Diffuse changes in the liver are not considered a separate disease; their presence may indicate the proliferation of the organ parenchyma, which is characteristic of many pathological conditions. The changes are of a different nature; in all cases, a detailed examination is used to confirm the diagnosis.
What is liver parenchyma? Parenchyma is active epithelial cells that perform the functions of ensuring optimal blood composition and normal outflow of bile. The structural elements of the liver parenchyma are covered on the outside with capsules of fibrous connective tissue.
Depending on the severity, diffuse changes in the liver parenchyma can be:
- Insignificant. Diagnosed quite often. Characteristic of the early stages of a viral or bacterial inflammatory process and pathological conditions caused by exposure to adverse factors.
- Expressed. Accompanied by swelling and enlargement of the organ. Characteristic of chronic hepatitis, cirrhosis, diabetes mellitus, severe obesity, primary and secondary malignant tumors.
- Moderate. Moderate diffusions develop against the background of intoxication of the body with drugs, prolonged consumption of alcoholic beverages and fatty foods.
Based on the nature of changes in the structure of the liver, the following are distinguished:
- Diffuse changes like steatosis. Characterized by the appearance of scattered fatty inclusions. The accumulation of large amounts of fat contributes to the destruction of healthy liver cells, followed by the formation of cysts that change the structure of the organ. Diffuse focal changes in the liver, such as steatosis, can be found in both elderly people and children.
- Changes in the type of hepatosis. Healthy liver tissues have a homogeneous structure; they contain blood vessels and bile ducts. Hepatosis is characterized by the accumulation of excess fat inside the cells of the organ. Healthy hepatocytes are gradually destroyed.
- Fatty infiltration. The liver is actively involved in nutrient metabolism. Fats from food are broken down by enzymes in the intestines. In the liver, the resulting substances are converted into cholesterol, triglycerides and other compounds important for the human body. The development of diffuse changes like fatty infiltration leads to the accumulation of large amounts of triglycerides in the tissues.
Depending on the reasons that contributed to the change in the structure of the organ, it can be swelling, sclerotic, hypertrophic and dystophic.
What are diffuse liver changes and how to avoid them?
The sequential interaction between atoms or molecules of two substances with the acquisition of some properties and qualities of others, in which the concentration of molecules in the entire volume of contacting substances is equalized, is called diffusion.
Under the influence of many negative factors, the natural reaction is disrupted, both in the surrounding world and in the human body, provoking an imbalance in physical balance and the development of diffuse changes. The organs of the digestive and excretory systems are especially at risk of diffuse changes:
- Stomach;
- Liver;
- Pancreas;
- Spleen;
- Intestines;
- Kidneys.
Diffuse changes in the liver can be either quite minor or quite serious pathologies.
Diffuse changes in the liver do not have clear age boundaries; this phenomenon can affect both newborns and the elderly. In children, this phenomenon is called a congenital pathology of the organ, and in an elderly person it develops subsequently from hepatitis or severe poisoning.
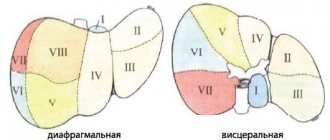
Diffuse changes in the liver affect its parenchyma, the size and structure of the organ, affecting the reduction of the lumen of arteries and veins, the functioning of the gallbladder and bile ducts.
What is liver parenchyma? Liver parenchyma is usually called the tissue from which the organ itself consists.
Reasons for changes
The causes of diffuse changes in the liver are usually called:
- irrational and irregular nutrition;
- passion for losing weight with fasting and dietary supplements;
- regular consumption of alcoholic beverages;
- smoking;
- intoxication, subsequently long-term treatment with medications;
- infections;
- hepatitis;
- parasites in the organ channels;
- formation of gallstones.
Symptoms
In the case when the changes occur at a sluggish stage, no external symptoms of organ disease are observed.
In the acute stage, the following signs of diffuse changes in the liver are noted:
- pain, heaviness in the right side, under the ribs;
- colic;
- increased body temperature;
- jaundice;
- feeling of bitterness in the mouth;
- a noticeable bulge on the skin of the right hypochondrium;
- digestive disorders;
- emotional instability, tearfulness, aggression.
What will the ultrasound indicate?
Ultrasound will indicate diffuse changes in the structure of the liver and organ cells, as well as violations of their functions.
The cells enlarge, become dense and heterogeneous. Liver tissue undergoes degeneration; scars, nodules, accumulations of fat, hemorrhages, or areas of parasite habitation may be observed.
The doctor will point out areas with different echogenicity: low, high or high. This will indicate development:
- hepatitis A;
- amyloidosis;
- fatty or alcoholic hepatosis;
- oncology;
- helminth infections.
For example, the sound passage and echogenicity indicated by the doctor indicate disturbances in the liver tissue; increased echogenicity of the bile ducts with diffuse changes in the liver indicates cholelithiasis, cholangitis or cholecystitis. Reduced echogenicity indicates hepatitis.
If an ultrasound examination is not enough, the doctor may recommend an MRI or computed tomography scan, where the tissue can be examined step by step.
Minor diffuse changes in the liver are treated with:
- hepatoprotectors (for example, Essentiale);
- diets No. 5;
- If there are no contraindications, tubage can be performed.
Essentiale
One honey-like hard gelatin capsule contains 300 mg of essential phospholipids derived from soy.
These phospholipids are similar to endogenous phospholipids, but are more functional due to their high levels of polyunsaturated fatty acids. They have the main property: to integrate into the cell membranes of damaged liver cells and help the process of their regeneration.
But, in the current situation, the doctor has the right to set the dosage and course of treatment depending on individual characteristics and the course of the change procedure.
Diet No. 5
Dietary nutrition for diffuse changes in the liver and its diseases involves avoiding:
- fried;
- muffins;
- animal fats (fatty meat, lard);
- sausages;
- canned food;
- marinades;
- mushrooms;
- legumes;
- radish, radish, garlic, horseradish, green onions and sorrel;
- sour fruits and berries;
- fat-saturated dairy and fermented milk products;
- alcoholic and carbonated drinks;
- coffee, cocoa, strong black tea;
- semi-finished products and fast food products.
It is important to switch to a safe protein diet, limiting vegetable fats and excluding animal fats, as well as strict dosing of salt and sugar. In case of organ disease, the emphasis is on porridge, stewed, boiled vegetables, soups, low-fat meat and dairy dishes.
Moderate diffuse changes in the liver are treated a little differently:
- hepatoprotectors;
- diet No. 5;
- antibiotics;
- antihistamines;
- with the addition of a vitamin-mineral complex.
