Analysis of hormonal levels in women is the most important study to determine the state of the patient’s reproductive system, identify the cause of the development of problems such as infertility, menstrual irregularities, hirsutism, severe acne, etc.
An analysis of female hormones during menopause is carried out in the event of the development of severe menopausal symptoms (severe emotional lability, nervousness or depression, heart rhythm disturbances, rapidly progressing osteoporosis, frequent “hot flashes”, insomnia, dryness and atrophy of the vaginal mucosa, etc.)
The hormonal profile is also examined when planning pregnancy and during pregnancy.
Hormone testing is prescribed by an endocrinologist or gynecologist. How to check a woman’s hormonal levels should be decided exclusively by a specialized specialist, since hormone tests are performed according to special schemes, depending on the day of the menstrual cycle.
All treatment is prescribed individually, based on a comprehensive examination.
Independent interpretation of tests and selection of treatment is strictly prohibited and can lead to serious health consequences.
Which hormones to test to determine a woman’s hormonal imbalance?
The main tests for hormonal levels include studying the level of:
- luteinizing hormone (LH);
- estradiol (hormone e2);
- prolactin;
- testosterone;
- follicle-stimulating hormone (FSH);
- DHEA sulfate;
- thyroid stimulating hormone (TSH).
According to indications, the level of somatotropic hormone (GH), adenocorticotropic hormone (ACTH), 17-ketosteroids and cortisol (hydrocortisol) is additionally determined.
How are hormones produced?
Since female sex hormones are fundamental factors ensuring good health and mood, we should talk in more detail about the types of sex hormones. This will allow you to better understand the functional component of this aspect.
The endocrine system consists of endocrine glands, which to a large extent are the “producers” of hormones. The glands include:
- pituitary;
- thyroid gland;
- ovarian follicles;
- thymus;
- adrenal glands;
- epithelial body;
- hypothalamus.
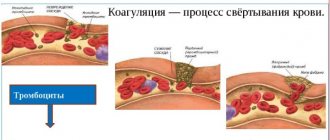
After the production of hormones by these glands, the blood transports these substances to all internal organs.
To date, science has identified more than 60 substances that are involved in the process of balancing hormonal levels. Moreover, these processes do not depend on age and gender.
Indications for hormonal testing
These studies are carried out if the patient has:
- infertility;
- spontaneous abortions;
- menstrual disorders;
- delayed puberty or premature puberty;
- inter-cycle discharge;
- dysfunctional uterine bleeding;
- decreased sexual desire;
- pain during sexual intercourse;
- dryness and atrophy of the vaginal mucosa;
- signs of endometriosis;
- hirsutism;
- anovulation;
- symptoms of polycystic ovaries;
- chronic inflammatory processes in the pelvis;
- galactorrhea;
- mastopathy;
- neoplasms in the uterus, ovaries and mammary glands;
- signs of sexual infantilism;
- obesity;
- cardiovascular pathologies at a young age;
- signs of osteoporosis;
- obesity;
- lactation disorders after childbirth;
- pain in the mammary glands;
- severe PMS;
- severe menopausal disorders;
- hair loss;
- acne, etc.
Hormonal levels are also examined to determine the ovulatory period, assess the control of ongoing hormonal therapy, control drug induction of ovulation, before in vitro fertilization, assess the condition of the feto-placental complexes, etc.
Progesterone
Progesterone is a steroid hormone of the corpus luteum of the ovaries, necessary for all stages of pregnancy. It prepares the endometrium of the uterus for implantation of a fertilized egg, and after its implantation it helps maintain pregnancy.
What are the indications for prescribing a blood test for progesterone in women?
- identifying the causes of menstrual irregularities;
- identifying the causes of infertility;
- identifying the causes of dysfunctional uterine bleeding;
- assessment of the condition of the placenta in the second half of pregnancy;
- diagnosis of true post-term pregnancy.
What preparation is required for a progesterone blood test?
The analysis is carried out on days 22-23 of the menstrual cycle, unless other dates are indicated by the attending physician. Blood is taken in the morning on an empty stomach, that is, when 8-12 hours pass between the last meal and blood collection. You can drink water. If it is not possible to come to the laboratory in the morning, you can fast for at least 6 hours before taking blood, excluding fats from your morning meal.
