What is an in vitro fertilization program?
Thanks to the revolutionary development of assisted reproductive technologies, a method of treating infertility has emerged that has given great hope to infertile couples. This is a method of in vitro fertilization, embryo transfer, which today is the most effective method of treating infertility, helping even in the most seemingly hopeless situations. IVF, embryo implantation is used for absolute female infertility (in the absence or complete obstruction of both fallopian tubes), for male infertility, for infertility of unknown cause, as well as for ineffective conservative or surgical treatment of other forms of infertility. Therefore, doctors believe that it is impossible to continue treating infertility with other methods for more than 1.5–2 years if their ineffectiveness is obvious. The sooner a couple contacts an in vitro fertilization clinic, the higher their chances of success. During in vitro fertilization, after stimulation of the woman's ovaries, several follicles with eggs mature. Directly in vitro fertilization is carried out in this way: the doctor punctures the ovary, extracting eggs, which are then fertilized with the sperm of the husband or donor outside the mother’s body. If the quality of the spouse's sperm is reduced, a single sperm is injected using a microneedle (ICSI method). After a few days, embryo transfer takes place: the embryos obtained through IVF fertilization are transferred into the woman’s uterine cavity. Next, the embryo attaches and the embryo in the uterus continues to develop. After embryo transfer, one attempt at IVF fertilization, embryo implantation gives a chance of conception from 20% to 30%, which is even slightly higher than the average rate of pregnancy naturally. The likelihood of conception and successful development of the embryo during the procedure after embryo transfer depends on the age of the spouses, their state of health, the quality of the drugs used, the quality of the resulting embryos, as well as some other factors. The correct day for embryo implantation is determined by a specialist doctor. After embryo transfer, the days after embryo transfer should be supervised by a specialist. The failure of one attempt at IVF fertilization does not mean that this method - embryo transfer - was ineffective. Each subsequent IVF attempt and embryo implantation significantly increases the total chances of a successful pregnancy after embryo transfer. Within a year of treatment, in vitro fertilization after embryo transfer gives an almost ninety percent chance of getting pregnant. In the three decades since the birth of Englishwoman Louise Brown, the first child born from an egg fertilized in vitro (1978), more than three million children have been born using this method. Modern assisted reproductive technologies and embryo transfer have already helped millions of infertile couples around the world. We hope that they will help you too. If you do not have the funds to transfer embryos, then you can try to perform in vitro fertilization for free, or transfer embryos using a special state program. However, it should be remembered that free in vitro fertilization is much more difficult than a paid procedure - since if you fail, you will wait a long time for the next chance to get free in vitro fertilization. Good luck!
What precedes surgery?
Before the puncture, the patient undergoes a comprehensive examination of the body using laboratory and instrumental research methods.
The set of diagnostic measures includes:
- visual examination of the reproductive organs on a gynecological chair;
- a general blood test, which provides information about the general condition of the body and the presence of inflammatory processes;
- blood test for hormones (estradiol, progesterone, prolactin, thyroxine, FSH, LH, testosterone, etc.);
- examination of the pelvic organs and in particular the ovaries using ultrasound;
- study of anamnesis data.
After the diagnosis, the reproductive specialist decides on which day of the cycle to perform in vitro fertilization. Artificial insemination is preceded by active hormonal therapy, carried out to stimulate the maturation of follicles. 36 hours before the expected date of surgery, the patient receives an injection of the hormone human chorionic gonadotropin (Pregnil). From this moment on, she is under the strict supervision of the attending physician. It is very important not to miss the moment of follicle maturation and their spontaneous rupture with subsequent release into the abdominal cavity.
To prevent premature rupture of follicles, the likelihood of which is stimulated by its own hormones secreted by the pituitary gland, GnRH is used. Gonadotropic hormones influence the production of female sex hormones and are also involved in the process of oocyte maturation. Among the most commonly used drugs by reproductologists are: Decapeptyl-Daily (Diferelin-Daily), Orgalutran, Cetrotide, Menopur and others. Hormonal agents in the form of injections begin to be used from the 6th day from the start of the follicle stimulation process. The therapeutic course on average does not exceed 5 injections.
Ultrasound examination of the ovaries allows you to identify follicles suitable for fertilization. The number of mature follicles should not exceed 18-20. Rapid growth of follicles threatens their lack of sexual maturity. An experienced specialist will determine exactly which follicles to take. The size of the follicles and their appearance do not always meet the expectations of a reproductive specialist. A larger size may indicate the presence of two eggs in the follicle. The more female germ cells are subsequently identified, the higher the chances of successful fertilization. You must have at least 3 eggs.
Follicular fluid collected by aspiration is transferred to an embryologist for further examination for:
- germ cell maturity;
- absence of genetic abnormalities;
- presence of pathogenic flora (bacteria, viruses).