Antibiotics
In cases where the treatment of a disease cannot be done without antibiotic therapy, fluoroquinolones are often prescribed. Their action is particularly marked by a gentle attitude towards the cells of the organ. In particular, Ciprofloxacin (Tsiprolet A, Tsifran, Tsifomed) is especially popular.
The effectiveness of Ciprofloxacin is observed due to the effect of the antibiotic on DNA synthesis in the structure of the bacterium.
The usual daily dose of Ciprofloxacin-containing drugs is 2 tablets, which are recommended to be taken twice a day, at 12-hour intervals one hour before meals or 2 hours after meals.
Diffuse changes in the liver parenchyma of viral origin are treated with:
- antiviral therapy;
- hormonal agents;
- vitamin-mineral complex;
- and good nutrition as part of diet No. 5.
Diffuse changes in the liver and pancreas caused by bacteria are treated mainly with antibiotics, in particular aminoglycosides.
Aminoglycosides are one of the first antibiotics; they act by disrupting the bacterial chain of protein synthesis by ribosomes. Recently, Amikacin injection has become popular in the treatment of liver diseases.
The injection is placed into the muscle tissue.
Also, to protect and restore the organ, a hepatoprotector, a vitamin complex and dietary nutrition are added to the treatment.
In the presence of parasites, diffuse changes in the organ require treatment with anthelmintics, drugs to relieve symptoms of intoxication, hepatoprotectors, and diet.
Anthelmintic
Chloxyl is often prescribed for the treatment of liver parasites. Take it for 2, 3 or 5 days as recommended by the doctor.
An hour later, after breakfast with a glass of tea and 100 grams of bread, you need to take an anthelmintic solution of powder in half a glass of milk. An adult should take 6-10 grams of the active substance per day.
After completing the Chloxyl course, you need to start taking choleretic drugs and undergo duodenal intubation.
In this case, initially, it is customary to treat the disease that is the root cause of the condition, namely, to eliminate the stones. Next, the doctor will recommend adhering to a strict diet No. 5, taking choleretic drugs and hepatoprotectors.
There are many drugs that increase bile flow, some of the most frequently prescribed are Allochol and Chophytol.
Chophytol is a dark, rich brown solution with a possible yellow precipitate. As a rule, before taking it directly, it is diluted with water; adults should drink a teaspoon of Hofitol before meals, three times a day.
(Is the article useful?)Loading...
This organ is made up of tissue called parenchyma. It is formed mainly from liver cells - hepatocytes, which renew old or dead areas of tissue. The liver is completely regenerated in about a year and a half. If diffuse (that is, affecting the entire organ) changes are detected in it, then more often this means an increase in parenchymal tissue, less often - its decrease. Such violations can be either minor or large-scale.
Even a banal flu does not go away completely for the liver, but it, as a rule, gets off with minimal changes in the parenchyma. Another thing is severe diffuse lesions after hepatitis of any kind, chronic alcohol poisoning or giardiasis. If scar (fibrous) tissue begins to grow in an organ, it will significantly increase in volume and undergo irreversible structural changes.
The liver does not complain for a long time about the difficult conditions of its existence. Organ misfortunes are discovered only by chance during an ultrasound due to completely different patient complaints. Often there is an enlargement of the liver - hepatomegaly, as a result of which the structure of the organ begins to degrade. The density of the parenchyma becomes increased, and its echogenicity is many times higher than normal, that is, ultrasound is reflected from the parenchyma at a much higher speed.
With diffuse changes, the enlarged organ is easily detected by palpation, and this diagnostic procedure causes pain to the patient. If such changes do not occur in an acute form, a person may not experience it. But as the pathology progresses, the symptoms of hepatomegaly become more obvious. Appears:
- heartburn;
- halitosis;
- nausea;
- yellow tint, itchy skin;
- ascites (fluid in the abdominal cavity).
Excessive consumption of alcohol and fatty foods causes hardening of the liver parenchyma. Viral infections and parasites also entail partial, diffuse-focal changes in it. However, they can trigger the development of tumors. With hepatitis, echographic signs of diffuse changes in the liver are often weakly expressed, although the organ is already significantly enlarged.
Liver damage in children
Pathological disorders of the liver parenchyma are not uncommon in children of different ages.
The main causes of diffuse changes in the parenchyma in children are:
- Pathologies of the heart muscle, defects;
- Immature digestive system in infants;
- Damage to the body by parasitic infections;
- Long-term use of medications;
- Bile outflow disorders;
- Neoplasms.
Diffuse changes in the liver parenchyma in children of any age are diagnosed, as in adults, through ultrasound examination and laboratory tests. Treatment will directly depend on the factor and cause that provoked the disturbances and changes in the parenchyma.
Types of changes
Various types of changes can occur in liver tissue: in density, shape and composition.
Pathological deviations are divided into certain types:
- Diffuse. Occur throughout the parenchyma;
- Local. Part of the parenchyma is damaged;
- Focal. There is a compaction or one small lesion.
Focal type
Focal lesions can be multiple, merging or single. Focal changes are diagnosed by echography. The degree of echo-reflection classifies focal lesions as those without echostructure and those with echostructure (weak, strong or mixed). As the pathology worsens, the echogenicity of the lesion may change.
Using echography, it is possible to determine the development of areas of calcification (seals) in the parenchyma. They occur less frequently in children than in adults.
The appearance of focal lesions of the parenchyma is promoted by cirrhosis, chronic hepatitis, tuberculosis, echinococcosis, and hypomotor dyskinesia of the bile ducts. Pathology also develops as a result of stagnation of bile in the liver, malaria, sepsis and parasitic infestations.
Lesions whose echostructure cannot be identified are parenchymal cysts. It is possible to detect formations using an echogram only when they reach a size of 3–5 mm in width. Formations in the form of cysts are divided into specific types, differing in the cause of formation (congenital or acquired) and methods of appearance (false and true, parasitic and non-parasitic).
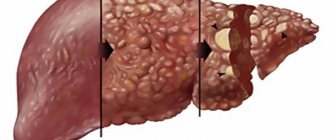
Diffuse changes are acute and chronic hepatitis, fat accumulation, cirrhosis, changes under the influence of other diseases. With hepatitis, the patient's liver size increases, but its structure does not change.
Violations of the parenchymal surface appear when the inflammatory process continues to progress. In this case, thickening of the thin wall of the liver is recorded. During the examination, weak echogenicity is determined against the background of increased sound conductivity.
