Why is oncocytology performed?
Why is the research performed and what is it? Oncocytology is a microscopic analysis of cells taken from the cervix. The main purpose of the procedure is to identify oncological abnormalities.
Thanks to oncocytology, it is possible to detect cervical cancer at the initial stages of development. This increases the likelihood of complete cure of benign and malignant tumors.
Using the analysis, precancerous conditions are identified:
- Leukoplakia.
- Erythroplakia.
- Polyps on the cervix.
- Dysplasia.
The structure of the cells collected for analysis is two-layer. Thanks to this, the cervical cavity is protected from the penetration of harmful microorganisms from the external environment. Double-layer cells are the best option for oncocytology.
Changes in the structure of the cervical epithelium suggest that pathological processes occur in this area that can lead to the development of a cancerous tumor.
https://youtu.be/_rpToiYPGLU
Research methods
There are 2 ways to perform oncocytology:
- Simple. It is used in public medical institutions and antenatal clinics. This method is called the Leishman method.
- Liquid. The study is carried out mainly in private clinics. This method is considered the most reliable.
In the first case, the material is applied to sterile glass and sent for further study. A smear is taken only from a specific area. Test results using the Leishman method take 10-14 days to prepare.
In the second case, the biological material is placed in a liquid medium that preserves the original properties of the cells. The analysis results are prepared in about 5-10 days.
There is another way to perform oncocytology - the Pap test or the Papanicolaou technique. The method is practiced in private medical institutions. The biological material is placed, as in the simple method, on a special glass slide. The difference between the Papanicolaou test and the Leishman method is the way the epithelial cells are stained before examination under a microscope.
How is the research conducted?
Oncocytology is not accompanied by pain and for this reason does not require the administration of painkillers before taking a smear. After the study, there is no damage to the epithelium or changes in its structure.
A smear is taken by a gynecologist. First, the specialist inserts a dilating speculum into the vagina, then, using a spatula, removes epithelial cells from the cervix. If necessary, the doctor collects samples of material from the cervical canal.
After the procedure, bleeding from the vagina may occur. After a few days, the bleeding goes away on its own without treatment.
The collected biological material is placed on a sterile piece of glass or in a liquid medium. Epithelial cells are treated with fixing compounds and staining solutions. The conclusion is issued by a morphologist who studies the material under a microscope.
Based on the results of this conclusion, the gynecologist draws up an appropriate treatment regimen.
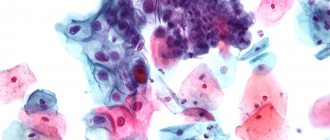
Normal squamous epithelial cells
The presence of squamous epithelial cells in the smear is normal, since the entire cervix is covered with squamous epithelium. The normal volume of these cells in a smear can be up to 15 units per field of view. The absence or greater volume of cells indicates the presence of abnormalities in the body. However, an accurate diagnosis can only be established by assessing all study parameters. A small number of squamous epithelial cells in a Pap smear (up to 5 per field of view) indicates insufficient production of estrogen in a woman’s body.
In medical practice, there have been cases when there are no squamous epithelial cells in a Pap smear. This indicates that they are atrophied. In addition, such cell death may indicate a high likelihood of developing cancer . In this situation, in addition to the usual cytology test, the doctor recommends that the woman undergo additional tests to obtain more accurate results.
Converse research results or an excessive increase in the number of squamous epithelial cells in a cytology smear (from 15 or higher in the field of view) is most often a sign of cervical inflammation, diffuse mastopathy or primary infertility. If there are benign formations in the genitourinary system or during hyperkeratosis, an increased number of squamous epithelial cells may also be observed. Hyperkeratosis is a disorder of the keratinization process in the body. At the same time, the amount of squamous epithelium produced in the body is not controlled.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
In addition to the number of squamous epithelial cells in the smear, the size and condition of the cells are also studied. All these data are evaluated to obtain accurate information about the woman's health.
The size and general condition of flat cells is studied according to indicators such as:
- form;
- structure;
- sizes.
Indicators consisting not only of flat epithelial cells, but also cylindrical and multilayered ones . Such research results can be observed if the smear collection procedure is not entirely accurate. Then cells from different layers of the epithelium enter it. However, the presence in the smear of cells that are abnormal in their structure may indicate that inflammatory processes are occurring in the uterus, including a high probability of the presence of papillomavirus, benign lesions of the cervix or dysplasia in the woman’s body.
