Treatment and prevention of cervicitis. Effective drugs for cervical inflammation. Exclusively for the site svetulka.ru
Cervicitis is an inflammatory process in the cervix, its lower section located in the vagina. The cervix is a natural obstacle to the penetration of pathogenic bacteria into the uterus and its appendages.
The barrier function is ensured by the narrow opening of the cervical canal connecting the uterine cavity with the vaginal cavity, and the presence of cervical mucus, the viscosity of which depends on the phase of the menstrual cycle.
Under unfavorable factors, the protection weakens, which makes the woman’s genitals vulnerable to attack by bacteria and viruses and provokes inflammation. Since the vulva, vagina and cervix are a single unit, cervicitis rarely occurs as an independent disease.
Most often it is accompanied by an infectious and inflammatory process in other parts of the female genital organs: vagina, uterus, ovaries, tubes. By itself, it may not cause any discomfort in a woman and may be discovered by chance when taking a smear for flora.
Causative agents of cervicitis
Cervicitis is common among girls and women aged 16 to 35 years who are sexually active. The causative agents of the disease are nonspecific flora - opportunistic bacteria (staphylococci, streptococci, E. coli, enterococci, etc.) and sexually transmitted infections (chlamydia trachomatis, ureaplasma urealyticum, mycoplasma hominis, genitalium, trichomonas, gonococcus), sometimes viruses and anaerobic microflora (gardnerella , fusobacteria, bacteroides, etc.).
Conditional pathogens penetrate the vagina and cervix from the intestines or through the blood and lymph flow, and are specifically infected during sexual intercourse. Infections, especially hidden ones, sometimes remain in a woman’s cervical canal for years without causing inflammatory processes, but when the immune system is weakened, they can make themselves felt at any time in the form of colpitis, cervicitis, adnexitis, endometritis and other diseases of the pelvic organs.
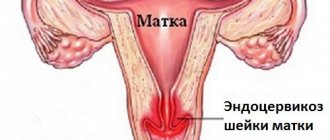
Endocervicitis: treatment with folk remedies complements drug therapy
Inflammatory processes of the reproductive system organs occur quite often in women, and one of them is endocervicitis. Treatment with folk remedies does not replace the use of medications, but only complements their effects. However, before you start using them, be sure to consult your doctor about this.
Drug therapy
The development of inflammation of the cervical canal is caused by staphylococci, streptococci, E. coli, trichomonas, corynebacteria, ureaplasma, mycoplasma, chlamydia and other microorganisms. Therefore, at the first stage, antifungal, antibacterial, antichlamydial or antitrichomoniacal agents are prescribed. For fungal infections, the following are indicated:
For chlamydial infection, drugs from the group of tetracycline antibiotics are prescribed. These include metacycline, doxycycline and tetracycline. Macrolides (azithromycin, josamycin), quinolones (ofloxacin) can also be used. Treatment is supplemented with topical preparations (dimethyl sulfoxide, chlorophyllipt), which are used to treat the cervix.
If endocervicitis is a manifestation of the atrophic process that occurs due to a lack of estrogen in a woman’s body, then estriol is used. This product contains natural female sex hormone.
When treating cervicitis, combination drugs can be used, which, for example, include terzhinan. The latter is produced in the form of vaginal tablets that contain:
In rare cases, allergic reactions may occur when using terzhinan. Some women experience irritation and a burning sensation at the beginning of treatment.
Together with such drugs, vitamins and immunomodulators are prescribed - agents that stimulate the functioning of the immune system. Isoprinosine is a synthetic drug that increases the body's immune defense and has antiviral properties. Its contraindications include:
At the second stage of treatment, it is necessary to restore the normal microflora of the vagina. For such purposes, eubiotics are used - preparations that contain certain microorganisms.
Acylact belongs to this group. It contains acidophilic lactobacilli. These microorganisms are active against various opportunistic and pathogenic microorganisms. The drug is available in the form of vaginal suppositories, stimulates the growth of its own microflora and reduces the frequency of re-development of the infectious process.
