Causes of diffuse changes
A diffusely heterogeneous structure of the myometrial layer appears for a number of reasons:
- endometriosis or adenomyosis;
- blood diseases, including anemia;
- exposure to stress and regular emotional shocks;
- caesarean section or other operations performed on the uterine cavity;
- abortions, curettage or mechanical cleanings;
- hormonal disorders;
- infectious and inflammatory processes.
It is possible to determine what the true cause of diffuse changes in the myometrium is only after a comprehensive examination. An ultrasound examination alone will not be enough. Childbirth also becomes an indirect cause of the formation of structural changes and heterogeneous foci, however, this natural process does not significantly affect the condition of the muscular layer of the reproductive organ. A woman will have to give birth at least 2 times for diffuse deformation of the muscle layer to begin.
There are also physiological reasons for diffuse changes in the structure of the middle muscular layer - the uterine myometrium. They do not cause persistent pathology. Natural causes provoke the appearance of a temporary heterogeneous structure. These include cyclical changes in hormonal levels, pregnancy and the postpartum period. Diffuse changes and distortion of the structure of the uterine layers are diagnosed during reproductive age and menopause. The pathological process can remain unattended for a long time. The absence of complaints does not guarantee a woman that diffuse disorders do not occur in the uterus.
Causes
The myometrium acts as the muscular layer of the reproductive organ. It contains several types of fibers, a characteristic structure, and three shells. The first layer consists of the serosa and circular muscle fibers.
The middle part of the myometrium is the most powerful, since it contains only muscle tissue, while the structure is supplemented by large main vessels. The inner layer consists only of longitudinal fibers.
Anatomy of the uterus. Source: pervenets.com
The structure of the uterus is heterogeneous precisely due to the fact that the myometrium is quite diverse in terms of its constituent elements. There may be several reasons for the development of diffuse changes, and they are divided into traumatic and less traumatic.
In the first case, the heterogeneous structure in the uterus may be due to previous abortions, against the background of which pathological foci appeared. Low-traumatic causes include childbirth, or spontaneous termination of pregnancy, in which a miscarriage occurs.
Signs
There are many known signs of structural and diffuse changes in the uterine myometrium, however, all of them are indirect. Knowing about the complaints, the gynecologist cannot make a reliable diagnosis - heterogeneous structure of the myometrium. The doctor only has assumptions. Additional diagnostics will confirm your suspicions. The reason to consult a doctor in women with structural and diffuse changes in the myometrium is:
- large blood loss during menstruation;
- painful monthly uterine contractions;
- discomfort during urination;
- discomfort during sexual intercourse;
- painful ovulation;
- brown spotting in the middle or second half of the cycle;
- long absence of pregnancy, primary or secondary infertility.
Most often, diffuse heterogeneous changes in the myometrium are asymptomatic for women.
Diagnostics
It is possible to determine that the myometrium lining the median wall of the uterine cavity is diffusely heterogeneous or has an altered structure using ultrasound scanning. During the procedure, the sonologist evaluates the echogenicity, thickness and homogeneity of this area. If there are any non-compliances with the standards, they are described in detail in the ultrasound report. It should be noted that there are no standards for structural changes. If diffuse distortions are detected, then this already indicates pathology.
To differentiate the diagnosis, the gynecologist may prescribe a series of tests, including blood tests for tumor markers and sex hormones.
If diffuse heterogeneous changes are accompanied by pathological signs in the endometrium, diagnostic curettage is prescribed, which itself becomes a provocateur of the formation of heterogeneous myometrium and its diffuse changes with structural disturbances. If the doctor recommends starting the examination with this manipulation if the endometrium is normal and excludes other methods, it makes sense to consult another specialist.
A clearer picture of what is happening in the uterine cavity is given by endoscopic examination: hysteroscopy or laparoscopy. The procedure is prescribed to patients with a questionable ultrasound result and can go from diagnostic to therapeutic.
Endometriosis
The finding of diffusely uneven myometrial structure suggests that this condition is caused by uterine endometriosis. The disease is characterized by heterogeneous growth of the mucous layer of the reproductive organ and its penetration into the muscular layer. During an ultrasound examination, the sonologist may discover that there are peculiar cellular zones - foci - in the myometrium. Symptoms of the pathology include irregular menstruation and constant pain in the pelvic area.
Often, a woman turns to a gynecologist with a complaint about the lack of pregnancy, and during diagnosis she is diagnosed with endometriosis of the uterus with structural changes in the muscle layer. The disease has three forms:
- genital (uterus, ovaries, fallopian tubes and peritoneum are affected);
- extragenital (adjacent organs are affected);
- mixed (combines the previous two).
If diffusely heterogeneous myometrium is detected, it should be understood that this condition cannot be eliminated in one day. To normalize the function of the muscle layer, the cause of the structural changes must be eliminated.
Endometriosis is corrected with hormonal drugs and minimally invasive interventions. It is also necessary to try to find the exact cause of the development of uterine endometriosis, which is not always possible.
Symptoms of the disease
Often, an enlarged uterus is discovered by chance during a regular medical examination. However, most women who closely monitor their own health observe the following signs of organ pathology:
- monotonous aching pain located in the lower quarter of the abdominal region;
- a sharp drop in hemoglobin level in the blood;
- manifestation of incontinence (urinary incontinence);
- discomfort during or immediately after sexual intercourse;
- engorgement and pain on palpation of the mammary glands;
- menorrhagia (painful and heavy menstruation);
- flatulence, bloating and a feeling of painful fullness in the abdomen;
- a sharp increase in body weight caused by hormonal imbalances;
- discharge of large coagulated blood clots during menstruation;
- uterine or vaginal bleeding between menstruation;
- pain in the lumbar region;
- frequent migraine headaches;
- pathologies of reproductive function leading to miscarriages and fetal death.
If a woman experiences several of the symptoms listed above, it is advisable to immediately obtain a qualified consultation with a gynecologist.
Adenomyosis
Diffuse changes in the myometrium can be caused by adenomyosis. With this disease, the structure of the muscle tissue becomes heterogeneous, and foci of the endometrium are identified in it.
