Sarcoidosis is a systemic disease that can affect various organs and tissues of the human body. The pathology occurs everywhere and affects patients of all ages. However, according to the observations of specialists, young and middle-aged women are more often affected by the disease.
Sarcoidosis
Sarcoidosis is a disease about which ordinary people know little, and most know nothing at all. Not even all medical workers are aware of it. What is this mysterious disease that can lead to a forced lung transplant, and in some cases goes away spontaneously? What details are known about this disease, its causes and symptoms, what place does sarcoidosis occupy in the ICD, what are its most common forms? In what cases do doctors take a wait-and-see approach, when are medications needed, and is alternative treatment for sarcoidosis possible?
How does sarcoidosis affect the heart?
The formation of granulomas in the cardiovascular system can be of any location, but most often it occurs directly in the myocardium. Granulomas impede the normal functioning of the heart, preventing the “pumping” of blood and its delivery to all tissues of the body.
In particular, clusters of immune cells can affect the heart's electrical system, causing irregular heartbeats and even severe arrhythmias. In extreme cases, the effect of sarcoidosis on the heart leads to the development of heart failure, a potentially life-threatening condition.
Sarcoidosis in adults
Sarcoidosis is a disease that usually develops in adulthood. People between 20 and 40 years of age are most vulnerable to it.
Sarcoidosis in men
Men develop sarcoidosis much less frequently than women. However, the presence of occupational hazards associated with contact with small particles of dust, gas, various suspensions in the air, and prolonged smoking significantly increase the likelihood of the onset of the pulmonary form of the disease.
Sarcoidosis in women
Female gender is an additional risk factor in the development of any autoimmune disease. Since Beck's sarcoidosis can be classified in this group, it turns out that it most often develops in girls and young women aged 20 to 40 years. However, in identifying this disease, an additional role is played by the fact that representatives of the fairer sex more often undergo fluorographic examination, since they are more attentive to their health.
Tests to diagnose sarcoidosis
The diagnosis of sarcoidosis is made through various types of exams, during which the patient's general condition is assessed, paying special attention to skin lesions, regularity of heartbeat and breathing, the presence of pressure points and the shape of the lymph nodes.
Only after this can additional diagnostic studies be carried out:
- Blood analysis. Allows you to evaluate the levels of blood cells, thus identifying possible leukopenia and thrombocytopenia, and assessing organ function indicators. For example, in cases of liver damage, alkaline phosphatase levels increase, while elevated creatinine indicates kidney damage.
- Radiography. Particularly suitable for detecting granulomas in the lungs.
- Magnetic resonance imaging. Particularly useful in the diagnosis of sarcoidosis of the nerves and possible damage to the muscles and heart. It is also useful in identifying granulomas in the abdominal cavity: liver, spleen and pancreas.
- Six minute test. This test is done to test the patient's ability to exert effort while observing changes in the heartbeat.
- Breath test. Performed to assess the subject's breathing capacity.
- Hemogas analysis. Used to assess the ability of the lungs to regulate the levels of carbon dioxide and oxygen in the blood. It is performed using arterial blood sampling.
- Biopsy. It consists of obtaining a piece of tissue for subsequent examination under a microscope. It can be performed in cases of sarcoidosis of the lungs, bronchi, skin, conjunctiva and lymph nodes.
Finally, let's say that differential diagnosis , since the formation of granulomas can be caused by infections, mycobacteria, fungi or parasites. Differential diagnosis is carried out using special tests to determine the presence or absence of pathogenic microorganisms.
Sarcoidosis disease: what is it?
The disease sarcoidosis still raises many questions among practicing doctors and is a difficult mystery for them. The reasons are that, despite the development of medical science, little is still known about it. Synonyms for the disease sarcoidosis are Besnier-Beck-Schaumann disease. The essence of this disease is the appearance of granulomas (dense nodules) in various tissues of the human body, which are its main criterion in diagnosis. Most often they occur in the intrathoracic and peripheral lymph nodes, lung tissue, liver, eyes, spleen and less often in other organs: bones, skin.
Typically, the disease sarcoidosis debuts in both sexes between the ages of 20 and 40, but women still suffer from it more often than men. In childhood, this disease practically does not occur. It is not a contagious disease, but symptoms of sarcoidosis are often observed in several members of the same family, that is, there is a version about the hereditary nature of its transmission. Considering the difficult nature of the diagnostic search, the number of patients with this disease in different countries is not reliably known: the situation is more or less clear with the assessment of incidence in European countries, the USA, Japan, and Australia. However, how many patients with sarcoidosis there are in African or Asian countries remains a mystery due to the lack of accurate statistics.
Hemorrhoids kill the patient in 79% of cases
A special feature of the disease sarcoidosis is the completely unexpected nature of its course: some people, after a certain time, recover on their own without any treatment. Doctors still cannot answer the question: why does this depend and how to give the patient an accurate prognosis. For the same reason, they cannot reliably say how long people with sarcoidosis live, since the disease sometimes behaves completely unpredictably.
The prevalence of Beck's sarcoidosis in Russia ranges from 22 to 47 people per 100 thousand population, which allows us to classify this disease as rare.
Causes of sarcoidosis
Beck's sarcoidosis is an autoimmune disease, for most of which the exact cause is unknown to science. This disease is not infectious and is not transmitted from one person to another, but there are frequent cases of familial onset of the disease. However, there is also no evidence that the disease sarcoidosis is genetically determined. And, nevertheless, there are works that confirm the influence of nationality and race on the course of this disease. For example, in dark-skinned people it occurs more often, in the Japanese a complication in the form of myocarditis is quite common, and in people of the Caucasian race - erythema nodosum.
