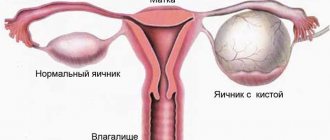
An increase in the number of neoplasms has been observed for quite a long time. The ovary is an organ of the female reproductive system. The frequency of neoplasms in the ovaries and their varieties is particularly numerous. All ovarian tumors are usually divided into benign, malignant and borderline ovarian tumors.
Hormonally active tumors are neoplasms that develop from the endocrine glands and are characterized by excessive release of hormones or the products of their formation.
Hormone-producing tumors can be diagnosed in all glands of the human body. The tumor releases large amounts of hormones, which leads to symptoms and signs of hyperfunction. Hormone-producing tumors can have both a benign and malignant course.
Hormone-producing ovarian tumors are neoplasms that are usually divided depending on the hormone that they secrete. A hormone-active ovarian tumor intensely secretes either estrogens or androgens.
Hormone-active ovarian tumors that secrete estrogen include granulosa cell tumor, theca cell tumor, folliculoma, and tumors that combine several types. The clinical picture of hormonally active tumors caused by hyperestrogenemia is manifested by menstrual irregularities and local symptoms.
Hormone-active androgen-secreting ovarian tumors include arrhenoblastoma, chyle tumors, masculinoblastomas, and combination tumors. The clinical picture is dominated by the phenomena of virilism.
The Yusupov Hospital guards the health of the population around the clock. The wide profile and versatility of the Yusupov Hospital allows it to provide emergency care, diagnose and treat a huge number of diseases. Specialists are not afraid to take on complex cases, to guide patients from the beginning of diagnosis to full recovery, continuing to conduct dynamic monitoring to avoid relapse.
Diagnostic procedures at the Yusupov Hospital are carried out quickly, without queues or waits, and with high quality, because all the equipment is modern, from leading manufacturers. Treatment of diseases, including hormone-producing ovarian tumors, is carried out in conditions of absolute trust and consensus between the patient and the doctors of the Yusupov Hospital. Modern protocols, standards, and individual and effective approaches are used. Knowledge in every industry is growing. Medications are selected for everyone to get the maximum effect from therapy. Specialists work in a team, complementing each other's work.
The wards of the Yusupov Hospital are designed for a number of patients from one (superior ward) to four. There are intensive care rooms equipped to all standards. The nutrition of patients is also selected individually, since patients with cancer already suffer from poor or no appetite, dyspeptic symptoms and stool disorders.
The Yusupov Hospital also willingly treats patients after specific treatment for the fastest and highest quality recovery possible. Signing up for a consultation will help resolve some issues, obtain the necessary information, etc. You can sign up by phone or online.
Causes of hormone-producing ovarian tumors
The etiology of the development of any type of neoplasm is not fully understood. Research is ongoing, but so far achievements will be limited only to identifying possible causes:
- Hormonal disorders. A woman’s hormonal background and a history of pregnancy and childbirth are of great importance. Due to ovulation, ovarian tissue is damaged, which is accompanied by subsequent regeneration. But sometimes such increased cell division becomes pathological. There is no ovulation during pregnancy and breastfeeding, so at this time the risk of developing a neoplasm is significantly reduced. Facts such as early onset of menstruation, late menopause, lack of childbirth and refusal to breastfeed increase the risks.
- Compounded medical history and genetic predisposition. Two percent of neoplasms are associated with this factor. With an unfavorable family history and cancer diagnosis in close relatives, patients have a high risk of developing ovarian cancer. In this case, it is necessary to undergo examination and see a gynecologist.
- Eating large amounts of foods high in carcinogens and animal fats. Statistical data supports this statement due to the study of eating habits in certain countries of the world and their comparison with the incidence of cancer.
The reasons why some tumors produce hormones and others do not remain unknown at this time.
How can you recognize if you have an ovarian tumor?
Often the first symptoms of an ovarian tumor remain unnoticed by a woman or she does not pay much attention to them, which leads to late diagnosis of the tumor, when the process of metastasis begins and neighboring and distant organs are affected. At the same time as the removal of the primary tumor, women have to undergo treatment for cervical cancer abroad or treatment for breast cancer abroad.
