Category: smear Published 12/31/2017 · Comments: Comments to the entry Squamous epithelium in a smear are disabled · Reading time: 5 min · Views: - 5,093
Tests help track the activity of the reproductive system at the deepest levels. When visiting a gynecologist, almost every woman is prescribed a smear for microflora.
This analysis monitors the general nature of the discharge and is also aimed at determining the concentration of various substances in the smear. One of these is the epithelium. Should it be in the smear at all and what does a high concentration of cells indicate?
Why find out the concentration of epithelium?
Epithelial cells are skin tissue cells.
There are 2 types of them:
- flat;
- cylindrical.
The epithelium must be contained in the smear, but only in a certain amount. This phenomenon can be explained by the fact that the vaginal and uterine cavities are covered from the inside with squamous epithelial cells.
If the concentration of squamous epithelium begins to increase, this indicates an inflammatory process and other pathological conditions of the genital organs. If the cylindrical epithelium grows, tumor processes are most likely occurring in the woman’s body.
Sometimes it happens that epithelial cells in a smear are not detected at all during analysis. This phenomenon can occur due to a large amount of the hormone testosterone in a woman’s body and general hormonal imbalance, as well as due to the death of epithelial cells due to certain diseases.
Colpocytogram indices
A vaginal smear can be used for a colpocytogram, a study that determines the content of various types of epithelial cells in the vaginal discharge.
The percentage of epithelial cells changes depending on the day of the cycle, that is, under the influence of hormones. Hormonal colpocytology is used to clarify a number of diagnoses, including hormonal infertility, pathological menopause, and amenorrhea.
In addition, the study helps to accurately identify the day of ovulation, which is important in the treatment of certain types of infertility and for determining the duration of pregnancy.
For hormonal cytological diagnostics, freely detachable biomaterial from the vagina will be required.
Smears are taken every 4 days over several menstrual cycles. This is usually done on days 8, 14 and 22. For amenorrhea, a smear is taken once a week.
READ Composition of vaginal microflora according to microscopic examination of a smear
Contraindications for colpocytological examination:
- inflammation of the vagina;
- uterine bleeding.
The detection of young parabasal cells in a smear (the norm for them is to be at the base of the epithelial tissue, and not on its surface) indicates a disruption in the processes of epithelial maturation. Most likely, the defect is due to weak hormonal levels.
Based on a colpocytological study, the doctor derives a maturation index (MI), showing the percentage of cells in the main, intermediate and superficial layers of epithelial tissue in the smear. The index consists of three digits from 0 to 100.
The first shows the percentage of parabasal cells, the second - intermediate, the third - superficial.
Table 1. Decoding of the IP
| Parabasal | Intermediate | Superficial | Diagnosis |
| There is | No | No | Severe atrophy |
| There is | There is | No | Moderate atrophy |
| No | There is | There is | Moderate proliferation |
| No | There is | There is | Pronounced proliferation |
Note: proliferation is the growth of tissue, atrophy is the thinning of tissue.
KPI or CI is an important index that shows the level of estrogen production. The CPI changes during the menstrual cycle in accordance with changes in the amount of estrogen. During ovulation, the index will be maximum - 60 - 80%.
EI is the second index characterizing estrogen saturation. During ovulation it is 45%.
Crowding index - noted on the study form not with numbers, but with plus signs. Using this indicator, the level of influence of progesterone on epithelial tissue is assessed.
Three plus signs indicate severe crowding, two indicate moderate crowding, and one indicates mild crowding.
A cytological study of hormonal levels is carried out in cases of threatened miscarriage and cycle disorders. The method allows you to evaluate the functioning of the ovaries and the level of estrogen saturation.
Cytology is used to evaluate treatment, monitor hormonal changes during menopause, and identify the threat of miscarriage.
Interpretation of results requires professional qualifications. It is better not to try to decipher the symbols and numbers written in the laboratory on your own, since the interpretation of the smear results should be carried out taking into account a number of additional factors: day of the cycle, gestational age, etc.