There are several theories about the possible origin of the disease sarcoidosis. Among them are infectious-mediated (the influence of fungi, protozoa, bacteria), hereditary and associated with the fact that the disease is directly associated with the presence of occupational hazards and appears in people working in specific industries (workers in agriculture, the chemical industry, post offices, millers and firefighters). The prevalence of pulmonary sarcoidosis is also slightly higher among smokers.
What does Beck's sarcoidosis mean?
Beck's sarcoidosis is one of the names for this disease. In addition, it has several synonyms: Beignet and Schauman. However, the first name is the most common.
Place of sarcoidosis in ICD 10 revision
This disease has its place in the International Classification of Diseases, 10th revision. However, sarcoidosis in ICD (D86) is represented by several subtypes of the disease, which depends on the location of the lesion. Here are the most common:
- D86.0 – pulmonary sarcoidosis,
- D86.1 – sarcoidosis of the lymph nodes,
- D86.2 – pulmonary sarcoidosis with damage to the lymph nodes,
- D86.3 – cutaneous sarcoidosis,
- D86.8 – sarcoidosis of other specified and combined localizations,
- D86.9 – sarcoidosis, unspecified.
This disease belongs to the group: individual disorders involving the immune mechanism. Thus, the very location of the disease sarcoidosis in the ICD 10 revision does not allow it to be classified as a specific group, since there is no specific localization of the process, as, for example, happens with pneumonia, tonsillitis or pyelonephritis.
Treatment of sarcoidosis with folk remedies
The use of alternative medicine methods is allowed by doctors if it does not disrupt the functioning of organs that have suffered from granulomas. For this reason, you should first consult with a specialist. For sarcoidosis, the following recipes are used:
- Mix 1 tbsp. l. dried herbs: oregano, sage, marshmallow root, knotweed and calendula. Pour a glass of boiling water over 1 tbsp. l. collection, leave for half an hour in a thermos. Drink 1/3 tbsp. 3 rubles/day for 1 month.
- 1 tbsp. Pour a spoonful of crushed elecampane root into a glass of boiling water. Boil for 20 minutes, add 7 apricot kernels. Strain before use. Drink 1/3 cup 3 times a day for 3-4 weeks.
Forms of sarcoidosis
Doctors distinguish various forms of sarcoidosis, and they are primarily due to the different localization of the appearance of granulomas. The disease behaves so unpredictably that it is difficult to predict exactly where in the patient they will appear.
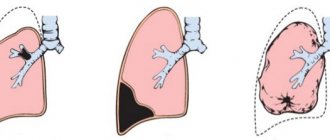
Pulmonary sarcoidosis: stages of the disease
The most common of all existing forms of this disease is pulmonary sarcoidosis. It is no coincidence that pulmonologists see such patients more often than others, because it is to them that internists or general practitioners refer them.
This form of sarcoidosis develops due to the fact that peculiar neoplasms specific to it appear in the lung tissue - granulomas of epithelioid cells with giant nuclei. They gradually increase in size and merge with each other. In appearance, they are very reminiscent of similar lesions in the tuberculosis process; it is for this reason that these diseases are often differentiated from each other. However, unlike the latter, there are no foci of caseous necrosis and mycobacteria inside these formations, they do not disintegrate, so the prognosis for pulmonary sarcoidosis is completely different. These lesions may suddenly disappear spontaneously, or sometimes they resolve with the formation of areas of fibrosis (scar tissue).
Thus, the clinical manifestations of pulmonary sarcoidosis directly depend on the number of lesions and their effect on respiratory function, that is, how much lung tissue is lost from the gas exchange process. This is one of the few chronic diseases in which complete self-healing is possible, which is what patients and their doctors hope for.
Clinical manifestations are very dependent on the stage of sarcoidosis, of which there are only 3. At each of them, the volume of the pathological process is different, so medical tactics are also different. Moreover, the damage begins not from the lungs, but from the fact that the patient develops sarcoidosis of the intrathoracic lymph nodes. After this, as it progresses, when doctors diagnose stage 2 sarcoidosis, the parenchyma of the lungs themselves is also involved in the process. However, at each stage, spontaneous remission or complete recovery may occur, which distinguishes this disease from most others.
Identifying the stage of sarcoidosis in the diagnosis is very important for understanding the advanced stage of the process and determining treatment tactics.
Stage 1 sarcoidosis or sarcoidosis of the intrathoracic lymph nodes
If a patient is diagnosed with sarcoidosis of the intrathoracic lymph nodes or stage 1 of the disease, then granulomas usually appear in the bronchopulmonary, tracheobronchial, bifurcation or paratracheal lymph nodes. In most cases, these changes are an incidental finding during routine fluorography or x-ray examination of the chest organs for a completely different reason. If there is sarcoidosis at this stage, there are usually no symptoms. Only in rare cases may a patient complain of a feeling of heaviness in the chest, which intensifies with breathing, but almost no one makes such complaints. In some cases, there are nonspecific symptoms such as weakness, malaise, sweating, weight loss, prolonged low fever, etc. However, they may indicate a large number of other ailments, among which sarcoidosis of the intrathoracic lymph nodes is far from the first place. Some patients experience spontaneous recovery, but sometimes the initial stage of the disease smoothly turns into stage 2 sarcoidosis.