The use of folk remedies
They can be used after consulting a doctor. Such remedies do not replace drug treatment and, if used, only complement it.
Folk remedies should not be used as an independent method of therapy. This can lead to further progression of the inflammatory process and deterioration of women's health.
Recipes from traditional medicine are used only in cases where there are no acute manifestations. The most common means include:
They are used both independently and in combination with each other. Methods of using these funds include the following:
During treatment, you should abstain from sexual activity and take special care of your personal hygiene. It is also recommended to wear underwear made from natural fabrics.
Traditional medicine recipes can be used only after the permission of the attending physician. In this case, the main method of treatment for endocervicitis will be drugs prescribed by a specialist, and folk remedies only complement them.
Have you been diagnosed with endocervicitis?
Yes, unfortunately, I’m currently undergoing treatment 20 29 29 0
Source: https://teammy.com/notes/273122print
Symptoms of cervicitis
Symptoms of cervicitis may often be absent, and their presence depends on the stage of the disease and its causative agent. Common signs of inflammation of the cervical canal may be pain in the lower abdomen, profuse vaginal discharge, sometimes with an unpleasant odor, itching, and burning. Gonococcal cervicitis usually occurs with an acute clinical picture (profuse purulent discharge, pain, difficulty urinating).
Cervicitis caused by herpes is also difficult to miss. The cervix is strongly hyperemic, loose, and ulcerated. When the cervix is affected by Trichomonas, multiple hemorrhages in the cervical canal and copious watery discharge, accompanied by a burning sensation, are observed. Viral cervicitis (caused by HPV) can be characterized by the formation of condylomas. Chlamydial, ureaplasma, mycoplasma infections can be asymptomatic or have mild symptoms.
Untreated or improperly treated cervicitis progresses to the chronic stage. With chronic cervicitis, the symptoms are usually mild. A woman complains of mucous or purulent-mucous discharge, pain during sexual intercourse. Upon examination, the doctor diagnoses swelling, redness and thickening (hypertrophy) of the cervical mucosa, and the appearance of erosion.
Often, a chronic inflammatory process in the pelvis leads to disruption of the menstrual cycle, the appearance of intermenstrual bleeding, the release of a small amount of blood after sexual intercourse, the formation of cysts on the cervix and the spread of inflammation to nearby tissues.
Traditional treatment
1. For candidiasis:
take 20 grams of juniper, sage, tansy, birch buds, 10 grams of yarrow, eucalyptus, alder cones. Brew two tablespoons of the mixture with 200 ml of boiling water, steam in a sealed container for 10 minutes, set aside from heat for half an hour, pass through a sieve and consume 70 ml in the morning, at lunch and in the evening after a meal. Duration of treatment is 4 – 12 weeks. For douching at night, add 10 ml of an alcohol preparation of eucalyptus or calendula to the prepared decoction. Do the procedure every day for 14–21 days.
2.
For viral etiology:
take 20 grams of mint, thyme, raspberry leaf, juniper cones, 10 grams of wormwood and adonis.
Brew 2 tablespoons of the collection into 400 ml of boiling water, keep covered for 60 minutes, pass through a sieve and consume orally the day before. It can be combined with oral tincture of Eleutherococcus, 40 drops twice a day ( not at night
) for a month.
3.
Take the same amount of wormwood, oak bark, bird cherry flowers, twice as much strawberry leaf and three times as much rose hips. Grind everything in a coffee grinder, take 1 liter of boiling water for 2 tablespoons of the mixture, and leave in a thermos for 8 hours. Drink 100 ml three times a day on an empty stomach. Duration of treatment is 12 – 16 weeks.
Types of cervicitis
The classification of cervicitis depends on various factors.
The following types of cervicitis are distinguished:
1. By localization
- exocervicitis (inflammatory process in the vaginal part of the cervix, i.e. outside);
- endocervicitis (inflammatory process in the inner lining of the cervical canal, i.e. inside).