You should contact the clinic as soon as possible if you have the following symptoms:
- The appearance of pain in the lower abdomen, iliac and suprapubic region, independent of the menstrual cycle. Such pain can be different: aching, weak, sudden and intense, tingling. The cause of pain can be sexual intercourse, lifting heavy objects, or intense sports activities.
- Disturbed menstrual cycle.
- A girl's puberty begins before the age of 12. Her breasts are enlarged, hair begins to grow in unusual places, and blood appears from the vagina.
Don't wait for these symptoms to appear all at once. If at least one of them or a combination of two signs is present, consultation with a gynecologist is necessary.
As the tumor grows, the early clinical picture intensifies and is supplemented by later signs of the presence of a tumor:
- the urge to urinate becomes more frequent;
- Frequent constipation and flatulence bother you;
- loss of appetite;
- there are constant disruptions in the menstrual cycle.
If a tumor is not detected and treated in time, even if it is benign, there is a risk of developing serious complications: torsion of the tumor stalk, cyst rupture, infection, bleeding, severe pain, peritonitis. These problems can be avoided with regular preventive examinations.
Clinic of hormone-producing ovarian tumors
Estrogen-producing ovarian tumors can be diagnosed at any age: granulosa cell is the most common in children and young girls, and theco cell is the most common during menopause. Granulosa cell tumor develops from granulosa tissue; the structure of thecoma resembles follicular cells. Clinical symptoms and signs in girls:
- early puberty;
- irregular hemorrhagic discharge from the genital opening;
- The vulva is blue, the vagina is folded, the uterus is enlarged in size, the “pupil” symptom is determined.
- Somatic development in this case corresponds to what it should be.
At an older age, with an estrogen-producing ovarian tumor, symptoms of menstruation disorders in the form of dysfunctional bleeding from the uterus come to the fore. Girls experience infertility. In women over fifty, hemorrhagic discharge from the genital tract appears and glandular hyperplasia develops.
Androblastoma is a masculinizing hormone-producing tumor that inhibits the function of the pituitary gland and, as a result, estrogen levels decrease. Clinical signs:
- Lack of menstruation;
- Reproduction disorders in the form of infertility;
- The mammary gland decreases in size;
- The voice becomes rough and low;
- Hair growth changes to male type;
- Libido suffers;
- The clitoris enlarges;
- Body shapes acquire masculine features, etc.
Most often, patients complain of lack of menstruation and reproductive disorders, and sometimes they experience pain in the lower abdomen.
Diagnosis of hormone-producing ovarian tumors:
- Consultation with a specialist with collection of complaints, medical history and life history.
- Bimanual examination.
- Biochemical and clinical tests of blood and urine.
- Determination of CA-125 level in blood serum,
- Determination of the level of sex hormones.
- Ultrasonography.
- Computed and magnetic resonance imaging.
- If necessary, other additional research methods are carried out.
- The final conclusion and diagnosis is made by histological and cytological examination of a biopsy taken through surgery.
Get a free consultation
Leading specialists of the Center will answer your questions.
To get a consultation
Find out the price
What are the types of ovarian tumors?
According to the histogenetic principle, ovarian tumors are classified as follows:
- Epithelial tumors;
- Sex cord stromal tumors;
- Germ cell tumors;
- Follicular cyst. Corpus luteum cyst. (Tumor-like processes).
Within each class of tumors (except for the fourth point) there are benign, borderline and malignant forms.
In addition to possible malignant degeneration, there is a danger of other complications of ovarian tumors:
- torsion of the cystoma leg;
- cyst suppuration;
- hemorrhage into the cyst;
- rupture of the cyst membrane.
The decision on treatment tactics is made in each case individually, depending on the nature of the ovarian tumor, the woman’s age and the results of a special examination.
What are the most common symptoms of ovarian tumors?
Most often, ovarian tumors occur without symptoms.
- Early and relatively constant symptoms of ovarian tumors (benign and malignant) include pain, sometimes very mild, referred to by patients only as “straining” in the lower abdomen, mostly unilateral.
- Sometimes there is a feeling of heaviness in the lower abdomen, constant or periodic abdominal pain without a specific localization, sometimes in the epigastric region or hypochondrium.
- The pain may stop for more or less long periods of time.
- The disease may first manifest itself as sudden sharp pain as a result of torsion of the tumor stalk or rupture of its capsule.
- Relatively early but rare symptoms of the disease include difficulty urinating or bowel function as a result of pressure from even a small ovarian tumor located in front or behind the uterus.