READ What does the presence of cocci in a smear mean in women?
Indications for taking a smear
The smear is part of a routine examination by a gynecologist. It is also recommended to take it if a woman is bothered by the following symptoms:
- painful sensations in the lower abdomen that appear outside of menstruation;
- an unpleasant odor appeared from the vaginal cavity;
- the nature of the discharge has changed;
- the genitals are very itchy.
Also, such an analysis is mandatory for women who are planning to become pregnant or are preparing for immediate conception. Another indication for a smear test is long-term antibiotic therapy.
Preparing for analysis
Carrying out gynecological tests requires particularly careful preparation. If the patient neglects it, then she will most likely receive unreliable results. Before taking a smear for the presence of epithelium, you must adhere to the following rules:
- take the test no earlier than the 5th day of the cycle;
- 24 hours before the study, avoid sexual intercourse, douching and the use of medications that are introduced into the vaginal cavity;
- You should also stop using vaginal lubricants, they greatly change the structure of the vaginal flora;
- 2 hours before taking a smear, do not visit the toilet (do not urinate).
The biomaterial is collected using special sterile instruments. A smear is taken from the cervix and vaginal cavity. In some cases, a smear is taken from the urethra, or more precisely from the external opening of the urethra.
After taking a smear, the material is applied to a glass slide and marks are made accordingly (U - smear from the urethra, C - from the cervix and V - vagina). Then the finished slides with the biomaterial are sent to the laboratory.
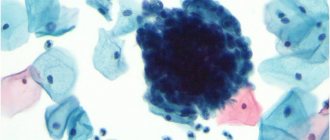
Epithelial cells are stained with special dyes and examined in the laboratory. All components of the smear are painted in different shades and, due to the color difference, the nature of the genital discharge can be identified and assessed.
Methods for eliminating atypical cells
If there is a large amount of atypical epithelium, radical methods aimed at destroying cells may be required. After this, the number of cells is normalized, and the epithelium in the smear is restored. The norm for women during the recovery period is individual, so after surgery, after some time you need to visit a gynecologist and take a smear test again.
The following methods are usually used to treat dysplasia:
- Laser therapy is the most modern and effective method. In addition to removing the atypical area, you can also examine its depth and act on all layers of tissue. This procedure is very painful and traumatic, so bleeding may begin after a few days.
- Diathermy - cauterization, is the effect of electricity on an atypical area. It is the fastest and easiest method. After cauterization, scars may remain on the cervix, which in some cases cause the development of infertility.
- Cryothermy is the effect of ultra-low temperatures on the damaged area. The method is effective only in the initial stages of dysplasia. With the development of cancer cells or the occurrence of atypical processes in the cells of the basal layer, it does not produce any results.
All these procedures are aimed at destroying atypical cells under the influence of temperature or a laser beam. In place of the destroyed cells, squamous and cylindrical epithelial cells appear, which are normal for the cervix and vagina.
The epithelium in the smear, the normality of which has been restored after such procedures, will not carry the risk of developing cancer. If the treatment procedures are not effective, it is likely that a hyperectomy (removal of the uterus and cervix) will have to be performed.
A flora smear is aimed at identifying infectious and inflammatory diseases of the urogenital area (cervical canal, vagina and urethra). Microscopy of a smear from the surface of the mucosa allows you to determine the number of epithelial cells and inflammatory cells (leukocytes), the type and number of microorganisms present (bacteria, protozoa or fungi).
A smear is taken in the mirrors using a spoon, brush or a special bacteriological loop, after which the material is distributed in a thin layer on a glass slide and dried at room temperature. It is mandatory to mark the place where the smear is taken. The resulting preparation is stained and examined under a microscope.
The most informative smear is when:
- the material is collected during the active phase of the disease.
- no local or general treatment was carried out before taking the material, or 4 weeks after the end of taking antibacterial drugs orally, or 10 days after local treatment.