The main difference between adenomyosis and endometriosis is the localization of germination of the mucous layer. With endometriosis, the lesions are more extensive. Adenomyosis is characterized by ingrowth of the endometrium only into the myometrium and is manifested by diffuse changes in its structure.
Often adenomyosis occurs without obvious signs. With the same degree of probability, a woman may be bothered by abdominal pain and discomfort during palpation. The causes of adenomyosis include trauma to the uterine mucosa and muscle layer. Damage can occur during diagnostic curettage, abortion, or during inflammation.
Treatment of adenomyosis begins with drug correction. The patient is prescribed hormonal drugs that regulate the functioning of the ovaries, anti-inflammatory and painkillers. It is often necessary to introduce an artificial hormonal menopause into a woman. If this technique is ineffective, surgical treatment is performed, which involves removing the reproductive organ. The appointment of surgical intervention is prescribed to patients with mandatory consideration of age and desire for subsequent birth of children.
Treatment
To avoid unpleasant consequences when diffuse changes in the myometrium are detected, early diagnosis and active treatment of adenomyosis are necessary.
Methods for getting rid of this pathology include medication, surgery and combination treatment.
Drug therapy
Treatment of diffuse changes in the myometrium with medications is aimed at:
- to prevent complications;
- to stop the progression of pathology by suppressing estrogen production;
- to preserve reproductive function;
- to eliminate pain syndromes and prevent cancer.
All groups of drugs have many side effects and serious contraindications, therefore they are taken only as prescribed by a gynecologist and after a detailed study of the complete (and not introductory) instructions for the drug by the patient herself.
Main groups of medications:
- Estrogen-progestogen contraceptives (Jess, Janine, Diane 35, Yarina, Demoulin, Non-ovlon, Marvelon).
Able to suppress ovulation and estrogen secretion. They help in the initial stages of structural changes in the endometrium and myometrium. Prohibited if you are prone to thrombosis or have high blood viscosity.
- Progestin drugs - Visanne, Duphaston, Norkolut, Utrozhestan, Getstrinone. Prescribed for varying degrees of myometrial damage.
- Antigonadotropic (agonists of gonadotropic releasing hormones), including Nemestran, Danol, Buserelin-Depot, Danogen, Lucrin-Depot, Zoladex, Diferelin.
When used as injections once every 28 days, significant atrophy of diffuse, nodular and focal changes in the body of the uterus is achieved.
The main advantage of these drugs is the combination of a more pronounced therapeutic effect with a minimal percentage of side effects and relapses.
With combined treatment, including medications and surgery, relapses are diagnosed in only 7 to 12 patients out of a hundred.
Surgery
Surgical treatment consists of maximal removal of concentrations of endometrioid cells.
Among the main methods: laparoscopic surgery, laser vaporization (evaporation of abnormal cells), cryodestruction and radio wave method, in which healthy tissue is not affected and the recovery process is shortened.
After therapy and surgery, a certain interval (from 1 to 4 months) is required before conception for the uterus and the entire body to fully recover.
One of the most popular methods for examining the uterus is ultrasound. Sometimes, based on the results, the patient is informed that she has diffuse changes in the wall of the organ. Questions arise about how dangerous it is and whether there are effective treatments. Women face this kind of problem quite often. The consequence of abnormal changes in the structure of the uterine muscles can be a violation of reproductive function. If pathology is detected at an early stage, it is not difficult to eliminate. In advanced cases, surgery is required.
Myometrial structure
The myometrium is one of the layers of the uterus, which is muscular and is located in the middle of the lining. Its inner side is covered with endometrium. In a normal state, the myometrium is calm, but in the presence of any influencing factors, the muscles begin to contract and become hypertonic.
What is hypertonicity? Local hypertonicity of the myometrium is not a normal condition of the uterus and occurs with local thickening of the myometrium. When it appears, treatment and stimulation must be carried out. When carrying a child, it can lead to termination of pregnancy.
The main role during childbirth is given to the myometrium, because due to the fact that its muscles begin to contract, the fetus is pushed out through the birth canal.
The state of the myometrium is influenced by the state of the hormonal background (the amount of estrogen and oxytocin should be normal).
Uterine epithelium. What characteristics are normal?
The uterus consists of three layers: integumentary, muscular and internal mucosa (endometrium).
The lining of the uterus is formed by several epithelia. Several layers of squamous epithelium line the inside of the vagina (flat cervix). This stratified squamous epithelium (MSE) is sometimes called squamous epithelium and is layered. The cervical canal of the uterus is lined with a single layer of cylindrical cells. Among the cylindrical cells there is a special glandular epithelium that secretes mucus.
Between the two types of epithelium there is a transformation zone: here the MPE passes into the glandular one.
The surface of the cervix is normally smooth and pink, since it is lined with a uniform layer of epithelium, this is the basal epithelium. As a result of a gynecological examination, there should be no mucosal defects or pathological formations on the surface. The Schiller test indicator should be uniformly brown.
Cytological analysis of the mucous membrane on the fragment under study should reveal a single number of leukocytes, as well as flat epithelial cells. The number of white blood cells may vary depending on your menstrual cycle.
Normally, leukocytes are characterized by pure cytoplasm and intact nuclei. Signs of phagocytosis are not observed. A vaginal smear may contain mucus and individual cells with altered cytoplasm.
Changes in diseases
The pathology of the myometrium varies in the thickness and size of each layer.
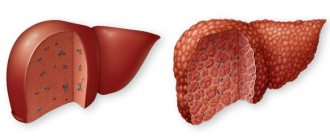
The beginning of the menstrual cycle is characterized by a size of 2-3 millimeters, and the middle by a size of 14-15 millimeters. Also, changes in the myometrium are characteristic of endometriosis or adenomyosis. During ultrasound, changes in the myometrium with endometriosis may be invisible due to the fact that they are most often too small. But it is these changes that lead to the fact that the structure of the myometrium becomes heterogeneous.
