Colpitis in women - what is it? Symptoms and treatment The most common age when colpitis occurs in women is reproductive age. Typically, the vagina of sexually mature women is protected from vaginal infections by an acidic environment and intact mucous membrane. But a sensitive environment that largely protects against pathogens can quickly become out of balance due to antibiotics, excessive hygiene, or estrogen deficiency.
When this natural vaginal defense mechanism is compromised, bacteria, fungi and other pathogens can easily cause this inflammation. They are often transmitted during sexual intercourse and through environmental exposure to the vagina, when it is most susceptible to infection.
Causes of colpitis in women
Various reasons can cause the development of the inflammatory process at different ages:
- During reproductive age, women are more likely to develop specific colpitis that is infectious in nature. The predominant type of disease is trichomonas, which is sexually transmitted. Bacterial and candidal colpitis are somewhat less common, the causes of which are mainly hormonal imbalances during pregnancy.
- In women after menopause, nonspecific colpitis is most often observed, which is caused by staphylococcus and streptococcus. However, candidiasis, trichomonas, and other types of colpitis occur. But they develop in the presence of additional risk factors.
- In childhood, the disease develops mainly due to the entry of microflora of the gastrointestinal tract into the vagina. Streptococci, staphylococci and even pinworms become provocateurs.
So, at any age, the causes of the development of the disease are: either one’s own opportunistic microflora, or infectious microorganisms belonging to the group of fungi, viruses or bacteria.
General recommendations
The effectiveness of treatment for colpitis directly depends on a whole range of measures. The therapeutic course consists of the following stages:
- destruction of pathogenic microorganisms (antibiotics and antifungal drugs);
- when the body’s immune defense decreases, general strengthening therapy is carried out using immunomodulators and vitamin complexes;
- local treatment, which includes douching with antiseptic agents and introducing suppositories and vaginal tablets that have an antimicrobial effect into the vaginal cavity;
- following a special diet (refusal of spicy, sweet and fatty foods).
In order to make sure that the treatment brings the desired result, throughout the course of therapy the woman must take the necessary tests at regular intervals.
Reference! In patients under 55 years of age, a control smear is taken on the fifth day from the start of the menstrual cycle.
But in older women and young girls, control is carried out only after completing the full course of treatment.
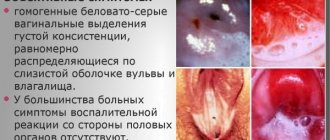
Symptoms of colpitis, photo
The clinical picture of the disease is quite varied and is largely determined by the type of pathogen and the form of its course.
The main signs of colpitis in women are:
- burning, itching in the vagina;
- possible redness and swelling of the labia;
- aching or nagging pain in the lower abdomen;
- the discharge has an unpleasant odor
- pain during coitus;
- dysuric disorders (frequent and painful urination);
- temperature increase;
- the amount of vaginal discharge increases significantly, the nature of which is different (curdled, purulent, homogeneous milky, foamy, bloody or mixed with blood).
In the case of acute colpitis, all manifestations are pronounced: burning and itching are significant, heaviness in the lower abdomen suggests problems with internal organs, discharge is abundant. In severe cases of the disease, a significant increase in temperature is possible, up to 38 degrees or higher. As a rule, this picture is characteristic of specific colpitis (gonorrheal or trichomonas).
With chronic colpitis, the picture is less bright, the symptoms are erased. The disease lasts a long time, with periodic exacerbations. The discharge becomes moderate, serous or serous-purulent.
When examined on a chair in the mirrors, swelling, hyperemia and “looseness” of the vaginal mucosa are revealed. Petechial and pinpoint hemorrhages are noticeable on the mucosa; reddish nodules (infiltrates) and erosive areas may appear. In advanced cases, the cervix is involved in the inflammatory process, which leads to cervicitis or pseudo-erosion.
Kinds
Types of colpitis differ in the pathogen that causes it, as well as in the form. Acute and chronic colpitis are divided into types. Their symptoms differ in their severity and duration. So, during the period of exacerbation, the signs of the pathological process are clearly expressed - pain, unpleasant discharge, itching, burning (such manifestations also differ according to the type of pathogen). And in chronic cases they are less pronounced, but last longer - in some cases up to several years. The chronic form is characterized by periods of exacerbations and remissions.
Since the symptoms and pathogen are different, this means that medical measures will be aimed primarily at eliminating the microbe that caused the pathology.