- The material is collected in the middle of the menstrual cycle (in the absence of obvious clinical manifestations of the disease) or in the active phase of the disease in the absence of bleeding.
- during the day before the procedure there was no sexual intercourse, no use of any vaginal means, including douching, vaginal douches, tampons.
- toilet of the external genitalia on the eve of the study was carried out without the use of soap and gels.
- It is not recommended to take a bath the day before collecting the material.
- It is not advisable to conduct a transvaginal ultrasound or colposcopy one day before the smear.
- It is also not recommended to urinate 2 hours before the smear.
It is not prohibited to take a smear for flora on other days, however, you need to understand that the diagnostic significance will be low due to the large number of false positive results.
In any case, the conclusion about the presence of any disease should be based on two criteria - clinical manifestations and smear results.
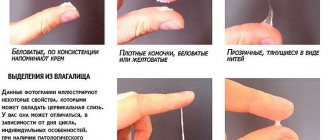
Flora smear is normal
The normal microflora of the vagina is very diverse and contains a large number of bacteria. In women of reproductive age, the dominant microorganism is lactobacilli , however, in addition to them, ureaplasma (in 80%), gardnerella (in 45%), candida (in 30%) and mycoplasma (in 15%) are found - these are opportunistic microorganisms that, when reduced, immunity can multiply excessively and lead to inflammation and require appropriate treatment. In the absence of clinical manifestations, such as pathological discharge with an unpleasant odor or itching in the perineal area, the detection of these microorganisms should not be interpreted as pathology.
Chlamydia and viruses can also be found in women who do not show any complaints, however, these agents are not part of the normal microflora and their presence indicates a hidden infection.
The vaginal microflora is dynamic and can change on different days of the menstrual cycle. There are periods when lactobacillary flora dominates and days when gardnerella predominates. A significant imbalance of microorganisms, accompanied by clinical symptoms, underlies conditions such as bacterial vaginosis and candidiasis. These conditions can often recur with even the slightest change in the woman's general health or the use of antibiotics. Women with a family predisposition are especially affected.
A flora smear (general smear) is the first step in assessing the infectious and inflammatory process of the urogenital area. It allows you to quickly determine one of the following conditions:
- Norm
- Vaginal microflora disorder - bacterial vaginosis
- Infection caused by fungi of the genus Candida - thrush
- Sexually transmitted infections - gonorrhea and trichomoniasis
- Nonspecific (bacterial) vulvovaginitis - leukocytes in a smear in large numbers without detectable specific microbial flora. If a large number of leukocytes are detected in the smear and there is a clinical picture of inflammation, it is possible to prescribe a broad-spectrum antibiotic that destroys up to 90% of bacteria. In the absence of a therapeutic effect, to determine the infectious agent, it is necessary to carry out bacteriological culture, since it is microscopically impossible to determine the exact type of microorganism that caused the inflammation. Bacterial culture is usually accompanied by determination of sensitivity to antibiotics, which allows you to select the optimal drug and achieve a good treatment effect.
A flora smear DOES NOT DETERMINE:
- Hidden and intracellular infections (herpes, HPV, chlamydia, mycoplasma, ureaplasma, HIV). To identify these agents, it is necessary to determine the agent's DNA by PCR.
- Pregnancy
- Pretumor (cervical dysplasia) and tumor (cancer) pathology . For this purpose, there is a cytology smear, the essence of which is to determine qualitative changes in the epithelium using special stains.
Flat epithelium in a smear
Quite often in the smear results you can see the phrase “squamous epithelium in large quantities.” What does it mean?
Normally, the smear should contain squamous epithelium - these are desquamated cells of the mucous membrane of the cervix and vagina. The norm is considered to be no more than 10 cells in the field of view, although this is a relative indicator. An increase in the amount of desquamated epithelium can be observed during the inflammatory process, irritation of the mucous membrane (including active sexual activity) and the use of various vaginal products and procedures.