- The first symptom may be an enlarged abdomen or the appearance of a “hardening” in it.
- With malignant ovarian tumors, as well as with the malignancy of benign tumors, at first there are usually no pronounced features of a malignant nature.
The most noticeable symptoms, but not the earliest ones, are:
- deterioration of general condition;
- fast fatiguability;
- weight loss.
Painful sensations are more pronounced, intestinal bloating is more often noted, especially in the upper part, and satiety from small portions of food, which is due to the large volume of the tumor, the appearance of metastases in the omentum and in the visceral peritoneum, creating difficulties in the passage of gases, and the accumulation of ascites (fluid in the abdominal cavity ).
As the tumor grows or ascites increases, the abdomen enlarges and shortness of breath develops. Tumor progression is sometimes accompanied by an increase in body temperature.
Thus, the analysis of subjective and objective symptoms of the disease in cases of both early and advanced stages of malignant ovarian tumors showed that focusing on symptoms cannot serve the purposes of early diagnosis, since symptoms characteristic only of the early stages of the disease have not been identified.
How common are benign tumors?
Benign ovarian tumors (BOT) make up from 66.8% to 80.3% of all ovarian tumors, which is 4 times the number of malignant tumors of these organs.
The most common types of tumors found are germ cell (mature teratoma) and epithelial tumors.
What are the causes of benign ovarian tumors?
Epidemiological factors that determine the spread of tumors of the reproductive system include genetic predisposition, metabolic characteristics caused by the nutritional structure, including the consumption of vitamins A, C, E.
The nutritional factor affects changes in the hormonal status of women. Food rich in fats and proteins leads to stimulation of the endocrine system, changes in hormonal balance towards increasing the content of gonadotropic and steroid hormones of the ovary and, ultimately, to a more frequent appearance of neoplasms in hormone-dependent organs. 36% of patients have various menstrual dysfunctions.
Of the extragenital pathologies predisposing to the development of ovarian tumors (mucinous), the following can be noted:
- obesity;
- diabetes;
- thyroid diseases.
In the anamnesis of patients with benign ovarian tumors, a high frequency of chronic inflammatory processes of the genitals, as well as operations on the pelvic and abdominal organs, was noted.
Late menarche increases the risk of developing benign ovarian tumors. A low risk of benign ovarian tumors is observed with hypomenstrual syndrome and the use of contraceptives.
In addition, risk factors for the occurrence of benign ovarian tumors include:
- lack of sexual activity or its irregularity;
- use of the IUD;
- primary and secondary infertility (after abortion);
- artificial abortions;
- pathology during childbirth;
- use of biogenic stimulants;
- diseases of the gastrointestinal tract, liver, kidneys.
How do benign ovarian tumors develop?
Typically, benign ovarian tumors occur in women under 50 years of age.
At the initial stage of development, the disease is asymptomatic. Subsequently, complaints of dull nagging pain in the lower abdomen, lumbar and groin areas appear. As a rule, pain is not associated with menstruation. They arise due to irritation and inflammation of the serous membranes, irritation of nerve endings, tension of the tumor capsule, and disruption of the blood supply to the tumor wall. If the tumor stalk is twisted and/or ruptures, the pain will be paroxysmal.
Another complaint may be menstrual dysfunction. Complaints of constipation and dysuria usually appear with large tumors. Most often, benign ovarian tumors are discovered during medical examinations, by chance.
Among benign ovarian tumors, dermoid cysts are in first place in frequency. They are characterized by inclusions of mature tissues that are not related to the tissues of the reproductive system (bones, cartilage, skin, teeth).
The incidence of malignancy of dermoid cysts does not exceed 2%, while in 75% of cases this occurs over the age of 40 years. The risk of torsion of the tumor stalk is 15% due to the high mobility of the tumor, which is usually located anterior to the uterus. Both ovaries are affected in 10% of cases. The recommended scope of surgery for dermoid cysts is resection of the ovary within healthy tissue.
The risk of epithelial ovarian tumors increases with age. In women under 50 years of age, serous ovarian cystadenomas are the second most common (66 and 20%, respectively). Serous cystadenomas are usually multilocular, sometimes with papillary growths. Tumor-forming epithelial cells secrete serous fluid that fills the cavities. Mucinous tumors of the ovaries are usually multilocular, with a smooth capsule, bilateral in 10% of cases and can reach significant sizes. The contents of the cysts are mucous.