Only a doctor can evaluate the results of the study and make a preliminary diagnosis based on the analysis.
Indications for the procedure
An analysis for oncocytology of the cervix must be done for all women who are sexually active. The study is performed not only in case of suspected pathology of the genitourinary system, but for the prevention of cervical cancer.
Oncocytology is mandatory if cancer is suspected. Indications for taking a smear are also:
- pregnancy (2nd or 3rd trimester);
- damage to the cervix after childbirth;
- age over 30 years;
- irregular menstrual cycle;
- papillomavirus infection;
- genetic predisposition to cancer.
The procedure is recommended for women who have bad habits, suffer from genital infections and immunodeficiency several times a year. After 30 years of age, cervical cancer screening is performed once a year. The examination deadlines must be strictly adhered to. Otherwise, the identified cancer cells will be difficult to eliminate.
The study is not performed for inflammation of the reproductive system. The pathogenic flora that provoked the pathology will distort the informative picture.
Normal cervical structure
Tissue for a smear is taken from the surface of the epithelium of the cervix and cervical canal. The cells that are capable of being exfoliated fall on the cytobrush. Therefore, mature epithelial cells normally predominate in a smear. The higher their degree of maturation, the greater the chance that the smear will show normal values. During atrophic processes, the epithelium is exfoliated in an immature state.
With a normal structure of the cervix and the absence of pathology, the following types of epithelial cells are found:
- Superficial
Large cells with a multifaceted shape, close to an oval or circle. Their nuclear material is enclosed in an oval shape, the epithelium is scattered, and has a yellow-pink cytoplasm. In less mature cells, the arrangement in the smear is crowded, in layers or heaps, and the cytoplasm is cyanophilic, with a bluish tint.
- Intermediate
Large epithelial cells, the nuclei of which contain a large number of chromatin blocks; the cytoplasm is painted pinkish or bluish and has pronounced folding. Intermediate cells are often lysed by lactobacilli, but they never destroy the surface type of epithelial cells.
- Parabasal
Small immature cells, oval or round in shape, large, vesicular nuclei. Cells are not destroyed by bacteria, but are subject to autolysis.
- Basal
Smaller in size than parabasal ones, but with large nuclei, characteristic of the postmenopausal or postpartum period, until the menstrual cycle has been restored.
Columnar epithelium may appear in the smear, which lines the cervical canal. They form small groups, arranged in stripes and honeycombs. Sometimes there are goblet cells containing mucus and secretion granules.
A normal smear may contain single leukocytes. Their number may increase before menstruation, but their structure is different from those that appear during inflammation. Quiescent leukocytes are characterized by a preserved or pyknotic nucleus, clear cytoplasm, and no signs of phagocytosis.
How to prepare for oncocytology?
The accuracy of the results largely depends on the preparatory activities. A smear for oncocytology is not taken during menstruation. The best time to do the test is before your period starts or immediately after it ends.
A few days before the event, a woman must refuse:
- from sexual relations;
- from using tampons;
- from douching;
- from the use of vaginal suppositories;
- from taking a bath;
- from taking antibiotics and anti-inflammatory drugs.
It is recommended that you avoid going to the toilet for several hours before your appointment as this may affect the accuracy of your results.
Research results
The cytogram is considered normal if no atypical cells were found in the test results. A positive result does not indicate with 100% accuracy a precancerous or cancerous condition.
Out of 100 smears taken, about 50 are considered uninformative because the conditions for preparing for the procedure were violated or the laboratory received an insufficient amount of material. In this case, oncocytology is performed again.
The reasons for obtaining an unreliable result include infection of a woman with the following sexually transmitted infections:
- gonococci;
- chlamydia.
The papilloma virus also causes changes in the structure of the epithelium and the formation of benign elevations on its surface - genital warts. For this reason, women suffering from HPV should undergo oncocytology 2 times a year.
A breakdown of the results by class is presented in the table
| Class | Characteristic | Recommendations |
| 1 | No atypical cells were detected. All elements of biological material have a normal structure and shape | No treatment required |
| 2 | Single abnormal structures were identified, indicating the development of an inflammatory process. No cells indicating the presence of tumors were found | Additional diagnostic measures are required using other techniques |
| 3 | A small number of anomalous elements were detected | Regular diagnostic measures are required to study the results over time |
| 4 | Cancer cells found in smear | Additional diagnostic measures are required followed by drug treatment |
| 5 | There are a large number of cancer cells | The patient needs treatment in an oncology clinic |
The diagnosis is made definitively only after a comprehensive diagnosis. A few months after treatment, tests are repeated.