If a large number of epithelial cells (30-40-50 or more) are detected in a smear, it is first necessary to exclude inflammation!
Degrees of vaginal cleanliness
When analyzing a smear for flora, a laboratory doctor can assess the number of leukocytes, as well as the ratio between normal, opportunistic and pathogenic flora. This is a rather subjective method of assessing vaginal health, but it allows you to quickly decide on further tactics.
What does hyperconcentration of epithelium in a smear indicate?
A high level of squamous epithelium indicates mainly inflammatory processes in the genital organs. They can be located in the vagina/uterus (vaginitis) or in the urethra (urethritis).
Such inflammations have a different nature and can be caused by parasitic, fungal, and bacterial infections. Menopause can also be a cause, since during it the concentration of hormones drops significantly, or intoxication with chemicals.
If a woman has vaginitis, she will experience the following symptoms:
- redness of the surface of the vulva;
- strong and foul-smelling vaginal discharge;
- pain and itching in the vagina.
Urethritis is most often caused by gonococci, herpes, chlamydia and cytomegalovirus. Women of childbearing age and young men are most prone to pathology. Also at risk are those who have a large number of sexual partners and have sex without a condom.
In women, urethritis is usually accompanied by the following symptoms:
- pain in the genitals;
- chills and fever;
- frequent urge to urinate;
- copious discharge;
- burning when urinating.
If there is a lot of squamous epithelium in the smear, the concentration of leukocytes and mucus of key cells is carefully examined. Columnar epithelium usually grows due to cancer processes in the genital organs. If the doctor suspects cancer, the woman is sent for a series of additional tests.
In some cases, it happens that the concentration of epithelium in the vaginal microflora increases due to normal physiological conditions. An example of these are those in which the processes of renewal of the epithelial layer are stimulated.
This phenomenon always occurs during menstruation. If you find a lot of epithelium in the smear, do not start to panic and wait for the final test results. Most likely you are fine, you just did not prepare for the study correctly.
[ads-pc-2]
Opportunistic flora
In gynecology, opportunistic microbes are those microbes in a flora smear that may not cause any diseases until they begin to multiply excessively. The main types of such microbes:
- cocci;
- ureaplasma;
- diphtheroids;
- Candida mushrooms.
The bacteria in the smear, which represent opportunistic flora, with some exceptions, are aerobic flora, that is, they require access to oxygen to live. Anaerobes - Leptothrix and Klebsiella.
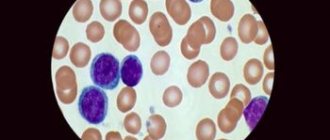
Cocci
Cocci are round shaped bacteria.
According to the staining method, there are gram-positive and gram-negative.
Gram-positive cocci (staphylococci, streptococci and enterococci) are opportunistic, their presence is considered normal within the following limits:
- staphylococci – up to 104;
- streptococci – up to 105;
- enterococci – up to 105.
Gram-negative cocci are causative agents of dangerous diseases. These include gonococci, the causative agents of gonorrhea.
Ureaplasma
These are very small bacteria that, when multiplied above 104 units, cause inflammatory diseases. They prevent conception.
Leptothrix
This is a representative of the anaerobic UP flora, a gram-positive rod-shaped microorganism. Leptothrix itself in a flora smear is dangerous only during pregnancy and can cause a miscarriage.
In non-pregnant patients, the discovery of leptothrix is not a cause for concern.
It is necessary to additionally retake the test, since leptothrix often accompanies other infectious diseases, for example, chlamydia or trichomoniasis.
Diphtheroids
As representatives of the UP flora, they can be present in a smear in small quantities. When their level is exceeded, vaginosis begins . Diphtheroids are similar to the bacteria that cause diphtheria, Corynebacterium.
If corynobacteria were found in the flora smear, their quantity is determined. In case of moderate amounts, a course of drug treatment is prescribed.
