What does blood INR show, the meaning of the abbreviation
INR stands for International Normalized Ratio. This study is carried out according to international standards. Blood clotting function is measured after a series of special procedures.
INR analysis is one of the most important research methods that determines the rate of blood clotting. Its purpose is determined by a single standard for all patients. Regardless of the location of the examination and the type of device, the result will always be identical.
The following data is used to determine information:
- Prothrombin time. Information is obtained through a blood clotting test. Average time (10-16 seconds).
- International Sensitivity Index (ISI) . Thromboplastin is produced by a large number of companies. Each of the produced substances contains a passport indicating their purity and sensitivity.
After the procedure, doctors prescribe treatment based on the results of the test to regulate blood flow functions. The frequency of analysis is also important. When performing an INR test once a month, the accuracy of treatment prescription is 50%, if once a decade - 80%.
Treatment is determined by the doctor individually for all patients, since each organism has its own reaction to the interaction of drugs and the dose of Warfarin. The examination is prescribed when taking vitamin K antagonists, which reduce the level of prothrombin levels in the blood.
INR analysis is regularly performed when:
- varicose veins;
An INR blood test can be prescribed for varicose veins.
- heart defects;
- thrombophlebitis;
- circulatory disorders in the brain area;
- acute coronary syndrome;
- atrial fibrillation.
Patients who have artificial filters installed to prevent blood clots from passing through a blood vessel are also eligible for testing.
Before the introduction of the INR, warfarin levels were determined using a prothrombin time (PTT) test. This method is characterized by low research cost, but does not provide accurate results. Devices often establish different ratios for the level of Warfarin in the blood of one patient.
What is INR and why is it prescribed?
Long-term use of anticoagulants should be accompanied by control of blood clotting.
It can be done in a laboratory by donating blood for analysis. INR (or international normalized ratio) is an important laboratory test that reflects the ratio of the patient's prothrombin time to the prothrombin time of a healthy person. This standardization of prothrombin indicators allowed doctors to bring different methods of studying the state of the blood coagulation system to a single, understandable and generally accepted indicator. This laboratory test produces consistent results that are consistent across different laboratories. The INR test has been approved by various international organizations and experts from the World Health Organization.
The introduction of the INR standard allowed for effective control of the quality and safety of therapy for patients prescribed blood thinners (for example, Warfarin, Sinkumar, Finilin). Anticoagulants are prescribed for a tendency to increased thrombus formation, which is observed in many pathologies: thromboembolic complications in coronary insufficiency, myocardial infarction, heart defects, pulmonary embolism, thrombosis, thrombophlebitis, etc.
An increase in INR values indicates a predisposition to bleeding, and the doctor decides to reduce the dosage of anticoagulants. When the values of this test decrease, the patient's risk of developing blood clots increases. Such indicators indicate the low effectiveness of blood thinning drugs, and the doctor decides to increase the dose.
When is a test ordered?
The examination is prescribed when taking vitamin K antagonists, which reduce the level of prothrombin levels in the blood.
INR analysis is regularly performed when:
- varicose veins;
- heart defects;
- thrombophlebitis;
- circulatory disorders in the brain area;
- acute coronary syndrome;
- atrial fibrillation.
Patients who have artificial filters installed to prevent blood clots from passing through a blood vessel are required to undergo testing every six months.
Before the introduction of INR, warfarin levels were determined using prothrombin time (PTT) analysis. This method is characterized by low research cost, but does not provide accurate results. Devices often establish different ratios for the level of Warfarin in the blood of one patient.
You should also consult a doctor if you have the following symptoms:
- intestinal infection;
- Changes in rest and working hours;
- constant bleeding from the nose and gums;
- climate change.
If you change your working hours, you need to take an INR blood test after a few days. Without treatment with anticoagulants and monitoring of blood counts, severe illness may develop.
Testing can be prescribed in 3 cases:
- For chronic illness. In this case, the test is prescribed to all patients taking Warfarin and similar coagulants.
- Single . This type of research is carried out under certain circumstances. These include surgical operations, pregnancy, and the study of diseases with impaired hemostasis.
- Personal expression of will. The procedure can be prescribed at the request of a person who wants to diagnose blood vessels. Most often, older people, men and women whose relatives were previously susceptible to heart attacks, are forced to carry out diagnostics.
Minor deviations from the norm can be caused by changes in climate and physical activity. If abnormalities in the blood plasma are detected in time, the functioning of the blood vessels can be restored by adjusting the diet or medications.
A frequently prescribed INR test does not mean that the patient’s health is worsening. This procedure may be prescribed to monitor indicators when changing the dosage of medications taken by the patient or diet.
Indications for use
Most often, it is recommended to donate blood for INR along with other indicators required to evaluate different parts of the homeostasis system. This procedure is indicated for diagnosing pathologies caused by increased thrombus formation, or, conversely, a tendency to severe bleeding. But most often it has to be prescribed to patients who are constantly taking anticoagulant drugs in order to keep the dosage of the drug under control.
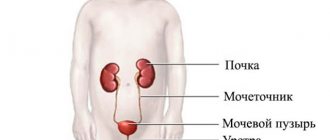
Another almost equally common indication is severe liver pathologies - hepatitis and cirrhosis. Considering that the liver is an organ responsible for the secretion of many enzymes that can influence the homeostasis system, disturbances in its function certainly affect coagulation.
For patients undergoing therapy with indirect antigoagulants (most often when taking Warfarin or drugs based on it), INR analysis is prescribed regularly, sometimes even every 7-10 days. This frequency may be necessary when dosage adjustments occur due to any changes in the health status of patients with factors leading to thrombus formation. For example, deep vein thrombosis, antiphospholipid syndrome or the presence of artificial valves.
Based on this indicator, the doctor can make adjustments to anticoagulants, as well as assess the patient’s condition. Almost all recommendations for selecting the dosage of anticoagulants are determined by the results of the INR and are generally accepted for different countries.
Preparing for analysis
An INR blood test is a study that requires compliance with certain rules before collecting biomaterial. You need to donate venous blood on an empty stomach. It is necessary to refuse food for more than 8 hours. Drink only water. It is strictly forbidden to drink alcohol the day before the procedure.
1 hour before the test, you need to avoid physical activity and smoking. It is not recommended for women to undergo the procedure during menstruation.
Moderate alcohol consumption has a positive effect on blood clotting, and the Warfarin index decreases accordingly. However, alcohol abuse will lead to an imbalance in INR levels. In small doses, alcohol can be taken together with anticoagulants.
In addition, alcoholic drinks lead to impaired coordination of a person, which increases the likelihood of falling and injury. This can be life-threatening for a patient taking coagulants. All of the above rules are subject to an exception in case of a critical situation and emergency care.
After passing an urgent analysis, a repeat procedure is prescribed, once the body’s performance has been restored. You can also control blood clotting at home. There are special devices for self-testing of plasma in the blood. The disadvantage of such devices is their high cost.
Where can the analysis be carried out and how is it done?
An INR test can be taken at any clinic, providing a referral from a doctor; today, there are even small portable devices for testing blood INR, which a person can use at home. This is very convenient, especially for people who are constantly on medications that will improve blood quality. Patients who use anticoagulants donate blood for INR every two weeks; there are a number of cases when blood has to be donated much more often.
This test is done by drawing blood from a peripheral vein. In order for the analysis results to be reliable, the patient must eliminate fatty foods and not drink alcoholic beverages during the day. Alcohol leads to an increase in blood clotting and a decrease in INR levels. If a person does not suffer from alcoholism, then the indicators are not reliable, because usually the body is not under the influence of alcohol.
As for alcohol addicts, they experience the opposite reaction - blood clotting decreases, and INR increases. If the patient takes medications to treat concomitant diseases, then the advisability of their use on the eve of the analysis is decided with the doctor on an individual basis. There are a number of medications that can affect the diagnostic procedure and distort the indicators. The analysis is done in the morning on an empty stomach, you cannot drink juices or coffee, it is advisable to drink only water.
The process of drawing blood is practically no different from the usual drawing of blood from a vein; the only difference may be in the amount of blood withdrawn. The doctor bandages the patient’s hand with a tourniquet so that the vein is better visible, disinfects the future puncture site and inserts the needle. The resulting blood is sent into a test tube and studied for several hours. The test is practically painless, but if you lose consciousness during similar tests, be sure to tell your doctor. He will prepare in advance a bottle of ammonia, which quickly brings consciousness to those who have fainted. A good tip for sensitive patients is to look the other way when the doctor takes blood.
Carrying out analysis
The procedure can be carried out in several ways:
- Portable device. Testing using special devices has been carried out since the 1990s. This device produces instant results. The blood is dipped onto the test strip and inserted into the device. The monitor will display the test result with all the exact data. This type of procedure is performed both in the hospital and at home.