If the cytogram is positive, women are prescribed:
- Colposcopy. The study allows you to study in detail the condition of the cervix and vaginal mucous membranes.
- Biopsy. The study is prescribed only if malignant cellular structures are detected.
- Histological analysis.
Cytological method in the diagnosis of tumors and tumor-like processes
Cytopathology, clinical or diagnostic cytology, studies the cellular composition of pathological processes. It was officially recognized as a separate medical specialty in 1941 after the work of G. Papanikolaou and N. Trout. To the credit of our country, the development of a cytological diagnostic method began in 1938 in the clinical diagnostic laboratory of the Moscow Research Oncological Institute. P.A. Herzen. In 1941, Professor N.N. At the institute's session, Schiller-Volkova reported on the first results of the study of vaginal discharge, sputum and punctures. In the development of cytology, three main stages can be distinguished: exfoliative, mainly gynecological cytopathology; aspiration cytology, the rapid flowering of which begins in the 80s and is associated with the introduction of ultrasound diagnostics, and the current stage of development is determined by the use of immunocytochemical and molecular research methods, as well as automated screening in gynecological cytology.
The cytological method is technically simple, fast, relatively cheap, and low-traumatic. However, the “ease” of the cytological method is deceptive, since the cytological study should end with the formulation of a conclusion, based on which treatment tactics are developed.
Based on the method of obtaining the material, cytology can be divided into preoperative (exfoliative, abrasive, aspiration) and intraoperative. Exfoliative cytology includes the study of vaginal smears, sputum, urine, pleural, peritoneal, pericardial, cerebrospinal, synovial fluid, etc. This section of cytology is distinguished by the simplicity of the technique for obtaining a large number of different types of cells, including the inflammatory series. Cellular material may not be well preserved. To obtain informative material, pus-like masses, crusts, and necrotic plaque are removed from the surface of the pathological focus. If the resulting material is a liquid, then sodium citrate is added to it to prevent the liquid from curdling.
Abrasive cytology obtains material from a specific area of internal organs, including examining subepithelial lesions using fiberoptic instruments. With this collection of material, the cells are well preserved, and the preparations are easy to interpret. The material is obtained from the cervix, vagina, endometrium, respiratory, gastrointestinal, and genitourinary tracts.
Fine-needle biopsy now makes it possible to obtain material from almost any organ. The method is constantly being improved and gives optimal results, which makes it highly effective and economical in terms of diagnostics.
The material taken for cytological examination is placed on the edge of a slide and another slide or cover glass is spread evenly, without pressing too much, in a thin layer over the entire surface of the specimen.
In recent years, in addition to routine cytological smears, a liquid system has been used to obtain high-quality monolayer cytological preparations: punctates are added to a special accumulation medium, after which they are centrifuged at 1000 revolutions for 5 minutes at medium acceleration in a centrifuge (Cutospin-3, Cytospin-4). The use of liquid cytology techniques has a number of advantages: it ensures the safety of cellular structures, reduces background, cells are concentrated in one place - a “window”, which reduces the time for viewing the specimen and significantly saves expensive sera when conducting immunocytochemical studies. To create an archive and enable subsequent study of the material, the Cell-block technique is used, which produces preparations that occupy an intermediate position between cytological and histological.
Wet fixation of the drug in alcohol immediately after taking smears is used for Papanicolaou staining. In other cases, the smears are dried in air and then fixed in the laboratory. The most common method of fixation is in equal volumes of alcohol and ether (Nikiforov’s mixture). For immunocytochemical studies, fixation with acetone is used. When staining smears, panchrome staining with azure-eosin is used according to the Romanovsky-Giemsa method in various modifications (Leishman, Pappenheim), as well as hematoxylin and eosin staining, especially when examining gynecological material, Papanicolaou staining is used. It is possible with routine examination or special staining to identify bacterial flora, including Koch's bacilli, leprosy, Helicobacter, Trichomonas, etc.
Cytological diagnosis is based on the following principles:
- The difference in cellular composition in normal and pathological conditions.
- Evaluation of not one individual cell, but a collection of cells, great importance is attached to the background of the preparation.
- The cytologist must have a pathological basis.
- Each study ends with a conclusion.