If corynebacteria are more than a certain threshold, then additional research needs to be carried out for the presence of other infections, since these bacteria are often associated with others.
Klebsiella
A representative of the flora, Klebsiella under certain conditions (with decreased immunity, pregnancy) can cause urinary tract diseases .
Candida mushrooms (soor)
What does a positive soor in a flora smear give? If fungi of the genus Candida are isolated from a smear, this indicates candidiasis.
These fungi are also representatives of the UP flora; they are introduced into the vagina from the outside. Candidiasis is caused by decreased immunity.
With candidiasis, a smear on the flora can be found:
- filaments of pseudomycelium (mycelium). Pseudomycelium is represented by filamentous growths of blastospores with constrictions.
- blastospores (spores). If blastospores are detected in the analysis of a vaginal smear for flora, it means that the woman’s body is affected by candidiasis.
The number of blastospores depends on the extent and stage of the disease. Blastospores are embryonic cell forms formed by budding from maternal cell forms.If blastospores are found in a flora smear, the female body must be examined for yeast spores.
In addition to identifying candidiasis, such an analysis will determine which antifungal drug should be used if the diagnosis is confirmed.
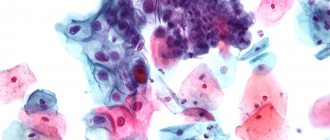
Key (atypical) cells
The key cells in a smear for flora are epithelial cells on the surface of which microorganisms have collected (this is especially typical for gardnerella in women, which causes bacterial vaginosis). The presence of atypical cells in a smear is a sign of an infectious disease .
Organization of treatment
It completely depends on what caused the appearance of a large amount of epithelium in the smear. If the problem is inflammatory processes (vaginitis and urethritis), then treatment most often consists of taking antibiotics and using immunomodulators and medications to restore the microflora after treatment.
If cancerous processes are detected, a slightly different treatment is prescribed. A biopsy is performed to understand whether the process is malignant or benign.
If there is a need to remove the tumor, it is cut out. When such a pathology is detected in the early stages, it is cured while maintaining all functions of the reproductive system.
Hyperkeratosis of squamous epithelium
Recently, women are increasingly being diagnosed with squamous epithelial hyperkeratosis. This means that the cells of the surface layer undergo exfoliation and keratinization too actively. As a rule, this disease occurs in women after 40 years of age, during menopause. But in recent years, hyperkeratosis (or leukoplakia) has also appeared in young girls. This suggests that the patient's body produces too much progesterone, and this may be the cause of infertility. The main danger of hyperkeratosis of squamous epithelium is that it creates a pathological environment in tissues that is favorable for the development of cancer tumors in the cervix.
Among the causes of leukoplakia are the following:
- disorders in the endocrine system – hormonal imbalance;
- problems in the immune system (frequent colds, sore throats);
- chronic form of human papilloma or chlamydia;
- injuries (for example, piercing of the intimate area).
Hyperkeratosis has no external signs, so a woman does not know about it until she goes to the gynecologist and receives smear data for cytology. Moreover, upon examination, a specialist can already speak with 80% confidence about hyperkeratosis if he finds small white spots-plaques on the ectocervix. To confirm the diagnosis, a cytological analysis and colposcopy (examination of the patient with a colposcope - an illuminated binocular) are prescribed.
Treatment of hyperkeratosis is determined by the patient’s age and reproductive function. In some situations, surgical intervention is possible, in others, surgery is a last resort, as it creates scars on the uterus, causing complications during childbirth. In addition, the following applies:
- cryodisruption (cauterization of hyperkeratosis foci with liquid nitrogen);
- radiosurgical therapy;
- laser vaporization (exposure to leukoplakia plaques with a laser beam to avoid scarring)
In the complex treatment of hyperkeratosis, hormonal and antibacterial therapy is used. In this way, it is possible to prevent the transition of leukoplakia to the oncological stage.