2. According to the clinical picture
- acute cervicitis (has an acute manifestation)
- chronic cervicitis (usually erased)
3. By method of injury
- focal (focal lesion)
- diffuse (mixed)
4. Depending on the pathogen
- specific cervicitis (caused by sexually transmitted infections)
- nonspecific cervicitis (caused by the proliferation of opportunistic microflora)
- mixed cervicitis (caused by the presence of sexually transmitted infections and opportunistic microflora)
Sex with cervicitis
Often, sexual intercourse with cervicitis causes inconvenience and discomfort.
If this is not observed and if the inflammation is not associated with the presence of a sexually transmitted infection in the body, sexual intercourse is not prohibited. An infectious inflammatory disease of the cervical canal mucosa, lasting two months or more. It is characterized by scanty clinical symptoms: an increase in the amount of mucous vaginal discharge with the appearance of pus in it and nagging pain in the lower abdomen. To diagnose endocervicitis, speculum examination, extended colposcopy, transvaginal ultrasound, and laboratory tests are used. During treatment, etiotropic antimicrobial agents, eubiotics, immunocorrectors, and physiotherapy are prescribed. According to indications, minimally invasive surgical interventions, tracheloplasty and radioconization are performed.
Causes of cervicitis
What causes cervicitis? There are quite a few reasons for the development of the inflammatory process in the cervix. First of all, this is infection with sexually transmitted infections, disruption of the vaginal microflora, uncontrolled use of antibiotics, use of an intrauterine device, frequent douching, improper genital hygiene, ovarian dysfunction, and hormonal disorders.
Also, cervicitis is caused by cervical ruptures during childbirth, abortion, diagnostic curettage, leading to irreversible scar changes, ectropion (cervical inversion), uterine prolapse, benign formations, severe stress, decreased immunity. The allergic nature of the occurrence of cervicitis cannot be ruled out, for example, a reaction to lactex (condom), components of vaginal suppositories, spermicides, etc.
Treatment of chronic endocervicitis
With a confirmed diagnosis of chronic inflammation of the endocervix, a comprehensive etiopathogenetic approach is recommended. Conservative therapy is preferable, the main objectives of which are:
- Elimination of the source of infection
. Taking into account the sensitivity of the causative agent of the disease, antibiotics, antifungals, antitrichomoniacal, antichlamydial and other agents are prescribed. Usually, oral administration of drugs and their parenteral administration are supplemented with local effects (vaginal suppositories, etc.). - Restoration of the vaginal biocenosis
. Due to chronic inflammation and the use of antimicrobial agents in the vagina, the normal balance of microorganisms is disrupted. Timely administration of eubiotic drugs helps prevent relapses of endocervicitis and activation of opportunistic flora. - Immune corrective therapy
. Since immunodeficiency often becomes the background for the development of the disease, patients are shown vitamin-mineral complexes and immune stimulants. Their use makes it possible to increase general and local resistance to infectious agents, as well as normalize the immune response.
In the treatment of chronic endocervicitis, a combination of medication and physiotherapy is effective. Physiotherapeutic techniques enhance the anti-inflammatory effect of antibacterial agents and accelerate repair processes. Patients are prescribed low-frequency and high-frequency magnetic therapy, magnesium electrophoresis in the uterine zone, diadynamic currents, UHF, vaginal laser therapy, darsonvalization through a vaginal electrode, and mud tampons. In some cases, conservative treatment of endocervicitis is supplemented with surgical methods. If a large number of nabothian cysts are detected, in which the pathogen can persist, diathermopuncture is performed. For persistent cases, cryodestruction, laser vaporization, and radiocoagulation are indicated. If chronic inflammation is combined with cervical deformation, epithelial dysplasia or elongation, radioconization and tracheloplasty may be performed.