The criteria for the cytological diagnosis of malignant neoplasms are composed of an assessment of the cell, nucleus and nucleolus.
Cell:
– increased in size, sometimes gigantic, rarely the size is close to normal, which complicates cytological diagnosis, for example, in colloid, tubular cancer, mastitis-like variant of lobular breast cancer, follicular thyroid cancer, carcinoid, renal cell clear cell cancer, well-differentiated spindle cell sarcomas;
– change in shape and polymorphism of cellular elements;
– violation of the ratio of nucleus and cytoplasm in the direction of increasing the proportion of the nucleus;
– dissociation of the degree of maturity of the nucleus and cytoplasm, for example, a young nucleus in keratinized cytoplasm in highly differentiated squamous cell carcinoma.
Core:
– increase in size, polymorphism, tuberosity, uneven chromatin pattern, the most constant sign is uneven contours, hyperchromia, cell division figures in cytological preparations are relatively rare.
Nucleolus:
– the number of nucleoli is greater than in a normal cell, the nucleoli are increased in size and irregular in shape.
Despite the presence of malignancy criteria in the vast majority of cells, in some cancer cells these criteria may be absent or incompletely expressed. It is necessary to pay attention to the peculiarities of the relative arrangement of cells and the nature of intercellular connections. The conclusion is formulated based on a set of characteristics with a sufficient amount of cellular material. An attempt to evaluate a smear using inadequately collected material is the most common cause of erroneous conclusions.
The main tasks of cytological diagnostics are as follows:
- Formulation of the conclusion before treatment.
- Intraoperative urgent diagnostics.
- Monitoring the effectiveness of treatment.
- Assessment of the most important prognosis factors for the course of the disease.
The cytological report before treatment includes:
- determination of the histogenesis of neoplasms;
- establishing the degree of differentiation of the tumor process;
- clarification of the extent of tumor spread;
- studying background changes;
- identification of some prognosis factors;
- possibility of studying bacterial flora.
A modern cytological report not only states the presence of cancer, but also indicates the histological type of tumor and the degree of differentiation according to generally accepted international classifications (ICD-O and WHO).
The criteria for the reliability of the cytological method are the results of comparison with a planned histological examination. The highest percentage of coincidences of the cytological conclusion with the final histological conclusion is observed in the study of formations of the skin, breast, thyroid gland, and with metastatic lesions of the lymph nodes. The results of the study of hyperplastic processes in the endometrium are unsatisfactory (reliability 30–50%) and force us to look for ways to improve diagnostics. The reliability of cytological diagnosis of cervical pathology is 75–90%. 3–24% of studies, depending on the location and method of obtaining the material, are unsuccessful due to inadequately obtained, uninformative material.
Table 1
. Reliability of cytological studies of tumors of various locations.
| Localization | % agreement between cytological and histological diagnosis | % agreement according to literature data | % of failed punctures |
| Lung | 95,5-97 | 79-98 | 2,9-3,0 |
| Breast | 95,8-97,4 | 90-96 | 2,6-8,3 |
| The lymph nodes | 98,4-98,7 | 90 | 1,6-10,7 |
| Leather | 91,2-92,7 | 90-98 | 2,4-12,5 |
| Soft tissue (without indicating the histological type of tumor) | 90,2-93,8 | 65-93,4 | 5-12,3 |
| Gastrointestinal tract | 92,3-97,5 | 73-93,6 | 2,5-4,4 |
| Thyroid | 85,5-93,2 | 57-94 | 1,6-4,2 |
| Cervix | 89,5-93,2 | 65-90 | 3,5-4,5 |
| Endometrium | 78,9-84,8 | 30-90 | 3,8-15,4 |
| Bud | 86,2-89,3 | 76,4-91,3 | 7,1-11,5 |
| Exudates | 95,7-100 | – | 1,2-2,7 |
A confident cytological conclusion about the presence of a malignant neoplasm, coinciding with clinical symptoms and data from other diagnostic studies, is regarded as morphological confirmation of the diagnosis of a malignant tumor. This places high demands on the cytological method and forces us to look for ways to prevent possible errors. Based on the nature of errors, cytologists can be divided into two large groups: false negative and false positive. False-negative conclusions prevail and lead to underdiagnosis of the tumor process, most often due to the small amount of informative material in the punctate. There are also objective difficulties in assessing changes, most often associated with high differentiation of the tumor, for example, it is almost impossible to diagnose follicular thyroid cancer with minimal invasion, and it is difficult to diagnose the tubular, mastitis-like form of lobular breast cancer.