Egg retrieval can also be done using laparoscopy. This technique is practiced if it is impossible to perform surgical manipulations through the vaginal wall. The use of laparoscopy is rational for multiple adhesions in the ovaries, as well as in the case of individual characteristics of the reproductive organs.
While genetic material is being collected from a woman, her sexual partner (spouse) prepares seminal ejaculate for further study by an embryologist. The quality of sperm depends on the physiological characteristics of the sperm.
The quality of sperm is influenced by the following factors:
- Mobility. The most active individuals are selected for fertilization.
- Quantity. To carry out the procedure, you need to have as many sperm as there are eggs, but the greater the number, the higher the chances of a successful result.
- Appearance. An experienced specialist will easily identify sperm unsuitable for fertilization. Violation of structure and shape may indicate the presence of chromosomal abnormalities.
- Bacteriological examination will determine the presence of pathogenic flora. Infected sperm is unsuitable for IVF.
Seed material can be frozen and later used if necessary.
After the adaptation process, female and male cells are combined in a test tube and further developments are observed.
Program outline. Embryo implantation. Before and after embryo transfer
The IVF program consists of several stages. Each stage is important in its own way, so you need to treat it very responsibly, strictly following all the doctor’s recommendations.
Stage I Determination of the in vitro fertilization program, including treatment tactics after a preliminary examination.
Stage II Preparing spouses for such an important procedure as IVF fertilization: correction of hormonal abnormalities, including spermatogenesis disorders, treatment of infections
Stage III Stimulation of superovulation, ultrasound monitoring (10–30 days).
Stage IV Introduction of human chorionic gonadotropin (hCG) for the final maturation of eggs before in vitro fertilization (1 day).
Stage V Follicle puncture, egg collection, sperm donation. Fertilization of an egg with the sperm of a spouse or donor (1 day). Stage VI Cultivation of embryos, observation of embryo fragmentation (2–5 days).
Stage VII On the selected day of embryo transfer - transfer of embryos into the uterine cavity, after embryo transfer - freezing of the remaining embryos as necessary (1 day).
Stage VIII Days after embryo transfer - hormonal support for early pregnancy after embryo transfer. It is important that the implantation of the embryo is successful. (up to 10-14 weeks).
Stage IX Pregnancy test associated with the detection of the blood hormone hCG (2 weeks after embryo transfer, IVF fertilization).
Stage X ultrasound – diagnosis of pregnancy (3 weeks after embryo transfer, in vitro fertilization procedure).
Stage XI Pregnancy management.
XII stage of Childbirth (maternity hospital).
What is ovarian puncture
Ovarian puncture is a medical procedure that involves taking the contents of the reproductive gland for further use.
The procedure is performed exclusively within the walls of a hospital. The patient first undergoes a series of preparatory procedures, and the doctor chooses the method of pain relief. The puncture is a mandatory condition of the IVF protocol. After receiving the material, fertilization is carried out in vitro. The final stage of in vitro fertilization is the transfer of embryos into the uterus. The puncture also involves the treatment of tumors of the gonads. Using a well-known procedure, the contents of the cyst are collected for subsequent study. The histology performed gives a clear picture of the tumor process.
The procedure is a minimally invasive procedure. It is known that the smaller the area of tissue damage, the faster the recovery and the lower the risk of complications. Based on this, we can call ovarian puncture a safe procedure. However, we should not forget that it is still a surgical intervention and also requires the use of anesthesia.
Today, ovarian puncture is recognized as a safe and accessible medical procedure. All women, without exception, who want to undergo IVF with their own eggs are subjected to it.
Preparation for the procedure
Lifestyle for both spouses
In order for the body to be ready for such a procedure as embryo transfer and the upcoming pregnancy, it is necessary to maintain a healthy lifestyle. The diet should be varied, rich in vitamins, proteins, containing a moderate amount of fats, as well as carbohydrates. No strict diets. When you need to donate blood for biochemical or hormonal studies, you can have breakfast only after drawing blood. It is recommended to take vitamin and mineral complexes intended for pregnant women. An alternative is to take folic acid, potassium iodide, and vitamin E in small doses a month before the start of the program. Avoid taking medications that are contraindicated during pregnancy. Smoking, even passive smoking, should be avoided. You should not drink more than two cups of coffee per day, and alcohol consumption should be kept to a minimum. Avoid hot baths, steam baths, saunas. Try to lead an active, mobile lifestyle. Try to ensure that the treatment has as little impact on your mood as possible. Avoid significant stress, as well as physical or psychological stress. After embryo transfer, the importance of a healthy lifestyle increases even more
Sexual contacts
The general nature of sexual activity during the in vitro fertilization procedure should not change. You can have sex with the same frequency as always. But you need to abstain from sexual intercourse for 3-4 days so that your husband can accumulate a sufficient amount of sperm. Also, the spouse should refrain from masturbation. Abstinence should continue for about seven days until the day of embryo transfer arrives. Sexual intercourse after embryo transfer should be avoided until pregnancy tests show that the embryo has been successfully implanted and the embryo is developing properly. Both spouses should try to avoid casual sex. Detected genital infections must be treated, so subsequent sexual intercourse should be carried out with a condom. When in vitro fertilization is performed, after embryo transfer, pain during sexual intercourse is possible due to enlarged ovaries.