- Laboratory research. At the moment, this testing method is more widely used. Blood is taken from a vein and sent for testing. After a certain time, a response comes with the indicators, and the specialist prescribes further treatment.
After completing a course of treatment in a hospital, the drug intake is not reduced. Warfarin is prescribed by a doctor for a long time, often for life. When conducting the analysis yourself, you need to know all the treatment standards for an increased or decreased coefficient. The patient can create a treatment schedule in advance by agreeing with his attending cardiologist.
It is more convenient to carry out INR testing yourself. However, most patients are afraid of this method or are simply not able to. Since most of the patients are elderly, they do not have the physical ability to attend training lectures to know how to use the device.
What is it for
It would seem, why carry out such complex calculations when there are actual indicators of blood clotting. The fact is that not everything is so simple. The features are:
- INR is an indicator purely for assessing the effectiveness and correctness of treatment with indirect anticoagulants (warfarin, syncumar, warfarex). The peculiarity of their action is that they affect only some blood clotting factors. None of the methods can so accurately show the state of this particular link of the blood coagulation system;
- Varying degrees of purification and sensitivity of thromboplastin used by laboratories;
- Standardized doses of indirect anticoagulants for certain types of thrombotic diseases worldwide.
What does this ultimately give? Specialists obtain a true indicator of blood plasma clotting. In this case, any errors, external influences and links of hemostasis that can affect its value are excluded.
Wherever the study was conducted, the resulting indicator would be identical and would be assessed equally in any medical institution in the world. Thus, it is possible to select the required dose of anticoagulants and monitor treatment.
To study INR you need blood from a vein
International norm INR
According to international standards, the INR index should be within 1.0. In case of pathologies or incorrect dosage of medications, the indicator will deviate from the norm. If the Warfarin index is increased, it is necessary to reassign the dosage of the drug. This can cause complications in the body and bleeding.
A low index is due to ineffective treatment, and therefore not blood thinning. With this treatment, the structure of blood vessels changes and blood clots form. Under these conditions, it is necessary to increase the dosage of coagulants.
INR in a laboratory blood test - what is it?
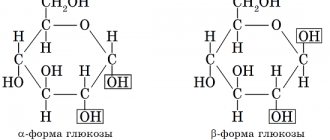
Laboratory blood testing allows you to determine many parameters indicating the presence or absence of signs of pathological processes. When a mixture of calcium and tissue thromboplastin is added to the plasma, the process of fibrin clot formation begins. The interval required for clot formation is called prothrombin time.
By dividing the measured prothrombin time by normal (control, standard) and raising the result to the power of the international sensitivity index (ISI), depending on the type of reagent used during the study, the INR value is obtained.
Norm for adult men and women, pregnant women
INR blood test is, first of all, accessible indicators about the functioning of the circulatory organs for each person. The standard ratio for adult men and women is similar. It varies from 0.8 to 1.2. If the result of the analysis falls within the established norm, then the person is healthy and has no pathological diseases.
During pregnancy, doctors pay increased attention to monitoring blood clotting, since during the period of bearing a child, the expectant mother’s body will change. In a pregnant woman, the INR index will be increased. This is considered normal. An index of more than 4.0 will be considered a violation of the body's functioning.
What determines the change in the index?
PTI is essentially the amount of prothrombin protein in the blood. If it is not enough, there is a risk of bleeding.
Reasons for reduced PTI:
- Vitamin K deficiency;
- Pathological changes in the liver;
- Lack of fibrinogen, another blood protein that is involved in clotting;
- DIC syndrome;
- Excessive amounts of heparin, a substance produced in the liver that regulates clotting;
- Amyloidosis is a disorder of protein metabolism, in which certain groups of proteins in combination with polysaccharides are deposited in organs and tissues;
- Nephrotic syndrome - kidney damage;
- Pancreatitis - inflammation of the pancreas;
- Neoplasms in the gallbladder;
- Leukemia and other diseases associated with blood clotting;
- Intestinal diseases and dysbiosis;
- Taking certain medications (coagulants);
- Congenital vascular anomalies;
- Pathologies in the thyroid gland.
An increase in the prothrombin index (hypercoagulation), which can cause blood clots and blockage of blood vessels.
The reasons may be as follows:
- Heredity;
- Congenital bleeding defects;
- Increased red blood cell count;
- Oncological diseases;
- Lack of heparin;
- Pregnancy (especially in the third trimester);
- Taking hormonal drugs and other medications (anticoagulants, coumarins, antibiotics, strong laxatives, barbiturates, corticosteroids).
Norm for children
For newborn children, the norm is considered to be a coefficient from 0.8 to 1.2. Below is a table with general indicators that a healthy child should have.
| Test | Standard positive indicators |
| Blood clotting time | 4 – 8 min. |
| Thrombin time | 27 – 33 min. |
| Prothrombin | 75 – 140% |
| Lupus coagulant | negative |
| Thrombotest | IV – V Art. |
| Prothrombin index | 72 – 103% |
| Fibrinogel | 6.0 – 12.0 µmol/l. |
| Activated recalcification time (ATR) | 55 – 72 sec. |
| Duke bleeding | less than 4 min. |
| Blood clot retraction | 28 – 38% |
Normal analysis values
The normal blood test for INR in adults does not depend on age or gender. For both men and women it varies from 0.85 to 1.25. On average, the INR should be equal to 1.
The normal values are slightly higher for those taking antiplatelet agents and anticoagulants. Their target value of the international normalized ratio is from 2 to 3. That is, for such patients, an increase in INR is physiological and does not indicate the presence of pathology of the coagulation system. But for people who do not take medications, any change in INR up or down indicates some kind of disease.
Below is a table of recommended INR norms depending on the patient’s condition.
| Recommended norms | States |
| From 0.85 to 1.25 | For people not taking blood thinners |
| From 1.5 to 2 | For patients with atrial fibrillation to prevent thrombosis |
| From 2 to 3 | For those who regularly take anticoagulants |
| From 3 to 4 | In the treatment of thromboembolism in peripheral arteries |
| From 3 to 4.5 | For the prevention of thrombosis after surgical interventions using prostheses |
Decoding the results
There are proteins in the blood that are defined as coagulation factors. These proteins are found in the liver and are easily affected by a drug such as Warfarin.
Before undergoing an INR blood test, the transcript should look like this:
| Cause | Indicators |
| Heart valve defects | 2.0-3.0 units. |
| Therapy of venous thrombosis | 2.0-3.0 units. |
| Treatment of pulmonary embolism | 2.0-3.0 units. |
| Vascular disease | 2.9-4.6 units. |
| Treatment of atrial fibrillation | 2.0-3.0 units. |
| Preliminary examination before surgery | 0.7-1.3 units. |
With the help of decoding, you can find out about the patient’s diseases.
These include:
- myocardial infarction;
- polycythemia;
- liver disease;
- poor absorption of fats in the gastrointestinal tract;
- vitamin K deficiency in children;
- chronic disease of the blood coagulation system;
- pre-infarction condition;
- malignant tumor.
If the indicators indicate a unit of 6 or more, then the patient needs urgent hospitalization. Otherwise, bleeding may occur.
In this situation, those patients who have diseases of the internal organs (kidneys, stomach, intestines) are at risk.
Blood INR: measurement, interpretation, norms
Many people hear the blood INR indicator. What does it mean? Why do doctors pay so much attention to him? How important is the determination of blood INR in medical practice? Read about this in our article.
What is blood INR?
The abbreviation INR blood stands for International Normalized Ratio . However, for a person not involved in medicine, this is an empty phrase. To understand the essence of blood INR and its role in the body, you need to take a short excursion into the physiology of the circulatory system.
The liquid state of blood in the human body is ensured by the coordinated work of the coagulation and anticoagulation systems. Fluidity, an important property of blood, is ensured by the anticoagulant system, and during bleeding, clotting ability becomes important. If the functioning of these systems is disrupted, a person experiences increased bleeding (for example, constant bleeding of the gums when brushing teeth, frequent nosebleeds) or a tendency to thrombosis - the formation of blood clots that can “pass” through vessels of larger diameter and “get stuck” in vessels of smaller diameter diameter It is dangerous when they enter the vessels of the heart and brain, because in these cases they lead to heart attacks and strokes and, as a result, to disability.
Normally, a healthy person is in a state of slight hypercoagulation, i.e. in a healthy body there is a slightly increased functioning of the coagulation system. However, in the absence of diseases, this feature does not lead to acute vascular accidents (heart attacks and strokes). In the presence of certain diseases (and first of all, the very common atrial fibrillation), the already existing tendency to thrombus formation sharply increases. Doctors have long noticed this feature, therefore, if a person has diseases accompanied by increased thrombus formation, they prescribe antithrombotic therapy (anticoagulants and antiplatelet agents) to prevent heart attacks and strokes. I would like to emphasize that these drugs are prescribed strictly by a doctor, since if used independently and uncontrolled, they can have serious life-threatening consequences. The severity of the effects of these drugs is closely related to the concept of blood INR.