Endometriosis is one of the most common diseases among women. It is a pathology of the mucous membrane of the uterus and cervix. It is characterized by the proliferation of endometrial cells outside the uterine cavity.
One of the main determining parameters on ultrasound is the echostructure. Which, in its normal state, has low indicators (with endometriosis the indicators are 1-5 mm).
Endomyometritis is characterized by inflammation of the anterior wall of the mucous and muscular lining of the uterus. Often endomyometritis makes itself felt with quite severe pain, which is caused by introduced infectious bacteria (usually after childbirth or abortion).
Chronic endomyometritis occurs due to improper treatment. Develops gradually. First it penetrates the walls of the endometrium, and then breaks the muscle layer. It is important to know that endomyometritis develops only in the presence of defects in the uterine mucosa. Symptoms include abdominal pain and characteristic discharge. Diagnosis of endomyometritis and its chronic form is not difficult.
When fibroids and inflammation of the uterus occur, the homogeneous structure of the myometrium is also disrupted. Myoma is a benign tumor and when it occurs, the echostructure of the myometrium is disrupted and calcification begins. Diagnosis is carried out using intrauterine ultrasound or three-dimensional echography.
Another disease in which the homogeneity of the myometrium is disrupted is myometritis. Its development is provoked by infections on the uterine mucosa. Symptoms are comparable to those of endometriosis.
Sonographic changes
Sonographic signs of pathological growth of the endometrium are its uniform or local thickening, which does not correspond to the day of the monthly cycle, as well as heterogeneity of the structure. The term echogenicity refers to the ability of human body tissue to reflect ultrasonic waves. Healthy internal organs and various glands have normal echogenicity or, as it is also called, isoechoicity. If an ultrasound sensor detects increased echogenicity and heterogeneity of tissue structure, this may be evidence of pathological changes in the uterine mucosa.
The diagnosis of endometriosis can be confirmed by identifying lesions with abnormal density that are able to perfectly reflect ultrasound waves. In addition, ultrasound determines the thickness of the uterine walls and in the case of endometriosis, this indicator can vary within 4-5 cm.
Heterogeneous myometrium
Changes that occur in heterogeneous myometrium with hyperechoic inclusions can provoke the appearance of not only uterine diseases. Myometrial heterogeneity in the early stages usually does not manifest itself with any symptoms and is detected only during a preventive examination by a gynecologist. But if you do not have time to identify disorders in the early stages, the symptoms can begin to manifest themselves in a very unpleasant way.
Symptoms of heterogeneous myometrium:
- Painful periods;
- Abdominal pain;
- Painful sensations during ovulation;
- Bloody discharge in the middle of the menstrual cycle;
Reasons for appearance:
- Genetic predisposition;
- Trauma during childbirth or caesarean section;
- Disorders of the inner layer of the uterus;
- Psycho-emotional disorders;
- Problems with the thyroid gland;
Diagnostics
Nowadays, medicine makes it possible to detect the appearance of diffuse changes even at their early appearance, which significantly increases the possibilities for successful and rapid treatment. The main diagnostic method is ultrasound, which determines the atypical structure of the homogeneous myometrium.
Methods for performing ultrasound:
- Before the procedure, the woman drinks significant volumes of water to ensure that her bladder is as full as possible.
- Ultrasound using a vaginal probe does not require preparation, but may cause discomfort during deep penetration;
Indications for ultrasound:
- Disruptions in the menstrual cycle;
- Abdominal pain;
- Infertility;
What does ultrasound reveal?
- Uterus size;
- Position of the reproductive system;
- Size and volume of the endometrium;
- Myometrial structure
Other diagnostic methods:
- Examination by a gynecologist;
- Biochemical blood tests;
- Bimanual examination;
- Carrying out an MRI procedure;
Diagnostic methods
Diagnostic scheme:
- Examination by a gynecologist. No changes are detected in the mirrors. On bimanual examination, the uterus is enlarged, spherical in shape, with smooth walls;
- Ultrasonography. Characteristic echo signs speak in favor of diffuse adenomyosis. The structure of the organ reveals multiple anechoic and echopositive inclusions. There is an unevenness of the border between the endometrium and myometrium. Adenomyosis indirectly confirms the enlargement of the uterus in size. The echo picture of the diffuse form of adenomyosis is quite specific, which allows it to be differentiated from uterine fibroids and endometrial hyperplasia;
- CT scan. The heterogeneity of the myometrium is characteristic due to the formation of a large number of foci. There is no clear boundary between the heterotopia and the muscular layer of the uterus. The myometrium has the appearance of a honeycomb;
- Magnetic resonance imaging. On an MRI image, foci of adenomyosis are defined as low-intensity space-occupying formations with unclear contours;
- Endometrial aspiration biopsy. Allows you to take material for histological examination. Performed on an outpatient basis;
- Hysteroscopy. Gives you the opportunity to see the uterus from the inside. Adenomyosis is characterized by the appearance of passages, changes in relief, and wall density. Foci of diffuse endometriosis are distributed evenly throughout the organ. During hysteroscopy, tissue can be taken for biopsy.
Examinations before surgery
Before surgical treatment, all patients undergo preoperative preparation. This includes the following research methods:
- clinical and biochemical blood tests;
- clarification of blood type and Rh factor;
- clinical urine analysis;
- examination of vaginal smears to analyze the nature of the microflora;
- chest x-ray.
These research methods are recommended but not required. This set of examinations allows for a full diagnosis and identification of concomitant pathologies.
Myometrial structure
Myometrium is the middle muscular layer of the uterus, which is a formation of many bundles of myocyte cells with layers of connective tissue. Myometrial structure:
- Submucosal layer - located under the basal part of the uterine layer of the endometrium. It consists of many bundles of muscles located in an oblique longitudinal direction.
- The middle layer is vascular. This layer has the greatest thickness; a large number of small blood vessels - capillaries - pass through it.
- The subserosal (another name for the supravascular) layer contains muscle bundles of a circular and longitudinal type. Located near the serous uterine membrane.