Pulmonary sarcoidosis stage 2
Sarcoidosis grade 2 is characterized by combined damage to the lymph nodes and lung tissue. This stage of the disease is usually a natural development of sarcoidosis of the intrathoracic lymph nodes, in which miliary (smallest) or focal (larger) formations appear in the lungs. In terms of their radiological signs, they are very similar to disseminated pulmonary tuberculosis, however, these are two completely different diseases and the tactics for them are not the same. In the second case, the patient definitely requires treatment, because he is contagious to those who live next to him. A patient with stage 2 sarcoidosis does not pose any danger to others, and doctors choose individual tactics, which may include watchful waiting, that is, without the use of medications.
In some cases, even at this stage of the disease, the patient may not experience any negative sensations and these changes will be only an accidental finding during an X-ray or fluorography. However, usually patients are still bothered by shortness of breath, cough, chest pain; during auscultation, dry or moist rales are sometimes heard in the lungs. This is usually accompanied by nonspecific symptoms, such as weakness, low-grade fever, chills, sweating, and fatigue. If a patient has combined sarcoidosis, the symptoms may indicate the appearance of extrapulmonary symptoms, as complications develop in the liver, spleen, bones, joints, and eyes.
Stage 2 sarcoidosis can progress to stage 3 of the process, and spontaneous recovery can occur.
Pulmonary sarcoidosis stage 3
At stage 3 of sarcoidosis, granulomas in the lungs and lymph nodes transform into areas of fibrosis, or scar tissue. This is an alternative to spontaneous recovery and is the final stage of the process. These foci of fibrosis fall out of gas exchange, since the lung tissue in them is no longer actually such and is a regular scar. At the same time, an increased load is placed on other parts of the lung (healthy ones), since the need for oxygen does not decrease, they grow and emphysema forms. Unfortunately, this process is irreversible and no medications can completely help the patient.
As a rule, this stage of the process is not asymptomatic. The patient is worried about shortness of breath, cough with scanty sputum, weakness, weight loss, dizziness, decreased tolerance to physical activity, frequent colds, respiratory diseases, etc.
During the course of the disease at any stage, periods of exacerbation, remission, and spontaneous recovery are distinguished. According to the rate of growth of pathological changes, the process can be slow, abortive, chronic or progressive.
Sarcoidosis of peripheral lymph nodes
Sarcoidosis of lymph nodes located outside the chest is a fairly common complication of this disease. It occurs in 25% of patients with this disease. In this form of sarcoidosis, the following lymph nodes are affected:
- back and front cervical,
- elbows,
- supraclavicular,
- inguinal
With sarcoidosis, the lymph nodes become larger in size and have a densely elastic consistency, but fistulas do not form. They are painless and do not cause suffering to the patient if they do not increase to such an extent that they compress the surrounding tissues, organs and blood vessels.
Sarcoidosis of the lymph nodes is a prognostically unfavorable sign of this disease, as it usually indicates the malignant, transient nature of the process. Often the course of the disease becomes persistently relapsing. If a person is suspected of having sarcoidosis, a biopsy of the lymph node is very important for the doctor, because it can reveal the presence of epithelioid cell granulomas specific to this disease.
Sarcoidosis of the skin
Sarcoidosis of the skin occurs in about a third of patients with this disease, that is, only these people have specific skin lesions that allow a specialist to easily make a diagnosis. Often they are generally the first signs of the disease, which appear long before complications from the respiratory system, and they are more obvious than all the others. However, not every doctor, seeing such bright and specific areas of damage, will be able to determine that it is sarcoidosis of the skin, since it occurs very rarely.
The most common symptoms of this disease are the following:
- Erythema nodosum.
This skin manifestation of the disease is the result of secondary vascular damage - vasculitis. That is, visually the doctor sees round, dark, fairly dense nodes on the skin that are painful on palpation. They cause discomfort to the patient and sometimes cause serious suffering. The most common localization of the process is on the lower extremities. A biopsy for this form of sarcoidosis is not diagnostically informative, since the nodes are a consequence of vasculitis and do not contain epithelioid cells with giant nuclei characteristic of this disease. Considering the painfulness of the process, erythema nodosum must be subject to adequate treatment, and the sooner it is started, the more likely a favorable outcome.
- Sarcoid plaques.
They are painless convex skin lumps, burgundy in color with a clearing in the center. They do not itch, itch or cause any discomfort. They are usually located symmetrically on the buttocks, lateral surfaces of the body, face and limbs. They are usually part of the structure of the disease sarcoidosis, the symptoms of which affect several organs and systems at once and are complemented by the involvement of the lungs, lymph nodes, spleen, and liver in the process. These skin lesions persist for quite a long time, usually do not go away on their own, cause mental suffering to the patient, as they are a significant cosmetic defect, and therefore require mandatory treatment. If a patient has cutaneous sarcoidosis, plaque biopsy followed by histological analysis is an excellent method for accurately verifying the diagnosis.
- Lupus chills.
Cutaneous sarcoidosis, which occurs in this form, visually resembles the rashes that appear with systemic lupus erythematosus. They are represented by bright symmetrical purple rashes on the sides of the nose, cheeks, fingers and ears. They are painless, do not itch or cause discomfort. However, given the fact that they are in a visible place, these skin lesions represent a major cosmetic defect and cause mental suffering to the patient. As well as sarcoid plaques, lupus pernio is usually combined with other localizations of damage in this disease.