Diagnosis of cervicitis
Very often, cervicitis is asymptomatic, which complicates its diagnosis and, accordingly, treatment, because not all women visit a gynecologist for prevention, although most often the disease is discovered during a preventive examination and tests. A diagnosis of cervicitis is made based on the following tests and studies:
- gynecological examination
The doctor examines the woman’s genitals using special gynecological mirrors for suspicious formations on the cervix (polyps, condylomas, erosions), swelling, and pathological discharge.
- microflora smear (microscopic examination)
Shows the presence of an inflammatory process in the cervical canal (increased leukocytes in the smear), identifies some possible pathogens of the disease (Trichomonas, Candida, Gardnerella, gonococcus), shows a violation of the microflora (mixed, coccal flora).
- cytology smear (Pap test)
A smear for oncocytology allows one to diagnose the presence of atypical cells (precancer or cervical cancer) in a woman at a very early stage.
- culture for microflora and sensitivity to antibiotics
Bacterial culture on the flora allows you to identify opportunistic pathogens of cervicitis (Escherichia coli, staphylococci, streptococci, enterococci, etc.)
- PCR diagnostics for STDs (sexually transmitted infections)
Taking a scraping from the cervical canal to determine whether the patient has a hidden infection (sexually transmitted diseases) that may be the cause of cervicitis. It is necessary to be examined for such sexually transmitted infections as chlamydia trachomatis, ureaplasma urealyticum, mycoplasma hominis, mycoplasma genitalium, human papillomavirus, trichomonas, gardnerella, herpes virus.
- colposcopy
Examination of the cervix and vagina using a special optical device - a colposcope - under magnification. If necessary, during colposcopy, the doctor can also take material for examination (biopsy).
Pregnancy and cervicitis
Pregnancy against the background of cervicitis threatens premature birth or miscarriage, infection of the unborn child, as well as severe complications after childbirth.
The most common and dangerous is the ascending route of infection, when it enters the body through the vagina. This is how amniotic fluid can become infected. If the fetus is infected in the early stages of development, there is a possibility of the formation of congenital defects, as well as placental insufficiency. If infection occurs later, fetal development may be delayed. When the fetus becomes infected in the first three months of pregnancy, the infection covers the entire body of the unborn child.
During pregnancy, cervicitis often occurs in a latent form, which complicates its detection.
azithromycin) is used as the main drug in the treatment of an atypical form of inflammation in pregnant women
) in the form of tablets and topical preparations.
Treatment of cervicitis
Treatment of cervicitis depends on the cause of its appearance, the causative agent of the disease and the severity of the inflammatory process. Typically, therapy consists of prescribing systemic or local antibacterial and antimicrobial, sometimes antiviral drugs to suppress the activity of pathogenic microorganisms and drugs to restore the intestinal flora and vaginal microbiocenosis.
For chronic recurrent cervicitis, the use of immunomodulators and physiotherapeutic treatment is also recommended. The hormonal cause of cervicitis requires correction of the hormonal status by a competent gynecologist-endocrinologist.
It must be remembered that the course of treatment for gynecological diseases must always be completed to the end, especially with regard to antibiotics. Many patients, having felt improvement, quit treatment, which is a big mistake. The infection is not killed, but acquires resistance (resistance) to the group of antibiotics used for treatment, which precludes the possibility of their use in the future.
Also, during treatment of an infectious-inflammatory process, it is necessary to abstain from sexual intercourse, even using a condom, not only to avoid the risk of re-infection, but also since many vaginal suppositories have a destructive effect on latex.
Treatment methods for cervicitis in gynecology
1. Antibiotics and antimicrobials for the treatment of cervicitis.
With a slight inflammatory process in the cervix caused by nonspecific flora, it is usually sufficient to sanitize the vagina with anti-inflammatory antibacterial suppositories and broad-spectrum vaginal tablets (Terzhinan, Polizhinaks, Hexicon, Elzhina, Betadine, etc.)
If a patient is diagnosed with acute cervicitis, or cervicitis accompanied by a more severe disease (endometritis, adnexitis, etc.), after identifying the pathogen, systemic antibiotic therapy is prescribed. If opportunistic flora is detected, an antibiotic is prescribed according to sensitivity culture (most often these are Amoxiclav, Ceftriaxone, Levofloxacin, Tsiprolet, etc.).