Minimum preliminary examination
When you are indicated for an IVF procedure or embryo transfer, a number of studies can be done at your place of residence. Find out the required minimum examinations. Usually this is a spermogram of the spouse, a hormonal analysis, an image of the uterus, fallopian tubes, a blood test, and a vaginal smear analysis for the presence of infectious diseases. When you come to your initial appointment with a doctor, do not forget to take with you all the available results of previous examinations, extracts from medical records, etc. All this will be needed for the embryo implantation to be successful. Infections Before the procedure, it may be necessary to be examined for some infections that, after embryo transfer, pose a danger to the embryo and have a negative impact on its development, as well as on the pregnancy. These include, for example, herpes, cytomegalovirus, rubella, toxoplasmosis. These infections are widespread, but often occur hidden. The scope of diagnosis is determined by the attending physician.
Hormonal examination Often, infertility is accompanied by hormonal abnormalities. Their timely detection, as well as correction, can increase not only the likelihood of pregnancy after embryo transfer, but also the chances of its favorable course. Most hormones are tested from days 1 to 5 of the menstrual cycle. Therefore, the first visit should occur during this period. Blood is donated from a vein, usually in the morning, on an empty stomach.
Visit to an andrologist, sperm examination
Treatment of infertility with IVF involves a mandatory examination by an andrologist, including sperm testing. Before a sperm analysis, the spouse must follow some rules: abstain from sexual activity for 3 to 7 days (optimally 5), do not drink alcohol, do not take steam, no hot baths, do not urinate for two hours before visiting the doctor, eat only low-fat, non-spicy foods.
Planning visits to the doctor Treatment with IVF and embryo transfer takes place on an outpatient basis, but requires discipline and punctuality from patients. Before starting the program, plan your activities so that you do not have night shifts so that you can undergo ovulation stimulation (for 2-4 weeks), and then come for puncture and embryo transfer on the day of embryo implantation. The presence of the husband is required for a preliminary examination and sperm donation during follicle puncture. After the embryo transfer, you will be issued a sick leave certificate.
Agreements If you are planning to start treatment with IVF or other methods of assisted reproduction, which include ICSI, artificial insemination, fertilization with donor sperm, egg donation, surrogacy, then first decide with your doctor all the ethical and legal issues that concern you. For each type of treatment, a legal agreement is concluded with the clinic, which must be signed by both spouses.
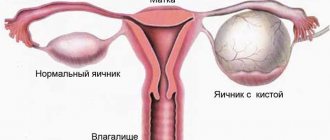
Why is an ovarian cyst punctured?
An ovarian cyst is a pathological neoplasm, the internal contents of which are liquid or semi-liquid exudate. The disease has an increased risk of relapse even after complete therapy.
Important! Puncture of the formation, with an existing cyst, is carried out in each case, and allows you to determine the source of the pathology and the method of further treatment.
There are no special indications for ovarian puncture. Only the attending physician can determine the need for a prescription. As a rule, a puncture is performed to diagnose the disease and simultaneously remove the tumor.
Puncture is more often performed for functional tumors that cannot be eliminated with conservative therapy
Before undergoing ovarian puncture, the patient must undergo some tests and examinations. This will reduce the risk of negative consequences during the procedure.
The manipulation requires the use of general anesthesia, and the drug is administered intravenously. The duration of the manipulation is approximately 40 minutes. After 1-2 hours, the woman can go home. The general condition will be normal.
The advantages of ovarian puncture are as follows:
- determining the shape and size of a paired organ,
- detection of the inflammatory process in the ovary,
- clarification of the nature of the tumor or cyst,
- determining the cause of internal bleeding.
In the case of an ovarian puncture for therapeutic purposes, the internal contents of the cyst are completely removed, and a liquid antibiotic or alcohol solution is injected into the resulting area.
The puncture is performed under ultrasound control
The introduction of the drug allows you to fasten the walls of the tumor. Removal of a cyst using this method is prescribed when the tumor size is at least 16-18 cm. Smaller tumor-like growths cannot be corrected by puncture.
Stimulation of superovulation
In order for the likelihood of pregnancy to be higher after one IVF attempt, after embryo transfer, it is necessary to obtain several eggs suitable for fertilization. For this purpose, before the procedure, the so-called stimulation of superovulation is carried out, when the woman is prescribed medications that cause the simultaneous maturation of several follicles. Various drugs can be used to stimulate superovulation. Before stimulation begins, the doctor discusses with you the most appropriate treatment option, selects medications, and determines the sequence of their use, which is called the “stimulation protocol.”