When donating blood, you must provide the nurse with additional information - about the day of the cycle, weeks of pregnancy, menopause; as well as taking medications that affect the level of hormones in the blood.
What are the deadlines for completing the analysis?
1 day.
What are the normal levels of progesterone in the blood of women?
| Women | Progesterone level, nmol/l |
| Follicular phase | 0,32 — 2,23 |
| Ovulatory phase (mid cycle) | 0,48 — 9,41 |
| Luteal phase | 6,99 — 56,63 |
| I trimester | 8,90 — 468,40 |
| II trimester | 71,50 — 303,10 |
| III trimester | 88,70 — 771,50 |
| Postmenopause | < 0,64 |
How is blood tested for hormones, on an empty stomach or not?
Patients are often concerned about the question: is blood taken for hormones on an empty stomach or not?
All hormonal studies are carried out exclusively on an empty stomach.
Also, it is not recommended to have sex one or two days before taking hormones.
You should avoid drinking alcohol at least one day before the test.
You should not smoke before blood collection.
In the morning before the test, you are allowed to drink still water.
On the eve of the study, it is recommended to refrain from visiting the sauna, heavy physical activity, and avoid stress.
The attending physician and laboratory staff must be notified of all medications taken by the patient. This is due to the fact that many medications can affect hormone levels.
Read more: How many days before donating blood for testing can you drink alcohol?
Normal hormone levels in men; Table 1.
| Dihydrotestosterone | 250 – 990 pg/ml |
| Testosterone | 345 – 950 ng/dl |
| Sex binding globulin | 13-70 nmol/l |
| FSH | 1.37 - 13.58 mEdl |
| LH | 2 - 9 mU/l |
| Estradiol | 16 – 73 pg/ml |
| Prolactin | 2.5 - 15 ng/ml |
| Progesterone | 0.35 – 0.63 nmol/l |
The norm for hormone analysis in men may vary in different laboratories, so the data given in the table may not always coincide with the norm in different laboratories. It is advisable that the hormonogram be assessed by an experienced specialist who will take into account all the nuances of each individual patient and determine at what level the pathology is identified and how to deal with it. As a rule, hormonal medications are prescribed to correct hormone levels.
source
Analysis of luteinizing hormone levels
The pituitary gland is the most important endocrine organ in humans. It is responsible for the synthesis of prolactin, adenocorticotropic, thyroid-stimulating, somatotropic, follicle-stimulating, luteinizing, etc. hormones.
Normally, pituitary hormones influence all organs and systems of the body. They affect the growth and development of the body, metabolic processes, the functioning of the reproductive system, the synthesis of hormones by other endocrine organs, etc.
Luteinizing hormone is produced by the anterior pituitary lobe. Normally, LH and FSH regulate the functioning of the reproductive system, are responsible for stimulating the synthesis of estrogens by ovarian tissues, support the maturation of the corpus luteum, activate the synthesis of progesterone, induce the onset of ovulation, control the maturation of follicles in the ovaries, etc.
Tests for LH levels in women are taken from the 3rd to the 8th or from the 19th to the 21st day of the cycle.
The level of luteinizing hormone in a woman’s body depends on the phase of the menstrual cycle and the age of the patient.
An increase in LH can be observed if the patient has:
- basophilic pituitary adenomas;
- hypergonadotropic hypogonadism;
- ovarian wasting syndrome;
- PCOS (polycystic ovary syndrome);
- endometriosis;
- exhaustion and anorexia;
- renal failure, etc.
Also, LH levels may increase during heavy physical activity, treatment with goserelin, ketoconazole, mestranol, naloxone, spirolactone, tamoxifen, troleandomycin, etc.
A decrease in LH is normally observed during pregnancy, after stress, surgery, and with long-term smoking of large quantities of cigarettes.
Also, low luteinizing hormone can be observed with:
- hypothalamic forms of amenorrhea;
- hypogonadotropic forms of hypogonadism;
- pituitary dwarfism;
- obesity;
- luteal phase insufficiency;
- Sheehan's disease;
- atypical forms of polycystic ovary syndrome
- treatment with anticonvulsants, carbamazepine®, conjugated estrogens, digoxin®, oral contraceptives, pravastatin®, progesterone®, tamoxifen®, valproic acid®, etc.