The most common types: mycotic, trichomonas, gardnerellosis, gonorrhea, candidiasis, streptococcal, staphylococcal, chlamydial.
Specific
Specific or primary colpitis develops directly in the structure of the mucous membranes of the vagina.
A vaginal disease occurs when infectious agents penetrate during sexual intercourse, therefore trichomonas, mycotic, gonorrheal, yeast, gardnerellosis and other types are distinguished (depending on the pathogen). Its development can also be triggered by microtrauma during an examination by a gynecologist or during intimate contact (for example, if the immune system is currently weakened, it is difficult for it to resist attacks from pathogens from the external environment). Therefore, treatment must include antibacterial drugs and means to increase the body’s natural resistance.
Non-specific
Nonspecific colpitis develops against the background of the penetration of an inflammatory process from the cavity of the vagina and uterus or when infectious reactions penetrate into the vagina from the vulva.
With this type of disease, the stages are: serous, mucous and purulent. With chlamydial infection, purulent catarrh forms almost immediately. The yeast species is characterized by swelling, redness of the surface of the epithelium, whitish inclusions appear on it, which quickly develop into extensive spots. Fungal colpitis is characterized by severe itching and burning, and the release of a curd-like substance from the vaginal cavity. The Trichomonas type is characterized by copious foamy discharge and hyperemia of the mucous membranes. With an exacerbation of gonorrheal vaginitis, swelling and inflammation of the mucous membrane appear, such symptoms are especially pronounced in the area of the posterior wall, this is accompanied by copious purulent discharge, bleeding, burning, and distension.
Allergic and atrophic
Allergic colpitis develops due to the negative effect of any irritants on the mucous membranes of the external genitalia.
Such allergens can be substances contained in ointments and condoms. Under the influence of a certain allergen, biochemical reactions in the structures are activated, against the background of which swelling and inflammation occur on the mucous membranes. Atrophic colpitis most often develops in women in old age, when menopausal changes occur in the body. During this period, the concentration of hormonal substances decreases sharply, resulting in a decrease in the level of lactobacilli on the surface of the mucous membranes. But this form of the disease can also appear in women who are middle-aged or even young. The reasons for this are long-term use of certain hormonal medications, surgical interventions to remove the uterus and ovaries.
Atrophic colpitis
The disease is typical for the postmenopausal period; in addition, it can develop in women with artificially induced menopause. Due to the reduction in estrogen levels, a symptom complex occurs, which is manifested by itching, dryness, discomfort in the vaginal area, pain during sexual intercourse, and spotting after sexual intercourse.
Atrophic colpitis (also known as senile colpitis), as a rule, develops due to estrogen deficiency, which leads to a decrease in the secretion of the vaginal glands and thinning of the mucous membrane of the organ.
Causes of vaginitis
Colpitis is a disease of women of childbearing age. Provoking reasons may be:
- menopause;
- psychosomatics;
- decreased immunity;
- hormonal problems;
- unbalanced diet;
- long course of antibiotics;
- failure to comply with personal hygiene rules;
- viruses that have penetrated the vaginal mucosa.
The disease can develop quickly (with the appearance of characteristic symptoms) or not make itself felt at first. Therefore, it is so important to visit a gynecologist for preventive purposes.
Nonspecific colpitis
What is nonspecific vaginitis? The main stimulating factor of the disease is a violation of the microflora of the genital organs. When the number of pathogenic bacteria prevails, nonspecific colpitis begins.
The disease can be caused by:
- pathologies of the endocrine system such as obesity, diabetes, insufficient ovarian function;
- atrophic processes, vascular changes in the vaginal mucosa during menopause;
- prolapse of the vaginal walls, other anatomical changes of the vulva;
- woman ignoring hygiene rules;
- infectious diseases that suppress a woman’s immunity;
- mechanical, chemical or thermal injury to the vaginal mucosa;
- taking antibiotics;
- allergic reactions provoked by hygiene products, contraceptives;
- disruptions at the hormonal level.
Trichomonas colpitis
This form of the disease is caused by Trichomonas, which is sexually transmitted. The household route of infection with Trichomonas, as some patients prefer to think, is impossible, since the pathogen quickly dies in the external environment. The symptoms of Trichomonas colpitis are so pronounced that the diagnosis is not difficult. Characterized by significant leucorrhoea, which has a very unpleasant odor. The discharge is usually foamy and has a yellowish tint.