In the presence of hepatitis, unexpressed inflammatory processes in the parenchyma cause a heterogeneous level of echogenicity. When cirrhosis is diagnosed, lesions with impaired echogenicity begin to grow in number as a result of the rapid destruction of a homogeneous structure. The size of the lesions varies from 0.5 cm to 2 cm.
Heterogeneity of the parenchyma can be caused by stagnation in the bile ducts, fatty degeneration of the parenchyma, and impaired metabolism.
Reasons for changing the structure
A hardening of the liver may be a sign of organ damage. Pathology can be located both inside the organ and outside its borders.
The most common reasons include:
- alcoholism;
- long-term therapy with antibiotics and other strong medications;
- poor nutrition;
- cirrhosis;
- neoplasms;
- sclerosing type cholangitis;
- hepatitis of various etiologies;
- dystrophy that developed against the background of fatty infiltration;
- dysfunction of the digestive system, which developed against the background of problems with the pancreas;
- chronic form of infectious lesions of other body systems;
- congenital and acquired metabolic abnormalities;
- extrahepatic diseases (diabetes mellitus, etc.).
Lumps clearly visible on an ultrasound image may indicate oncological formations. Diffuse changes in the structure can also be caused by prolonged abuse of fried and fatty foods, as well as working in harmful conditions.
Attention! The higher the echogenicity of the liver during ultrasound, the larger the diffuse damage to the organ and the denser its parenchyma.
With cirrhosis, different areas of the liver exhibit different echogenicity. Also, this disease is characterized by a heterogeneous structure, changes in the normal parameters of the organ and portal vein.
Hepatitis
With hepatitis, there is an increase in echogenicity, an increase in liver volume, growth of fibrous tissue and compaction of the periportal tracts. This pathology affects the entire organ, so the ultrasound image reveals diffuse tissue damage.
The type of hepatitis cannot be determined from the picture. But still, from this study it is possible to identify the form of the disease.
During the acute stage the following are observed:
- seals;
- increase in organ volume;
- the vascular pattern is enhanced;
- heterogeneous structure;
- dilated bile ducts;
- foci of inflammation.
Neoplasms
A common cause of dense parenchyma on an ultrasound image is benign or malignant neoplasms.
Benign tumors grow slowly and do not metastasize. But at the same time, observation by a doctor is required, who will monitor the growth of education and the effectiveness of therapy if it is necessary to prescribe it.
On ultrasound, a benign tumor appears as a dense area with clear edges. Sometimes lesions with blood or fluid are also detected.
Malignant neoplasms in the liver can be metastases that appear as a result of oncology of other internal organs. On ultrasound they appear as numerous areas of compaction. When they are identified, additional examinations and tests are prescribed to help establish an accurate diagnosis.
Other causes of liver lumps
Round capsules with liquid contents detected on ultrasound may indicate the presence of a cyst, abscess or parasitic liver disease. To clarify, additional diagnostic measures are carried out.
Stagnation in the intrahepatic bile ducts can also cause disruption of the structure of the organ. Clinical tests are performed to confirm bile stagnation. An increase in bilirubin levels is strong evidence of the development of this process.
Diet to cleanse the liver
| Exclude | Allowed |
|
|
Meals should consist of small portions 5 to 6 times a day. Food should be steamed, baked or boiled. Meat is used for soups, fish - for aspic. You can eat a little vinaigrette, sauerkraut or squash caviar. Instead of sugar, xylitol is used. The daily dose of salt should not exceed three grams.
Treatment of diffuse changes in the pancreas
The specialist cannot prescribe therapy to combat this pathology. Surgical intervention is also irrelevant. With the help of medications, you can only alleviate the symptoms of the disease, as well as help this organ perform its direct functions. For this, painkillers and enzymes are most often prescribed. Enzymes compensate for the deficiency of necessary substances in the body for the normal functioning of the pancreas, and painkillers help relieve pain.
Diet
An important place in the treatment of liver parenchyma is played by a special nutritional system, according to which fried and fatty foods must be completely excluded from the diet. Products containing fiber and potassium are healthy and recommended.
The use of alcoholic beverages and soda is strictly prohibited.
It is recommended to include dietary meats, low-fat dairy products, pureed soups and cereals, sours and homemade jelly in the diet. Decoctions of medicinal herbs that can replace coffee and black tea are useful. Bread should be used stale, soups and cereals can be seasoned with vegetable oil, butter should be used in limited quantities. You should also limit the amount of salt and sugar you use.
You need to take food in small portions, at the same time. You need to have dinner three hours before bedtime.
Cleansing the liver requires a special diet; at the initial stage of congestion in the bile ducts, it is enough to adhere to a diet to ensure that the detoxification process is successful without additional aggressive influences.
In addition, a diet for cleansing the liver is also a preventive method that prevents the appearance of new stones after a planned cleanse.
Unloading the liver lasts at least a week, but it is better to create a two-week menu so that the toxins are completely eliminated.
During cleansing you should avoid the following products:
- Products containing pure carbohydrates - sugar, refined grains (polished rice, oatmeal, etc.).
- Pasteurized, canned products containing dyes, stabilizers, food flavors, hydrogenated oils, fats.
- Sea fish and seafood are not allowed due to the possible content of mercury elements in them.
- All types of sausages and ready-made store-bought pates are not allowed.
- Alcohol is strictly prohibited.
A liver cleansing diet should include the following ingredients:
- Each meal should be accompanied by at least one fresh fruit or vegetable. For example, oatmeal made from whole grain oats plus an apple.
- Porridge should be cooked in water from unrefined grains - brown rice, oats, buckwheat.
- The menu includes legumes - beans, lentils, river fish, nuts.
- Meat should be limited and use the white part of chicken, lean beef, rabbit meat, and turkey. Meat dishes are steamed or baked without adding oil or fat.
- You should eat boiled or raw grated beets (as a salad component) every day.
- Every day there should be vegetable oil on the menu - in porridges, in salads.
- You should limit the consumption of whole milk and potatoes, it is good to eat 100 grams of natural yogurt, cottage cheese, and drink a glass of low-fat kefir every day.
- The serving size should not exceed 150 grams, food should be taken in fractions - 5-6 times a day.
- An excellent way to unload the liver is the long-known, time-tested diet No. 5 according to Pevzner.
- Every day you need to drink at least 1.5 liters of sour juice, still mineral water, grapefruit juice.
A diet for cleansing the liver is not always an effective method; in case of chronic congestion, severe slagging, it will not be possible to do without laxatives or hepatoprotectors.
Therapy for diffuse changes in the liver area
Therapeutic measures aimed at combating diffuse transformations will depend on which disease is the cause of the development of this pathology. For less pronounced changes, the patient is prescribed medications that help restore organ cells. The most effective drugs are Gepabene and Essentiale.