Read: About the norms of luteinizing hormone in women, deviations and rules for preparing for analysis
Medical reference
Female sex hormones affect many organs and systems of the female body; in addition, the condition of the skin and hair, and general well-being, also depend on them. It’s not for nothing that when a woman is nervous or even behaves inappropriately, those around her say: “Hormones are raging.”
The rules for donating blood for female hormones are approximately the same for all hormones. Firstly, tests for female sex hormones are taken on an empty stomach. Secondly, the day before the test it is necessary to exclude alcohol, smoking, sexual intercourse, and also limit physical activity. Emotional stress (therefore, it is advisable to take the test in a calm state of mind) and taking certain medications (primarily hormone-containing ones) can also lead to distorted results. If you are taking any hormonal medications, be sure to tell your doctor.
Different female sex hormones are released by women on different days of the menstrual cycle (counting from the first day of menstruation).
FSH, LH, prolactin - on days 3-5 of the cycle (LH is sometimes tested several times during the cycle to determine ovulation).
Testosterone, DHEA-s - on days 8-10 of the cycle (in some cases allowed on days 3-5 of the cycle).
Progesterone and estradiol - on days 21-22 of the cycle (ideally 7 days after expected ovulation. When measuring rectal temperature - 5-7 days after the temperature starts to rise. With an irregular cycle, it may be taken several times).
Luteinizing hormone (LH)
Luteinizing hormone is produced by the pituitary gland and regulates the activity of the sex glands: it stimulates the production of progesterone in women and testosterone in men.
The release of the hormone is pulsating in nature and depends in women on the phase of the ovulation cycle. During puberty, LH levels increase, approaching values typical for adults. In the menstrual cycle, the peak concentration of LH occurs during ovulation, after which the level of the hormone decreases. During pregnancy the concentration decreases. After the cessation of menstruation (postmenopause), the concentration of LH increases.
The ratio of luteinizing hormone and follicle stimulating hormone (LH/FSH) is important. Normally, before the onset of menstruation it is 1, after a year of menstruation - from 1 to 1.5, in the period from two years after the onset of menstruation and before menopause - from 1.5 to 2.
3 days before taking blood for LH analysis, it is necessary to exclude sports training. Do not smoke for at least an hour before taking blood. Blood must be donated in a calm state, on an empty stomach. LH analysis is done on days 4-7 of the menstrual cycle, unless other dates are indicated by the attending physician. For irregular cycles, blood is drawn to measure LH levels every day between 8 and 18 days before your expected period.
Since this hormone affects many processes in the body, LH analysis is prescribed for a variety of conditions:
- increased hair growth in women (hirsutism);
- decreased sexual desire (libido) and potency;
- lack of ovulation;
- scanty menstruation (oligomenorrhea) or absence of menstruation (amenorrhea);
- infertility;
- dysfunctional uterine bleeding (associated with cycle disorders);
- miscarriage;
- premature puberty or delayed puberty;
- growth retardation;
- underdevelopment of the genital organs;
- polycystic ovary syndrome;
- endometriosis;
- monitoring the effectiveness of hormone therapy.
Luteinizing hormone (LH) levels:
- children under 11 years of age 0.03-3.9 mIU\ml;
- men 0.8-8.4 mIU/ml;
- women: follicular phase of the cycle 1.1-8.7 mIU/ml, ovulation 13.2-72 mIU/ml, luteal phase of the cycle 0.9-14.4 mIU/ml, postmenopause 18.6-72 mIU/ml.
Elevated LH levels may mean: insufficiency of gonadal function; ovarian wasting syndrome; endometriosis; polycystic ovary syndrome (the ratio of LH and FSH is 2.5); pituitary tumors; renal failure; atrophy of the gonads in men after inflammation of the testicles due to mumps, gonorrhea, brucellosis (rarely); starvation; serious sports training; some rarer diseases.
A decrease in LH levels is observed when; hyperprolactinemia (increased prolactin levels); luteal phase deficiency; obesity; smoking; surgical interventions; stress; some rare diseases.