How are benign ovarian tumors diagnosed?
Diagnosis includes bimanual gynecological examination and pelvic ultrasound.
CT is recommended if a malignant ovarian tumor or a tumor originating from neighboring organs is suspected.
X-ray of the abdominal cavity sometimes suggests the nature of the pelvic mass formation: rare scattered calcifications are characteristic of serous tumors, large shadows for a dermoid cyst.
The diagnostic value of CA-125 for benign ovarian tumors is low, since the marker can also increase in other diseases in women of the childbearing period - uterine fibroids, pregnancy, inflammatory diseases of the uterine appendages, endometriosis.
How are benign ovarian tumors treated?
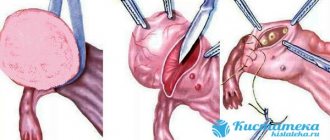
Treatment of patients with benign ovarian tumors is surgical. Laparoscopic operations have found widespread use.
What are the characteristics of ovarian tumors from the sex cord stroma (benign)?
Benign ovarian tumors from the sex cord stroma include ovarian fibromas. The tumor is usually small in size and can have a diffuse form (the entire ovary is affected) and limited form, when the ovarian tissue is partially preserved and the tumor has a pronounced capsule.
Ovarian fibroids most often occur in women near or postmenopausal, but can also occur in younger women.
Fibroids are slow growing and can take 10 years or more to develop. Fibroma is asymptomatic until it reaches a significant size and begins to put pressure on neighboring organs. Fibroids are often accompanied by anemia and ascites may occur.
Treatment is surgical, and in young women it is advisable to limit the removal of only the tumor and preserve reproductive function. The prognosis is favorable.
What are the features of benign epithelial tumors?
Epithelial tumors are the most common benign ovarian tumors.
Epithelial tumors are divided into coeloepithelial (serous) tumors and pseudomucinous tumors.
Coelioepithelial serous tumors form predominantly in elderly women and occur without noticeable symptoms. Treatment is only surgical.
Of all the benign ovarian tumors, coeloepithelial papillary tumors are the most potentially malignant. These tumors mainly occur in women between 20 and 40 years of age, but they also occur after 40.
The clinical picture of papillary tumors is characterized by pain and heaviness in the lower abdomen, and in some cases ascites is possible. Treatment is surgical.
Pseudomucious tumors are the largest ovarian tumors. They usually occur in older women, less often in reproductive age. Women complain of pain, heaviness in the abdomen and an increase in its volume. Treatment consists of removing the tumor.
What are ovarian tumor processes? What are their features (how do they manifest themselves, features of diagnosis and treatment)?
Among ovarian neoplasms, tumor-like processes account for about 30-40%, and true ovarian tumors, respectively, 60-70%.
The most common forms of ovarian tumor formations
Follicular cyst A follicular cyst is formed from an unovulated follicle, in which follicular fluid accumulates and atrophy of the cells lining its inner surface occurs. The size does not exceed 10 cm, and a larger size indicates an ovarian tumor. A follicular cyst tends to develop backwards, and if a follicular cyst is detected, observation of the cyst for some time is indicated before making a decision about surgery.
Corpus luteum cyst A corpus luteum cyst can form as a result of an inflammatory process in the ovaries. In the cells of the wall of the corpus luteum cyst, the same changes are observed as in the menstrual corpus luteum. Most often, the corpus luteum cyst undergoes independent resorption, when the contents dissolve and the cavity collapses. In rare cases, a corpus luteum cyst develops into a corpus alba cyst. The prognosis is favorable.
Paraovarian cyst A paraovarian cyst is formed from the epididymis, located in the mesosalpinx. Paraovarian cysts generally develop asymptomatically and only when large in size can cause mild pain. Treatment is surgical. The prognosis is favorable.
Tubal-ovarian inflammatory cyst Tubal-ovarian inflammatory cyst is formed as a result of fusion of the tube and ovary affected by the inflammatory process. Treatment is surgical. The prognosis is favorable.
What are borderline ovarian tumors?
Borderline ovarian tumors are low-grade tumors. For a long time they do not go beyond the ovaries. Borderline tumors in most cases occur in women aged 30-50 years.