Vaginal suppositories include Hexicon, Macmiror complex, Elzhina, Fluomizin, Polygynax, etc. You can also treat the cervix with a diluted solution of Chlorophyllipt alcohol, Miramistin, Normoflorins. If cervicitis is caused by sexually transmitted infections, the patient is recommended to be treated together with her sexual partner.
Most often recommended are Vilprafen Solutab, Unidox Salutab, Levofloxacin, etc., depending on the pathogen. Trichomonas cervicitis is treated with Trichopolum, Klion-D tablets and Terzhinan, Fluomizin, Ginalgin suppositories. For cervicitis of a fungal nature, Flucostat, Mikosist and analogues are prescribed, as well as effective vaginal suppositories for thrush - Pimafucin, Neo-Penotran, Livarol, Ginezol, etc.
Herpetic inflammation is controlled by antiviral suppositories Viferon, Genferon, taking Acyclovir, vitamins, and immunostimulants. It is also recommended to irrigate the vagina with Miramistin, Panavir or Epigen-intim sprays. If HPV is detected after removal of condylomas, complex immunostimulating treatment (injections, suppositories) is carried out. As a preventative measure, the use of Epigen spray is recommended.
To treat allergic cervicitis, eliminating the allergen is usually sufficient. For swelling, you can take any antihistamine (Zyrtec, Suprastin, etc.). Atrophic cervicitis, caused by a lack of estrogen, involves the local use of hormonal ointments (for example, Ovestin), which restore the epithelium of the vaginal mucosa.
2. Preparations for restoring intestinal and vaginal microflora.
Vagilac, Provag capsules or Femilex suppositories with lactic acid, Latozhinal, Laktonorm, etc. will help restore the vaginal flora after treatment with antibiotics and antimicrobial suppositories. It is also worth taking care of the intestines; for this, Normoflorin, Bifiform, Hilak Forte and other drugs with beneficial bacteria are prescribed.
3. Immunomodulators for the treatment of cervicitis.
In the chronic course of cervicitis, to maintain immunity in the fight against infections, gynecologists prescribe immunomodulatory drugs to patients. The most popular among them are Galavit, Genferon, Polyoxidonium, and Epigen Intim spray to maintain the immunity of the mucous membranes of the genital organs.
4. Physiotherapy for chronic cervicitis.
For patients who are often diagnosed with cervicitis, or the disease is accompanied by complications, it is also recommended to undergo 7-10 sessions of physiotherapeutic treatment: magnetic therapy, laser, acupuncture, darsonvalization, mud therapy, etc.
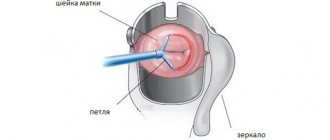
5. Surgical treatment of cervicitis.
Advanced cervicitis sometimes requires surgical intervention - laser cauterization, cryodestruction, diathermocoagulation, etc. These methods of treating cervicitis are used after stopping the inflammatory process and eliminating the infection. At the same time, treatment of concomitant gynecological diseases is carried out.
Treatment of cervicitis in pregnant women
How to treat cervicitis during pregnancy? Treatment of cervicitis in women who are pregnant or breastfeeding is complicated by the fact that it is necessary to select drugs and suppositories that do not have a negative effect on the child. But nowadays, in principle, there are a large number of antibiotics and vaginal suppositories approved for pregnant and nursing mothers; the main thing is to correctly determine the causative agent of the disease and sensitivity to the drugs.
Most often, for the treatment of inflammation in gynecology during pregnancy and breastfeeding, vaginal tablets Terzhinan, Fluomizin, Polygynax suppositories (with caution), Hexicon, Pimafucin, Clotrimazole are prescribed. Among antibiotics, penicillins, some cephalosporins, and macrolides are allowed as prescribed and under the supervision of a physician. After completion of therapy, it is also necessary to restore the intestinal and vaginal flora with the previously listed drugs.