Since antithrombotic drugs thin the blood by preventing blood clots, it is extremely important to monitor blood counts that reflect “how thin” the blood is. The main indicator is blood INR. The widely used indicators PTT (prothrombin time) and PTI (prothrombin index) are slowly receding into the background, because the method for determining these indicators involves the use of each specific laboratory with its own reagent with individual sensitivity. Therefore, results may vary greatly between laboratories. The APTT (activated partial thromboplastin time) indicator is determined during treatment with heparin (strictly in hospital conditions). The blood INR indicator was introduced into medical practice in order to somehow standardize the indicators of the blood coagulation system. It is not for nothing that the abbreviation INR blood stands for international normalized ratio.
The most common antithrombotic drug prescribed by doctors is warfarin. This is a well-studied medicine with an extensive evidence base. But it is precisely when using warfarin that it is so important to determine the blood INR. The normal range of blood INR values during warfarin treatment is 2.0-3.0. If the blood INR is less than 2.0, then the risk of ischemic stroke increases, but if the blood INR is more than 3.0, the risk of cerebral hemorrhage increases. The graph below clearly shows within which blood INR values the risks of dangerous complications are minimal (the so-called “therapeutic window”).
By the way, in a person who does not use warfarin, the blood INR value ranges from 0.85-1.35.
Where can I measure blood INR?
There are 3 main ways to measure blood INR. First: you go to the clinic to see your local physician, who, after the necessary examination, prescribes a blood test for you, which you take either in the same clinic for free, or in a private laboratory at your own expense (this depends on the capabilities of your clinic). The second method is almost the same, the only difference is that the blood INR test is done by a therapist in his office (provided that he has the appropriate equipment to carry out this analysis). The third way: purchase a small portable device for testing blood INR yourself. Of course, this device is not cheap, but with it you will be confident in your safety every day, especially since warfarin treatment is usually very long, and in some cases lifelong. Therefore, you purchase this device for long-term use, making a huge contribution to your health and quality of life.
It is important to remember that warfarin, like any medicine, can interact with other drugs and substances, changing its activity. This is important to consider, since in this case dose adjustment is necessary to maintain the blood INR within the range of 2.0-3.0 . Below is a table of warfarin interactions.
Spectrum of drug and food interactions of warfarin*
| Drugs that increase the activity of warfarin | Drugs that reduce the activity of warfarin | Dietary restrictions |
| Amiodarone, anabolic steroids, antabuse, acetaminophen, bispeptol, influenza vaccine, isoniazid, lovastatin, metronidazole, miconazole, norfloxacin, NSAIDs, omeprazole, ofloxacin, propronolol, salicylates, tamoxifen, tetracycline, thyroxine, phenytoin, fluconazole, fropafenone, quinine din, cimetidine, ciprofloxacin, erythromycin | Azathioprine, barbiturates, cabamazepine, cholestyramine, cyclosporine, griseofulvin, rifampicin, sucralfate | Alcohol, herbs, green tea, ginger, garlic and more |
*Plus resistance to warfarin
In conclusion, I would like to add that there are currently new oral anticoagulants (NOACs) that are easy to use and do not require the labor-intensive process of determining blood INR and other indicators. A significant negative side of these drugs is their high cost. The table below provides examples of new oral anticoagulants.
Laboratory monitoring of NOACs
| Controlled indicators | Dabigatran | Rivaroxaban | Apixaban |
| Platelets | No control needed | No control needed | No control needed |
| INR | No control needed | No control needed | No control needed |
| APTT | If it is increased by 2 or more times, the risk of bleeding increases | No control needed | No control needed |
| Prothrombin time | No control needed | Prolonged time may increase the risk of bleeding | No control needed |
Author: therapist A.V. Kosova
Increased INR value: reasons
An INR blood test with an increased coefficient is evidence of low blood clotting. This circumstance can lead to bleeding or hemorrhage. Even with minor damage to the skin, there will be high bleeding.
If the patient has diseases of the internal organs, for example, a liver ulcer, then heavy bleeding will begin in those places. Patients in such situations undergo urgent hospitalization and restoration of the coagulation system with the help of special drugs.
An elevated INR analysis usually corresponds to the following diseases:
- disease of the digestive system, which causes poor absorption of fats;
- insufficiency of proteins in blood plasma;
- copious blood transfusions;
- liver disease (cirrhosis, toxic damage, hepatitis C);
- treatment with Warfarin;
- heart muscle failure;
- lack of vitamin K in the body;
- pancreatic oncology;
- obstructed passage in the biliary tract (jaundice);
- excessive consumption of fatty foods and alcoholic beverages.
In what cases is an INR test prescribed?
One of the most reliable tests that allows us to draw a conclusion about the functioning of the blood coagulation system is prescribed for:
- conducting a preoperative examination, diagnosing diseases accompanied by the formation of blood clots, increased bleeding,
- taking coagulants, anticoagulants (to control/correct the dosage of drugs),
- hepatitis, cirrhosis, other severe liver diseases,
- antiphospholipid syndrome,
- heart defects,
- carrying out therapy for pulmonary embolism, venous thrombosis, heart attack,
- monitoring the patient’s condition after cardiac valve implantation,
- increased risk of postoperative complications associated with changes in blood clotting,
- regular nosebleeds, gum bleeding, hematomas, heavy, prolonged menstruation in women,
- pain, hardening, swelling of joint tissues, manifested during anticoagulant treatment,
- cancer diseases,
- pregnancy,
- hematuria, detection of blood in feces, vomit, sputum expelled by coughing.
Reduced value: reasons
There is also the opposite condition. It's called hypercoagulability. Under such circumstances, the blood begins to thicken, resulting in the formation of blood clots that can block the passage of blood to vital organs. This disorder leads to thromboembolism and infarction of the myocardium, intestines and spleen.
A decrease in INR values occurs when:
- infectious diseases with elevated body temperature;
- dehydration of the body;
- DIC syndrome;
- excess vitamin K;
- last stage of pregnancy;
- use of hormonal drugs;
- diarrhea and vomiting (after exceeding the dose of Warfarin).
Deviations of MHO from the norm
Increased rate
An increase in INR indicates:
- liver diseases,
- vitamin K deficiency,
- digestive disruptions (destabilization of bile transportation, fat absorption),
- congenital pathologies of the blood coagulation system,
- hemorrhagic disease,
- side effects after taking antibiotics, hormonal complexes, anabolic steroid drugs,
- presence of bleeding,
- exacerbation of hypertension,
- polycythemia,
- pre-infarction or infarction condition,
- progressive oncology,
- the need to change the dosage of Warfarin and other medications that thin the blood.
With an INR value greater than 6, immediate therapeutic measures are required due to the high risk of bleeding.
Reduced INR
A decrease in INR may be caused by:
- the use of certain subtypes (glucocorticoids, diuretics, contraceptives, anticonvulsants) of drugs,
- increased antithrombin (III) level,
- change in hematocrit,
- vein thrombosis, thromboembolic complications,
- consequences of childbirth, operations, traumatic injuries,
- severe dysfunction of the immune system,
- excess vitamin K in the body,
- cancer diseases,
- DIC syndrome,
- drawing blood from a catheter installed in the central vein,
- insufficient filling of the test tube with biomaterial or insufficient thoroughness of mixing the blood with the anticoagulant, ingress of additional substances into the biological fluid under study that distort the results,
- violation of the conditions (duration, temperature) of plasma storage.
If the calculated INR value is below 0.5, the patient needs medical attention, since when the level of blood clotting increases to critical values, the resulting blood clots can cause irreversible circulatory disorders.
If the INR value is increased or decreased, repeated examinations are required to exclude the factor of laboratory error.
You can share your opinion about the article using the form below. We are waiting for your comments.
Which doctor solves the problem of low and high INR
The selection of the Warfarin dosage and the entire period of treatment and restoration of the circulatory system is carried out by a cardiologist. Your doctor will monitor your test results and schedule the test. Depending on changes in blood plasma, the dosage of the necessary drugs may be reassigned.
The cardiologist can also change the frequency of the INR blood test based on the latest readings. If the results are poor, blood plasma testing will be prescribed more often (once a week). In the future, with the improvement and normalization of blood circulation in the vessels, the analysis can be performed once every 15 days and up to 1 month.
Preparation and delivery of analysis
The preparatory process for conducting an INR analysis is not labor-intensive or time-consuming, but in order to get a reliable result, it is necessary to take into account some points. Firstly, you should not donate blood after intense physical activity, physiotherapy, massage, intravenous infusions or intramuscular injections, as this may affect the indicator.