The prognosis for the cutaneous form of sarcoidosis depends primarily on the nature of the process. If the rash appears suddenly, sharply, spontaneously, then the likelihood of self-healing or a quick response to adequate therapy is more likely than with a chronic, sluggish process.
Sarcoidosis of other organs
In addition to the most common localizations, there are rarer forms of sarcoidosis. They are often extremely difficult to recognize, since the changes are nonspecific, that is, they outwardly resemble many other diseases. Here are the most common localizations of this disease:
- Sarcoidosis of the spleen.
Occurs in 10-40% of patients. It manifests itself as an increase in the size of this organ (splenomegaly), or an increase in its work to destroy blood cells (hypersplenism). In some cases, this organ has to be removed, since the massive spleen interferes with normal movement and causes pain in the left hypochondrium.
- Sarcoidosis of the organ of vision.
This form occurs in 25% of all patients with this disease and is the most dangerous, because without timely treatment, sarcoidosis can lead to blindness. It is represented by anterior, posterior uveitis, uveoretinitis. With this type of complication, in 80% it is possible to detect simultaneous damage to nearby lymph nodes and lymph nodes of the roots of the lungs, changes in the bones, spleen and liver.
- Sarcoidosis of the hematopoietic organs.
Occurs infrequently. However, complications from the operation of this system are not uncommon, because many drugs used as basic therapy inhibit it and lead to erythro- and neutropenia.
- Sarcoidosis of the kidneys.
Occurs in 10% of patients with this disease. It may cause the appearance of granulomas that interfere with the normal process of urine formation, as well as secondary deposition of calcium salts, which also negatively affects the functioning of these organs.
- Sarcoidosis of the musculoskeletal system.
Presented with complications from joints, bones, muscles. The most dangerous is the appearance of cysts in the bones of the skull and spine.
- Sarcoidosis of the heart.
It is one of the most serious forms of this disease, because in this case granulomas form in the heart muscle and prevent its full contraction.
- Neurosarcoidosis.
It also belongs to the most severe forms, but the prognosis depends primarily on which nerves are involved in the pathological process.
- Sarcoidosis of the digestive organs.
It is represented mainly by the diffuse formation of granulomas in the liver parenchyma. Most often, patients are bothered by heaviness in the right hypochondrium caused by the enlargement of this organ (hepatomegaly).
Classification
Pulmonary sarcoidosis begins with damage to the alveolar tissue and is accompanied by the development of interstitial pneumonitis
Depending on the area of localization of the first granulomas, sarcoidosis is distinguished:
- lungs and respiratory organs, as well as other organs and systems;
- lymph nodes - lymph nodes of the mediastinum, neck, intrathoracic, etc.;
- generalized.
In the vast majority of cases, the disease begins with damage to the lungs or intrathoracic lymph nodes.
Depending on the clinical picture, the following stages of sarcoidosis are distinguished:
- the first, characterized by the active formation of nodules, the involvement of new organs and systems in the pathological process and the appearance of the first acute signs of the disease;
- the second, accompanied by the onset of remission (during this period, practically no new formations arise, the growth of old ones stops, the condition of the patients stabilizes, and no new complaints appear);
- the third, characterized by a stable course of the disease, an increase in granulomas and their necrotization, deterioration of the condition of patients, multiple disorders of the functions of organs and systems.
Sarcoidosis develops slowly, but it is usually not possible to completely overcome it.
Sarcoidosis: symptoms of the disease
If a patient has sarcoidosis, the symptoms of the disease can be completely varied. Starting with the fact that they may not exist at all. At the first stage of the disease, when there is only damage to the intrathoracic lymph nodes, patients do not complain of anything. Sometimes they may only be bothered by nonspecific symptoms, such as weakness, fatigue, weight loss, loss of appetite, prolonged low-grade fever, chest pain without a specific localization.
When foci appear in the lung tissue, shortness of breath, cough, sometimes sputum appears, episodes of respiratory infectious diseases become more frequent, and dry or moist rales can be heard in the lungs. This is often accompanied by skin complications (erythema nodosum), eye damage (uveitis), and enlarged liver and/or spleen.
At the third stage of the disease, the patient experiences respiratory failure, which is caused by the exclusion of part of the lung tissue from gas exchange and emphysematous growth of the rest. A person has a hard time with physical activity, during which he experiences shortness of breath (typically difficulty breathing), and periodically he has bouts of coughing with phlegm. At the same time, such patients already have one or more combined lesions of other organs.
Prevention of sarcoidosis
In order to avoid exacerbations of the disease, it is necessary to pay special attention to a healthy lifestyle . If a patient is diagnosed with pulmonary sarcoidosis, then it is most important for such a person to quit smoking, which directly affects breathing difficulties and provokes complications of the disease. It is recommended not to take medications and avoid contact with chemicals that are harmful to the liver, and to avoid toxic volatile substances, dust and gases that are harmful to the lungs. Patients with sarcoidosis always have high levels of calcium in the blood, which contributes to the formation of stones in the bladder and kidneys. Given this, patients should not eat foods high in calcium. In order to prevent exacerbation and complications of the disease, it is necessary to regularly undergo the required courses of therapy and visit a specialist for regular health monitoring.