Such a phenomenon as the heterogeneous structure of the myometrium occurs in women aged 20-40 years who do not have children and have never been pregnant only due to the development of pathological processes of various nature in the uterus.
Essence of the question
What is myometrium? The myometrium is the middle layer of the muscles of the uterus, which in turn consists of three layers of muscles. Its structure is as follows:
- The first layer (also known as the outer layer) is the subserosal layer of muscles, which are located in the longitudinal and circular directions. Above this layer is lined the serous membrane.
- Under the first layer is the strongest one - the middle one. It is represented by circular muscles. This layer contains arteries and veins that nourish the uterus.
- The inner layer is represented only by longitudinal muscle fibers.
Thanks to these three layers, the uterus has the ability to contract, expelling blood during menstruation and the fetus during pregnancy. The hormones estrogen, oxytocin and progesterone influence muscle contraction. Their secretion is most intense during menstruation and pregnancy. Normally, a woman should not feel the uterus. It is felt only during labor, birth or pathologies.
Normal indicators
The structure of the myometrium in a woman without a history of pregnancy is homogeneous. Minor heterogeneous inclusions are allowed, but only in cases where there is no alarming symptomatic picture, there are no infectious or inflammatory diseases of the reproductive system.
Layers are not delimited. The thickness increases towards the uterine fundus, which is necessary to ensure full contraction of the uterus during childbirth. The echogenicity index is identical to the norms of the parenchyma of such internal organs - kidneys, pancreas, liver.
Causes of the pathological condition
Heterogeneous myometrium has both a physiological nature and is a sign of the development of pathological conditions of the uterus. Changes in a woman’s body with age lead to physiological heterogeneity in the structure of the uterine layer. There are no symptoms indicating illness. This condition of the uterus is detected only by ultrasound. Reasons for structural change:
- difficult birth with complications;
- the impact of frequent stressful situations;
- operations in the uterine cavity, during which the middle muscular layer of the uterus was damaged;
- genetic predisposition;
- performing a caesarean section;
- thyroid dysfunction.
Depending on the reasons that led to the structural change in the myometrium, an ultrasound examination reveals deviations from the norm in such indicators as tone and echogenicity, the thickness of the uterine layers, and the size of the organ.
How to treat an enlarged uterus
Before treatment, the doctor must identify the cause of this unpleasant phenomenon and make a diagnosis. The treatment method will depend on the diagnosis, it may be:
Drug treatment; — hormonal therapy; - surgical intervention (partial or complete removal of the uterus).
Menstrual Fibrosis: What's Really Happening?
You always try to get rid of drugs because such a thing is never an easy choice as it is painful and takes at least a month to fully recover.
Uterine fibromatosis is an estrogen-dependent pathology, and then with menopause there is certainly a slowing down or even stopping of the growth of fibroids: the disorder in some cases will also tend to be slight and partial regression, but a true and definite cure is unfortunately impossible, Thus , intervention is one of the proposed alternatives, and although women are no longer fertile during this period of life, in any case they try not to have their ovaries removed in order to preserve their psychophysical well-being; this is, of course, if the ovaries were not attacked by the disease. If the cause of an enlarged uterus is fibroids or fibroid tumors, a woman may complain of pain in the back or lower abdomen, bloating, irregular menstruation, or urinary incontinence. She may even feel the uterus putting pressure on nearby organs.
Fibrous tumors can be treated non-surgically or surgically. Surgical options include hysterectomy (gynecological surgery in which the uterus is amputated) or myomectomy (removal of a benign tumor from the muscular wall of the uterus). Non-surgical methods: prescription of medications or embolization of a fibrous tumor (blockage of blood vessels with specially injected emboli).
However, the sexuality and sex life of a woman with a fibromatous uterus are not affected: indeed, some studies show an increase in pleasure and libido and therefore an improvement in sexual performance. The only real prevention that can be achieved is to monitor your health over time with regular checkups with a gynecologist, as early diagnosis can save your fertility.
Hypertrophic and elastic fibers. This increase and expansion of the spiral muscle fibers before birth is of great importance in increasing the contractile capacity of the uterus. In the first half of breast enlargement, the uterus is mainly due to increased muscle mass, and in the second half due to stretching and growing fetuses. Significantly increased blood flow to the uterus. The surface of the uterus under the peritoneum develops a dense, dilated varicose vein. Blood circulation increases significantly, which determines the risk of bleeding during injury and childbirth.
At an early stage, the uterus can be returned to its previous size; the most important thing is not to ignore the symptoms indicating its enlargement.
Having heard from the gynecologist about the change in the size of the female organ, the patient asks the question: the uterus is enlarged - what does this mean?
The development of varicose veins determines the tendency to thrombophlebitis and BTE both before and after birth. Oxygen consumption also increases, and its birth date is higher than that of the brain. The so-called lower segment of the uterus is formed. The muscles of the ostrum are too weak and do not participate in the movement of the fetus during childbirth. Excessive stretching of the hip walls of osteoarthritis can lead to rupture in the area of the old cytrarrhea in the polyfinger. The height of the uterus depends on changes in the device. This is extremely important for vaginal delivery - matte stick to the pelvis.
The uterus is a hollow organ designed to bear a fetus. In women of reproductive age, its size is 8 cm, and its weight is from 50 to 80 g. If an enlargement of the organ occurs, the patient is sent for examination.
This condition is common among women before menopause. Age affects the size of the uterus, and this is normal. But if a woman experiences painful symptoms, then pathology may develop. A thorough diagnosis will help identify it.
In 80% of cases before birth, the uterus is slightly curved to the right, as the left edge and left apnea approach the anterior abdominal wall, and the right ones move away. The position of the uterus also depends on the position of the body - if a pregnant woman lies on the left, the fundus also tilts to the left and back.
Peskakek's sign - when implanted near the uterine horn, a limb is formed that causes asymmetry of the uterine body. The ovary that gave rise to the corpus luteum is larger. His development then slowed down to 16 weeks. stops functioning. Follicular maturation stops - no ovulation. The mucus is hypertrophied, becomes swollen, and slanted.