Follicle stimulating hormone (FSH)
FSH stimulates the formation of follicles in women; when a critical level of FSH is reached, ovulation occurs.
FSH is released into the blood in pulses at intervals of 1-4 hours. The concentration of the hormone during the release is 1.5-2.5 times higher than the average level, the release lasts about 15 minutes.
The ratio of luteinizing hormone and follicle-stimulating hormone (LH/FSH) is important. Normally, before the onset of menstruation it is 1, after a year of menstruation - from 1 to 1.5, in the period from two years after the onset of menstruation and before menopause - from 1.5 to 2.
Indications for prescribing FSH analysis:
- lack of ovulation;
- infertility;
- miscarriage;
- scanty menstruation (oligomenorrhea) or absence of menstruation (amenorrhea);
- decreased libido and potency;
- dysfunctional uterine bleeding (disturbing the cycle);
- premature puberty or delayed puberty;
- growth retardation;
- polycystic ovary syndrome;
- endometriosis;
- monitoring the effectiveness of hormone therapy.
FSH analysis is done on days 4-7 of the menstrual cycle, unless other dates are indicated by the attending physician. 3 days before taking blood, you must avoid sports training. Do not smoke for at least 1 hour before blood collection. You need to be in a calm state and on an empty stomach.
FSH standards:
• children under 11 years of age 0.3—6.7 mIU/ml;
• men 1.0—11.8 mIU/ml;
• women: follicular phase of the cycle 1.8-11.3 mIU/ml, ovulation 4.9-20.4 mIU/ml, luteal phase of the cycle 1.1-9.5 mIU/ml, postmenopause 31-130 mIU/ml .
Increased FSH values occur with: endometrioid ovarian cysts; primary hypogonadism (men); ovarian wasting syndrome; dysfunctional uterine bleeding (caused by menstrual irregularities); exposure to x-rays; renal failure; some specific diseases.
A decrease in FSH values occurs with: polycystic ovary syndrome; secondary (hypothalamic) amenorrhea (lack of menstruation caused by disorders in the hypothalamus); hyperprolactinemia (increased prolactin levels); fasting; obesity; surgical interventions; contact with lead; some specific diseases.
Estradiol
It is produced in the ovaries in women, the testes in men, and estradiol is also produced in small quantities by the adrenal cortex in men and women.
Estradiol in women ensures the formation of the reproductive system according to the female type, the development of female secondary sexual characteristics, the formation and regulation of menstrual function, the development of the egg, the growth and development of the uterus during pregnancy; is responsible for the psychophysiological characteristics of sexual behavior. Ensures the formation of subcutaneous fat tissue according to the female type.
It also enhances metabolism in bone tissue and accelerates the maturation of skeletal bones. Promotes sodium and water retention in the body. Reduces cholesterol levels and increases blood clotting activity.
In women of childbearing age, the level of estradiol in blood serum and plasma depends on the phase of the menstrual cycle. From the beginning of the menstrual cycle, the content of estradiol in the blood gradually increases, reaching a peak towards the end of the follicular phase (it stimulates the release of LH before ovulation), then in the luteal phase the level of estradiol decreases slightly. During pregnancy, the content of estradiol in serum and plasma increases at the time of birth, and after birth it returns to normal on the 4th day. With age, women experience a decrease in estradiol concentrations. During postmenopause, the concentration of estradiol decreases to the level observed in men.
Indications for prescribing a blood test for estradiol:
- puberty disorder;
- diagnosis of menstrual irregularities and the possibility of having children in adult women (in combination with determination of LH, FSH);
- scanty menstruation (oligomenorrhea) or absence of menstruation (amenorrhea);
- lack of ovulation;
- infertility;
- premenstrual syndrome;
- discirculatory uterine bleeding (disturbing the cycle);
- hypogonadism (underdevelopment of the genital organs);
- osteoporosis (thinning of bone tissue in women);
- increased hair growth (hirsutism);
- assessment of the functioning of the fetoplacental complex in early pregnancy;
- signs of feminization in men.
On the eve of the estradiol analysis, it is imperative to exclude physical activity (sports training) and smoking. In women of reproductive age (from approximately 12-13 years of age and before the onset of menopause), the test is performed on days 4-7 of the menstrual cycle, unless other dates are indicated by the attending physician.