Sarcoidosis: diagnosis of the disease
Sarcoidosis is a complex and rare disease. It occurs infrequently and each patient has different clinical manifestations. For this reason, if a patient has developed sarcoidosis, diagnosis can take a lot of time and the result will depend primarily on the competence of doctors: not every one of them has encountered a similar disease.
The first and very important step in verifying the diagnosis is the examination of such a patient. If only the intrathoracic lymph nodes are affected, it may be completely uninformative. However, starting from stage 2 and in the presence of damage to other organs, the diagnosis of sarcoidosis will certainly reveal important facts already at the examination stage, especially if there is damage to the eyes, joints, liver, spleen and peripheral lymph nodes.
The doctor carefully talks with the patient, asks if he has lost weight recently, how he tolerates the usual physical activity, if there is shortness of breath or cough, if there is a low fever without signs of a cold. Patients with sarcoidosis often describe their condition vaguely, because there are no specific symptoms for this disease and the patients themselves do not attach much importance to many of them for several years.
Sarcoidosis: biopsy and its role
If a patient is suspected of having sarcoidosis, a biopsy is one of the most important methods in the diagnostic search. Indeed, with this disease, granulomas (small focal formations) appear in various organs, consisting of macrophages and epithelioid cells (giant multinucleated ones). It is on the basis of their detection that doctors can make this diagnosis, which in its clinical manifestations is similar to a whole list of others, among which tuberculosis and systemic connective tissue diseases take the first place.
Biopsies are most often taken from intrathoracic or peripheral lymph nodes, but the initial diagnosis of sarcoidosis may require an invasive procedure on the lungs. Previously, it was always performed using the open thoracotomy method, but it is extremely traumatic and requires general anesthesia, which is not always possible. Today, doctors have access to methods such as transbronchial biopsy or using thoracoscopic instruments. With these methods, pain relief is less deep, and mechanical damage is not as serious as with classic thoracotomy.
Skin lesions with erythema nodosum are not suitable for puncture, since the cause of their appearance is vasculitis (vascular pathology). However, a biopsy of sarcoid plaques or formations in lupus pernio turns out to be informative, because cells characteristic of this disease are present in them.
Laboratory and instrumental research methods
If a patient is suspected of having sarcoidosis, the diagnosis of the disease is carried out through a large list of various measures. Among them there are both laboratory and instrumental methods.
Laboratory diagnosis of sarcoidosis includes the following mandatory points:
- general clinical analysis of blood, urine,
- biochemical analysis of liver and kidney function indicators, the presence of acute phase proteins and rheumatic tests,
- tuberculin test, which will always be negative, which makes it possible to differentiate this disease from tuberculosis,
- blood gas composition is examined in patients in serious condition.
Instrumental methods for diagnosing sarcoidosis are as follows:
- X-ray examination of the chest organs,
- magnetic resonance, positron emission or computed tomography,
- spirometry (assessment of external respiration),
- endoscopic ultrasound examination of intrathoracic lymph nodes,
- electrocardiographic examination and echocardiography of the heart,
- additional diagnostic methods are carried out depending on the presence of a specific form or complications of the disease.
Symptoms and diagnosis
Various causes of sarcoidosis lead to the formation of the same symptoms. Externally, the disease manifests itself as weakness, fever, weight loss, and an increase in the size of the lymph nodes. Weakness appears due to metabolic disorders; tissues lack nutrients and oxygen.
Patients feel especially bad in the morning; they do not feel rested and complain of fatigue. The patient's condition is similar to "chronic fatigue syndrome." Often headaches are added to weakness. Fever is mainly observed in the acute form of the disease. In this case, the patient’s body temperature rises to 38 degrees.
Weight loss is a consequence of metabolic disorders in the body and constant inflammation. When granulomas form, lymph nodes become inflamed and increase in size, especially those located in the chest area.
Dystrophic changes in the spine
As the disease spreads in the lungs, other signs appear:
- shortness of breath, especially after minor physical activity;
- cough of reflex origin, not accompanied by sputum and mucus;
- occasional mild chest pain.
With subsequent development against the background of sarcoidosis, pneumonia can form, which is already accompanied by sputum production. Damage to other organs is also possible, which manifests itself in heart rhythm disturbances, the appearance of skin lesions, in women – mammary glands, the development of uveitis, disruption of the endocrine system, etc.
The most important sign of the disease is the appearance of nodules in tissues, which can be detected by histological examination.
At the first symptoms of sarcoidosis, you should consult a doctor. In any case, an elevated temperature for several days is an alarming sign, and its cause must be found out. The specialist begins the diagnosis by examining the patient and collecting an anamnesis. It collects information about hereditary predisposition to the disease in the family and the presence of dangerous conditions of professional activity.
Assesses the condition of the respiratory system and looks for specific skin defects such as lupus pernio, sarcoid plaques or erythrema nodosum. The combination of these signs with problems of the bronchopulmonary system often indicates sarcoidosis.
On X-ray, pulmonary sarcoidosis appears as small tissue lumps
Then the doctor prescribes laboratory diagnostic methods:
- general urine analysis;
- general urine analysis;
- general and biochemical blood test;
- mantu sample;
- blood testing for the presence of elements such as angiotensin-converting enzyme, tumor necrosis factor alpha, copper;
- Kveim-Silzbach test;
- blood and urine testing for calcium levels.
These examinations make it possible to detect an inflammatory process in tissues and often the factor that provokes it (for example, tuberculosis) or to distinguish sarcoidosis from a similar disease. To confirm the diagnosis, instrumental diagnostics are used:
- radiography;
- endoscopy;
- computed and magnetic tomography;
- scintigraphy;
- ultrasound;
- spirometry;
- electrocardiogram and fundus examination if necessary.