The uterus is enlarged in the following diseases:
- Myoma is a benign tumor. This is the most common disease in which the size of the uterus changes. The disease occurs in women of reproductive age. It is dangerous due to its complications: possible transformation into a malignant tumor, miscarriage, infertility. Myoma is caused by hormonal imbalance, irregular sexual intercourse, sexual disharmony, past abortions, hereditary predisposition, obesity, diabetes and many chronic diseases. Insufficient physical activity is also considered a provoking factor.
- An ovarian cyst is a cavity filled with fluid. The development of a cyst often leads to an increase in the size of the uterus. Abdominal trauma and hormonal imbalance in the female body can cause a cyst.
- Adenomyosis of the uterus is the growth of the endometrium into the uterine layers. With this disease, there is an overgrowth of the muscle membrane, which leads to an enlargement of the organ. If the hormonal balance is disturbed, some kind of surgery was performed on the organ, or abortions were performed, then the development of adenomyosis is possible.
- Oncology. Malignant neoplasms are observed in women of all ages. But those who have started menopause are especially susceptible to them. An enlarged uterus is one of the symptoms of the disease. The development of a tumor is more likely in women who are prone to obesity, in nulliparous women and in those who approach menopause at a late age.
- State of molar pregnancy. This pathology is associated with abnormalities of the placenta. With it, the fetal tissue begins to grow. Molar pregnancy is associated with genetics - a genetic error occurs during fertilization.
Any of these pathologies requires examination and treatment.
Varicose veins are common, especially in the lower third of the vagina and vulva, and are a condition for severe bleeding during childbirth. Juicy, bluish, stronger pigment. Bartholin, sweat and sebaceous glands are secreted more abundantly. Under pressure, the calastrum may disappear. Changes in the mammary gland are caused by: placental estrogen; progesterone; prolactin.
Drowsiness, unbalanced behavior, changes in taste and smell, increased salivation, constipation, morning vomiting. The latter suppresses follicular development and prevents ovulation, hormones, estrogens, progesterone, lactogenic hormone. Radially around the navel of the chest in the hips of the breeches. . Gradual relaxation, stretching, thinning, especially noticeable in the navel area. This creates the preconditions for the appearance of hernias. In Primaria it is less pronounced. In large ears, the presence of small hernias up to Br leads to expansion and intensification of complaints.
General symptoms
If heterogeneity of the myometrium is caused by injuries and pathologies of the uterus, a number of symptoms are observed:
- severe, prolonged pain in the lower abdomen during menstruation;
- disruption of the menstrual cycle – periods start late and take too long;
- vaginal discharge mixed with blood, the appearance of which is not associated with menstruation;
- inability to conceive a child with regular sexual activity.
https://youtu.be/b4hZ_t1W4CY
Signs appear in the later stages of development of the pathological process, when the disease that caused the structural change in the myometrium has already led to a number of complications. With age, the production of female hormones decreases, which causes a change in the structure of the myometrium, which will be heterogeneous throughout its entire volume.
Symptoms of the disease, treatment
Changes in the structure of the endometrium can be asymptomatic or, conversely, acute.
The clinical picture is based on the disease, which entailed disturbances in the homogeneity of the mucous membrane. At an early stage, a disruption of the menstrual cycle occurs, menstruation is inconsistent and painful. A girl or woman develops whitish discharge and pain in the lower abdomen.
Failure to promptly contact a gynecologist with this problem can lead to serious complications, namely:
- Oncology
- Hematometra (rupture of the endometrium and accumulation of blood in the uterine cavity)
- Bleeding
Treatment of diseases that affect the heterogeneity of the mucous membrane plays the most important role.
In addition to the main therapy, the sick woman is prescribed a course of hormonal medications and antibiotics. A course of physiotherapy is prescribed strictly according to indications and only in the absence of a feverish state.
In case of a chronic process or a condition that threatens the woman’s life, surgical intervention is performed. Its essence lies in the fact that during the operation the affected part of the endometrium is excised.
A specialist will talk about disturbances in the structure of the endometrium in the video:
The border between the heterogeneous structure of the uterine mucosa and its transition to a pathological state is very thin. The essence of prevention of this type of pathology is the fight against the appearance of gynecological diseases that cause disruption of the structure and thickness of the endometrium.
Diagnostic results
Detection of a heterogeneous structure during ultrasound diagnostics is not a basis for immediate therapy. Only a doctor can correctly decipher the diagnostic results, having data on other parameters of the uterine cavity and the general condition of the organs of the genitourinary system.
In the absence of any pathologies, the structure of the middle layer of the uterus, the myometrium, is homogeneous. The thickness of the fundus differs from this indicator in the middle part, which is a physiological norm, since in this way the functionality of the uterus is maintained.
Deviations from the norm are hypoechoic and hyperechoic inclusions in the echostructure of the layer. Myometrium with hyperechoic inclusions does not always indicate pathology. If this indicator is detected, additional diagnostics are carried out.
In pathologies, the following results are found:
- With uterine fibroids, the structure of the middle muscle layer is heterogeneous in some places, and on ultrasound examination it looks like foci. The entire myometrium is strongly compacted.
- Nodular myoma – the echostructure of the myometrium is heterogeneous, the vascular pattern is mottled along the periphery. Myoma nodes appear hypoechogenic.
- Diffuse myoma is a uniform compaction of the uterine tissue, hyperechogenicity is detected in the form of inclusions of different sizes.
- Endometriosis is the proliferation of cells outside the endometrium. This disease is the most common cause of structural changes in the muscular layer of the uterus. During an ultrasound examination, endometriosis is revealed as a cellular heterogeneous structure of the myometrium; formations between the uterine cavity and neighboring organs, similar to fistulas, are detected.
- With myometritis (a complication after an inflammatory process on the uterine mucosa), there are no symptoms. Ultrasound reveals heterogeneity in the structure of the myometrium; in the protracted form, adhesions are present.
Why does this happen?
The main causes of heterogeneous myometrium:
- and its internal genital type, also called uterine adenomyosis.