If nonspecific microflora attaches, the discharge becomes green. The infection spreads very quickly, affecting the cervix, the uterus itself and the urethra, which is manifested by dysuric disorders and pain in the lower abdomen. Sexual intercourse is unpleasant and even painful, accompanied by discharge mixed with blood. [adsen]
Diagnostic methods
Examination for vaginitis consists of several types of examination. This allows you to obtain the most complete clinical picture, identify the causative agent of the inflammatory process and draw up a treatment plan.
Laboratory research methods. During the examination, the gynecologist takes samples of discharge from the vagina, cervix, cervical canal, and urethra. These materials are sent to the laboratory for diagnostics. There, the nature of the pathogen and its resistance to various drugs are determined.
- Culture for gonococcus.
- Bacterial culture to determine the pathogen culture.
- Based on the results of bacterial culture, it becomes possible to identify resistance and susceptibility to various drugs and groups of antibiotics.
- General blood and urine tests to determine the level of immune response.
- Blood test for HIV and syphilis to exclude these pathologies from the list of possible causes.
- Oncocytological examination allows us to exclude the possibility of the presence of neoplasms.
- Colcoscopy, during which the bacterial composition, acidity, and odor of the discharge are examined.
Objective research methods. This group includes those diagnostic techniques that do not require additional tests.
- Examination of the external genitalia for the presence of rashes, ulcers, and inflammations. Additionally, the glands of the vaginal vestibule are examined and the discharge on the external genitalia is assessed.
- The examination of the pelvic organs is carried out during the period of the most pronounced discharge. To carry it out, you should not carry out hygiene procedures at least 12 hours before the examination.
- A bimanual examination, like a rectal examination, allows you to assess the condition of the vaginal walls and check for the presence of seals.
- Examination of the walls of the vagina and cervix, performed using a special gynecological speculum.
Additionally, ELISA and PCR analysis can be performed to determine the type of pathogen. But due to the complexity of conducting such a study, it is used in controversial cases.
How to treat colpitis in women?
Basically, treatment of colpitis comes down to the destruction of pathogens and restoration of microflora.
To treat colpitis, a woman is prescribed antibacterial, antiviral, antifungal drugs: Vokadin and Terzhinan. Vocadine is a pill that is inserted deep into the vagina. It is necessary to administer two tablets per day per week. If colpitis has become chronic, then one tablet before bedtime is enough, but the treatment is extended for two weeks. "Terzhinan" is also produced in tablets. Before inserting them into the vagina, they must be immersed in water for half a minute so that they get wet. One tablet taken before bed is enough. The treatment period is ten days.
Treatment of colpitis and prescribed medications are determined depending on the infection that caused the disease.
- If Trichomonas is the culprit, then the doctor prescribes Metronidazole. In this case, the woman and her sexual partner need to be treated so as not to become infected again.
- If the cause of colpitis was fungi, then medications are used: Ketoconazole, Clindamycin, Fluconazole. When the disease is caused by a gonorrheal bacillus, the following medicine is prescribed: Tetracycline, Cefixime, Ceftriaxone.
Bacterial treatment destroys the vaginal microflora; after treatment it needs to be restored. To restore the microflora, Linex and Bifidumbacterin suppositories are used. The duration of treatment is determined by the doctor.
Treatment of colpitis requires adherence to a certain diet. All pickles, smoked meats and spicy dishes should be removed from the menu. Their place will be taken by vegetables, fruits and dairy products. Close intimacy with men should also be avoided. More attention needs to be paid to perineal hygiene.
Treatment of the disease
Treatment of colpitis is based on an integrated approach and is aimed at eliminating the causative agent of the disease. When choosing medications, the type of colpitis , existing concomitant diseases and the woman’s age are taken into account. Self-medication is unacceptable. The use of drugs should be carried out after visiting a gynecologist and following the treatment regimen recommended by him.
During therapy, you should refrain from intimacy in order to prevent infection from occurring, strictly adhere to a special diet excluding sweet and spicy foods, maintain personal hygiene, and wash yourself more than twice a day.
Local treatment involves the use of disinfectant solutions for douching based on:
- boric acid;
- potassium permanganate;
- soda;
- a decoction of herbs with an anti-inflammatory effect (oak bark, chamomile).
Reference! The course is designed for 4–5 days with a frequency of douching up to three times a day.
Also, suppositories and tablets are used for local effects . Their choice depends on the type of colpitis pathogen.
For nonspecific vaginitis, agents with anti-inflammatory antifungal action are recommended:
- "Terzhinan";
- "Vocadine";
- "Polygynax".