Normal estradiol levels:
- children under 11 years of age < 15 pg/ml;
- men 10-36 pg\ml;
- women: reproductive age 13-191 pg/ml, during menopause 11-95 pg/ml.
An increase in estradiol levels occurs with: hyperestrogenism (increased estrogen levels); endometrioid ovarian cysts; hormone-secreting ovarian tumor; estrogen-secreting testicular tumor in men; liver cirrhosis; taking anabolic steroids, estrogens (oral contraceptives).
A decrease in estradiol levels occurs with: hyperprolactinemia (increased prolactin levels); hypogonadism (underdevelopment of the genital organs); insufficiency of the luteal phase of the cycle; threat of miscarriage due to endocrine problems; intense physical activity in untrained women; significant weight loss; high carbohydrate, low fat diet; vegetarian diet; pregnancy, when a woman continues to smoke; chronic prostatitis in men; some specific diseases.
Progesterone
Progesterone is a steroid hormone that produces the corpus luteum of the ovaries in women and, during pregnancy, the placenta. In women, its concentration in the blood is much higher than in men. Progesterone is called the “pregnancy hormone” because it plays a decisive role in its normal progression.
If fertilization of the egg occurs, then progesterone inhibits the synthesis of gonadotropic hormones of the pituitary gland and inhibits ovulation, the corpus luteum does not resolve, but continues to synthesize the hormone up to 16 weeks, after which its synthesis continues in the placenta. If fertilization does not occur, the corpus luteum resolves after 12-14 days, the concentration of the hormone decreases and menstruation occurs.
Indications for prescribing a progesterone test:
- absence of menstruation;
- menstrual irregularities;
- infertility;
- dysfunctional uterine bleeding (associated with hormonal imbalance);
- assessment of the condition of the placenta in the second half of pregnancy;
- searching for the causes of true post-term pregnancy.
A blood test for progesterone is usually carried out on days 22-23 of the menstrual cycle, in the morning on an empty stomach. You are allowed to drink water. If blood is drawn during the day, the fasting period should be at least 6 hours, excluding fats on the previous day. When measuring rectal temperature, the concentration of progesterone is determined on the 5-7th day of its maximum rise. With an irregular menstrual cycle, the study is most often carried out several times.
Progesterone norm:
- children 1–10 years old 0.2–1.7 nmol/l;
- men over 10 years old 0.32-2.23 nmol/l;
- women over 10 years of age: follicular phase 0.32–2.23 nmol/l, ovulation 0.48–9.41 nmol/l, luteal phase 6.99–56.63 nmol/l, postmenopause <0.64 nmol/ l;
- pregnant women: first trimester 8.90-468.40 nmol/l, second trimester 71.50-303.10 nmol/l, third trimester 88.70-771.50 nmol/l.
Progesterone is increased during : pregnancy; corpus luteum cyst; lack of menstruation caused by various diseases; dysfunctional uterine bleeding (due to hormonal imbalance) with prolongation of the luteal phase; impaired placental maturation; renal failure; dysfunction of the adrenal glands; taking certain medications (corticotropin, ketoconazole, progesterone and its analogues, mifepristone, tamoxifen, etc.).
Progesterone is reduced with : absence of ovulation (primary and secondary amenorrhea, decreased secretion of progesterone in the 2nd phase of the menstrual cycle); insufficient function of the corpus luteum; chronic inflammation of the female genital organs; hyperestrogenia (increased estrogen levels); insufficient function of the corpus luteum and placenta (threat of miscarriage); intrauterine growth retardation; true post-term pregnancy; taking certain medications (ampicillin, carbamazepine, oral contraceptives, danazol, estriol, pravastatin, prostaglandin F2, etc.).
17-OH-progesterone (17-Oh-P, 17-hydroxyprogesterone)
17-OH progesterone is a steroid hormone produced in the adrenal glands, genitals and placenta. In the adrenal glands, 17-OH-progesterone is converted into cortisol.
An increase in 17-OH progesterone in the blood during the menstrual cycle coincides with an increase in the concentration of luteinizing hormone (LH), estradiol and progesterone. Also, the content of 17-OH increases during pregnancy.