- Myometritis. In the vast majority of cases, it is a consequence of complicated endometritis, so in fact we are talking about endomyometritis.
- . It can lead to local nodular changes or almost total thickening of the myometrium (in the diffuse form of the disease).
Each of these diseases not only has special symptoms, but also leads to characteristic changes in the myometrium. They can be differentiated using ultrasound; in the protocol of the study, the specialist describes the echographic picture of the detected pathology and indicates its type.
Adenomyosis is the most common cause of myometrial changes
Endometriosis is the pathological growth of endometrial cells outside the lining of the uterus. With predominant damage to the myometrium, they talk about it, which can be of diffuse and nodular type, and of varying degrees of severity.
This disease is classified as benign hyperplasia of a hormonal-dependent nature. So it is typical for women of reproductive age, and in the postmenopausal period and against the background of adequately selected hormonal therapy, the activity of the process subsides.
With adenomyosis, growths of endometrioid tissue appear in the myometrium. They can be of two types:
- In the form of blind branched deepening pockets communicating with the endometrial layer of the uterus. In such cases, the ultrasound report usually indicates that the echostructure of the myometrium is heterogeneous and cellular. In severe degrees of the disease, germination of the entire thickness of the myometrium is noted, which is accompanied by the formation of fistula-like formations between the uterine cavity and other structures of the small pelvis.
- In the form of nodes - closed round lesions with an uneven central cavity filled with blood or a chocolate-colored liquid mass. They are usually multiple, of varying sizes, with an uneven distribution in the uterine wall. With this variant of the disease, the conclusion of an echographic examination usually notes that the myometrium is heterogeneous with signs of adenomyosis.
Any endometriotic formations undergo repeated changes in accordance with a woman’s ovarian-menstrual cycle and lead to an inflammatory process. Under the influence of sex hormones, cells of the abnormally located endometrium grow and are rejected in the same way as in the uterine mucosa. This leads to the appearance of clinical symptoms of the disease.
Adenomyosis is characterized by cyclic uterine bleeding, which is more profuse and painful compared to normal menstruation. And the emptying of stagnant cavities and endometrioid pockets leads to the appearance of chocolate-colored discharge from the genital tract. They are actually menstrual blood that has accumulated and undergone incomplete decomposition.
Adenomyosis can lead to chronic iron deficiency anemia and persistent pelvic pain. It is also a common cause. Therefore, pregnancy planning requires an ultrasound scan as part of a comprehensive examination, even if the patient does not have obvious clinical symptoms of endometriosis.
Changes in the myometrium with fibroids
Myoma is a benign neoplasm of the uterus of hormonal-dependent etiology. The peak incidence occurs at the age of 40-45 years, which is associated with age-related endocrine changes in the reproductive system.
Fibroids and their location relative to the uterus
Most often, fibroids look like a node caused by local proliferation and hypertrophy of cells in the muscular layer of the uterus. Such a formation can be located in the thickness of the myometrium or protrude towards the mucous or serous layers, having a wide base or a formed pedicle. Myomatous nodes can be single or multiple, of different sizes and locations. A more rare form of the disease is diffuse myomatosis.
The ultrasound picture of fibroids depends on the form of the disease:
- In the nodular form, ultrasound reveals local changes in the myometrium with enlargement and deformation of the uterus. Myomatous nodes are usually hypoechoic, heterogeneous in structure, with an increased vascular pattern in the periphery. In the thickness of large formations, foci of softening, necrosis, local hemorrhages, and calcifications can be detected.
- In the diffuse form of myomatosis, the uterus is almost uniformly thickened and enlarged. Its muscle layer has a heterogeneous, predominantly hypoechoic structure, with uneven foci of fibrosis. Diffuse myomatosis is often accompanied by the process of tissue calcification. In this case, ultrasound describes that the myometrium is heterogeneous with hyperechoic inclusions.
Myoma can lead to pelvic pain, recurrent acyclic uterine bleeding, and algodismenorrhea. But a low-symptomatic form of the disease often occurs, when neoplasms are detected in the absence of certain complaints. And the diagnosis is based on data from a gynecological examination and ultrasound of the pelvic organs.
Pregnancy
Sometimes during pregnancy, women undergoing examination are faced with the concept of “heterogeneous myometrium” - what does this mean? On ultrasound, this means that a pathological process may be occurring.
When a pregnant woman undergoes an ultrasound, the goal is not to examine the muscular uterine layer; the doctor’s task is to assess the condition of the fetus and uterus as a whole. As a rule, at this moment, a heterogeneity of structure is accidentally discovered in a pregnant woman.
The condition of the muscle layer in pregnant women is monitored if its heterogeneous structure was diagnosed before pregnancy. In late pregnancy and during childbirth, the myometrium, if its structure is highly cellular, can rupture. This complication can only be avoided by conducting a complete examination of the woman before pregnancy.
If the structure of the muscle layer is heterogeneous and a pregnant woman has an alarming symptomatic picture, she must be registered with regular examination by a doctor. Pathologies leading to changes in the state of the myometrium at the structural level can cause severe complications during childbirth.
The presence of fibroids in a pregnant woman can lead to a difficult pregnancy. During natural childbirth, there is a high risk that the uterus will not contract enough, and heavy uterine bleeding may occur. If the pathological process is prolonged, fibrosis may occur and scars will form, which will lead to rupture of the birth canal.
In the early stages of pregnancy, a structural disorder causes increased uterine tone. With this pathology there is a high risk of arbitrary termination of pregnancy. In the later stages, uterine hypertonicity, caused by heterogeneity of the myometrial layer, can cause premature obstetrics.
Myometrium during pregnancy
The appearance during pregnancy is one of the important reasons requiring immediate consultation with a doctor. Despite the fact that an increase in uterine tone does not always lead to or, this condition is accompanied by compression of the vessels supplying nutrients and oxygen, which negatively affects its development.
Myometrial hypertonicity during pregnancy can occur as a result of exposure to the following factors:
- decrease during the first 10 weeks of pregnancy (during the period when it is not yet fully mature for independent functioning);
- increased levels of androgens (male sex hormones);
- inflammatory diseases of the female genital organs;
- infantility (underdevelopment) of the uterus.