Borderline tumors account for about 10% of all serous tumors. Borderline ovarian tumors can be serous, mucinous, endometrioid, or Brenner tumors. Borderline tumors are staged according to the FIGO (International Federation of Gynecological Oncology) classification adopted for ovarian cancer (OC).
Serous tumors arise as a result of the immersion of the surface epithelium deep into the ovary. Small inclusions called psammoma bodies are often found in serous tumors. If there are papillary growths on the capsule, the tumor is called papillary.
Mucinous tumors account for 8-10% of all epithelial ovarian tumors. These tumors have mucous contents and can reach gigantic sizes, occupying the entire abdominal cavity. In 95% of cases they do not extend beyond the ovaries. To make a correct diagnosis, you should study as many sections as possible.
Endometrioid borderline tumors resemble the endometrium in structure; their histological structure is very diverse.
Borderline Brenner tumors are extremely rare; not a single case of microinvasion or recurrence has been described after radical removal of this tumor. The diagnosis is made, as a rule, by urgent histological examination of the removed tumor.
How are borderline ovarian tumors treated?
The main treatment method for borderline tumors is surgery.
In cases where, with the size of the tumor within stage I, preservation of reproductive function is desirable, unilateral salpingo-oophorectomy with wedge-shaped resection of the contralateral ovary and the infracolic portion of the greater omentum is possible.
In cases of complete removal of the tumor in patients with local forms of the disease and the diagnosis is established based on the results of studying the removed tumor, repeat surgery is not required. Chemotherapy or radiation therapy is not indicated.
In the case of a widespread process (stages II-III), surgical intervention is performed to the extent of extirpation of the uterus and appendages, resection of the greater omentum and cytoreductive measures similar to those carried out for ovarian cancer. Chemotherapy is indicated in cases where invasive tumor implants are identified during surgery (even if they are completely excised). The same chemotherapy regimens are used as for the treatment of ovarian cancer.
Treatment of hormone-producing ovarian tumors
For some types, it is sufficient to resect the formation within healthy ovarian tissue, or unilateral removal of the appendages. In case of malignant lesion, it is necessary to remove the uterus with appendages and omentum.
After removal of the hormonally active tumor, most signs and symptoms will be eliminated and menstrual and reproductive functions will improve.
Further dynamic monitoring, regular examinations and examinations are mandatory.
The Yusupov Hospital works with patients with all types of ovarian tumors. Diagnosis, treatment and recovery at the Yusupov Hospital are carried out efficiently and effectively. You can make an appointment by phone or online.
Author
Natalya Aleksandrovna Vyaznikova
Oncologist
Treatment methods
Identification of an ovarian tumor is a clear indication for its surgical removal. The type of operation performed will be selected for each patient individually, depending on the nature of the lesion, the size of the formation, the patient’s age and her reproductive status.
Most often, in this condition, an operation called adnesectomy is practiced. Ovarian resection and laparoscopy may also be performed.
In advanced cases, complete removal of the uterus is performed. This will avoid a recurrence of the pathology, but at the same time it will forever deprive the woman of the opportunity to carry and give birth to a child on her own. That is why such an operation is performed as a last resort for women after forty years.
If the patient is in menopause, diagnosing an advanced tumor will require removal of both ovaries along with the tube. This method is due to the prevention of the transition of the tumor to a bilateral process of development.
After surgery, restorative hormonal therapy is traditionally prescribed. Antibiotics, vitamins and restoratives can also be used.
The recovery period after such treatment is long. It can be 6-12 months. In this condition, a woman is recommended to undergo a follow-up examination with a doctor every month and undergo tests.
As additional measures during the rehabilitation period, it is important to adhere to a diet and limit intimate relationships until the wounds have completely healed.
Bibliography
- ICD-10 (International Classification of Diseases)
- Yusupov Hospital
- Cherenkov V. G. Clinical oncology. — 3rd ed. - M.: Medical book, 2010. - 434 p. — ISBN 978-5-91894-002-0.
- Shirokorad V.I., Makhson A.N., Yadykov O.A. The state of oncourological care in Moscow // Oncourology. - 2013. - No. 4. - P. 10-13.
- Volosyanko M.I. Traditional and natural methods of preventing and treating cancer, Aquarium, 1994
- John Niederhuber, James Armitage, James Doroshow, Michael Kastan, Joel Tepper Abeloff's Clinical Oncology - 5th Edition, eMEDICAL BOOKS, 2013