During the first week after birth, 17-OH-progesterone levels fall, remain persistently low throughout childhood, and rise progressively to adult levels during puberty.
Typically, this test is prescribed when examining for:
- congenital adrenal hyperplasia;
- cycle disorders and infertility in women;
- increased hair growth in women (hirsutism);
- adrenal tumors.
The test is taken in the morning on an empty stomach; women are recommended to take it on the 5th day of the menstrual cycle.
Norm of 17-OH-progesterone:
- men 1.52-6.36 nmol/l;
- women over 14 years of age: follicular phase 1.24-8.24 nmol/l, ovulation 0.91-4.24 nmol/l, luteal phase 0.99-11.51 nmol/l, postmenopause 0.39-1, 55 nmol/l;
- pregnant women: I trimester 3.55-17.03 nmol/l, II trimester 3.55-20.00 nmol/l, III trimester 3.75-33.33 nmol/l.
17 Elevated progesterone indicates congenital adrenal hyperplasia or certain tumors of the adrenal glands or ovaries.
And reduced 17-on progesterone occurs with a deficiency of 17a-hydroxylase (it causes pseudohermaphroditism in boys) and Addison's disease (chronic insufficiency of the adrenal cortex).
Prolactin
Prolactin is a hormone that promotes the formation of sexual behavior. During pregnancy, prolactin is produced in the endometrium (the lining of the uterus), supports the existence of the corpus luteum and the production of progesterone, stimulates the growth and development of the mammary glands and the formation of milk.
Prolactin regulates water-salt metabolism, delaying the excretion of water and sodium by the kidneys, and stimulates the absorption of calcium. Other effects include stimulation of hair growth. Prolactin also regulates immunity.
During pregnancy (from the 8th week), prolactin levels increase, reaching a peak at 20-25 weeks, then decrease immediately before childbirth and increase again during breastfeeding.
A prolactin test is prescribed for:
- mastopathy;
- lack of ovulation (anovulation);
- scanty menstruation or its absence (oligomenorrhea, amenorrhea);
- infertility;
- dysfunctional uterine bleeding (hormonal imbalance);
- increased hair growth in women (hirsutism);
- comprehensive assessment of the functional state of the feto-placental complex;
- lactation disorders in the postpartum period (excessive or insufficient amount of milk);
- severe menopause;
- obesity;
- decreased libido and potency in men;
- enlarged mammary glands in men;
- osteoporosis (thinning of bone tissue in women).
One day before the prolactin analysis, sexual intercourse and heat exposure (sauna) should be avoided, and smoking 1 hour before. Since prolactin levels are greatly influenced by stressful situations, it is advisable to exclude factors that influence the research results: physical stress (running, climbing stairs), emotional arousal. Before the procedure, you should rest for 10-15 minutes and calm down.
Prolactin norms:
- children under 10 years old 91-526 mIU\l;
- men 105-540 mIU\l;
- women 67-726 mIU/l.
Elevated prolactin is called hyperprolactinemia. Hyperprolactinemia is the main cause of infertility and dysfunction of the gonads in men and women. An increase in prolactin levels in the blood may be one of the laboratory signs of pituitary dysfunction.
Reasons for increased prolactin : pregnancy, physical or emotional stress, heat exposure, breastfeeding; after breast surgery; polycystic ovary syndrome; various pathologies in the central nervous system; hypothyroidism (primary hypothyroidism); diseases of the hypothalamus; renal failure; cirrhosis of the liver; adrenal insufficiency and congenital adrenal dysfunction; estrogen-producing tumors; chest injuries; autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis, autoimmune thyroiditis, diffuse toxic goiter); hypovitaminosis B6.
Prolactin is reduced in true postterm pregnancy.
Analysis of follicle-stimulating hormone levels
A normal level of follicle-stimulating hormone is necessary to stimulate the maturation of germ cells, the synthesis and release of estrogens, ensuring the full maturation of follicles, and the onset of the ovulatory phase.
It is necessary to donate blood to check follicle-stimulating hormone levels on the fourth to sixth or nineteenth to twenty-first days of the cycle.
Elevated FSH can be observed with insufficient function of the gonads, dysfunctional uterine bleeding, menopausal disorders, renal failure, pituitary tumors, basophilic pituitary adenomas, endometrioid ovarian cysts, ovarian wasting syndromes, etc.