To prevent the occurrence of myometrial hypertonicity during pregnancy, it is recommended:
- determining the level of hormones in the body at the stage
Endometriosis, which is characterized by heterogeneity of the myometrium, is considered one of the dangerous diseases of the female body. These diseases often become one of the causes of infertility. It is for this reason that it is important to know the causes of endometriosis, its first symptoms and treatment methods.
Danger of diffuse changes in the myometrium
If a woman is diagnosed with endometriosis, she experiences disturbances in the homogeneity of the myometrial structure. It should be noted that such a tumor is benign. Until today, it is generally accepted that the cause of this phenomenon is the improper functioning of endometrial cells. This phenomenon occurs against the background of the fact that the endometrium itself begins to grow at an accelerated pace.
Speaking about the normal state of the female body, a homogeneous structure of the myometrium is observed, this indicates the well-coordinated work of myocytes, and during the onset of labor they have maximum contractile force. If a woman’s endometriosis progresses, bumps begin to appear on the myometrium. Nodes begin to be visible in its structure, and a change in the function of the myometrium occurs.
If a woman has been diagnosed with endometriosis, she should not worry about her life, since it does not lead to death. However, there is one serious disadvantage: as a result of this disease, a woman with almost 100% probability cannot have children. In terms of the development of infertility, diffuse focal endometriosis becomes especially dangerous, in which the affected cells accumulate in one area of the uterus, creating a focus. This also causes a heterogeneous structure of the endometrium; the uterus may be in hypertonicity, which ultimately causes various pathological consequences.
In the future, if the woman does not take any action, then extremely unpleasant symptoms may be added to those described above, for example, the occurrence of heavy bleeding between periods. However, the worst thing in this case is that with such a disease, a woman is not able to get pregnant. The only way to return all the joys of motherhood to her is only to restore her hormonal levels, as well as subsequent treatment of existing endometriosis.
What pathologies do reactive changes indicate?
Accidental trauma to the epithelial surface, which occurs as a result of surgery, improper douching or sexual intercourse, can lead to erosion. The integrity and structure of the epithelial coating is disrupted. The infectious process in the acute phase is one of the main causes of erosion. Sometimes, as a result of a pathological process, rotting of the squamous epithelium of the uterus occurs.
Erosion is a temporary process. As a rule, after 2-3 weeks the damaged area is restored, covered with lining epithelium and healed. Erosion refers to secondary changes in the cervix, that is, those that are associated with a change in the shape of the cervix, as well as displacement of the mucous membrane. The structure of the tissues does not change.
In the scientific literature, pseudoerosion is referred to as ectopia of the cervix. This type of reactive changes in epithelial tissue does not require any therapeutic intervention. Pseudo-erosion occurs during embryogenesis during the formation of the reproductive system in the fetus. Visual examination reveals areas of redness that stand out against the pink and smooth surface of the uterus. A cluster of cylindrical cells forms around the os of the uterus.
False erosion can be detected using colposcopy. The reddened area is not stained with iodine solution. If ectopia occurs as a result of childbirth, the doctor may prescribe a cauterization procedure.
Leukoplakia is a condition in which a white spot appears on the cervix, that is, squamous acetowhite epithelium (ABE) appears. Leukoplakia is characterized by thickening of the uterine epithelium. The white epithelium arises from keratinization of cells; the mature metaplastic epithelium hardens into a keratosis. This process is not the norm. Such a reactive change in epithelial tissue is considered a precancerous condition. It needs to be diagnosed and treated in time to avoid the development of cancer.
Erythroplakia is a pathology during which dark red or burgundy areas without a specific shape form on the surface of the cervix. In the affected areas, the epithelial tissue begins to thin out. The affected area changes its color depending on the degree of atrophic changes.
The reason for the reactive change is a violation of the microflora of the genital tract. To study the inflammatory process in detail, a hormonal analysis is prescribed, because Problems in the endocrine system can lead to the development of thinning.
Cervical dysplasia is a pathological process in which atypical formations appear at the junction of single-layer and multilayer epithelial tissue. Another name for dysplasia is neoplasia of the cervical epithelium. The main reason for this reactive change is the herpes virus and human papillomavirus. Dysplastic processes occur in three stages (designated CIN1, CIN2, CIN3), complications of the latter are very dangerous.
A polyp of the cervical canal occurs as a result of abortion and improperly performed gynecological manipulations. Damage received after sexual intercourse leads to protrusion of uterine tissue into the cervical canal, and a polyp is formed. Persistent inflammation of the genital tract is one of the main causes of the appearance of polyps. Usually the pathology is removed through surgery.
Lesions caused by HPV
HPV is one of the most dangerous viruses for reproductive health; some of its varieties are oncogenic. A wart resembles a papilla in appearance. Usually the spread is focal.
Flat papilloma of the cervix is a small single or multiple tumor. It is formed by two types of tissues - connective and epithelial. The virus causes cells to proliferate after infection. The peculiarity of uterine papilloma is its flatness; in other localizations, papillomas may look different.
Cervical condyloma is one of the most dangerous lesions of the female reproductive system. It is caused by the human papillomavirus. The most serious complication of condylomas is infertility, the formation of cysts on the ovaries. Human papillomavirus infection (PVI) requires timely diagnosis and treatment. The main symptom of this disease is the abnormal proliferation of multilayer epithelial tissue, such as acanthosis. Acanthosis is a pathological condition in which the integumentary cells become rough; there are two types - malignant and benign.
Causes of myometrial heterogeneity, why does this happen?
Among the most common causes of myometrial heterogeneity are:
1 Adenomyosis is one of the types of endometriosis, in which the inner mucous membrane of the uterus begins to grow into its other layers and even beyond the organ.
2 Endomyometritis is an inflammation of the mucous and muscular lining of the uterine body, which is often a complication of endometritis.