Drugs to stimulate superovulation
Preparations containing follicle-stimulating hormone Follicle-stimulating hormone (FSH) is responsible for the maturation of follicles, therefore, when stimulating superovulation, drugs containing FSH are used. Recombinant drugs are now considered the most effective. They increase the pregnancy rate and reduce treatment costs. One such recombinant FSH is the drug Puregon, created through genetic engineering. Nowadays, for maximum convenience of women, the Puregon Pen injector pen is used. The Puregon Pen injector pen is intended for self-administration of Puregon subcutaneously by patients. The pen is designed for reusable use using a cartridge with a ready-made Puregon solution.
Puregon-Pen reduces the pain of manipulation thanks to microneedling - this is a new method of administering FSH - Puregon, which provides the following advantages:
- maximum accuracy of administration of the dose of Puregon prescribed by the doctor,
- maximum possibilities for dose adjustment based on the individual characteristics of the patient,
- maximum ease of use,
- reduce additional stress associated with the treatment process itself, and therefore your confidence increases.
Drugs that suppress the production of the pituitary gland's own hormones (hormone agonists, antagonists) To prevent a woman's own pituitary gland hormones from interfering with the stimulation of superovulation, their production is blocked by antagonists. Orgalutran is a new antagonist that allows you to instantly block the pituitary gland and then quickly restore its function, which reduces the duration of treatment by almost half compared to traditional drugs (agonists). Agonists (triptorelin, goserelin, leuprorelin, buserelin) require fairly long-term administration. They need to be administered daily for 20–30 days, or once, but in a large dose, which dissolves in about a month.
Preparations containing human chorionic gonadotropin (hCG) Follicular puncture is carried out 36 hours after the injection of hCG, which initiates ovulation of mature follicles. The use of hCG allows you to obtain a mature egg ready for fertilization. One of the drugs containing hCG is Pregnil.
Technique for follicle puncture
Ovarian puncture is a surgical intervention that is carried out in compliance with the rules of asepsis and antisepsis in an operating room. The patient is asked to change into sterilized or disposable clothing. Before a woman is put under anesthesia, her blood pressure is measured and some indicators of the cardiovascular system are recorded.
After the onset of anesthesia, the gynecologist treats the puncture site with an antiseptic solution. The cervix is exposed in the speculum and fixed with bullet forceps. The inferior speculum is then removed and a hollow needle attached to an ultrasound probe is inserted into the vagina. Using ultrasound, the doctor locates the ovary and follicles, pierces them successively and sucks out the contents. The average duration of a puncture is 15-20 minutes. The follicular fluid along with the eggs is transferred to the embryology laboratory. Before fertilization, the oocytes undergo a thorough check.
The next stage is the interaction of eggs and sperm. When there is not enough genetic material, fertilization is carried out using the ICSI or PIXI method.
In some cases (with massive adhesions in the pelvis, abnormal location of the ovaries), it is impossible to obtain eggs using transvaginal puncture. In such cases, the woman is offered laparoscopy.
Superovulation stimulation protocols
During in vitro fertilization, different types of protocols are used. It should be remembered that there are no strict treatment regimens; individual variations are possible for each of the protocols below.
"Clean Protocol"
Some women use stimulation regimens without blocking the pituitary gland. For this purpose, only drugs containing FSH are used, for example Puregon Pan. This scheme is called “pure”. Its disadvantage is the likelihood of premature ovulation (rupture) of the follicle even before puncture, which makes it impossible to obtain eggs. With this protocol, the administration of stimulant drugs begins on the 2nd–3rd day of menstruation and continues for 9–14 days. The daily dose is adjusted by the doctor depending on the ultrasound data, which is usually performed 4-5 times during the entire stimulation period. For the final maturation of the follicles, hCG, for example Pregnil, is injected, and after 35–36 hours the follicles are punctured.
"Long Protocol"
The protocol is called “long” because, as a rule, it begins on the 21st–23rd (rarely from the 2nd–3rd) day of the menstrual cycle preceding stimulation. To block the pituitary gland, only an agonist is taken for the first 5 days from the start of treatment. After blockade of the pituitary gland is achieved, menstruation begins, and from the second to third day from its onset, stimulation is carried out with drugs containing FSH, in the same way as with the “pure” regimen, but together with the continued administration of the agonist.
"Optimal Protocol"
When using the new antagonist Orgalutran, the stimulation protocol is significantly shortened, although a pronounced, easily reversible blockade of the pituitary gland remains. Stimulation begins, as with the “pure” regimen, from 2–3 days of the menstrual cycle by daily administration of a drug containing FSH. Then, from the 5th or 6th day of stimulation, daily injections of Orgalutran are given, but stimulation continues. Thus, the “Optimal Protocol” becomes short and therefore effective. The combination of the new generation drug Puregon with Orgalutran (antagonist) is: - reduction of treatment time; - better tolerance of injections; - proven effectiveness. Thanks to this, the combined use of Puregon with Orgalutran can be called “Two components of hope in the treatment of infertility.”