Also, the level of the hormone may increase during treatment with ketoconazole, levodopa, nafarelin, naloxone, pravastatin, tamoxifen, etc.
A decrease in hormone levels can be observed with secondary hypothalamic amenorrhea, hypogonadotropic hypogonadism, obesity, lead poisoning, Sheehan syndrome, hyperprolactinemia, treatment with steroids, carbamazepine, tamoxifen, growth hormone, valproic acid, gonadotropin-releasing hormone, etc.
Read: What to do if follicle-stimulating hormone is elevated in women?
Free testosterone
Free testosterone is the biologically active part of blood testosterone.
What are the indications for prescribing a blood test for free testosterone in women?
- infertility;
- acne;
- hirsutism;
- anovulation;
- amenorrhea;
- oligomenorrhea;
- dysfunctional uterine bleeding;
- miscarriage;
- polycystic ovary syndrome;
- uterine fibroids;
- endometriosis;
- breast neoplasms.
What preparation is required for a blood test for free testosterone?
At least 8 hours pass between the last meal and the blood draw (preferably at least 12 hours). Juice, tea, coffee (especially with sugar) are not allowed. You can drink water.
What are the deadlines for completing the analysis?
6 working days.
Growth hormone level
A normal level of somatotropic hormone is necessary for the full growth and development of all organs and systems. For children, hormone levels are extremely important during growth (normal bone development) and puberty.
Indications for conducting research on this hormone are carried out if the patient has delayed growth and sexual development, early sexual development, accelerated growth, osteoporosis, myasthenia gravis, alopecia, a tendency to hypoglycemic conditions, constant sweating, porphyria.
Increased production of pituitary growth hormone can be observed if the patient has:
- pituitary gigantism;
- acromegaly;
- dwarfism;
- chronic renal failure;
- hypoglycemia;
- decompensated forms of diabetes;
- alcoholism;
- post-traumatic conditions.
Also, hormone levels can increase when treated with insulin, corticotropin, glucagon, estrogens, norepinephrine, dopamine, propranolol, dopamine agonists, arginine, oral contraceptives, etc.
A decrease in the level of somatotropic hormone is observed with gopophyseal dwarfism, hypopituitarism, hyperfunction of the adrenal cortex, chronic sleep deficiency, postoperative interventions, hyperglycemia, treatment with progesterone, glucocorticosteroids, alpha-blockers, beta-adrenergic agonists, bromocriptine, corticosteroids, etc.
Types of hormonal drugs in tablets
There are currently two types of products that can be sold over the counter that are aimed at helping women solve their health problems. This:
- Progestin agents.
- Combined.
Secondly, it usually contains two types of hormones that every woman must have in her body - progesterone and estrogen. When exposed to such components, the function and process of ovulation are suppressed, the external tissues of the uterus are changed, which becomes the reason that the sperm that enters the woman during sexual intercourse cannot stick to its surface. This is the reason that the egg cannot be fertilized. Such factors are important in the body of women when they do not need to become pregnant. These drugs are also recommended for those who experience painful menstruation, as well as those who have had an ectopic pregnancy. It is also noted that after stopping the course of taking such medications, women experience a general rejuvenation of the body and, in some cases, the main causes of infertility are eliminated. Therefore, such courses of taking funds are attributed to those who want and cannot get pregnant.
Determination of prolactin levels
A normal level of prolactin is responsible for the normal development and function of the mammary glands, full lactation, normal labor, maintaining sexual desire, normalizing immune reactions, etc.
The highest level of prolactin is observed in the morning, and in the evening there is a physiological decrease in the level of the hormone.
Indications for testing for prolactin are the presence of galactorrhea, pain in the mammary glands, mastopathy, anovulation, oligomenorrhea, amenorrhea, infertility, dysfunctional bleeding from the uterus, obesity, osteoporosis, etc.
An increase in prolactin levels can be observed with:
- prolactinomas;
- hypothalamic tumors;
- pituitary adenomas;
- primary hypothyroidism;
- cirrhotic liver damage;
- estrogen-producing tumors;
- herpes zoster, hypovitaminosis B6;
- therapy with antihistamines, neuroleptics, estrogens, calcitonin, metoclopramide, etc.