As a rule, the doctor uses the diagnostics that are available. More often this is an X-ray examination or ultrasound, equipment for which is available in all clinics. In some cases, accounting for about a third, the disease is asymptomatic and goes away on its own. In other cases, treatment is required.
How to treat sarcoidosis
After the diagnosis is made, all patients are interested in the answer to one question - how to treat sarcoidosis. However, not all of them can accept the fact that doctors are in no hurry to immediately prescribe them active therapy. The fact is that with this disease there is a high probability of spontaneous recovery without taking any pills. Therefore, if a patient is diagnosed with initial sarcoidosis, treatment consists of active observation: the patient comes to the doctor once or twice a year and undergoes the required amount of examinations. If no deterioration is detected, there are no signs of respiratory failure and the person calmly tolerates all normal physical activity, he is simply sent home. However, not all patients go so well; in some cases, sarcoidosis is treated with more active methods.
Sarcoidosis: treatment by a pulmonologist
The most common form of sarcoidosis affects the intrathoracic lymph nodes and lungs. Therefore, most often such patients are seen by a pulmonologist and are under constant supervision. If, as a result of the examination, it is revealed that all granulomas have spontaneously disappeared, then such a patient will be removed from the register after several months or years, which is rare for any chronic disease.
If, according to the results of the examination, it was revealed that the patient’s condition is deteriorating, the pathological process is gradually progressing, respiratory failure is increasing, erythema nodosum has appeared, damage to the eyes, bones, joints, the liver and spleen are greatly enlarged, then the question of how to treat sarcoidosis becomes relevant. In this case, the patient is managed jointly by a pulmonologist and a rheumatologist.
Today, if a patient has sarcoidosis, treatment is carried out with the following drug groups:
- Glucocorticosteroids (prednisolone) are the first-line drug. Initially, high doses are prescribed and gradually reduced after 4-6 months,
- cytostatics (azathioprine, methotrexate) are an alternative to corticosteroids, or are prescribed in cases of intolerance to them, the presence of steroid diabetes,
- bisphosphonates are prescribed to prevent osteoporosis during hormonal therapy,
- other drugs for treatment (pentoxifylline, alpha-tocopherol, chloroquine, inhaled bronchodilators, etc.)
However, there is no specific method of therapy for this disease, that is, all treatment is aimed at relieving symptoms and reducing the activity of the immune system against one’s own body.
If all possible methods of therapy have been exhausted, the patient is in a terminal condition due to progressive severe respiratory failure, then the only answer to the question of how to treat sarcoidosis in this case is one - donor lung transplantation. In our country, transplantation is not developed, so such patients often do not live to see the moment when they are invited for surgical treatment.
Is traditional treatment for sarcoidosis acceptable?
The answer to the question of whether alternative treatment for sarcoidosis is acceptable is not as simple as it seems at first glance. The fact is that until the patient feels well, doctors do not seek to prescribe him medications, since a large percentage of people experience spontaneous remission or get better altogether. However, not everyone is willing to sit and wait to see what his fate will be. Some patients choose traditional treatment for sarcoidosis, which is usually represented by various herbs, breathing exercises and other alternative options. But none of them is able to influence the prognosis, and if the patient does recover, it will certainly not be from such treatment, although he will be more confident of a favorable outcome.
Thus, if we consider the alternative treatment of early stage sarcoidosis as a possible “placebo effect”, which is known to work in 30-60% of patients, then it will not make you worse. However, if the patient’s condition quickly deteriorates and there is a need to prescribe basic therapy, then abandoning it in favor of alternative therapy is very risky.
Complications and prevention
If sarcoidosis is not treated in time, the development of other diseases that occur in the respiratory tract develops against the background of weakening of the body of the VGLU. Tuberculosis is considered one of the serious complications. Also, with accelerated inflammation, lung collapse and diffuse pneumosclerosis occur. Malfunctions in the body's functioning lead to disturbances in calcium metabolism, which can lead to the formation of kidney stones.
In an advanced form of the disease, when there is severe dysfunction, the patient may be given a disability.
For preventive purposes, quitting tobacco products is important. A healthy lifestyle has a positive impact. You should take vitamins and eat healthy foods. It is necessary not to skip medical examinations and be examined by doctors of narrow specialties.
Complete cure of the disease is possible if detected in the early stages of its course. The disease may slow down its development and not manifest itself for a long time. An advanced form of sarcoidosis leads to oncology, even death.
How long do people with sarcoidosis live?
Patients often ask doctors how long people with sarcoidosis live. However, there is no answer to this question. Most live long lives because the disease rarely causes life-threatening conditions. The prognosis depends on many parameters: the nature of the course, the extent of the pathological process, the initial state of health. In each case, the outcome will be individual.
Is disability common in pulmonary sarcoidosis?
Whether pulmonary sarcoidosis causes disability is another problem that can occur in people suffering from this disease. You should know that this disease is rare, people rarely suffer from it, and recovery can occur even without the use of drugs or folk remedies. Complications that are dangerous to health or even life rarely occur, and most often the heart, respiratory organs, and kidneys are affected. It is the pathologies of these important human organs that can cause disability.