Secondly, if the patient is taking anticoagulants, then the entire daily dose should be consumed no later than 16.00-17.00 on the evening before the examination. We should not forget that blood for INR is taken on an empty stomach, as for general or biochemical analysis, so at least 8 hours must pass after eating. At the same time, it is not correct to go hungry for more than 14 hours - this can also lead to changes in blood composition.
Normal INR values
To perform the analysis, biomaterial is taken from the cubital vein, as for most studies involving blood. Then the resulting liquid is mixed with a preservative in a test tube (usually citrate), the serum is separated from the cell mass and pure plasma is used for the diagnosis itself.
Reference! The action of citrate is aimed at binding calcium ions, which prevents blood clotting.
The laboratory then adds calcium to the serum, which neutralizes the preservative, and thromboplastin. Then the time spent on coagulation of pure serum is determined. This is PTV. Upon completion of all analytical tests, a mathematical calculation of the INR is performed. Some diagnostic laboratories use more modern methods of studying the quality of coagulation, for example, the PTT analysis according to Quick.
When performing it, dilution of the subject's serum biomaterial is carried out several times, and the entire procedure takes no more than one day. If the analysis result is required very quickly, then for an additional fee in some laboratories it is done and deciphered within 1-2 hours.
When anticoagulation therapy using indirect anticoagulation drugs, the patient should undergo an INR test at least once every 15-20 days. And after choosing the appropriate dosage and normalizing the patient’s condition, the analysis will be prescribed less frequently, approximately once every 6-8 weeks.
How to level up
INR blood test is a series of tests that determine the performance of all vital organs. If the index is low, cardiologists adjust, first of all, the dosage of Warfarin. They are also prescribed a special diet. The main requirement is to avoid foods containing vitamin K, as it helps lower the index.
The largest amount of this vitamin is found in green tea, lettuce, liver, spinach, cauliflower and white cabbage, green peas and brewed black tea. You should reduce your consumption of mayonnaise, apples and cucumbers.
When a doctor prescribes Warfarin, for greater effect, you can consume a number of products that promote an accelerated increase in levels when interacting with the drug. These include fish oil, garlic and red currants.
What is blood clotting
Blood clotting is one of the most important indicators of the homeostasis system. It is responsible for the process of stopping bleeding when the vascular wall is damaged. This system consists of numerous coagulation factors. They, interacting with each other in a very complex way, together make up the blood coagulation system in the human body.
The process of blood coagulation is a complex proenzyme-enzyme cascade of interaction between factors. The process is characterized by clear stages. In it, proenzymes gain the ability to activate the following coagulation factors.
Schematically, this process is divided into the following phases:
- Activation is a complex of cascade reactions. As they pass, prothrombinase is formed and thrombin is formed from prothrombin.
- Coagulation is the process of formation of fibrin protein from fibrinogen.
- Retraction is the process of obtaining a compacted fibrin clot.
The mechanism of operation of the coagulation system includes four components.
These include:
- Vascular - represents active compression of the vessel with a subsequent reduction in blood flow at the site of damage. This prevents blood loss.
- Cellular - it is characterized by the transition of platelets to a functional state. They begin to move, stick to each other and stick to the walls of the damaged vessel. Both previous processes trigger, in turn, the third component of the coagulation system.
- Plasmatic - this stage is characterized by the formation of a mesh structure from fibrin threads under the influence of activating substances. The fibrin network holds the formed elements, resisting blood pressure.
- Fibrinolysis - after the healing of the vessel wall, the process of eliminating the fibrin clot occurs. He has already completed his task.
Blood coagulation is a rather complex and multi-stage, cascade process. Its violation can happen at any stage.
How to lower the INR index
An increased level of Warfarin in the blood has a number of consequences if the diet is not followed or the drug dosage is incorrect. The patient is prescribed a special diet to restore the balance of the blood vessels.
The table will provide a list of recommended products:
| Product | Condition |
| Meat | low fat composition |
| Fruits | high sugar content |
| Confectionery | low fat composition |
| Cereal porridge | |
| Flour products | whole wheat flour |
| Bread or crispbread | stale or dried out |
| Vegetables | |
| Baked potatoes | without adding vegetable oil |
| Boiled egg | no more than 1 per day |
| Milk products | no more than 1% fat content |
Deviations
In a healthy person, the prothrombin index should always be normal - from 78 to 140%. This is a relatively constant indicator, so if there is a deviation from the norm, diagnostics and identification of the causes are required.
After studying the results, a number of conclusions can be drawn:
- Assess the risk of heart attack, stroke and vein thrombosis due to varicose veins;
- Assess the functioning of the digestive system;
- Assume the presence of a tumor in the pancreas, liver and other organs;
- Determine the effectiveness of medications;
- Determine vitamin K deficiency or deficiency.
A deviation from the norm must be treated or further examination must be carried out to determine the cause.
Consequences of high and low INR
INR blood test is an indication of the results of Warfarin indexation in the blood. If it deviates from the norm, the patient is prescribed a dosage adjustment of the drug and a change in diet.
If the regimen and dosage are not followed, harmful consequences may occur:
- formation of blood clots in blood vessels;
- increasing liver disease;
- pulmonary embolism.
As the level increases above 6, the likelihood of external and internal bleeding increases. Such phenomena can only be eliminated with medical help. If the values are too high, immediate hospitalization of the patient is required.
When a person is not susceptible to blood diseases, he does not need to undergo an INR blood test. However, experts recommend being examined once every 18 months. These measures will help detect disturbances in the functioning of the circulatory system and warn of a possible disease.
Types of analyzes
The coagulation system is very complex. To evaluate its performance, it is necessary to examine many indicators. Therefore, there are a huge number of clinical tests to evaluate this work. Their purpose is not easy to understand.
All clinical tests for the diagnosis of coagulation are divided into two large groups.
According to the classification of research, all methods are divided into:
- global (integral, general) studies;
- local (specific) studies.
Global tests reflect the result of the entire convolution cascade of reactions. They make it possible to identify the picture of ongoing disorders in the hematopoietic system. This group of tests reveals the tendency of the coagulation system to hyper- or hypocoagulation.
The integral group of tests includes:
- coagulation time of whole blood (Morawitz, Mas-Magro, Sukharev methods);
- test to determine thrombodynamics;
- thromboelastography;
- thrombin generation test (endogenous thrombin potential, thrombin potential).
Local tests are used to assess the functioning of individual parts of the blood coagulation cascade. They can also evaluate the performance of individual coagulation factors. These methods make it possible to very accurately determine the problem in the operation of the coagulation system down to each individual segment of the cascade.
Local tests include the following research methods:
- partial activated thromboplastin time (aPTT);
- prothrombin time study (prothrombin test, INR, PT);
- specialized reactions to detect a decrease in the concentration of individual factors.
In addition to the tests described above, clotting methods are also distinguished. They determine the time from the moment the reagent is added until the formation of a fibrin clot in a portion of the patient’s plasma.
Table of average cost of research in Moscow, St. Petersburg, regions
Currently, there are a large number of medical institutions capable of performing INR blood tests. Each of them has its own pricing policy and provision of services. The table will show the average cost for undergoing the procedure in different regions of the Russian Federation.
| Region of the Russian Federation | average cost |
| Moscow | 350 rub. |
| Saint Petersburg | 340 rub. |
| Samara | 310 rub. |
| Kemerovo | 280 rub. |
| Pskov | 255 rub. |
| Ekaterinburg | 270 rub. |
| Nizhny Novgorod | 290 rub. |
| Kazan | 330 rub. |
| Belgorod | 300 rub. |
| Rostov | 285 rub. |
| Tyumen | 300 rub. |
| Tambov | 260 rub. |
| Kaliningrad | 270 rub. |
| Volgograd | 280 rub. |
| Saransk | 265 rub. |
| Krasnodar | 300 rub. |
| Arkhangelsk | 300 rub. |
Since the average price for performing an INR analysis is indicated, this means that fluctuations in the cost of undergoing the procedure in one region can differ dramatically, taking into account the lowest and highest prices.
In what cases is it prescribed?
The PTI blood test is prescribed for pregnant women. The frequency is determined by the attending physician.
Regular studies are also required:
- When taking coagulants;
- With cirrhosis of the liver;
- For oncological diseases;
- For thromboembolism;
- For hepatitis;
- With congenital abnormalities of blood clotting (leukemia);
- For varicose veins;
- For disorders of the heart and blood vessels;
- For gynecological diseases;
- For gastrointestinal diseases associated with vitamin K deficiency;
- For autoimmune disorders;
- For atherosclerosis;
- With antiphospholipid syndrome;
- For an upcoming operation;
- After a heart transplant, with an artificial heart valve;
- After a stroke and heart attack;
- When taking hormonal drugs, including oral contraceptives;
- In people over 50 years of age.
A PTI analysis is required before surgery and during pregnancy.