The period of use is determined by the treating gynecologist.
For trichomonas colpitis the following are applicable:
- "Trichopolus";
- "Tinidazole";
- "Hexicon".
It is recommended to repeat the course three times after menstruation.
Candidal vaginitis can be easily eliminated by the following means::
- "Nystatin";
- "Pimafucin";
- "Clotrimazole".
After completing the course of therapy, the vaginal microflora should be normalized by:
- "Bifikol";
- "Lactobacterin";
- "Acylact".
At the same time, taking multivitamins is recommended.
Folk remedies
List of folk remedies that have an excellent effect on the treatment of colpitis:
- Pour 50 g of dry crushed coltsfoot leaves with a liter of boiling water, leave for 1 hour, then strain. The infusion is used for douching for chronic inflammation of the vagina, accompanied by pain (a decoction of blackberry leaves is also prepared).
- Coltsfoot leaf - 2 parts, nettle leaf - 1 part, St. John's wort herb - 1 part, common thyme herb - 2 parts, calamus rhizome - 2 parts, buckthorn bark - 1 part. Place two tablespoons of the resulting mixture in a thermos and pour 2 cups of boiling water. Leave overnight, and in the morning strain and take half a glass 3 times a day.
- Chamomile decoction: add 2 tablespoons of chamomile flowers to a liter of water and boil for 15 minutes. Then the decoction is cooled, filtered through cheesecloth and used for douching twice a day for two weeks (a decoction of calendula is also prepared).
- Yarrow herb - 20 g, sage leaves - 20 g, pedunculate oak bark - 40 g, rosemary leaf - 20 g. Mix everything, add three liters of water and boil. Use twice a day for douching.
- Chamomile inflorescence - 25 g, wild mallow flowers - 10 g, sage leaves - 15 g, pedunculate oak bark - 10 g. Pour two tablespoons of the resulting mixture with a liter of boiling water. Use for douching and vaginal tampons.
To treat inflammation of the vagina and cervix, which are caused by trichomoniasis, pathogenic fungi and various bacterial infections, use a 3% propolis solution mixed with 96% ethyl alcohol. Treatment lasts 7-10 days, the drug is used once a day.
Possible complications
Why shouldn't you start the disease? If you ignore the symptoms of colpitis, women experience many dangerous consequences:
- the chronic form is more difficult to treat with medications;
- provoking diseases of the genitourinary system such as urethritis and cystitis;
- in girls, lack of treatment can result in fusion of the inner or outer labia.
Many women consider colpitis to be a mild illness that can go away without treatment. However, if you ignore the symptoms, it will go into a sluggish form. The symptoms will become less pronounced, but this does not at all indicate a recovery process. At the first symptoms, you need to go to a gynecologist to find out the cause and prescribe treatment.
In the absence of treatment, cervicitis, an inflammation of the cervix, may occur. It is also possible that endometritis (inflammation of the uterine lining) and salpingoophoritis (disease of the appendages) may occur. Such pathologies can lead to infertility and increase the risk of ectopic pregnancy.
Importance of Therapy
Treatment of colpitis is mandatory at any age and with any severity of symptoms. This disease almost never goes away on its own, especially when local or general immunity is reduced.
The main complications of the inflammatory disease include high risks of infection spreading to the pelvic organs, genitourinary system, structural changes in the cervix, infertility or inability to carry a pregnancy, synechiae, etc.
Even if the acute symptoms go away on their own without medical intervention, it is necessary to visit a doctor: weakening of the symptoms may be due to the fact that the disease has become sluggish or chronic. As soon as factors that provoke and weaken the body appear (hypothermia, intimate contact, infectious disease, vitamin deficiency, etc.), pathogenic organisms become active again - recurrent colpitis is observed. If you have any alarming symptoms, you should make an appointment with a gynecologist.
Prevention
There is no one hundred percent protection against colpitis. Try to avoid exposure to pathogens, such as using condoms during intercourse and showering before and after.
You can try not to disturb the natural environment of the vagina. Just as poor hygiene can increase the likelihood of vaginitis, too much washing with soap, long bubble baths, vaginal douches or intimate sprays can be harmful. The vagina has very good defenses against infections, and excessive body hygiene can disrupt this protective mechanism and contribute to the occurrence of colpitis.
Also ensure proper toilet hygiene: when cleaning feces, movements should be exclusively from front to back. Do not wipe stool from the anus to the vagina. If you notice any symptoms, contact your gynecologist immediately.