With moderate diffusion, antibacterial agents, vitamin complexes, and antihistamines are prescribed.
If liver disease occurs due to viral exposure, then it is best to use antiviral medications. In severe cases of the disease, various hormonal medications are prescribed. And if the liver tissue has been damaged due to helminthic infestation, then antiparasitic drugs, vitamin complexes and hepatoprotectors will have to be used.
Surgical intervention is required only in cases where significant restructuring and stone formation occurs in the parenchymal tissues.
In some cases, when the size of the stones formed is small, therapy may be limited to taking choleretic drugs.
Diffuse liver changes: types and possible causes
Diffusion is a process of interaction between molecules and atoms of substances, the purpose of which is to achieve a certain concentration in a given area. If the balance is disturbed, the functional functioning of the internal organs is disrupted.
Diffuse changes in the liver are not a separate disease, but its consequence, manifested in the form of a significant increase in the parenchyma of the organ in question.
As mentioned above, diffuse changes in the liver are not a pathology, but one of its manifestations. There is no such disease in ICD-10, but there are a number of other diseases associated specifically with the liver and that can have a direct effect on the parenchyma.
Negative external influences lead to disruption of the connection between individual molecules. At the same time, changes also occur in the functioning of hepatocytes, which leads to the growth of connective and fatty layers.
Clinical manifestations
Diffuse changes in the parenchyma themselves are part of the clinical picture; they accompany any disease of the liver and pancreas. Accordingly, the signs of diffuse changes completely depend on the causes that caused the pathological condition and the severity of the disease.
It is worth noting that hepatitis and some other liver diseases can occur with a mild clinical picture, sometimes there are no characteristic signs at all. In such situations, diffuse changes are diagnosed as a result of a routine examination, or during the diagnosis of pathologies affecting neighboring organs.
Subclinical types of liver pathologies are often expressed by malaise, lethargy, general weakness, and lack of appetite. But all these symptoms are often mistaken for ordinary fatigue.
With the development of liver and pancreatic diseases, clinical manifestations become more obvious; they can be expressed as follows:
- white feces;
- yellowness of the sclera and skin;
- pain in the area of the right hypochondrium;
- dark color of urine;
- itching on the skin (in particular the intimate area).
Yellowness of the sclera and skin indicates the severity of pathological changes in the liver.
If a patient develops pancreatitis, they will feel nauseated, sometimes causing vomiting. In severe cases of pancreatic damage, severe tachycardia may be observed.
As the underlying disease progresses, signs of digestive disorders, intoxication of the body, and failure of insulin synthesis appear, which provokes the development of diabetes mellitus.
Medicines for the liver after antibiotics
Antibiotics are used to eliminate many diseases. Their long-term use negatively affects the health of all organs and systems. Medicines for the liver after antibiotics restore the filter, since it is the filter that removes the breakdown products of medications, toxins and other harmful substances from the body.
To restore the organ, special means are used - herbal remedies, that is, hepatoprotectors. The most popular medications:
- Medicines with herbal ingredients and milk thistle - Karsil, Liv 52, Galstena, Gepabene, Ovesol. Stabilize cell membranes and have an antioxidant effect.
- Essential phospholipids – Essentiale forte, Essliver, Phosphogliv. Accelerate regeneration processes and have an antifibrotic effect.
- Products with ursodeoxycholic acid - Ursolfak, Ursosan. Protect cell membranes, eliminate inflammation and accelerate the excretion of bile.
Folk remedies are excellent for treatment after antibiotics. But do not forget that such methods are auxiliary therapy, that is, an addition to the main treatment.
- Take milk thistle, corn silk and chicory in equal proportions, pour 200 ml of boiling water over them. The decoction should steep for 10-12 hours, after which it should be strained and taken before meals.
- Pour 2 cups of boiling water over the chicory flowers and simmer over low heat for 20-30 minutes. Strain the medicine, add a couple of slices of lemon and a spoonful of honey, drink as tea.
- Finely chop 1 kg of cabbage, add currants or lingonberries, kiwi and orange to it. Mix the salad well and prepare a dressing of lemon juice, olive oil, spices and apple cider vinegar. Eat the salad throughout the week with a piece of black bread.
Diagnostic methods
Diffuse changes occurring in the tissues of the pancreas and liver are detected using ultrasound examination. An ultrasound shows exactly how much a particular organ has enlarged. Echo signs of diffuse changes are considered to be pathological plexus of vessels and compaction of parenchymal structures. Such foci of compaction are usually found throughout the organ.
But ultrasound results are sometimes not enough to diagnose a particular disease that is associated with diffuse changes. To do this, it is necessary to additionally conduct instrumental examination. For this purpose, survey radiography and computed tomography are organized.
Treatment methods
Diffuse changes in the parenchyma are a process that destroys the pancreas or liver and entails serious pathologies.
However, timely detection of the disease and proper treatment guarantee a positive outcome in most cases. Therefore, when you hear an incomprehensible name of the disease, there is no need to be scared. Understanding the essence of pathology is not difficult. And having understood the issue, it is easy to prevent its development.
In fact, structural transformation of tissue is not a diagnosis. This is a kind of syndrome from which this or that pathology begins.
If the course of events is unfavorable, they develop into an illness of the internal organ. Thus, DI in the liver can result in hepatitis, and in the pancreas – pancreatitis.
In modern medicine, DI of the liver or pancreas parenchyma corresponds to the name - hepatomegaly.
These cellular transformations are usually detected by ultrasound. The changed tissue becomes heterogeneous and changes echogenicity:
- a healthy organ is weakly echogenic;
- with the appearance of pathology and its development, the ultrasound examination rate also increases.
But to confirm the suspicion, echographic signs alone are not enough. Biochemical blood and urine tests are also needed.
Internal organs can be hollow or parenchymatous. Hollow include, for example, the stomach or intestines, which have a certain cavity inside. And parenchymal organs, such as the liver or pancreas, resemble a homogeneous sponge.
Parenchyma is the main component of the pancreas in structural terms. It is the material from which the glandular layers of tissue in this digestive organ are built. Vessels and blood capillaries make their way through it. They nourish tissues with oxygen and chemical elements. And the enzymes produced in the glandular tissue are excreted into the main pancreatic duct.
When parenchyma cells die and are replaced, the normal functioning of the pancreas is disrupted. And, as a result, disruptions occur in the production of pancreatic juice, which is so necessary for the breakdown of fats, proteins and carbohydrates.