Reviews from doctors about the reliability of the study
Blood tests are performed with special devices. Doctors assure patients of the reliability of the results and the rare errors of the testing apparatus. For patients with chronic blood diseases, experts recommend creating an individual table that will show the diet, its types, and the correct dosage.
This will allow the patient to adhere to the regimen established by the doctor and not deviate from the schedule.
Compliance with all the rules and the correct dosage of Warfarin prescribed by your doctor will lead to the improvement and stabilization of blood vessels. Taking an INR blood test will help you avoid pathologies in the body and normalize its functioning.
After consulting a doctor, you can also resort to traditional medicine. Nettle, for example, is used to stop bleeding, as it thickens the blood well. Decoctions of ginger and cinnamon, on the contrary, thin the blood and increase blood circulation.
Doctors treating thrombosis and similar diseases recommend that absolutely all people undergo an INR blood test. If this procedure is mandatory for patients with chronic diseases, then for other people, cardiologists recommend testing once every 2 years. This will make it possible to determine the pathology in the embryo and prevent its further development.
Author of the article: Denis Balaykin
Article design: Oleg Lozinsky
Taking anticoagulants and coagulogram
Anticoagulants are drugs that prevent coagulation. These drugs have different mechanisms of action.
There are direct and indirect anticoagulants:
- Straight - usually used in hospitals. Heparin belongs to this group.
- Indirect anticoagulants are used long-term for continuous therapy. They are called thus due to the fact that it is not the active substance itself that slows down coagulation, but its indirect action. The most commonly prescribed drug, Warfarin, belongs to the group of indirect anticoagulants.
The selection of anticoagulants is carried out under the control of INR; the norms for this value when taking anticoagulants are given in the table below.
| Pathology | INR norm when corrected with anticoagulants |
| Prevention of deep vein thrombosis (postoperative) | 2,0—3,0 |
| Prevention for valve disease | 2,0—3,0 |
| Myocardial infarction (prevention of venous thromboembolism) | 2.0—3.0 (individually it is possible to increase to 4.5) |
| Treatment of pulmonary embolism | 2,0—3,0 |
| Treatment of venous thrombosis | 2,0—3,0 |
| Treatment of arterial thromboembolism, recurrent systemic embolism | 3,0—4,0 |
| Prevention after insertion of mechanical valve prostheses | 3,0—4,5 |
| Prevention of parietal thrombosis in atrial fibrillation | 1,5—2,0 |
Monitoring the adequacy of the dosage of anticoagulants is carried out using INR.
When prescribing anticoagulants, INR is tested before starting therapy. Then - every 2-3 days, then - once a week. If an acceptable INR value is achieved (on average 2.0-3.0), then the INR is then determined monthly. If the INR values are stable, then it is examined once every 3 months.
Taking anticoagulant drugs also affects other coagulation parameters.
Coagulants affect the following coagulogram parameters:
- thrombin time increases;
- prothrombin time increases;
- activated partial thromboplastin time increases 1.5-2.5 times.
Anticoagulant therapy requires strict monitoring of blood coagulation status. To achieve the required clinical effect, it is important to select dosages individually for each patient.
If insufficient dosage is used, it is impossible to obtain the desired clinical effect. If the dosage is too high, it is life-threatening for the patient.
Foods that increase INR while taking warfarin
The INR is always assessed together with the prothrombin level. This study is not carried out in isolation (INR is calculated based on the patient’s prothrombin level). Therefore, the reasons for changes in the level of INR in the blood should be interpreted together with the level of prothrombin.
The INR level is inversely proportional to the prothrombin level and the amount of blood clotting factors (the higher the INR level, the lower the prothrombin level).
Most often, the INR is elevated when:
- liver diseases;
- consumption coagulopathies (conditions in which, against the background of active thrombus formation, blood clotting decreases due to depletion of blood clotting factors);
- fibrinogen and/or prothrombin deficiency;
- vitamin K deficiency.
A low INR level is observed in patients with an increased risk of blood clots, the early stage of thrombosis. Also, a decrease in INR levels can be observed in the last trimester of pregnancy.
An increase in the level of prothrombin according to Quick is observed with:
- tendency to thrombosis, development of thromboembolic conditions, myocardial infarction, pre-infarction conditions, increased blood viscosity due to hypohydration, with hyperglobulinemia;
- taking certain medications: drugs that can inhibit the effect of coumarin (vitamin K drugs, barbiturates), corticosteroids, oral tablet contraceptives, meprobamate drugs, antihistamines;
- polycythemia;
- the presence of malignant neoplasms in the patient.
All drug treatment and diet must be prescribed by the attending physician. Self-medication is unacceptable and can cause irreparable harm to health. Patients taking warfarin do not require a special diet. In this regard, the diet depends on the underlying disease.
Most often, patients are advised to limit the consumption of alcoholic beverages, red meat, fatty, fried meats, and also increase the consumption of fruits, vegetables, lean fish, nuts and greens.
Note: High Iron Foods Label
For what purpose do they donate blood to study this protein?
Drawing conclusions from the results of such an analysis, a qualified physician can determine:
- Possible heart attack or pre-stroke condition,
- The appearance of blood clots, with varicose veins,
- Does a specific organism need vitamin K?
- Are there any abnormalities in liver function?
- What is the state of the blood levels responsible for clotting?
This analysis is especially necessary during imminent surgery. Since doctors need to take such features into account and know the recovery time after injuries.
PTI indicators indicate a disorder in blood clotting, which leads to bleeding or the formation of blood clots. The last two factors can lead to serious complications.
Reasons for decreased INR
An increase in the international normalized ratio indicates insufficient blood clotting and increased fluidity. This condition requires immediate action, as massive bleeding may develop. An increase in INR to 6 is considered critical.
If a patient has an elevated INR blood test, this indicates one of the following diseases:
- congenital insufficiency of the blood coagulation system (hemophilia, idiopathic thrombocytopenic purpura);
- reduced amount of vitamin K (hemorrhagic disease of the newborn);
- severe liver disease with the development of liver failure;
- adverse reaction to taking certain medications: anti-gout, antibiotics, hormonal drugs.
A decrease in the results of a blood test for INR in women and men below 0.85 indicates the presence of the following pathological conditions:
- change in hematocrit level;
- an increase in the concentration of antithrombin III in the blood;
- side effects when taking medications: diuretics, oral contraceptives, anticonvulsants, corticosteroids;
- blood was taken for analysis from the central catheter.
It is also possible for indicators to decrease if the technique of performing a blood test for INR is violated. For example, if the blood plasma was at a temperature of 4 ° C for a longer time than required.
A decrease in INR levels indicates hypercoagulation, that is, an increased tendency to form blood clots or emboli.
What is prothrombin itself?
Prothrombin is a special protein found in the blood and formed in the liver under the influence of vitamin K.
If the amount of vitamin K is insufficient, prothrombin levels drop.
Prothrombin is the parent of thrombin, which affects thrombosis. This protein directly affects the increase or decrease in blood clotting.
To study PTI, it is necessary to observe the rate of plasma coagulation for each person individually, since the indicator depends on the person. The ratio of time between these two values will be the prothrombin index.
If PTI is studied using the Quick method, then the functioning of prothrombin is detected according to the schedule. This graph gives more accuracy due to the fact that it is built on the basis of marks from the results of studies of plasma coagulation at dilutions of different concentrations.
Kwik analysis results are displayed as a graph
IPT always consists of analyzing a coagulogram, which is a comprehensive blood test for clotting.
How to take a correct coagulogram?
When taking a coagulogram, like any other analysis, to obtain an absolutely accurate result, there are recommendations:
- Come for analysis exclusively on an empty stomach, stopping eating at least 8 hours before the test,
- If you want to drink, you are allowed to drink only clean drinking water without gas. Before delivery, you need to drink 200-250 ml of water (1 glass),
- No later than 24 hours in advance, do not smoke cigarettes, or quit this habit no later than 2 hours in advance,
- Don't worry before donating blood. Coagulability may increase due to stressful conditions and experiences,
- When using any medications, you must notify your doctor.
Taking a blood test for prothrombin
It is difficult for a person who does not understand the abbreviation INR to make out this combination of letters. Moreover, many believe that such an analysis after deciphering the first letters will not give anyone any explanation. In fact, an INR blood test is a specific blood test to determine the amount of prothrombin in the body. As mentioned above, prothrombin is a complex protein. In addition, this element allows you to assess how the patient’s blood clotting process proceeds. Thanks to this analysis, doctors assess the condition of the liver and gastrointestinal tract, and also identify pathological processes in these organs, if any. A laboratory test to determine prothrombin in humans is considered the most necessary test that is aimed at assessing coagulation. INR results are presented in several forms:
- PTT is the period during which a drop of blood clots - this phenomenon is measured in seconds;
- determination of prothrombin according to Quick is the ratio of the activity of the element, which is measured as a percentage;
- PTI is the ratio of PTI of a sick person in relation to a healthy one;
- The INR is a comparison of people's PT to the prothrombin period.