Overdiagnosis of tumors in our material for many years does not exceed 1%, however, it can cause unnecessary and sometimes crippling treatment. True overdiagnosis, that is, a false cytological conclusion about the presence of a tumor, is explained by several of the most typical reasons.
Severe proliferation of cellular elements is the most common cause of overdiagnosis of cancer. For example, proliferation of the epithelium of the ducts and lobules of the mammary gland in fibroadenoma and proliferating adenosis, especially with enlargement of the nuclei, most often leads to overdiagnosis of breast cancer. Correct diagnosis is helped by analysis of the nuclear characteristics of tumor cells: the presence of smooth nuclear contours and uniform distribution of chromatin.
Reactive changes in the epithelium are also a common cause of inadequate cytological diagnosis. The most serious errors occur in renal angiomyolipoma, in which reactive changes in the renal epithelium with enlargement and nuclear polymorphism lead to an erroneous diagnosis of well-differentiated renal cell clear cell carcinoma. The diagnosis of angiomyolipoma is aided by the detection of vascular structures and spindle cells expressing vimentin, desmin, and HMB-45.
Chronic autoimmune thyroiditis of the Hashimoto type is accompanied by the formation of papillary-like structures, the assessment of which must be approached with caution and remember that in this process, reactive changes in the epithelium can be mistaken for papillary thyroid cancer. Chronic dermatitis and ulcers are characterized by atypical reactive growths of stratified squamous epithelium, which often present insurmountable difficulties in differential diagnosis with well-differentiated squamous cell carcinoma. Pronounced dystrophic changes in cells are also one of the reasons for erroneous cytological diagnosis. For example, severe fatty degeneration of hepatocytes can lead to overdiagnosis of clear cell renal cell carcinoma metastasis, especially when a diagnosis of kidney cancer has already been made.
A major problem in cytology is the differential diagnosis of various degrees of dysplastic changes in the epithelium and intraepithelial cancer. In severe dysplasia, the presence of polymorphic large cells with large irregularly rounded nuclei, sometimes with enlarged nucleoli, binucleate cells with a heavy chromatin pattern can be incorrectly assessed as cancer. With dysplastic changes in the squamous epithelium, it is necessary to take into account that most of the cells are similar to the cells of the deep layers, large atypical cells are in close connection with cells without signs of atypia, and there are stromal cells. To objectify the differential diagnosis of various degrees of dysplasia and intraepithelial cancer, it is desirable to carry out morphometry of cells and nuclei, which can significantly reduce the percentage of erroneous conclusions.
Often the cause of overdiagnosis of metastatic lesions in the lymph nodes is complexes of enlarged endothelial cells and histiocytes forming epithelial-like structures, as well as the presence of macrophages containing brown pigment. If there are diagnostic difficulties, an immunocytochemical study with a small set of antibodies (factor VIII, cytokeratins, EMA, HMB-45) helps, which allows you to confirm or reject the presence of metastases of cancer or melanoma.
To avoid errors in morphological diagnosis, a clear indication of the nature of the treatment performed is of great importance. For example, taking the fairly common antibiotic tetracycline leads to the accumulation of brown pigment in the thyroid cells and an erroneous diagnosis of melanoma metastasis. Taking Mercazolil for goiter is accompanied by a sharp polymorphism of the follicular epithelium, which causes cytological and even histological overdiagnosis of follicular cancer. Radiation therapy causes pronounced changes not only in tumor cells, but also in normal epithelium: enlargement, cell polymorphism, pathological keratinization, which causes overdiagnosis of cancer.
There are also objective diagnostic problems, for example, in the differential diagnosis between endometrioid well-differentiated adenocarcinoma and atypical endometrial hyperplasia, seborrheic (basal cell) keratoma and basal cell carcinoma, infectious mononucleosis and Hodgkin's disease, where the percentage of erroneous conclusions is quite high and further development of cytological diagnostic criteria is required .
Knowledge of the clinical picture, the nature of the treatment, the use of modern methods of morphological diagnosis using immunocytochemistry and morphometry helps to reduce cases of overdiagnosis to zero.