Reasons for the appearance of parenchymal disease. The following physiological factors can trigger the onset of the syndrome:
- metabolic disorders;
- insufficient saturation of the organ with blood;
- problems with the bile ducts;
- age-related cell degradation.
Transformation of the parenchymal tissue of the parenchyma can begin against the background of other chronic problems:
- heart failure;
- pathologies of the thyroid gland;
- cholelithiasis;
- inflammation of the spleen.
Systematic poisoning of the body with alcohol, nicotine, industrial pesticides, and medications has a great influence on the biochemical composition of parenchyma cells.
Another common cause of hepatomegaly is an unhealthy diet - a preference for fatty and spicy foods containing many harmful additives and preservatives.
DI is found extremely rarely in children. A child may receive the syndrome as a congenital or genetic trait. In most cases, pathology is a consequence of the natural aging of the body or the result of a negligent attitude towards health.
This is not a diagnosis, but disturbances in the structure of the liver, which indicate hidden pathological processes. Medicine does not consider such changes to be a disease, but they must be treated so as not to bring the organ to a state incompatible with life.
This organ is made up of tissue called parenchyma. It is formed mainly from liver cells - hepatocytes, which renew old or dead areas of tissue.
The liver is completely regenerated in about a year and a half. If diffuse (that is, affecting the entire organ) changes are detected in it, then more often this means an increase in parenchymal tissue, less often - its decrease.
Such violations can be either minor or large-scale.
The liver does not complain for a long time about the difficult conditions of its existence. Organ misfortunes are discovered only by chance during an ultrasound due to completely different patient complaints.
Often there is an enlargement of the liver - hepatomegaly, as a result of which the structure of the organ begins to degrade.
Excessive consumption of alcohol and fatty foods causes hardening of the liver parenchyma. Viral infections and parasites also entail partial, diffuse-focal changes in it. However, they can trigger the development of tumors.
With hepatitis, echographic signs of diffuse changes in the liver are often weakly expressed, although the organ is already significantly enlarged. Further more. With cirrhosis, total diffuse changes in liver tissue occur.
There are masses of heterogeneous areas, and the echogenicity of the liver parenchyma is increased to the maximum.
Moderate
Signs of minor liver degradation are common. If they appeared in it, then they are also present in the pancreas.
An ultrasound diagnostician determines the presence of moderate diffuse lesions in the liver by increased tissue density, heterogeneity of its structure, and distortion of the pattern of blood vessels.
Parenchyma compaction and other echo signs of pathology can manifest themselves through a feeling of discomfort after a fatty meal, a bitter taste in the mouth, headaches, fatigue, and irritability.
The liver reacts to metabolic disorders and intoxication of the body in a very unique way: its cells accumulate fat. Over time, steatosis or fatty infiltration develops, simply - obesity of the organ.
The disease is insidious in that it has no symptoms and is often detected by chance during an ultrasound examination of the abdominal cavity. Sometimes a person feels nauseous, weak, tired, and drowsy. Then inhibition may appear in his movements, and monotony in his speech.
Even later, a person is overtaken by jaundice, ascites, dizziness, and convulsions.
Functional immaturity of the stomach and intestines in children, the toxic effects of worms often lead to the development of reactive hepatitis, that is, caused not by liver pathologies.
This disease either has no symptoms or manifests itself as mild malaise, digestive disorders, low-grade fever, or emotional decline.
With adequate treatment of diffuse abnormalities, liver activity can be restored completely.
If in the early stages of diffuse-focal degeneration the organ increases in volume, then at a later stage it decreases and shrinks. Its echostructure is diffusely heterogeneous, and its echogenicity is very high.
The patient is persistently haunted by pain in the right hypochondrium and right shoulder; his tongue, sclera and skin under his eyes are jaundiced.
The main treatment for diffuse lesions in the liver consists primarily of eliminating their causes: obesity, alcohol abuse, taking medications that are toxic to this organ, etc. Amino acids, vitamins E and group B improve the condition of the organ. To ensure that liver cells are restored, hepatologists (or therapists) prescribe medications:
- Essentiale forte N;
- Phosphogliv;
- FanDetox;
- Heptral;
- Result Pro;
- Gepabene.
According to indications, courses of treatment with antibiotics, antiviral, anthelmintic and choleretic drugs are carried out. Surgical treatment methods are used when it is necessary to remove stones and tumors in the liver.
Patients are prescribed dietary table No. 5 with a ban on fatty, spicy and smoked foods. Salty, sweet, sour foods, alcohol and soda are also prohibited.
Priority is given to lean varieties of meat and boiled fish, dairy dishes and soups, cereals and vegetables.
Only the attending physician will be able to determine competent and qualified treatment. Only he will be able to competently assess the degree of the degenerative process, as well as prescribe the necessary medications.
Self-medicating or taking traditional medicine methods is extremely dangerous for your health. It is best to take a comprehensive approach to the treatment process; this is the only way to get the maximum effect from therapy. The standard treatment regimen for diffuse liver changes is as follows:
- In case of viral infection of the liver, the patient is prescribed antiviral drugs. With their help, it is possible to suppress the activity of pathogenic microorganisms and reduce their toxic effects on the body. In addition, etitotropic therapy is prescribed - it is necessary to influence a specific human hepatitis virus. It is worth completely giving up smoking and smoking, as it has a powerful negative effect on the human body. To protect the remaining liver cells from destruction, the patient is prescribed hepaprotectors. These medications contain a large amount of vitamins and amino acids.
- Phospholipids are medicinal components that restore the normal structure of liver cells. In addition, they protect the organ from necrosis. This contributes to a significant improvement in the functioning of the entire gastrointestinal tract and prevents the development of complications.
- Herbal preparations - with their help it is possible to make the liver tissue work. Damaged structures are quickly restored, in addition, a powerful choleretic effect is exerted. This helps improve the digestion process and accelerates the removal of harmful waste and toxins from the body.
- For malignant neoplasms in the body, the patient is prescribed synthetic drugs.
- To restore liver function and get rid of the deficiency of useful elements, the patient is prescribed amino acids.
- Thanks to vitamin complexes, you will be able to increase the protective abilities of the entire body.
Taking medications alone to treat diffuse changes in the liver parenchyma is not enough. You should adhere to the principles of a healthy diet and also prevent exposure to toxic substances in your body. First of all, doctors pay attention to a person’s diet: any harmful foods that put a serious burden on the liver should be excluded.
Treatment
The type of therapy depends on the pathology that caused the development of the organ structure disorder. Individual treatment is prescribed for each patient. Most often, patients are prescribed hepatoprotectors and immunomodulators.