Normal PTI values in a person who does not suffer from diseases of the internal organs are approximately 80-100 units. If the patient takes Warfarin during the test, a drug that can reduce blood clotting, then the PTI values are reduced to 24-42.
At the moment, several methods have been developed for determining PTI indicators, but they do not give reliable results, especially if the analyzes were carried out in different diagnostic centers.
Most doctors prescribe INR to patients, since such blood biochemistry shows the most correct and truthful result, regardless of the laboratory conditions where it is carried out.
PTI during pregnancy: normal
During pregnancy, all women are required to undergo a coagulation test. It includes:
- PTI (prothrombin index).
- INR (international normalized ratio).
- APTT (activated partial thromboplastin time).
- Fibrinogen.
All these parameters are extremely important. Thus, an increase in PTI in the last stages of pregnancy to 150% or higher may indicate the risk of placental abruption. And if this indicator decreases before childbirth below 80%, there is a risk of bleeding during childbirth or in the postpartum period. Thus, it is especially important to evaluate the coagulation system late in pregnancy. To do this, a PTI analysis is performed. The norm of this indicator during pregnancy varies from 90 to 120%.
INR test
Analysis for the normalized ratio has a number of important features:
- The resulting figures are important values for assessing the correctness and effectiveness of the use of blood thinning drugs, especially indirect anticoagulants (Warfarin, Sinkumar, etc.). The specificity of the work of these medications is to influence only individual coagulation factors. And only an INR study can give accurate indicators of the state of these specific elements of the coagulation system.
- The result obtained depends on how pure and sensitive the thromboplastin is used.
- Diagnostics can show the effectiveness of indirect coagulants.
Thus, the INR analysis allows doctors to find out the exact indicators of plasma coagulation. This method makes it possible to almost completely eliminate the occurrence of errors and the impact of any internal or external factors on the result. The analysis technique is standardized, and its indicators will be equally accurate in any laboratory. Thanks to these properties, an INR test allows specialists to correctly select the dose of an anticoagulant drug and “keep their finger on the pulse”, monitoring the progress of treatment.
This testing is carried out only for those patients who are taking a course of indirect anticoagulants. To monitor the effectiveness of the drug over time, tests are taken once every two to three weeks, although, as prescribed by the doctor, this can be done more often. In each specific case, the frequency is selected based on the existing pathology, the patient’s condition and the duration of treatment.
If the result of the INR study is stable, then the period is increased to once a month. Blood is taken for analysis on an empty stomach, taking a sample from a peripheral vein.
Interpretation of INR analysis: decrease
A decrease in values below one indicates the possible presence of the following pathologies or laboratory errors:
- The presence of an increase or decrease in hematocrit.
- Increased amount of antithrombin III.
- Adverse reactions due to the use of contraceptives, glucocorticoids, anticonvulsants or diuretics.
- In the event that blood was drawn for research from a catheter located in the central vein.
A change in the INR in patients who took Warfarin or any other anticoagulants indicates the need for dosage adjustment of these drugs.
External bleeding in such cases can be provoked by even minimal mechanical stress or trauma. As for internal bleeding, they are caused (cavitary, uterine, gastric and others) by any disease and physiological process (for example, menstruation).
In the presence of hypercoagulability, the patient has an increased risk of blood clots and a serious complication (for example, thrombosis) is likely to occur. In such cases, the dosage of anticoagulants is increased.
We continue to consider the interpretation of INR in a blood test in adults and the norm.
Self-measurement of INR: what you need to know
If the patient independently monitors the INR at home, he has two options to monitor the effectiveness of treatment:
- self-monitoring: after receiving results that differ from the norm, the patient notifies his cardiologist;
- self-management: depending on the data received, the patient himself changes the dose of Warfarin depending on the schedule previously developed and available at home.
With this control method, the patient must:
- be able to use the device and test strips;
- know how to maintain the desired INR values;
- remember the influence of medications and dietary habits on INR values.
It is best to choose a self-control strategy. People using this method receive an effective and safe dose of Warfarin 70% of the time. The method is more convenient and does not require a visit to the doctor. Such patients are 2 times more likely to avoid a heart attack or stroke than with a laboratory test once a month.
However, self-monitoring is not suitable for all patients. More than 68% of patients do not agree to such a procedure at all. Of those who agreed to measure their INR themselves, about a quarter were unable to complete this task. The main reasons for failure:
- physical limitations, such as poor vision;
- inability to attend training sessions;
- inability to learn how to use the device;
- device failure.
Although self-monitoring is an effective method for measuring INR and regulating blood clotting, before purchasing such a device, you should consult with a cardiologist to determine whether it is suitable for a given patient.
Coagulogram - what kind of analysis is it, correct interpretation of the results
Why do you take a detailed hemotest?
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Blood circulates through the vessels in liquid form, but when they are damaged, it thickens and forms blood clots to close the wound and allow the damaged tissue to recover. This ability is controlled by the hemostasis system. Coagulation occurs in three stages:
- When damaged, the inner surface of blood vessels triggers thrombus formation processes. The walls of the blood vessels spasm to reduce blood loss.
- Platelets are produced in the bone marrow. Which are plates that rush to the damaged area and stick together to close the wound.
- The liver produces 15 clotting factors (mostly enzymes). Reacting with each other, they form a fibrin clot, which finally stops bleeding.
A hemostasiogram shows the state of hemostasis. Prescribed in the following cases:
- Before any operations to determine clotting time;
- during pregnancy before any type of delivery;
- pathologies of the hematopoietic organs and control of their treatment;
- varicose veins;
- liver diseases;
- for cardiovascular diseases with a high risk of blood clots;
- when taking certain medications;
- blood loss of various nature;
- chronic foci of inflammation in the body.
Before surgery, the clotting time is determined to avoid blood loss. And in case of heart disease, it is important to prevent thickening in order to prevent heart attack, stroke or thrombosis.
Watch an educational video animation about the human hemostasis system:
Preparing for such a procedure, how to take it correctly
To obtain reliable results, it is important to submit the examination material correctly.
To do this you need to remember:
- Blood sampling is carried out in the morning on an empty stomach. The last meal should be at least 8 hours before the test (preferably 12). The day before you should not drink spicy, smoked, fatty or alcoholic drinks.
- You should not smoke before taking the test.
- You can drink. But only clean water.
- Some medications affect clotting and may make the results unreliable. You must provide your doctor with a list of medications you are taking. If possible, you should stop taking medications 2 days before the examination.
The collection is made from a vein without using a tourniquet. It is important that the material being tested is sterile. The result is ready in 1–2 days.
Hemostasiogram is one of the most difficult studies. To make a correct diagnosis, it is advisable to also perform a general blood test (what does it include?). Then the picture will be complete.
Violations of the rules for collecting material for analysis, recent blood transfusions, and tissue from capillary blood entering the collected sample can affect the result.
What does a blood clotting test show?
A hemostasiogram may include a different set of indicators. It all depends on the purpose of the research. The doctor indicates the necessary parameters in each specific case.
Typically, as a result of a hemostasiogram, the following is determined:
- Prothrombin level. Prothrombin is a complex protein. Its quantity shows the state of the hemostatic system as a whole. When the norm increases, there is a tendency to thrombus formation, and when it decreases, to bleeding.
- Prothrombin index. The percentage of the patient's clotting time relative to the normal value.
- INR is the international normalized ratio of the prothrombin time of the test material to the average value of this time. If the norm is exceeded, a person is prone to bleeding; if it is lower, the person is prone to the formation of blood clots.
- APTT – activated partial thromboplastin time. Time to form a blood clot. Often studied under the influence of various factors.
- Fibrinogen. One of the main proteins in the formation of a clot during coagulation. Increased levels are typical during inflammatory processes. May indicate disorders in the cardiovascular system. A low amount of protein is observed with liver problems and a tendency to bleeding.
- TV – Thrombin time. Duration of the final stage of coagulation.
- Antithrombin III. Reduces clotting.
- Platelet level.
- Lupus anticoagulant. Normally absent. The presence may indicate autoimmune processes in the body.
