms of ordinary arthritis.
Abnormal changes can affect any part of the body - large shoulder or knee joints. There is also a risk of damage to all parts of the spine and sacrum. If the process becomes generalized, the collarbones and jaws may suffer.
This type of arthritis can get worse periodically. This happens several times a year, with exacerbations being seasonal. Provoking factors include stressful situations, traumatic injuries, colds, and hypothermia.
How is the disease treated?
Arthritis with psoriasis is not a death sentence, and it is not fatal, provided that you consult a doctor in a timely manner. According to medical protocol in rheumatology, the disease requires an integrated approach to stop progression.
Important information: Types and forms of psoriasis: what is the disease in severe and mild form?
Use of medications
All forms of medications are used for therapy - tablets, injections, external agents (for psoriatic plaques).
It is impossible to completely cure the pathology; you can only prevent the situation from getting worse.
And in some cases, as a rule, with early consultation with a doctor, it is possible to partially restore the functionality of the joint.
The following groups of medications are used in treatment:
- Immunosuppressive drugs (Cyclosporin A).
- Glucocorticosteroids (Sinalar).
- Antidepressants (Tenoten).
- Non-steroidal anti-inflammatory drugs (Indomethacin).
These drugs stop inflammatory processes, reduce the body’s immunological aggression, which is directed against its own cells, which promotes long-term remission.
Physiotherapy
Physiotherapeutic manipulations are prescribed only at a regressing stage. Physiotherapy has contraindications.
The following procedures give good results:
- Electrophoresis with hydrocortisone.
- UHF.
- Laser exposure.
- Therapeutic baths based on sea salt.
Exercise therapy under the supervision of a physician is also recommended. Therapeutic exercise allows you to maintain the functionality of the affected joint and improves its functioning.
Nutrition Basics for Arthritis
The diet should be light, excluding fried, fatty, smoked, and spicy foods. The menu includes fermented milk and dairy products, fruits and vegetables. You need to eat foods enriched with plant fiber.
Avoid alcohol and limit sugar consumption.
Modern diagnostic methods
If you have the described symptoms, you should definitely consult a doctor. To make a correct diagnosis, medical specialists resort to instrumental and laboratory diagnostic methods. It's differential.
There are no laboratory tests that can help make a correct diagnosis with 100% accuracy. In addition, if the patient has damage to the small joints of the hands, then laboratory tests may not show anything at all.
From laboratory tests, the patient is prescribed a general blood test. It may show an increase in erythrocyte sedimentation rate and a high concentration of leukocytes. If the patient has a malignant form, then anemia is diagnosed.
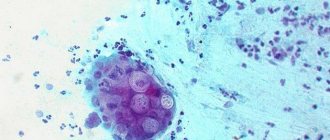
Additionally, a rheumatoid test is prescribed. The synovial fluid is examined - it is obtained by puncture from the joint. A high concentration of cells, especially neutrophils, is determined in the liquid. She also has pathological viscosity - below normal.
Instrumental diagnostic methods:
- X-ray examination. An accessible technique that allows you to see various changes. Sometimes the disease may appear on photographs as a form of rheumatoid arthritis. Against the background of the mutating species, transformations in the structure and shape of the joint are visible.
- MRI, CT. It is especially often used to diagnose lesions of the spinal column.
The main criteria for diagnosing the disease include involvement of the finger joints in the pathological process, multiple asymmetric lesions, the presence of plaques on the skin, and radiological signs. Another negative result when performing a rheumatoid test, family history.
To make a diagnosis, at least three criteria must be present, one of which is the presence of psoriasis in close relatives, psoriatic plaques on the body, or the absence of periarticular osteoporosis.