How does follicle puncture occur?
Puncture of follicles during IVF is carried out by puncturing the vaginal vault with a special needle, at the end of which there is a sensor. If a woman has specific structural features of the organs of the reproductive system, the egg puncture is performed through laparoscopy.
The patient, who is located in the gynecological chair, is given general anesthesia. After she falls asleep, the doctor uses a special needle to place a sensor connected to an ultrasound machine through the vaginal vault to the ovaries. Looking at the monitor, the doctor carefully “collects” the contents of the follicles through a special pump connected to the needle.
Depending on the size of the follicles and their number, the surgical intervention can last from 5 to 10 minutes. This time is enough for an experienced physician to use a single puncture to collect follicular fluid filled with eggs from both ovaries. At the same time, the sampling is carried out very carefully to minimize risks. The contents of the puncture devices have a special treatment that does not allow the egg to be damaged during the procedure. And at the tip of the needle there is a tiny air bubble, which helps to clearly see the contents of the cavity.
As soon as the necessary biological fluid is obtained, it is sent to the laboratory to identify the most viable eggs and further grow them in an optimal environment for them. After the collection of follicular fluid is completed, the anesthesia is stopped, and after 2-3 minutes the patient comes to her senses.
Immediately after the procedure, the woman cannot go home: she must spend 1-2 hours in a medical facility under the supervision of doctors. She is also prescribed a broad-spectrum antibiotic to prevent infection.
We do the injections ourselves
Before you start injections, carefully read the storage conditions of the drugs. Some of them require storage at temperatures close to 0°C. Others can be stored at room temperature. Puregon Pen, Orgalutran, Pregnil are stored at temperatures from 3°C to 25–30°C. Freezing of drugs, as well as direct sunlight, can change their activity.
How to give injections?
Using the Puregon Pen injector pen, patients inject themselves themselves, without additional assistance from medical personnel. It's simple, and most importantly, convenient. If a woman uses drugs that are administered with a syringe, you can seek help either in the treatment room of the clinic, or in the clinic at your place of residence, or involve someone familiar with injection skills. Puregon or Orgalutran are administered subcutaneously, Pregnil - intramuscularly. Injections should be done at one time, for example, in the afternoon, and the environment should be as calm as possible. Drugs must be administered slowly. Each administered dose is of great importance, so errors during administration can significantly affect the outcome of the entire treatment. If you forget to administer the drug, do not administer a double dose to make up for the missed injection, but consult your doctor immediately. Some drugs, for example Pregnil, are available in powder form, with solvent ampoules attached separately. Read the instructions carefully. Drugs can only be dissolved using a sterile syringe. The substance dissolves instantly, without foreign impurities.
Monitoring
During stimulation of superovulation, ultrasound monitoring of the growth of ovarian follicles, as well as the maturation of the endometrium, is carried out. This is necessary to adjust the dose of administered drugs, which can be increased or decreased. It all depends on the condition of these organs. On the one hand, it is necessary to obtain a sufficient number of mature eggs, but on the other hand, excessive stimulation can lead to complications. A follicle with a diameter of 17–20 mm is considered mature, with a thickness of the uterine mucosa (endometrium) greater than 8 mm.
Ultrasound monitoring
Monitoring is done by your healthcare provider, usually on days 2–3 of your menstrual cycle. At the same time, stimulant drugs are prescribed. The next follicular growth study is repeated after approximately 5 days. Further studies are carried out more often, almost daily, until the follicles reach sizes close to ovulatory. The study is carried out with an ultrasound sensor, which is inserted into the vagina. This procedure is painless. Do it safely. To ensure sterility, a disposable condom is placed on the sensor. The thickness of the endometrium is assessed, as well as the number and diameter of follicles, and the doctor decides whether to change the dose of drugs. When certain criteria are reached, usually on the 10th–14th day of the cycle, a decision is made to end stimulation. After this, hCG drugs are prescribed, the exact time of their administration is reported, as well as the date of the upcoming puncture.
What should you do?
If you are scheduled for an ultrasound monitoring day, you should not do any injections in the morning without your doctor's advice. An ultrasound through the vagina is performed with an empty bladder, otherwise the doctor will not be able to see the ovaries on the monitor. You will have to undress as if for a gynecological examination.
Administration of hCG
hCG drugs (Pregnil) are administered for the final maturation of the egg. The doctor will tell you the exact time of administration of the drug, which usually occurs in the evening hours. It is very important to strictly observe the time of drug administration. The route of administration is intramuscular. The rules of administration are the same as those described earlier for intramuscular agents. Check the dose of the drug carefully, as the ampoule may contain 1,500, 5,000 IU (International Units). Sexual intercourse should be stopped. It is very important not to be late, to arrive at the puncture on time, 35–36 hours after the hCG injection. It is advisable to take a robe, slippers, nightgown or long T-shirt with you to the puncture, and bring socks. When you have a puncture, your spouse will need to be present.