- D-dimer. Controls the process of thrombus formation. A rapid increase in this parameter can occur with diabetes, blood and kidney diseases.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
You can learn more useful information about taking this test for women’s health during childbearing years from the video:
Normal indicators and deviations in children and adults in the table
We present to your attention a table with normal blood test results for a coagulogram and possible causes of changes in hemostasis.
| Coagulogram indicator | Normal for children 3–14 years old | Normal in adults | Indicators are below normal | Indicators are above normal |
| Lee-White clotting time, min. | 5–10 | Hemorrhagic or anaphylactic shock. | Inflammation, burns, pregnancy, intoxication, kidney and liver diseases. | |
| Bleeding time (according to Duke), min. | 2–4 | – | Lack of platelets, alcohol intoxication, blood diseases. | |
| Prothrombin time (PT) according to Quick, sec. | 13–16 | 11–15 | – | Risk of blood clots |
| Prothrombin index (PTI), % | 70–100 | 73–122 | Liver diseases, thrombosis, pregnancy and childbirth. | Vitamin K deficiency, exposure to certain medications. |
| INR | 0,82–1,12 | Thrombosis. | Pathological processes of the liver and kidneys, lack of vitamin K, taking certain medications. | |
| APTT, sec. | 24–35 | 22,5–32,5 | Increased clotting, improper collection of material for analysis. | Reduced coagulability, liver and kidney pathologies, vitamin K deficiency. |
| Thrombin time, sec. | 10–16 | 14–21 | Taking certain medications. | Reduced fibrinogen, autoimmune disorders, liver disease |
| Fibrinogen, g/l | 1,7–3,5 | 2,7–4,013 | Liver diseases, consequences of bleeding, blood diseases. | Inflammatory processes, malignant formations, menstruation, pregnancy, heart disease, burns. |
| Antithrombin III, % | 80–120 | 75–125 | Ischemia, thrombosis, sepsis, congenital pathologies, last trimester of pregnancy. | Severe inflammatory processes, lack of vitamin K, hepatitis. |
| Lupus anticoagulant | negative | – | Autoimmune processes. | |
| D-dimer, ng/ml | 250–500 | – | Thrombosis, multiple hematomas, long-term smoking, postoperative period, liver disease. | |
Interpretation of possible disorders and diagnosis
The final diagnosis is made by a doctor. Based on a hemostasiogram, general blood test, medical history, and examination of the patient. Additional examinations may be prescribed.
Causes of hemostasis disorders:
- liver and kidney diseases of an acute and chronic nature;
- insufficient amount of vitamin K in the body;
- congenital or acquired diseases of the hematopoietic system;
- cardiovascular pathologies;
- pregnancy;
- burns, hematomas and other damage to the skin and connective tissue;
- taking certain medications;
- autoimmune processes;
- intoxication of the body;
- malignant tumors;
- inflammation of various localizations.
A coagulogram is prescribed by cardiologists, hematologists, surgeons, therapists, hepatologists, and gynecologists.
Diagnosis of cardiovascular diseases
In case of problems of the cardiovascular system, it is important to exclude blood thickening. Since there is a risk of blood clots forming and blocking blood vessels. A heart attack, stroke, or thrombosis may occur. In case of increased viscosity, thinning agents are prescribed.
A coagulogram is the most important study for determining blood clotting parameters, which is performed for safe surgery, for heart disease, and during pregnancy. Based on the results, you can judge the risk of bleeding or thrombosis.
Normal PTI indicators
The values of this protein are indicated as a percentage. Standards vary depending on the method of determination. According to Quick, normal grades range from 78 to 142 percent, while according to other studies, from 95 to 105 percent.
The ambiguity of the indicators is associated with the different sensitivity of the reagents; different types of laboratories use different ones. PTI is considered an outdated indicator, and an indicator almost never used in modern medicine. It was replaced by the INR (international normalized ratio).
Back in 1983, the Ministry of Health introduced this value in order to obtain the same PT results obtained by different laboratories with different reagents. The INR is not affected by the conditions created by the laboratory; the INR norm shows from 0.82-1.18 for the adult category of people, and from 2 to 3 during anticoagulant therapy.
Norm for women
As such, there are no differences in the results of levels between women and men. The norms are standard for both sexes.
Normal PTI during pregnancy
Great attention should be paid to analyzing the coagulogram, and in particular the PTI during gestation. All expectant mothers must undergo this procedure. The risk of bleeding or progression of thrombosis during childbirth is determined based on this analysis. When PTI readings are below 80%, it is low - as a result, coagulants are prescribed so as not to lose a lot of blood during childbirth. If the concentration percentage is 100, then the therapy is directed in the opposite direction.
Do not skimp on tests - this will help save the life of both you and your unborn child. Deciphering the analysis by a qualified doctor takes five minutes. And this will significantly speed up the treatment process.
What to do with an increased prothrombin level
How to reduce prothrombin level? This category of people must adhere to a certain diet and lifestyle.
You need to eat as many foods as possible that help thin the blood. It is important to understand that there are a number of foods that can cause blood to thicken.
List of necessary ingredients to lower prothrombin levels:
- Everyone knows oatmeal. Oatmeal not only helps stabilize digestion, but also prevents blood thickening. Ideally, you should consume this dish as breakfast. If desired, you can supplement the porridge with fresh berries.
- Tomato juice, especially when made from fresh vegetables yourself. Many people make the grave mistake of adding salt to juice.
- Beetroot is an ideal vegetable that helps reduce prothrombin levels.
- What is a diet without ginger? It can be added to tea. Ginger root thins the blood and prevents the formation of blood clots.
- Flaxseed oil, olive oil.
- Fish fat. Currently, it can be purchased in pharmacies in capsule form. This is an excellent odorless and tasteless option.
- It is recommended to use apple cider vinegar during cooking.
- A pineapple. It is enough to eat just a little to trigger beneficial processes in the body.
What rules should you follow during the diet:
- Give preference to vegetables, fruits and fresh berries.
- Meat may be present on the table, but in minimal doses.
- Meat can be replaced with fish.
- Limit your consumption of baked goods.
- It is best to cook in a double boiler.
- You need to eat more often, but in doses.
- Be sure to drink regularly.
What not to eat or drink:
- Smoked meats.
- Fatty, rich soups.
- Canned food.
- Alcoholic drinks.
Conditions in which it is advisable to get tested
To understand the indicators of a blood test for INR, you need to know how the coagulation and anticoagulation systems of the blood work.
The first mechanism prevents the development of excessive blood loss from the wound, hemorrhages in the body cavity and internal organs. The second mechanism prevents blood from clotting too actively, thereby preventing blood vessels from clogging with blood clots. The coagulation system, or hemostasis, is divided into two types: coagulation and vascular. Vascular hemostasis comes into play quickly, immediately after the integrity of the vascular wall is damaged. It is provided by the work of blood cells - platelets. But vascular coagulation alone is not able to completely stop bleeding.
https://www.youtube.com/watch?v=EenYDnE4HQU
Coagulation hemostasis is connected next. This mechanism exists due to the functioning of special proteins - coagulation factors. They are synthesized by liver cells. Therefore, with its diseases (hepatitis, cirrhosis), excessive bleeding occurs. Only the work of these proteins can ensure the final stop of bleeding.
The main way to check the condition of the bloodstream is a coagulogram. One of its most significant indicators is the level of prothrombin, or coagulation factor II. It is produced in the liver under the influence of vitamin K.
The level of prothrombin in the blood cannot be calculated directly. Its amount is calculated indirectly through the following coagulogram indicators:
- prothrombin time;
- prothrombin index;
- prothrombin level according to Quick;
- INR.
The prothrombin index and INR are most widely used in modern medicine, as they are the most informative.
Separately, it is also worth highlighting diseases and pathological conditions in which a blood test for INR is not necessary, but in some cases the doctor may prescribe it. Among them:
- long-term infectious diseases;
- sudden change in lifestyle;
- change in diet;
- climate change;
- the appearance of blood in the urine;
- prolonged menstrual bleeding in women;
- frequent nosebleeds;
- causeless bruises and hematomas;
- blood in the stool;
- constant appearance of blood when brushing your teeth;
- prolonged bleeding from minor injuries;
- periodic appearance of swelling, pain and redness of the joints, which may be due to the accumulation of blood in them.
You can carry out such a test in the following ways:
- Receive a referral for testing from a local doctor.
- The test is carried out in the therapist’s office directly if he has the necessary equipment.
- Purchase a portable device to determine the INR at home.
It is most convenient to do this test at home, since the patient does not have to visit the clinic very often, donating venous blood and wasting his time waiting in queues. To perform this test, you need fresh blood from your finger. A completely painless puncture is performed using a special device, which is a scarifier.
An INR test, according to WHO recommendations, is prescribed for all methods of therapy that require constant monitoring of blood clotting. It most accurately shows the state of the human circulatory system. This study was approved by all leading experts in anticoagulant therapy monitoring and antithrombotic treatment.
We looked at the interpretation and norm of INR in a blood test.
Monitoring anticoagulant therapy using INR
Answering the question of what a blood test for INR shows, it is worth saying that this is an effective method for monitoring therapy with anticoagulants and antiplatelet agents. These two groups of drugs thin the blood. Therefore, it is necessary to constantly monitor the state of the blood coagulation system to prevent the development of severe bleeding. This is especially true for treatment with such drugs:
- “Heparin”;
- "Warfarin";
- “Sinkumar”;
- “Finilin.”