A decrease in hormone levels can be observed with pituitary apoplexy, true post-term pregnancy, treatment with anticonvulsants, dopaminergic drugs, nifedipine, etc.
Main types of hormones
Hormones are divided into two main groups: estrogenic (female) and androgenic (male).
Female hormones are unique to the fair sex. They give women unique abilities to bear children. Estrogen also gives women a beautiful body and attractive appearance. At the same time, in the female body, in small concentrations, there are male hormones responsible for primary and secondary sexual characteristics.
Some hormones are responsible for sensitivity, emotions, and perception of everything around us. The correct balance of hormones provides a woman with harmony in her worldview, endowing her with instincts. With a lack of hormones, a woman’s health is impaired, diseases of varying severity appear, and years of life are reduced.
Estrogen
Estrogen is considered one of the main female hormones. Estrogen is a group of hormonal substances that are produced in the ovaries. This group of hormones is responsible for the structure of the figure: breasts, roundness of the hips. Estrogen is involved in the dynamics of body renewal at the cellular level, preserving the youth and beauty of skin and hair, affects the condition of blood vessels and fights cholesterol. The emotional outline and character are also influenced.
If there is not enough estrogen in the body, a woman can recognize this by the following signs:
- decreased sex drive;
- failure of the monthly cycle;
- brittle hair and weak nails;
- pale and dry facial skin;
- premature skin aging and wrinkles;
- male type vegetation;
- memory loss;
- migraine;
- hyperhidrosis.
What tests need to be taken during menopause?
Menopause is a physiological state of a woman in which estrogen production decreases, hormonal changes occur, and reproductive function is inhibited. In addition, such unpleasant companions as hot flashes, brittle bones, decreased libido and much more appear.
Only the doctor decides whether testing is necessary. He evaluates the obtained indicators along with the results of other survey methods.
Tests for estrogen and FSH can confirm the onset of menopause.
During this period, indicators of the hormones estrogen, FSH and LH are important for diagnosing and maintaining normal health. Low estrogen levels are an indicator for prescribing hormone replacement therapy. FSH is informative in determining the stage of menopause. To make an appointment with a specialized doctor and receive a free qualified consultation, use the service at https://45plus.rf/registration/.
Progesterone, gestagens and their analogues
Progesterone is a hormonal substance of the corpus luteum. It stimulates the appearance of changes in the uterine mucosa, which are characteristic of the secretory phase of the monthly cycle.
During pregnancy, it changes the mucous membrane to create optimal conditions for the development of a fertilized egg. Progesterone also significantly affects the reduction in contraction and excitability of smooth muscle fibers of the fallopian tubes and uterus, and has a stimulating effect on the excretory ducts of the mammary glands during lactation.
Reproductive dysfunction
About problems with the reproductive system they say:
- cycle disruption or complete absence of ovulation;
- it has been impossible to conceive a child for a long time;
- in case of successful conception, pregnancy is not systematically maintained;
- endometriosis.
If you can’t get pregnant for a long time, your progesterone, estrogen or prolactin levels may be too high or low. Before taking tests for these hormones, it is always necessary to inform the doctor whether you have taken medications and which ones, especially for various hormonal drugs.
In what cases are drugs from the gynecology and obstetrics section used?
This section of the site includes several broad groups of products. Each group contains a list of drugs that can help in a specific situation: - anti-inflammatory drugs. This category includes medications recommended for inflammatory processes of various natures. These can be infectious diseases, fungal infections, and so on; - contraceptives. Timely and correct intake of these medications is guaranteed to prevent pregnancy. At the same time, they are harmless to health, with the exception of cases of individual intolerance to the active components; - in case of hormonal imbalances. Such disorders are dangerous and can be expressed in the form of various pathologies. Taking these medications can bring your health back to normal; - various forms of mastopathy; - thrush, that is, fungal infections of the mucous membranes, skin, infections; - remedies for menopause. This period is characterized by a variety of manifestations. Gynecology medications will help normalize your well-being and overcome its consequences.
MORE ABOUT: At what age does menopause begin in women, at what age does menopause begin? What is the normal average age of menopause for Russian women?