Along with true cytological overdiagnosis, there is false overdiagnosis, when the cytologist gives a confident conclusion about a malignant process, but a histological examination of the tumor is not detected, that is, in fact, histological underdiagnosis occurs. Review of cytological preparations by several highly qualified specialists, repeated biopsies, and the clinical course of the disease further confirm the results of the cytological examination. Most false cytological overdiagnosis relates to the study of biopsy material from the bronchi and larynx, as well as in the study of lymph nodes, when cytological examination revealed single complexes of anaplastic cells that undoubtedly belonged to cancer. When preparing histological preparations, these complexes are lost in the finished histological preparations. The real loss of a few tumor cells during the preparation of histological preparations does not allow the clinician to ignore the cytological data and leads to the “gold” standard - a joint cytological and histological examination of the biopsy specimen.
Intraoperative cytological diagnostics is one of the main directions of the cytological research method. During the operation, using the cytological method, the nature of the pathological process, the degree of prevalence are clarified, with the identification of metastases in the lymph nodes, liver and other organs, the radicality of the operation performed is monitored, and the resection margins are examined. The role of cytology increases in developing indications for extended lymphadenectomy and in determining the so-called “sentinel” or “sentinel” lymph nodes, of which there can be six, and the use of the histological method is impossible due to the duration of the study. According to leading clinics, the error in urgent histological examination of “sentinel” lymph nodes is 25%, so they recommend the use of intraoperative cytological examination of prints from the surface of the cut lymph node. According to our data, the reliability of an urgent cytological examination to detect metastatic lesions of the lymph nodes is 97-99%.
It should be noted that there may be contraindications for urgent morphological examination. Urgent intraoperative morphological examination is not recommended for suspected intraepithelial cancer with a limited lesion due to the fact that there will be no material left for routine histological examination. Cytological criteria for intraepithelial carcinoma are just being developed, and a cytologist can make a diagnosis of cancer without indicating that it is Carcinoma in situ. For small intraductal papillomas, it is better not to perform an urgent histological examination, but a cytological examination will reliably help establish the nature of the process.
In case of urgent morphological diagnosis, macroscopic examination of the surgical material significantly helps. An experienced morphologist can already make a diagnosis through visual examination, but microscopic examination is necessary to confirm the diagnosis. For example, a tumor node of a classic stellate shape can be due to three completely different processes: cancer, sclerosing adenosis with a Semba center and lipogranuloma. And only microscopic examination allows a correct diagnosis.
The cytological method allows one to dynamically study the therapeutic pathomorphosis during chemoradiation and photodynamic therapy without injuring the patient.
The 20th century is called in medical circles the century of cytopathology. Assessing the capabilities of the cytological method, we can say that there are still opportunities for its development in combination with other disciplines and methods.
Immunocytochemical research is often decisive in the differential diagnosis of neoplasms, when during routine research insurmountable difficulties arise in establishing the histogenesis of individual tumors, determining the source of metastasis, and interpreting multiple primary lesions.
In recent years, tremendous progress has been made in the clinical use of various biological markers. Unlike serum markers, cellular markers are determined directly in tumor cells by ICC testing, which is based on the antigen-antibody reaction. These include oncogenes, estrogen and progesterone receptors, molecules mediating apoptosis, growth factor receptors, etc. All these indicators make it possible to study in more detail the molecular biological characteristics of tumor cells associated with the degree of differentiation, ability to invade and metastasize, sensitivity to chemotherapy, and, consequently, with the characteristics of the course and prognosis of the disease in each specific case.
There are no specific markers for the differential diagnosis of malignant and benign tumor processes, but today scientific research is being actively carried out to solve this problem. Thus, uniform staining of the germinal centers of lymphoid follicles using bcl-2 antibodies indicates follicular lymphosarcoma, while a negative reaction indicates a benign hyperplastic process; the reaction with HBME-1 antibodies in the ICC study of thyroid tumors is often positive in malignant neoplasms and practically absent in benign ones; galectin-3, expressed by thyroid carcinomas from A-cells (papillary, follicular) with no expression in follicular ones, is widely used in differential diagnosis adenomas, goiters and normal thyroid tissue.
To establish the histogenesis and differential diagnosis of tumors, schemes by CRTaylor and RJ Cote (1994) have been developed and are constantly being improved. The variety of monoclonal antibodies used in immunocytochemical studies of fine-needle punctures allows us to answer in each specific case the question of whether a given tumor is of epithelial origin or is a sarcoma, melanoma, or lymphoma. Immunocytochemistry is widely used for immunophenotyping of malignant lymphomas, without which, according to modern canons, it is impossible to begin treatment.