3 Uterine fibroids are a benign neoplasm in the muscular layer of the uterus. In this case, myomatous nodes can develop in a woman’s body or the myometrium can completely thicken, which is typical for the diffuse form of the disease.
Any of these diseases affects the appearance and condition of the myometrium. An ultrasound of the pelvic organs, which will reveal an echographic picture, will help to establish an accurate diagnosis.
Diseases
If the structure of the uterus is heterogeneous, what this means should be explained by the attending physician. The fact is that such a condition of the lining layer of the reproductive organ can develop as a result of the progression of gynecological diseases. Let's consider several of the most common pathologies in which the structure of the uterus is revealed to be heterogeneous, what this can mean.
Endometriosis. The presented disease is quite often diagnosed in women of different ages. The main feature of the pathology is that as it progresses, there is a diffuse enlargement of the uterus, namely, the endometrial layer.
Violations are detected through a diagnostic procedure such as ultrasound. It is this procedure that makes it possible to notice that the endometrium has begun to grow beyond the reproductive organ, and the echostructure is heterogeneous.
Endomyometritis. With the development of the inflammatory process, diffuse changes in the myometrium of the uterine body may be observed. The pathological focus is located on the mucous membrane of the reproductive organ, as well as in the muscle layer. A distinctive feature of the disease is that it develops with severe symptoms.
Since there are pathogenic bacteria in the uterus, the woman complains of a high degree of painful syndrome. Microorganisms can penetrate the reproductive organ during artificial abortion, labor, or during diagnostic gynecological procedures.
Myoma. Considering the conditions in which there is a diffusely heterogeneous structure of the uterus, what it is and how it manifests itself, it is necessary to remember about fibroids, which are represented by a benign tumor. As this disease progresses, the patient experiences changes in the homogeneity of the myometrium and also develops calcification. To confirm the diagnosis, vaginal ultrasound screening or three-dimensional echography is performed.
Myometritis. A pathological process in which the structure of the uterus is diffusely heterogeneous can also develop as a result of oversaturation of the vaginal environment with infections, in which bacteria settle on the mucous membrane of the reproductive organ. With the development of this disease, a woman will experience symptoms similar to endometriosis, so differential diagnosis is required.
All about diffuse changes in the myometrium
In order to determine the presence of such a disease in women at different stages, only the newest, latest, high-tech equipment is used, thanks to which timely treatment can be prescribed. When identifying signs of the disease, the most important sign, as before, remains the echostructure of the myometrium. The presence of this sign can be determined by performing an ultrasound examination of the pelvic organs. If the atypical echostructure of the myometrium is determined, we can immediately assume that the woman has endometriosis. There are also other diagnostic options that can determine the presence of heterogeneity in the structure of the myometrium.
Changes in the myometrium during adenomyosis, causes
Endometriosis is a fairly common gynecological disease in which endometrial cells grow outside the uterus. If foci of endometrial growth are localized primarily in the uterus, then this disease is called adenomyosis. According to its morphological forms, adenomyosis can be diffuse, nodular and mixed. And the severity of this disease depends on the depth of penetration of the pathological tissue into the muscular layer of the uterus.
Adenomyosis is a type of benign hyperplasia that occurs as a result of hormonal imbalance. Therefore, women who have entered reproductive age are susceptible to this disease. Against the background of fading sexual function, most patients experience a decrease in the foci of adenomyosis and their gradual atrophy.
Types of adenomyosis:
1 Diffuse - represents a uniform distribution of pathological tissue over all walls of the muscular tissue of the uterus, in which so-called blind pockets appear. The depth of these pockets varies, in some cases they can even form fistula tracts into the pelvic cavity.
2 Nodular - characterized by the appearance of multiple compactions (muscle conglomerates). They come in different sizes and are randomly scattered throughout the inner lining of the uterus. These pathological elements are usually filled with transparent or brown content. Ultrasound of the pelvic organs with this type of disease shows heterogeneity in the structure of the myometrium with signs of adenomyosis.
3 The mixed type of adenomyosis is represented by both types of elements.
The myometrium of every woman undergoes cyclical changes every month, and in the presence of endometroid tumors, such changes can trigger the onset of the inflammatory process. Foci of endometriosis located outside the uterus undergo the same changes as the lining of the uterus itself. They grow in preparation for the implantation of an egg and then are rejected, in other words, they menstruate. It is these factors that provoke the appearance of characteristic symptoms.
Women experiencing adenomyosis complain of heavy and very painful menstruation. The diffuse type of adenomyosis with many blind pockets causes a change in the color of the discharge, because during menstruation the brown contents of these pockets come out. In fact, this liquid is menstrual fluid that has already begun to decompose.
Heavy discharge can lead to symptoms of anemia: fatigue, apathy, and disability. Complaints of pain in the pelvic area are also quite common in such patients. Currently, adenomyosis is considered one of the most common causes of infertility due to the formation of adhesions, disruption of the anatomy of the fallopian tubes, or hormonal imbalance. That is why, during pregnancy planning, all women are recommended to undergo an ultrasound of the pelvic organs, even in the absence of signs of endometriosis.
What is this pathology?
Diffuse changes in the myometrium occur due to the development of endometriosis in the uterus, that is, the pathological proliferation of cells of the mucous membrane lining its cavity. The process can spread both outside the uterus and affect the muscular layer of the wall (myometrium). If the pathology affects the muscles, then it is called adenomyosis, and diffuse changes are observed on ultrasound. The walls of the uterus look thickened and heterogeneous due to the growth of endometrial cells into them.
As a rule, diffuse changes occur in women of reproductive age (most often in 25-30 year olds). They are less common after menopause.
The myometrium has several layers: internal (consisting of longitudinal muscles), middle (of circular muscles and blood vessels) and external (longitudinal muscles are covered with a durable serous membrane).
With adenomyosis, individual cysts filled with blood are formed in the myometrium, as well as cells formed by modified glands that penetrate from the mucous membrane into the muscle layers. In addition to diffuse changes in the myometrium, in which extensive damage to its wall occurs, there are also nodal (in separate areas isolated from each other) and focal (fibroids - benign tumors).