Also an important component of any therapy is a diet that involves avoiding fatty foods. In addition, you should give up alcohol and cigarettes.
Prevention
Regular preventative measures are recommended to maintain overall health. Cleansing the body and strengthening the immune system is beneficial for the liver. You should also adhere to a healthy lifestyle and proper nutrition (do not overeat, eat more vegetables and fruits).
Timely detection of the disease increases the chances of cure. This is why it is recommended to undergo an ultrasound every year, especially for people over 50 years of age. The liver is capable of self-healing, so identifying the disease at an early stage and promptly starting therapy increases the chances of a favorable outcome.
Related publications:
- Why does my liver hurt? Causes and treatment of liver pain
- How is liver palpation performed? Rules of procedure and interpretation of results
- How is an MRI of the liver done and what does it check? Can I eat before the procedure?
- Diagnosis of hepatitis C using RNA PCR - quantitative and qualitative analysis, interpretation
Method of administration and dosage of medications for the liver
In order for the treatment to be quick and effective, the doctor prescribes the patient the method of use and dosage of medications. For the liver, drugs of different release forms are used, so the therapeutic effect depends on the method of their use.
- Herbal hepatoprotectors
Gepabene is prescribed 1 tablet 2-3 times a day. If pain in the right hypochondrium appears at night, then an additional capsule is allowed before bedtime. The maximum daily dose is 6 tablets in 3 doses, duration of therapy is from 3 months.
- Essential phospholipids
The daily dose of Essentiale is 4-6 tablets in 3-4 doses, the duration of treatment is individual for each patient. The tablets are taken without chewing, washed down with water. The dosage of the solution for intravenous injection is up to two ampoules per day.
- Preparations of animal origin
Hepatosan is taken in doses of 200-400 mg, depending on the indications. The course of treatment is 10-20 days.
Ursosan is taken at a dose of 10 mg/kg body weight. The daily dosage is divided into 2-3 doses. For patients under 2 years of age, the dosage is selected individually.
- Biologically active additives
Liv 52 is taken for both therapeutic and preventive purposes. For children over 6 years old and adults, 1-3 tablets 2-3 times a day. Drops are used to prevent liver diseases, 10-20 drops 2 times a day for children over 2 years old and 80-160 drops for adults.
general information
So what is it - lumps in the liver? What does such a change in structure mean and why does it occur?
Ultrasound has been considered one of the most accurate diagnostic techniques for many years. With its help, you can identify even small changes in the structure of the parenchyma, determine pathology at an early stage of development and assess the severity of the lesion.
Liver ultrasound procedure
Ultrasound is performed using ultrasound. These waves pass through the tissue, creating visualization on the machine's monitor. Depending on how dense the liver is, the intensity of the shadows is displayed in the image. This procedure allows you to track changes in structural abnormalities and blood movement.
Attention! The study is a safe method that provides the most accurate and informative data. Its use is widespread in many areas of medicine.
Drugs affecting the nervous system
Tacrine, a drug used to treat Alzheimer's disease, causes hepatitis in almost 13% of patients. An increase in transaminase activity, usually during the first 3 months of treatment, is observed in half of the patients. Clinical manifestations are rare.
When the drug is discontinued, transaminase activity decreases; when taking it again, it usually does not exceed the norm, which suggests the possibility of adaptation of the liver to tacrine. Cases of death from the hepatotoxic effect of the drug have not been described, however, transaminase activity should be monitored during the first 3 months of treatment with tacrine.
Pemoline, a central nervous system stimulant used in children, causes acute hepatitis (probably caused by a metabolite) that can lead to death in patients.
Disulfiram, used to treat chronic alcoholism, causes acute hepatitis, sometimes fatal.
Glafenin. The liver's reaction to this analgesic develops within 2 weeks - 4 months after the start of use. Clinically, it resembles a reaction to Zinchofen. Of the 12 patients with a toxic reaction to glafenin, 5 died.
Clozapine. This drug for treating schizophrenia may cause FPN.
Liver and pancreas diseases - relationship
The pancreas is an unpaired organ of the gastrointestinal tract that does not have a cavity. There are ducts between the liver and pancreas, so disruption of the functionality of one organ leads to pathologies of the other.
If there is a history of mixed transformations in two organs, then the person is found to have metabolic disorders and vascular diseases. He often suffers from acute infections. With massive damage, symptoms appear in the form of jaundice, changes in the color of urine, feces, and skin itching.
Abnormal gland condition
In a normal state, organ tissues are characterized by a homogeneous structure. When performing an ultrasound against the background of DIP, the specialist sees blood vessels with bile ducts, and their density is significantly higher than normal values.
Mixed-type transformations in the liver are formed with hemangioma, disorders of sugar utilization in the body, cirrhosis, hepatosis, obesity, alcohol addiction, tumors, steatohepatosis, hepatitis. Provoking factors include parasitic diseases, infections and viruses, and starvation.
DIP in children
In a newborn baby, diffuse transformations of parenchymal tissues are a consequence of congenital pathologies due to infectious processes in the mother’s body during gestation. In children, mixed lesions form in the liver due to the use of antibiotics, since they are toxic and have a detrimental effect on the gland.
Folk remedies
Treatment with folk remedies, including the use of traditional decoctions and infusions of plants that have a positive effect on the liver, also gives good results. Such plants include plum juice, chicory herb decoction, and mixed herbal infusions. Eating pumpkin with honey is very beneficial. Milk thistle and agrimony root are widely used for the herbal mixture.
To prepare an infusion, a tablespoon of plants is poured into a glass of hot water and infused. Olive and pumpkin oil have shown good results as folk remedies for restoring the normal state of organs. For several weeks, it is recommended to drink a tablespoon of one of these oils in the morning on an empty stomach. But no means can give an excellent result if the diet for pancreas remains incorrect.
Prevention and prognosis
A basic component of therapy is dietary adherence. It is necessary to exclude alcohol-containing and carbonated drinks from the diet, and reduce the consumption of fried, spicy and fatty foods.
During the period of therapeutic measures, you should stop taking hepatotoxic drugs. In addition, vaccination is prohibited; it is advisable to refuse treatment of existing pathologies in the digestive system.
The diet is strict and is prescribed in accordance with the presence of intolerance to certain foods and the possible manifestation of allergic reactions in the patient to some components of the diet.
A special role is played by the normalization of bacterial flora of the large and small intestines. For this purpose, the patient is prescribed a course of antibacterial medications and enzyme agents.
The following are used as antibacterial drugs:
- Amoxicillin;
- Clarithromycin;
- Azithromycin;
- Cephalosporin.