Immunocytochemical research helps in determining the source of metastasis when the primary focus is undetected. Unfortunately, there are not so many organ-specific markers. These may include prostate specific antigen (PSA), which makes it possible to identify prostate cancer metastases in more than 95% of cases; thyroglobulin, expressed in 92–98% of follicular and papillary thyroid cancers, and calcitonin, expressed in 80% of medullary thyroid cancers. In some cases, thyroid cancer can express both calcitonin and thyroglobulin, which only with the help of enzyme-linked immunosorbent diagnostics makes it possible to diagnose dimorphic A -C-cell cancers.
One of the first indicators that entered the practice of treating patients with breast cancer (BC), and classified as cellular markers, were steroid hormone receptors. Steroid hormone receptors are proteins that specifically and selectively bind the corresponding steroids after they enter the cell.
According to WHO (2003), the expression of estrogen receptors (ER+) and progesterone receptors (RP+) in invasive ductal cancers is 70-80%; invasive lobular cancer expresses ER in 70-95%, RP in 60-70%, 100% expression of ER is noted in invasive cribriform and mucinous breast tumors. Edocrine therapy is most effective in patients with primary tumors with high levels of steroid receptors. In metastatic lesions, the degree of response to endocrine therapy also depends on the presence of ER and RP in the tumor: its effectiveness is about 10–15% for hormone-negative tumors, 27% for tumors with ER+ and RP-, 46% for ER- and RP+ status and 75% for tumors containing RE+ and RP+. Receptor-positive breast tumors have higher differentiation and a more favorable prognosis.
It should be noted that hormone receptors in benign breast formations have not yet been studied enough. There was an increase in the number of ER+ cells in normal breast tissue with increasing age, as well as in sclerosing adenosis, papillomas, fibroadenomas and leaf-shaped tumors. Coexpression of RE+/Ki-67+ with varying degrees of severity and ratio was mostly detected in pathology associated with the risk of developing breast cancer.
Estrogen receptors are expressed in endometrial, ovarian, cervical, thyroid, intestinal cancer cells, and neuroendocrine tumors, including carcinoids.
Immunocytochemical research makes it possible at the preoperative stage to establish the most important factors for the prognosis of the tumor process and to adjust treatment regimens. The proliferative activity of many neoplasms is assessed using Ki-67 antibodies in malignant lymphomas, tumors of the breast, prostate, pancreas, lungs, pituitary gland, and colon. A relationship was found between the values of the proliferation index and the degree of histological differentiation of the tumor and clinical prognosis for endometrial, ovarian, lung, breast, bladder cancer, lymphomas, and tumors of the nervous system.
Overexpression of oncoprotein C-erbB-2 (HER2/neu), which is a receptor for epidermal growth factor type 2, which gives cells the property of unlimited division, serves as a risk factor for disease relapse for a number of tumors: breast cancer, colon cancer, lung cancer, etc. Expression Oncoprotein C-erbB-2 is detected in 15–40% of breast cancer in IHC studies. The detection of oncoprotein C-erbB-2, according to some authors, is associated with a high degree of malignancy of the tumor, the absence of ER and RP, high mitotic activity, resistance to chemotherapy and requires the prescription of Herceptin.
The presence of metastases in the lymph nodes in tumor lesions is the main discriminating prognostic sign. Using immunocytochemical research, it is possible to detect single circulating keratin-positive breast cancer cells in the bone marrow and peripheral blood. The use of ICC research increases the detection of micrometastases in lymph nodes by 3.2–24%.
Immunocytochemical reactions are assessed both qualitatively when clarifying the histogenesis of the tumor, the presence of metastasis in a lymph node or other organ, immunophenotyping of lymphomas, and quantitatively when assessing proliferative activity, expression of hormone receptors in the tumor, oncoprotein C-erbB-2, etc. The immunocytochemical reaction can be nuclear, cytoplasmic and membrane. The nuclear reaction is manifested by intense staining of the nucleus and occurs when determining RE and RP, Ki-67, PCNA, p53, etc. The cytoplasmic reaction is characterized by diffuse staining of the cytoplasm or deposition of granules in the form of coarse spots and grains. Cytoplasmic staining is provided by chromogranin, synaptophysin, protein S-100, vimentin, desmin, thyroglobulin, calcitonin, cytokeratins, bcl-2, etc. Evaluation of this reaction requires great care and control, since background staining of the cytoplasm of cells may be mistaken for a true reaction. Membrane staining is observed when reacting with oncoprotein C-erbB-2 and EMA (epithelial membrane antigen). Staining in such cases only of the cytoplasm should not be counted as antigen expression. The marker of large cell anaplastic lymphoma CD-30 can be expressed both in the cytoplasm and on the cell membrane.