Recovery and well-being after IVF follicle puncture
Follicle puncture is a serious intervention in the functioning of the female reproductive system, which is accompanied by hormonal therapy, so the state of health after this procedure may be unpleasant.
Pain in the lower abdomen that lasts from two to four days is considered normal. Possible swelling of the ovaries up to 6 cm, slight bleeding, and an increase in temperature by 2-3 degrees.
Did you know? The first child born through IVF was a girl named Louise Brown. This happened in 1977 in England. Since then, more than five million children have been conceived artificially.
If the ovaries have enlarged to 12 cm or more, the lower abdomen is swollen and heavy spotting appears, then you need medical supervision.
Lifestyle
After the puncture, adhere to the principle of minimal exercise for one week. To avoid hyperovulation, provide yourself with eight hours of timely sleep and postpone any sexual intercourse for the next month and a half. Avoid stress and negative emotions. Regular swimming will have a good effect.
You may be interested in reading about when to take a pregnancy test after embryo transfer.
Diet
For two weeks after the procedure, continue the protein diet:
- exclude fruits (especially those rich in fiber), baked goods, and raw vegetables from your diet;
- drink a lot of clean water - at least four liters a day;
- avoid alcohol, fatty foods and caffeinated drinks;
- Buckwheat porridge with a small amount of olive oil, low-fat kefir and yogurt without additives, sesame and sea buckthorn oil will be useful.
Drugs
Since a corpus luteum forms at the site of the punctured follicle, medications must be prescribed to maintain normal hormone levels.
Important! In some cases, antibiotics may be prescribed after puncture to prevent the development of ovarian inflammation. They are prescribed for diagnosing low-grade fever, painful sensations in the lower abdomen during palpation and intestinal disorders.
Clexane is prescribed for normal healing of the ovaries and the prevention of blood clots, Dostinex or Pregnil - to prevent lactation and hyperstimulation.
Puncture
Puncture of the ovarian follicles is performed to obtain eggs. During the puncture, the doctor, under ultrasound guidance, empties the follicles through the vagina using a needle connected to a vacuum device. As a rule, the puncture is performed in the morning, strictly on an empty stomach, under intravenous anesthesia. There is no reason to be afraid, this procedure is painless, quick, and the thin needle will not cause any serious damage.
Before puncture
You can’t eat anything the night before, or even drink anything after midnight. You can shave the hair around the vaginal opening. You cannot use decorative cosmetics. Immediately before the puncture, already at the IVF clinic, you need to empty your bladder and put on a clean shirt. If you are allergic to any medications, be sure to notify the anesthesiologist about this.
After the puncture
You will wake up in 5-10 minutes, and 40-60 minutes after the puncture you will be able to get up. The doctor will tell you about the results of the puncture, how many eggs were obtained, and then determine the date of the next visit for embryo transfer. The next procedure is embryo implantation; your doctor will tell you on what day to schedule it. The doctor will also give you prescriptions for the next two weeks aimed at maintaining sufficient levels of pregnancy hormones after embryo transfer (hCG injections or progesterone preparations). It is better to have someone accompany you after the puncture. After the puncture, it is strictly forbidden to drive. If you feel pain in the lower abdomen, you can take a painkiller tablet after consulting your doctor. You can only obtain information about the quality of eggs, sperm, success of fertilization, fragmentation, and number of embryos from your attending physician.
What is special about this method?
Ovarian puncture during IVF is one of the main stages of a complex of surgical procedures performed by reproductive specialists in order to obtain a mature egg.
It involves taking follicular fluid from the follicles with the germ cells and oocytes they contain. The procedure is performed by aspiration using a transinductor with a transvaginal sensor attached to it. Ultrasound diagnostics allows you to control all stages of the procedure.
Puncture of the follicles occurs in the form of a puncture of the vaginal wall with a thin aspiration needle and its subsequent insertion into the body of the ovary. Having identified a mature follicle using ultrasound, the reproductologist inserts a needle into it. After puncture using suction, the follicular fluid with the germ cells and oocytes contained in it is placed in a sterile tube.
Preparation for follicle puncture is of no small importance. Maintaining a gentle daily routine and nutrition directly affects the result of surgical intervention. The gentle regime requires compliance with the following measures:
- restriction of sexual activity for one week before the planned date of puncture;
- reduction of physical and mental stress, frequent walks in the fresh air;
- balanced diet, emphasis on protein products of plant and animal origin;
- active drinking regime (at least 2 liters of water or fruit juice per day);
- minimize your stay in public places to prevent possible infection with viral diseases;
- compliance with the temperature regime when carrying out hygienic water procedures (water should not exceed 40 degrees);
- taking any medications of synthetic and herbal origin must be agreed with your doctor;
- eliminating the stress factor allows you to stabilize the psycho-emotional state of a woman before the procedure.