Enzyme preparations include drugs such as Festal and Pancreatin. Bifidumbacterin and Bifiform are used as agents that normalize intestinal microflora.
To protect hepatocytes from the negative effects of various factors, Essentiale and Phosphogliv are used.
The duration of the treatment course usually varies from three weeks to one month.
To reduce increased tone, antispasmodic drugs No-shpa and Papaverine hydrochloride are prescribed.
If diabetes mellitus is the trigger for the appearance of pathology in tissues, it is recommended to strictly follow a diet and take medications whose action is aimed at normalizing glucose levels, such as drugs from the group of biguanides, glinides, and thiazolidinediones. The use of these medications helps eliminate the negative factor in the form of high blood glucose levels.
In addition, traditional medicine prepared from medicinal herbs can be used at home as additional components of therapy. The use of such medications allows you to quickly get rid of pathology and normalize work. In addition, medications prepared according to traditional recipes contribute to long-term stabilization of sugar levels, which has a positive effect on the condition and does not cause progression of the pathological process.
To normalize the condition, it is recommended to take chicory decoction, plum juice, pumpkin with honey, and various herbal infusions. A good way to normalize the condition is to take one tablespoon of pumpkin or olive oil daily before meals.
Preventive actions involve eliminating the factors leading to the disease. To keep the pancreas and liver in good condition, you need to adhere to the basic principles of health. In the first place is the refusal of alcohol-containing products - the strongest provocateur of liver diseases, as well as pancreas.
A healthy lifestyle involves:
- feasible physical activity should alternate with proper rest;
- the diet should be thoughtful and balanced in order to avoid two extremes - foods that are difficult to digest and poor diets that do not replenish the body with the necessary nutrients;
- drinking regime;
- cultivating a positive perception of even difficult situations is stress prevention.
The prognosis for treatment of diffuse changes, especially if it is taken up in the initial stages, is very favorable. Nine out of ten cases have the possibility of recovery.
Due to the high chances of recovery, when the first adverse symptoms appear, you need to undergo an examination as quickly as possible in order to establish an accurate diagnosis and begin treatment.
Yuliia Yevtiekhova
31.10.2018
14 min. for reading
My name is Yulia and I am a general practitioner. In my free time, I direct my knowledge and experience to a wider audience: I write medical articles for patients.
Ask a questionDiplomaMake an appointment
Literature
- Cherenkov, V. G. Clinical oncology: textbook. manual for the postgraduate system. education of doctors / V. G. Cherenkov. – Ed. 3rd, rev. and additional – M.: MK, 2010. – 434 p.: ill., table.
- Ilchenko A.A. Diseases of the gallbladder and biliary tract: A guide for doctors. — 2nd ed., revised. and additional - M.: Publishing House "Medical Information Agency", 2011. - 880 p.: ill.
- Tukhtaeva N. S. Biochemistry of biliary sludge: Dissertation for the degree of candidate of medical sciences / Institute of Gastroenterology of the Academy of Sciences of the Republic of Tajikistan. Dushanbe, 2005
- Litovsky, I. A. Gallstone disease, cholecystitis and some diseases associated with them (issues of pathogenesis, diagnosis, treatment) / I. A. Litovsky, A. V. Gordienko. — St. Petersburg: SpetsLit, 2020. — 358 p.
- Dietetics / Ed. A. Yu. Baranovsky - Ed. 5th - St. Petersburg: Peter, 2020. - 1104 p.: ill. — (Series “The Doctor’s Companion”)
- Podymova, S.D. Liver diseases: A guide for doctors / S.D. Podymova. — Ed. 5th, revised and additional - Moscow: Medical Information Agency LLC, 2020. - 984 p.: ill.
- Schiff, Eugene R. Introduction to Hepatology / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray; lane from English edited by V. T. Ivashkina, A. O. Bueverova, M.V. Mayevskaya. – M.: GEOTAR-Media, 2011. – 704 p. – (Series “Liver diseases according to Schiff”).
- Radchenko, V.G. Fundamentals of clinical hepatology. Diseases of the liver and biliary system. – St. Petersburg: “Dialect Publishing House”; M.: “Publishing house BINOM”, – 2005. – 864 p.: ill.
- Gastroenterology: Handbook / Ed. A.Yu. Baranovsky. – St. Petersburg: Peter, 2011. – 512 p.: ill. – (National Library of Medicine Series).
- Lutai, A.V. Diagnosis, differential diagnosis and treatment of diseases of the digestive system: Textbook / A.V. Lutai, I.E. Mishina, A.A. Gudukhin, L.Ya. Kornilov, S.L. Arkhipova, R.B. Orlov, O.N. Aleutian. – Ivanovo, 2008. – 156 p.
- Akhmedov, V.A. Practical gastroenterology: A guide for doctors. – Moscow: Medical Information Agency LLC, 2011. – 416 p.
- Internal diseases: gastroenterology: A textbook for classroom work of 6th year students in specialty 060101 - general medicine / comp.: Nikolaeva L.V., Khendogina V.T., Putintseva I.V. – Krasnoyarsk: type. KrasSMU, 2010. – 175 p.
- Radiology (radiation diagnostics and radiation therapy). Ed. M.N. Tkachenko. – K.: Book-plus, 2013. – 744 p.
- Illarionov, V.E., Simonenko, V.B. Modern methods of physiotherapy: A guide for general practitioners (family doctors). – M.: OJSC “Publishing House “Medicine”, 2007. – 176 p.: ill.
- Schiff, Eugene R. Alcohol, drug, genetic and metabolic diseases / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray: trans. from English edited by N.A. Mukhina, D.T. Abdurakhmanova, E.Z. Burnevich, T.N. Lopatkina, E.L. Tanashchuk. – M.: GEOTAR-Media, 2011. – 480 p. – (Series “Liver diseases according to Schiff”).
- Schiff, Eugene R. Liver cirrhosis and its complications. Liver transplantation / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray: trans. from English edited by V.T. Ivashkina, S.V. Gauthier, J.G. Moysyuk, M.V. Mayevskaya. – M.: GEOTAR-Media, 201st. – 592 p. – (Series “Liver diseases according to Schiff”).
- Pathological physiology: Textbook for medical students. universities / N.N. Zaiko, Yu.V. Byts, A.V. Ataman et al.; Ed. N.N. Zaiko and Yu.V. Bytsya. – 3rd ed., revised. and additional – K.: “Logos”, 1996. – 644 p.; Ill. 128.
- Frolov V.A., Drozdova G.A., Kazanskaya T.A., Bilibin D.P. Demurov E.A. Pathological physiology. – M.: OJSC Publishing House “Economy”, 1999. – 616 p.