To obtain disability, it is necessary to provide not only information about the treatment, but also all x-rays confirming that it was the damage to the lung tissue that caused the pathology of important organs. Only in the case of severe complications is disability possible, but it is usually attributed to another disease that arose as a result of damage to the respiratory tract.
Forecast
Prognosis for pulmonary sarcoidosis should be treated with caution. On the one hand, a benign course of the disease and self-healing may occur, on the other hand, the disease is diagnosed too late, when changes have developed in the lungs that are incompatible with their normal function.
The prognosis for pulmonary sarcoidosis is favorable in the case of preclinical diagnosis of the disease (that is, before the onset of symptoms) and timely, well-calibrated treatment. Lung complications caused by sarcoidosis do not occur as often as with other diseases of the respiratory system. But you should beware of complications that arose at stages 3-4 of pulmonary sarcoidosis - they worsen the prognosis.
Death can occur with the development of severe complications - in particular, respiratory failure.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
12, total, today
( 172 votes, average: 4.59 out of 5)
Pneumococcal pneumonia: causes, symptoms, treatment, prevention
Hydrothorax: causes, symptoms, treatment principles
Related Posts
Signs of sarcoidosis of the lungs and lymph nodes
Characteristic symptoms of the pathology are weakness, hypertrophy of nodes and cough. Over time, respiratory and cardiac disorders develop. Occasionally the temperature rises to 39°C. This sign indicates that there is an acute inflammatory process in the body.
As the disease progresses, the patient notices a decrease in body weight. This is caused by inflammation and metabolic disorders. The state of health deteriorates significantly and the absorption of nutrients decreases. In addition, lymphadenopathy is observed in sarcoidosis. On palpation, the nodes are dense, not fused.
Sarcoidosis of the intrathoracic lymph nodes is characterized by the appearance of granulomas in the mediastinal nodes. As a result of the enlargement of the inflamed lymph nodes, compression of the bronchi and bronchioles occurs. The patient experiences respiratory problems that worsen after any physical activity. A compensatory mechanism for dilation of the bronchi is activated, but due to granulomas and hypertrophy of the lymph nodes, an increase in air volume does not occur.
Complications
Complications are observed with rapidly progressing untreated sarcoidosis (when there is doubt about the diagnosis and treatment has not yet been prescribed), as well as with its advanced forms. Most often, they were observed in patients who ignored preventive examinations for a long time and refused to do chest fluorography.
The most common complications of pulmonary sarcoidosis are:
secondary pneumonia (bacterial, viral or mycotic);
- pulmonary hypertension (increased blood pressure in the pulmonary artery system);
- addition of infection and development of secondary pneumonia;
- development of the pulmonary heart (expansion of its right sections due to an increase in blood pressure in the pulmonary circulation);
- acute and chronic respiratory failure, which can occur with any complications of pulmonary sarcoidosis.
Causes
The cause of the disease is currently not fully understood. But it has already been proven that the disease is not infectious in nature. Can you get sarcoidosis? Based on the non-infectious nature of the disease, we can confidently answer that it is impossible. Nevertheless, the following factors may be the impetus for the development of pathology:
- genetic predisposition to the development of the disease. If one of your relatives had this disease, then the likelihood of its development in subsequent generations is high;
- impaired immune response to invasion of the body by various viruses and bacteria;
- tuberculosis;
- HIV infection;
- side effect of long-term use of interferon and antiretroviral drugs;
- air pollution with dust particles (found among firefighters, miners, library and publishing workers), or particles of metals - copper, aluminum, zirconium, titanium, gold, cobalt, beryllium;
- smoking.
Young people aged 20-29 years are at risk; women are more likely to suffer from sarcoidosis.
Causes and mechanisms
Until now, the exact reasons that trigger the formation of nodules in the lungs are unknown, although intensive research has been conducted in this field for decades. Most doctors are inclined to believe that sarcoidosis is:
- not a cancer disease (due to the similarity of the names, patients confuse it with lung sarcoma);
- not an infectious lesion (contrary to the stereotypes of some patients, it is impossible to get infected from others - the associated infectious process in the nodules is a secondary phenomenon that is not transmitted from a sick person to a healthy one).
Doctors have more than once described familial cases of sarcoidosis - this “familiality” was explained:
- heredity;
- the influence of identical unfavorable environmental factors in which representatives of the same family live (this factor is disputed).
Local outbreaks of pulmonary sarcoidosis are periodically observed. But the data is insufficient to officially confirm the occupational and contagious risks of this disease.
note
One of the most frequently considered theories for the occurrence of pulmonary sarcoidosis is that the disease develops due to the inhalation of an unknown environmental agent, which begins to interact with the immune system, and it gives rise to the formation of nodules in the pulmonary parenchyma.
The role of such an agent is most often attributed to:
- Koch's bacillus (the causative agent of tuberculosis);
- viruses (in particular, representatives of the herpes group);
- some mushrooms;
- mycoplasmas (a type of bacteria that most often affects the genitourinary system).
These assumptions raise questions - for example, why in some cases does Koch's bacillus provoke tuberculosis, and in others - sarcoidosis without isolating the pathogen in pathological nodules? And why, with pronounced clinical manifestations, do they not become infected by contact with a sick person? Due to many inconsistencies and unconfirmed, although reasonable, assumptions, sarcoidosis continues to remain one of the main “dark horses” in medicine.
Also, some chemical elements are considered as agents that provoke the occurrence of sarcoidosis:
- zirconium;
- silicon;
- beryllium.