How is material collected during puncture? What sensations can they expect after the puncture, how much the operated area will hurt, and what happens afterwards. Don't panic. During the diagnostic period, the attending physician will explain in detail the essence of the proposed operation, determine the likelihood of possible complications, having studied the medical history in detail.
Don't worry about pain. Anesthesia administered before puncture of the follicles will completely relieve the woman of pain. The doctor decides which method of anesthesia to choose in each individual case.
There are two types of anesthesia used before surgery:
- Local anesthesia in the form of an anesthetic injection into the vaginal wall. Usually a 1% or 2% solution of novocaine is used. Some doctors prefer this type of pain relief as an alternative to toxic systemic drugs that worsen the physiological characteristics of the reproductive organs during the harvesting procedure.
- General anesthesia involves the intravenous administration of short-term anesthesia. This option is more acceptable due to the absolute rest required during the puncture.
The rationality of using any type of anesthesia is supported by test results and other anamnesis data. In any case, this issue is discussed with the doctor in advance.
Artificial insemination
When the day of the puncture arrives, the spouse must donate sperm to the laboratory assistant. The sperm is cleaned of excess plasma and prepared for fertilization, checking the quantity, quality, and motility of sperm. The follicular fluid filled with eggs obtained after puncture of the ovaries is examined under a microscope, the eggs are found, they are selected and washed. Each egg is carefully placed in a separate well in a special cup filled with a nutrient medium. Cups containing sperm are always signed immediately. Then, if there are enough sperm and they are motile, some of the sperm is added to the eggs, after which the incubator is left for approximately 12 hours. The sperm themselves must swim to the eggs and fertilize them. Then they check whether fertilization has occurred. Fertilized eggs, or rather embryos, continue to be cultivated for 2 to 5 days.
ICSI
If there are too few sperm, then the ICSI procedure is performed, that is, the injection of a single sperm using a microneedle. Under the control of a microscope, using micromanipulators, the embryologist selects only high-quality sperm and injects them into the egg.
Embryo transfer
When the embryo will be implanted and on what day to schedule the embryo transfer procedure is determined by the doctor. As a rule, this occurs 2–5 days after the puncture. Embryos can be transferred both at the stage of several cells - blastomeres, and at a later stage - blastocysts. The embryo transfer procedure is painless, although slight discomfort is sometimes possible. Speculums are inserted into the vagina, and a flexible catheter is inserted into the cervical canal. Embryos are transferred through this catheter, the number of which is determined by the doctor. It is usually recommended to transfer two embryos, since transferring a larger number is undesirable due to the risk of developing multiple pregnancies. After embryo transfer, the remaining high-quality embryos can be frozen so that they can be used in subsequent attempts.
What should you do when transferring embryos?
During insertion of the catheter, try to relax as much as possible without straining your lower abdomen. Try to be positive. After embryo transfer, you can remain horizontal for some time. It is better to return home with an escort. At home you should also relax and try to distract yourself from obsessive worries.
What to do next?
At this stage - after embryo transfer - the program ends. If there are no complications, the embryo has settled in the uterus and is developing successfully, then you will not be hospitalized. But if you wish, after embryo transfer, you can apply for a hospital stay. The doctor gives clear recommendations on further supportive hormonal treatment, which must be strictly followed. You may be prescribed drugs for hormonal support of pregnancy - progesterone or hCG. Try to spare yourself physically and psychologically in the first weeks after embryo transfer. Try to drink more. After embryo transfer, it is advisable to measure body weight, monitor urination, abdominal volume, and pulse rate. If you have any concerns, please contact the clinic immediately. There you will be issued a sick leave certificate for 10–14 days. If pregnancy occurs after embryo transfer, sick leave can be issued by the antenatal clinic at the place of residence.
Pregnancy - yes or no?