- Mikhailov, V.V. Fundamentals of pathological physiology: A guide for doctors. – M.: Medicine, 2001. – 704 p.
- Internal medicine: Textbook in 3 volumes - Vol. 1 / E.N. Amosova, O. Ya. Babak, V.N. Zaitseva and others; Ed. prof. E.N. Amosova. – K.: Medicine, 2008. – 1064 p. 10 s. color on
- Gaivoronsky, I.V., Nichiporuk, G.I. Functional anatomy of the digestive system (structure, blood supply, innervation, lymphatic drainage). Tutorial. – St. Petersburg: Elbi-SPb, 2008. – 76 p.
- Surgical diseases: Textbook. / Ed. M.I. Kuzina. – M.: GEOTAR-Media, 2020. – 992 p.
- Surgical diseases. Guide to examining a patient: Textbook / Chernousov A.F. and others - M.: Practical Medicine, 2016. - 288 p.
- Alexander JF, Lischner MN, Galambos JT Natural history of alcoholic hepatitis. 2. The longterm prognosis // Amer. J. Gastroenterol. – 1971. – Vol. 56. – P. 515-525
- Deryabina N.V., Ailamazyan E.K., Voinov V.A. Cholestatic hepatosis in pregnant women: pathogenesis, clinical picture, treatment // Zh. obstetrics. and wives disease 2003. No. 1.
- Pazzi P., Scagliarini R., Sighinolfi D. et al. Nonsteroidal antiinflammatory drug use and gallstone disease prevalence: a case-control study // Amer. J. Gastroenterol. – 1998. – Vol. 93. – P. 1420–1424.
- Marakhovsky Yu.Kh. Gallstone disease: on the way to diagnosing early stages // Ros. magazine gastroenterol., hepatol., coloproctol. – 1994. – T. IV, No. 4. – P. 6–25.
- Higashijima H., Ichimiya H., Nakano T. et al. Deconjugation of bilirubin accelerates coprecipitation of cholesterol, fatty acids, and mucin in human bile–in vitro study // J. Gastroenterol. – 1996. – Vol. 31. – P. 828–835
- Sherlock S., Dooley J. Diseases of the liver and biliary tract: Trans. from English / Ed. Z.G. Aprosina, N.A. Mukhina. – M.: GEOTAR Medicine, 1999. – 860 p.
- Dadvani S.A., Vetshev P.S., Shulutko A.M., Prudkov M.I. Cholelithiasis. – M.: Publishing house. House “Vidar-M”, 2000. – 150 p.
- Yakovenko E.P., Grigoriev P.Ya. Chronic liver diseases: diagnosis and treatment // Rus. honey. zhur. – 2003. – T. 11. – No. 5. – P. 291.
- Sadov, Alexey Cleansing the liver and kidneys. Modern and traditional methods. – St. Petersburg: Peter, 2012. – 160 pp.: ill.
- Nikitin I.G., Kuznetsov S.L., Storozhakov G.I., Petrenko N.V. Long-term results of interferon therapy for acute HCV hepatitis. // Ross. magazine gastroenterology, hepatology, coloproctology. – 1999, vol. IX, No. 1. – p. 50-53.
The effect of the disease on the body
Diffuse changes in the liver are a disorder that destabilizes the functioning of the entire digestive system. As healthy hepatocytes are replaced by adipose tissue, or cell death occurs altogether, the clinical picture of the disease gradually appears.
The liver loses its functionality to cleanse the body of toxins generated as a result of the metabolic process. As a result, corresponding signs of the disease develop, indicating changes in tissue structure.
Characteristic symptoms of disorders
There is a whole range of signs that suggest the presence of a pathology leading to tissue degeneration.
The development of disorders is accompanied by the appearance of pain and discomfort in the right side. The occurrence of discomfort is accompanied by increased physical exertion on the patient. In addition, this condition can be the result of eating large amounts of food rich in fat.
Painful sensations become constant, their intensity can increase under the influence of irritating factors.
Signs of degenerative processes can manifest themselves in any age group; sometimes such manifestations are detected in pediatric patients.
The main symptoms of the development of the pathological condition are:
- Feeling nauseous for no reason.
- Decreased appetite.
- The occurrence of belching with bitterness after eating.
- Frequent heartburn.
- Periodic occurrence of vomiting.
- Significant weakening.
- Rapid fatigue when exerting physical activity on a person.
- The appearance of frequent headaches and migraines.
In the male population, pathological changes can provoke problems with sexual function. When such a disorder develops, women experience hormonal imbalance. In the presence of diabetes, hormonal imbalance leads to exacerbation of the disease, which significantly affects dystrophic changes in the liver and pancreas parenchyma.
In patients suffering from this disorder, a change in the color of the skin and whites of the eyes is detected. Sometimes, with prolonged development of the disease, darkening of urine and discoloration of feces are detected.
Forms of pathological changes in the parenchyma
There are several types of the disease. All types of lesions can be divided into three groups.
The first group is minor lesions. This form of pathology is common among the middle-aged population. Most often, such forms of disturbance occur at different stages of hepatitis; unfavorable factors provoke such disruptions.
The second group – lesions of the parenchyma of moderate severity, occur due to poisoning by frequent consumption of alcoholic beverages and consumption of unhealthy foods. Taking vitamin complexes, as well as switching to eating natural foods and avoiding processed foods, helps correct the situation.
The third group - severe lesions, are observed in patients suffering from diabetes. Quite often they occur in the presence of obesity and tumors in humans.
There are several types of parenchyma changes. Doctors distinguish the following types:
- hypertrophic;
- sclerotic;
- swelling;
- dystrophic.
Each type has its own characteristic reasons for the formation of changes.
New information: Diabetic ketoacidosis: what it is, symptoms and treatment at home
Diffuse forms of pancreatic pathology manifest themselves:
- Moderate increase in parenchyma density. This pathology is caused by the occurrence of acute pancreatitis in the patient. This form is accompanied by tissue lysis produced by digestive enzymes. When performing an ultrasound, an increase in size is observed, the pathology is accompanied by the appearance of swelling of the walls.
- By reducing the thickness of the functional tissue, the disorder develops when the patient has chronic pancreatitis. The causes of such phenomena are considered to be disturbances in the functioning of the gastrointestinal tract.
In addition, lipomatosis may occur. This form of pathology is caused by the appearance of a fatty layer.
Regardless of the form and type of illness, when the first suspicion arises, you must contact your doctor. Only a full medical examination can clarify the cause of the pathological processes leading to tissue deformation.