To quantify the expression of the Mc marker. Carthy et al developed the Histo score (HS). The scoring system includes the intensity of immunocytochemical staining, assessed on a 4-point scale, and the proportion of stained cells and is the sum of the products of percentages reflecting the proportion of cells with different staining intensities per point corresponding to the intensity of the reaction. Color intensity in points: 0 - no staining, 1 - weak staining, 2 - moderate staining, 3 - strong, 4 - very strong staining. Calculation formula:
Histochemical score = ∑ P(i)×i
(histocount),
where i is the intensity of staining, expressed in points from 0 to 4, P(i) is the percentage of cells stained with different intensities.
The maximum number of Histo scores should accordingly be 400. Counting is carried out in three cohorts of 100 tumor cells in different fields of view (lens x 40).
In practical work, the use of semi-quantitative assessment is acceptable. The reaction is considered negative in the complete absence or expression of the antigen in less than 5%–10% of tumor cells, weakly positive in 5%–10% to 24% of cells, moderately positive in 25%–75%, pronounced in more than 75% of cells. When assessing the immunoenzyme reaction, the intensity and completeness of staining of the cytolemma of cells in the center of the tumor focus is taken into account. Thus, a bright, membranous, continuous reaction along the contour of the cell indicates a pronounced expression of the C-erbB-2 protein (+++), which in 95% of cases is confirmed by amplification of the C-erbB-2 gene, detected using FISH (fluorescent in situ hybridization) .
Comparing data from immunocytochemical studies of various tumors in order to clarify the histogenetic affiliation and the results of postoperative morphological conclusions, the following results were obtained: 89% of matches in the analysis of thyroid tumors, 83% in clarifying the histogenesis of the primary tumor and metastases in the lymph nodes, 89% in soft tissue tumors and skin and 100% – in the study of biological fluids. When determining the hormonal status of breast cancer, the percentage of agreement between ICC and IHC studies is 88.3%, when studying proliferative activity - 83%, when determining the oncoprotein C-erbB-2 - 93.2%.
When comparing the capabilities of ICC research when performing a puncture biopsy and IHC research during trepanobiopsy, the advantages of ICC, in our opinion, are undoubted. A puncture biopsy is a simpler procedure, is not accompanied by complications such as inflammation, bleeding, and allows you to obtain complete cellular material. If the puncture fails and the necrosis, tumor stroma, and surrounding tissues enter, the procedure can be repeated almost painlessly. In addition, there is no loss or masking of antigens during processing and dewaxing of the material using aggressive chemicals.
The use of immunocytochemical research makes it possible to expand the capabilities of morphological methods and, at the preoperative stage, to clarify histogenesis, diagnose multiple primary lesions, the degree of spread, and evaluate some indicators of prognosis and sensitivity of the tumor to chemohormonotherapy.
At the present stage of development in cytology, molecular and gene diagnostic methods are used: in situ hybridization, Southern Blotting, Northern Blooting, Western Blotting, DNK Microarray, etc. In scientific and practical work, cytologists use flow cytophotometry.
One of the ways to improve the cytological research method is the use of morphometry, which allows one to obtain objective quantitative parameters. For example, when processed on a computer, the most informative morphometric features related to the parameters of the nucleus were identified using the main diagnostic morphometric features: area, perimeter, optical density, nuclear polarization coefficient, number of nucleoli, their area and perimeter. Objective morphometric signs of various degrees of dysplasia have been developed in dyshormonal-hyperplastic processes of the mammary gland and cervix, which has reduced the share of subjectivity in determining the various degrees of dysplasia.
New methods of microscopy are being developed: phase contrast, fluorescence, confocal, etc. The creation of computer training systems and the development of the teleconsultation method also impose new requirements and will undoubtedly contribute to the development and improvement of the cytological diagnostic method.
Volchenko Nadezhda Nikolaevna
Doctor of Medical Sciences, Professor, Head of the Department of Oncocytology, Moscow Research Institute named after P.A. Herzen