Whether pregnancy has occurred or not will be known no earlier than the 14th day after embryo transfer. Do not try to independently determine pregnancy using tests until this moment, since at this stage the embryo cannot yet produce sufficient amounts of the hCG hormone. The answer may also be incorrect due to the use of certain hormonal medications. In addition, rapid test strips often give false results. Two weeks after embryo transfer, go for a blood test for the beta subunit of hCG, which is an indicator of pregnancy. If the test result is positive, it means pregnancy has occurred. Almost every one and a half to two days the amount of hCG will double. Pregnancy after embryo transfer, determined by hCG, is called “biochemical pregnancy”. She still needs ultrasound confirmation, which allows you to see the fertilized egg only starting from the 3rd week after embryo transfer. Therefore, after embryo transfer, you will need to come for an ultrasound diagnosis of pregnancy. If pregnancy occurs, you should be under constant supervision of obstetricians and gynecologists, since after embryo transfer you still have to carry a pregnancy that was achieved in such a difficult way. If you experience pain, bleeding or other worrying symptoms, contact your doctor immediately. The appearance of menstruation, a negative test result, and the absence of a fertilized egg according to ultrasound data indicate that pregnancy did not occur after embryo transfer. However, a negative result does not mean that the IVF method was ineffective. Subsequent attempts may be successful. As already mentioned, the probability of pregnancy after embryo transfer per attempt ranges from 20 to 30%, and with each subsequent attempt, the total chances of becoming pregnant increase over the course of a year of treatment to 90%. You can leave an interval of about 2 months between attempts. If you are unable to visit the center to diagnose pregnancy, then determination of hCG in the blood after embryo transfer and ultrasound can be carried out in clinics at your place of residence. But in any case, please inform your doctor at the IVF center about the diagnostic results and discuss further actions.
How to prepare for follicle puncture during IVF
There are certain principles that must be followed in order not to trigger hyperovulation after an hCG injection:
- Four days before the procedure and two weeks after it, abstain from all sexual contact.
- Switch to a protein diet, excluding from your diet all foods that can cause increased gas formation and intestinal motility.
- Drink plenty of water before and after the procedure, this will help the ovaries return to normal after enlargement.
- Skip dinner the evening before the puncture, and breakfast on the morning of the procedure.
- Arrive on time to avoid missing your egg retrieval time. If they come out of the follicles on their own, it will no longer be possible to collect them with a needle.
Possible complications
Ovarian hyperstimulation
As a result of stimulation of the ovaries after puncture, many so-called corpora lutea are formed at the site of the follicles. Some women do not tolerate excess hormones produced by the corpus luteum. In approximately 10% of cases, a mild form of hyperstimulation syndrome develops. This is indicated by pain in the lower abdomen, nausea, and abdominal enlargement. In more serious cases, weakness, decreased urine output, and severe bloating are observed. In rare, severe forms, breathing may become difficult and blood pressure may drop. Treatment for hyperstimulation syndrome usually involves drinking plenty of fluids and taking special medications, which can sometimes be administered intravenously. For mild forms of hyperstimulation, you can stay at home, but be sure to keep your doctor informed of your condition. More severe disease requires hospitalization.
Multiple pregnancy
To increase the likelihood of pregnancy using the IVF method, several embryos (no more than three) are usually transferred into a woman's uterus. Sometimes, after embryo transfer, this can lead to the development of multiple pregnancies. If more than two fetuses develop in the uterus, then carrying such a pregnancy can be quite difficult. There are methods to stop the development of one embryo without affecting the others. This operation is called fetal reduction and is performed under ultrasound guidance. Usually, after embryo transfer, two embryos are left. The likelihood of successfully carrying a pregnancy to term after embryo reduction is higher than if you leave triplets.
Ectopic pregnancy
If, after embryo transfer, weakness, dizziness, early signs of pregnancy, vague or sharp pain appear, then perhaps this is an ectopic pregnancy, in which the fetus develops not in the uterus, but outside it. Seek immediate medical attention as this condition is life-threatening as a ruptured pipe can cause severe bleeding. Ectopic pregnancy is usually treated with gentle laparoscopic surgery. If you experience any of the symptoms listed above, contact your doctor immediately. Write down the clinic's phone number, as well as the doctor's name. Also find out emergency phone numbers. By following all the doctor’s recommendations, you will reduce the risk of complications and at the same time the chances of a happy conception.
Postoperative period and recovery
Women undergoing oocyte retrieval should not worry. You should not be afraid of pain, since the maximum that is felt is the insertion of a catheter into a vein by the anesthesiologist. Recovery from anesthesia occurs over several hours, which the patient spends in the clinic. At this stage, you feel distracted attention, weakness, and slight dizziness. These disorders resolve quickly, so the patient usually goes home. It is recommended to be accompanied by relatives or friends, since anesthesia drugs are still present in the blood, and driving under their influence is prohibited.
Manipulations during egg retrieval are low-traumatic, so there is most often no serious pain in the postoperative period. There may be nagging pain when moving, small traces of blood on the underwear. Your doctor may prescribe painkillers and anti-inflammatory drugs at first.
Complications after puncture are very rare. But still, if the patient feels severe pain in the lower abdomen, vestibular disorders, or excessive weakness, it is necessary to urgently consult a doctor. Most often these are symptoms of internal bleeding. Compliance with all the rules for this procedure reduces the likelihood of such a complication to very low.
After puncture, during the first few days, patients may experience ovarian hyperstimulation. This syndrome is accompanied by nausea, pain in the lower abdomen, and bloating. In some cases, the body reacts with vomiting, urinary retention, constipation or diarrhea. The presence of such symptoms should be reported to your doctor.