Anticoagulants are prescribed to people with a tendency to excessive blood viscosity, with an increased risk of thrombosis (myocardial infarction and stroke, congenital and acquired heart defects, history of pulmonary embolism, varicose veins, thrombophlebitis).
Kwik indicators
Quick analysis is done for additional examination of the gastrointestinal tract, as well as the liver.
Quick analysis is performed in the following cases:
- When clotting is impaired.
- There are ailments associated with the liver.
- There is a process of increased thrombus formation.
- With a disease such as blood cancer.
- In cases associated with vitamin K deficiency.
What limits of indicators are acceptable:
- Up to 6 years – 80–100.
- From 6 to 12 - 79–102.
- From 12 to 18 - 78–110.
- From 18 to 25 - 82–115.
- From 25 to 45 - 78–135.
- From 45 to 65 - 78–142.
The norm for women and the norm for men, regardless of age, are identical.
Prothrombin time is an indicator that reflects the seconds during which plasma coagulates after adding the desired mixture to it.
- In children, especially newborns, this figure is 14–18 seconds.
- For adults, the normal figure is 10–15. The optimal value of prothrombin time ranges from 9–12 seconds.
Where is the INR test performed?
To donate blood and get INR results, you need to get a referral from your doctor for tests that are performed:
- in the clinic;
- laboratories;
- at home.
In addition, this test is often carried out in a doctor’s office, however, if he has all the necessary equipment. You can do an INR test yourself using a special portable device.
Testing for INR at home is the most convenient option for many patients, since they will not need to constantly visit the clinic.
Carrying out this test involves the use of blood from a finger (in this case, a man and a woman must know how to properly prepare for donating blood). To obtain it, doctors use a scarifier, which makes a painless hole in the skin. After this, special test strips are inserted into the device for determining INR, where the doctor applies a drop of blood. After some time, the INR values appear on the scarifier display.
According to the advice and recommendations of the WHO, an INR test should be prescribed for any method of treatment that requires regular monitoring of blood clotting levels. After all, this analysis most accurately reflects the functional state of blood coagulation in the patient and quickly gives a reliable result.
What does the increase indicate?
An increase in the INR indicates a predisposition to bleeding, and the doctor decides to reduce the dosage of anticoagulants.
When the values of this test decrease, the patient's risk of developing blood clots increases. Such indicators indicate the low effectiveness of blood thinning drugs, and the doctor decides to increase the dosage. When decoding INR in a blood test in adults, they rely on certain standards.
A change in INR values in people who did not take medications for the purpose of blood thinning indicates all sorts of pathological disorders occurring in the body. An increase in the INR value greater than one indicates the possible development of the following pathologies:
- The presence of congenital pathologies of the coagulation system.
- Vitamin K deficiency in the human body.
- The appearance of liver pathologies.
- Impaired absorption of fats in the intestinal area.
- A side effect of anti-gout drugs, and also some antibiotics, anabolic steroids and steroids.
First of all, such hypocoagulation is extremely dangerous due to the occurrence of internal and external bleeding. INR indicators are critical when deciphering a blood test of more than 6 units. Such jumps are especially dangerous in the presence of hypertension, inflammatory or ulcerative lesions of the digestive system.
Why measure INR and PTI?
In medical practice, INR analysis is very important for monitoring blood clotting ability in patients taking tableted (indirect) anticoagulants, for example, warfarin, phenylin, tromexane and others. They are often prescribed for conditions where there is a threat of thrombosis: heart rhythm disturbances, blood thickening, severe vascular atherosclerosis, thrombophlebitis, increased prothrombin.
Treatment with anticoagulants should always be carried out under the control of coagulation , because an insufficient dose can only “spur” thrombus formation, and excessive use, on the contrary, can reduce coagulation and lead to the development of bleeding.
It is the INR analysis that reflects the most objective picture of blood clotting, regardless of the time of day, food or liquid intake.
An analysis of the prothrombin index (PTI) reveals the very fact of a decrease or increase in blood clotting. It is always prescribed before operations, childbirth, blood transfusions and other procedures, and is prescribed to patients with cardiovascular pathology and the elderly. Deviation of PTI from the norm is an indication for examining the patient to determine the cause of the violations.
What INR values are considered normal?
In adults, the INR is approximately 0.7-1.3, but it often varies within a “radius” of 0.85-1.25.
If a patient takes anticoagulants as prescribed by a doctor, the INR level after testing is 2.0 or 3.0 units. If people do not take medicinal compounds aimed at thinning the blood flow, then abnormal INR values, up or down, indicate that the patient has serious pathological diseases.
The formation of elevated INR values that are greater than 1 indicates the presence of the following diseases:
- Pathologies and dysfunction of the liver.
- Lack of microelements and vitamin K in the body.
- Congenital or acquired pathologies of the coagulation system.
- The appearance of side effects as a result of taking antibiotics or anti-gout drugs.
- Impaired absorption into the intestinal walls of fats entering the body with food.
A condition in which elevated INR values and deterioration of coagulation occur is called hypocoagulation, which threatens the patient with the development of external or internal hemorrhages. Moreover, the first type of bleeding often occurs even after minimal damage to the skin (scratch, open wound, etc.). The causes of internal bleeding (uterine, abdominal, gastric, and so on) can be any disease and process occurring in the human body (for example, menstruation).
INR values exceeding 6.0 can be called especially dangerous and critical. This threatens serious problems with diseases of the vascular and urinary systems, inflammation and damage to the gastrointestinal tract by ulcerative formations, as well as hypertension. In these cases, the patient needs immediate hospitalization and effective treatment.
It is also worth remembering that if an upward change in INR results is observed in people taking anticoagulants as treatment, this indicates the need to adjust the dose of these medications.
When INR values decrease, the patient may develop the following pathological conditions:
- an increase in the amount of antithrombin in the body;
- jumps in hematocrit up and down;
- side effects on a woman’s body of diuretic medicinal compounds.
The collection of blood from the patient for the study is done from a catheter that was previously installed in the central vein.
A decrease in INR parameters is called hypercoagulation, in which patients have a high risk of serious complications such as pulmonary embolism and thrombosis.
Blood coagulation system
Normal blood thickness is ensured by the coordinated functioning of two systems: coagulation and anticoagulation. Its fluid state is regulated by anticoagulation mechanisms, and thrombus formation by coagulation mechanisms. When the balance between them is disturbed, a person has an increased tendency to bleed or form blood clots (thrombi).
One of the most significant indicators of a coagulogram, reflecting the state of the coagulation system, is a complex protein - prothrombin. It is also called coagulation factor II. It is formed with the participation of vitamin K in the liver. It is by the indicators of this protein, which is a precursor of thrombin, that the doctor can assess the state of the coagulation system and the patient’s tendency to bleeding or thrombosis.
Determination of the level of prothrombin in the blood can be carried out using the following methods:
- PTT (prothrombin time);
- prothrombin level according to Quick;
- PTI (or prothrombin index);
- INR.
In everyday clinical practice, doctors most often prescribe PTI or INR tests, since they most reliably reflect the state of the coagulation system.
What does an increase in INR mean?
Among doctors, it is generally accepted that deviation towards an increase is extremely undesirable and even very dangerous. Excessive blood thinning will inevitably lead to a deterioration in its coagulability, significantly increasing the chances of bleeding in both external and internal organs. If the INR is significantly greater than one, the attending physician is obliged to reduce the dose of anticoagulants taken by the patient.
In cases where high values are observed in people who do not take such medications, this may indicate:
- liver diseases;
- cancerous tumors;
- development of myocardial infarction;
- hemorrhagic disease;
- polycythemia;
- the presence of pre-infarction conditions;
- about problems with the outflow of bile.
If the INR factor exceeds 6 units, the person must be immediately admitted to hospital, since the risk of bleeding is extremely high, and treatment must be started as soon as possible.
Why control INR?
Doctors regularly measure the INR in people being treated with warfarin to balance the risk of excessive bleeding with the risk of blood clots. If the INR is too high, it means the blood is too thin. If the indicator is low, then the likelihood of thrombosis is higher.
- An INR value of more than 4.5 is accompanied by a risk of severe bleeding.
- And less than 2 increases the risk of heart attack, stroke and other thromboembolic complications.
When using Warfarin, regular monitoring of the INR is important because:
- there is very little difference between the most effective dose and the one that causes serious side effects;
- Each person requires an individual selection of the effective dosage of Warfarin;
- it is possible that there is an interaction between several medications that the patient is taking and their effect on clotting;
- Eating habits can also affect the effectiveness of Warfarin.
The more often the study is done, the more accurately the dose is selected. Thus, when analyzing once a month, the required dose is selected in 50% of cases, and with weekly monitoring – in 85% of patients.