The first two elements cause local reactions such as the formation of granulomas, but not systemic ones. And beryllium provokes the formation of nodules in the lungs, as in sarcoidosis, but without the immunological changes characteristic of sarcoidosis.
Scientists still cannot explain the fact that sarcoidosis is more common among non-smokers than smokers, regardless of smoking history.
Progress in the study of sarcoidosis is a clear understanding that the disease is associated with the immune reactions of the human body. The appearance of nodules (or tubercles) in the lungs is associated with the immune system - macrophages (cells that attack foreign elements that enter the body and devour them) and T-helpers (a type of lymphocytes that help the immune system fight negative factors, “signaling " about the presence of these factors - in particular, microorganisms, foreign proteins, and so on). Essentially, pulmonary sarcoidosis is lymphocytic alveolitis - a lesion of the alveoli associated with the presence of lymphocytes, which are abundant in the mentioned nodules.
The immune system in sarcoidosis behaves quite contradictorily:
- the level of cellular immunity is increased (that is, there are enough cells in the body that can attack and destroy foreign agents, regardless of the origin of these agents);
- the level of humoral immunity is reduced (the number of antibodies in the body that fight only certain enemy agents decreases).
Treatment
Having confirmed the diagnosis of sarcoidosis of the lungs and intrathoracic lymph nodes, treatment is prescribed based on the symptoms.
Considering the inflammatory-proliferative nature of the disease, basic therapy is carried out with corticosteroids, which effectively suppress both inflammatory phenomena and the formation of granulomas.
With the proliferation of lymphoid tissue, to reduce the impact on the course of the disease from the main source - sarcoidosis of the intrathoracic lymph nodes, treatment is usually supplemented with cytostatics, for example, Methotrexate.
Surgical intervention for this pathology is not very effective. Even radical excision of lymph nodes does not guarantee the possible appearance of granulomas in the future.
The intervention of a surgeon is justified only for the correction of life-threatening conditions: excision of areas of atelectasis or areas of emphysema, restoration of patency of the bronchial tree when blocked by granulations.
Symptoms of pathology
Symptoms of sarcoidosis are nonspecific, but they are worth paying attention to. The earlier the disease is identified, the greater the chances of reducing the harmful consequences of the pathology.
Sarcoidosis is accompanied by the following symptoms:
- weakness, especially in the morning;
- chronic fatigue syndrome;
- weight loss for no apparent reason;
- temperature up to 38 degrees;
- inflammation of the lymph nodes in the lungs.
More specific symptoms appear depending on the location of the disease. Thus, sarcoidosis of the liver can only manifest itself as an enlargement of the organ, and external symptoms are only of a general nature. Due to ocular sarcoidosis, disability may even occur - a person may lose vision. The disease very rarely leads to death, but reduces the quality of life.
Cutaneous sarcoidosis typically manifests as erythema nodosum. This change in the condition of the skin is often the first symptom of the disease. Cardiac sarcoidosis is characterized by rhythm changes, organ enlargement, and can be life-threatening. Unfortunately, this pathology is often diagnosed posthumously.
Diagnosis of the disease
With a simple examination, it is not possible to formulate an accurate diagnosis.
The disease can be diagnosed by X-ray of the lungs, CT and MRI of the lungs. With these research methods, one can notice a tumor enlargement of the lymph nodes, a “backstage” symptom (superimposition of the shadows of the lymph nodes on one another), and focal dissemination. Also, the acute course of the disease can be seen from blood test indicators, which indicate an inflammatory process. The initial increase in α- and β-globulins, during the development of the disease, changes to an increase in the content of γ-globulins. Data from lymphocytosis of bronchoalveolar lavage fluid (BAL) are used, but the reliability of this method in sarcoidosis may be low.
Also, most patients may experience a positive reaction to the Kveim-Selzbach test - the appearance of a dark red nodule after the introduction of a specific antigen under the skin.
Bronchoscopy and biopsy reveal various signs of sarcoidosis - dilated vessels in the mouths (roots) of the lobar bronchi, enlarged lymph nodes in the bifurcation zone.
But the most informative way to determine sarcoidosis is a histological study of a biopsy sample, which is obtained if a bronchoscopy, prescalal or open biopsy (for tumor markers), or puncture is performed.
Don't waste your time searching for inaccurate cancer treatment prices
*Only upon receipt of information about the patient’s disease, a representative of the clinic will be able to calculate the exact price for treatment.
Important! If sarcoidosis is diagnosed in a pregnant girl, this cannot be considered a reason to terminate the pregnancy, since this disease does not affect the fetus.
Why does sarcoidosis occur?
The disease is not infectious, and the causes of sarcoidosis are not fully understood.
The study revealed that lymphocytes in sarcoidosis exhibit unusual activity and produce specific substances that cause the formation of granulomas. Although sarcoidosis is a multisystem (affecting many organs) disease, the lungs are affected in 90% of cases. Women get sick more often than men, mainly at a young age. The study revealed that there are factors whose presence can provoke the disease.
These factors include:
- Heredity factor.
- The presence of reduced immunity and autoimmune reaction.
- Harmful environment.
- The presence of a focus of infection and chronic diseases.
- Allergic conditions.
There are also risk groups, which include people in certain professions who are more likely to develop sarcoidosis than others. These include:
- Doctors and other medical workers.
- Teachers of schools, colleges and universities.
- Agricultural workers.
- Firemen.
- Military personnel (especially naval aviation).