Inflammatory process of the mucous membrane of exocervicitis - what suppositories or drugs are used for treatment?
If a woman has signs or symptoms of inflammation of the vaginal neck, she should immediately contact a gynecologist, who, after examination and laboratory tests, will prescribe effective treatment. First of all, it will be aimed at neutralizing and eliminating the causative agent of the disease.
- If the cause of inflammation is candidiasis, then the doctor prescribes antifungal suppositories, for example, Nystatin.
- Antiviral suppositories, such as Acyclovir, are recommended if you need to eliminate a viral infection.
- If the disease occurs due to the proliferation of bacteria, then to eliminate the disease exocervicitis, the following suppositories for treatment will be prescribed: Terzhinan or Betadine. The choice of a specific drug depends on the general clinical picture of the disease.
- In some cases, the patient is prescribed the use of combined drugs that have an antibacterial and anti-inflammatory effect. Such a representative of the pharmacological market is terzhinan for exocervicitis.
- Hormonal suppositories are an effective treatment for the chronic form of the disease, in which the mucous membrane of the cervix thickens. In such situations, Ovestin vaginal suppositories are most often preferred. A similar product is also sold in tablet and cream form.
Complications of cervicitis
If the causative agent is correctly identified, cervicitis usually responds well to treatment. Complications of cervicitis can include: the appearance of cervical erosion, polyps, endometritis, adnexitis, pregnancy complications, intrauterine infection of the fetus, premature birth. These complications can subsequently cause infertility, so any gynecological diseases require careful diagnosis and proper treatment.
Surgery
If cervicitis develops against the background of severe deformation of the cervix due to scars or ruptures, it can be treated with surgery. Minimally invasive surgery is also used for the combination of cervicitis and background or precancerous diseases of the cervix - pseudo-erosion, leukoplakia, polyps, dysplasia of varying severity. Most often in these cases, knife conization of the cervix is performed - removal of part of the cervix along with the cervical canal. This operation can be performed using laser or radio wave surgery.
If cervicitis is combined with diseases of the uterus or appendages (for example, large fibroids), then in postmenopausal women the uterus can be removed, sometimes along with the ovaries and fallopian tubes.
Indications for use
To restore the natural microflora of the vagina during cervicitis, suppositories are used as an auxiliary remedy. It is impossible to eliminate the pathology with their help; the action of the drugs is aimed at suppressing the symptoms of the disease. Suppositories have the following effects:
- Relieving inflammation.
- Reduced pathogen activity.
- Removal of the affected epithelium.
- Normalization of discharge.
- Relief of pain syndrome.
- Activation of the regeneration process.
- Prevention of penetration of additional pathogens into the mucosa.
The use of suppositories is also recommended in cases of contraindications to oral administration of the drug due to concomitant diseases of the digestive or excretory system. The drug acts locally without being absorbed into the blood.
In this situation, it should be borne in mind that suppositories are not as effective as other treatment methods, so it is necessary to take additional measures to prevent the development of complications.
Vaginal suppositories are also prescribed as a course to prepare the vaginal environment for surgery.
Diclofenac: rectal suppositories for cervicitis
A suppository called Diclofenac is usually prescribed to relieve pain caused by an exacerbation of cervicitis. Diclofenac will not cure the inflammation itself, but will quickly relieve unpleasant symptoms and help the woman return to normal daily life.
Despite the fact that these suppositories are prescribed for inflammation of the cervix, they must be administered rectally. The main components will reach their goal by being absorbed into the blood. But with vaginal administration, the risk of bleeding will increase.
Using Diclofenac rectal suppositories is as easy as other vaginal medications. You just need to insert the suppository into the rectum, lying on your left side, bending your right knee.
Remain in a lying position for a few minutes, and also restrain the urge to have a bowel movement for an hour to ensure complete dissolution of the suppository. The dosage is selected individually. However, you need to ensure that the daily intake does not exceed 100 milligrams per day
.