A blood test for tumor markers is prescribed if a tumor is suspected. Those who are at risk of developing malignant tumors are recommended to undergo the study annually. The risk group includes people with a genetic predisposition to cancer, chronic diseases, precancerous pathologies, as well as those living in environmentally unfavorable regions or working in hazardous industries. In the presence of cancer, the analysis is carried out for monitoring purposes.
A blood test for tumor markers is used for early diagnosis of certain types of tumors, monitoring treatment, detecting metastases and relapse
Tumor markers are the metabolic products of tumor formation, as well as substances produced by normal tissues of the body in response to invasion of cancer cells. In the body of healthy people, some tumor markers are present in small quantities; an increase in their concentration in the blood and urine of patients indicates the development of cancer with a high probability. In some cases, tumor markers increase in some non-cancer diseases.
Before donating blood, you should not smoke for 24 hours; you should eliminate emotional and physical stress 30 minutes before donating blood.
To prescribe an analysis and interpret the results of the study, you must contact a qualified specialist who will explain what the blood test for tumor markers says and shows, how the material is taken and how the analysis is done, as well as how you need to prepare for it.
Indications for the study
To identify a malignant process, the study of specific proteins such as CEA, CA 15-3, ER/PR is most often recommended.
When to donate blood for tumor markers of breast cancer after the patient’s initial visit, the doctor decides. As a rule, he takes into account the following symptoms of the possible development of an oncological process:
- Change in appearance - volume and shape of the breast.
- Peeling and hyperemia of the skin in one of the areas of the mammary gland.
- Inverted nipple.
- Nodules in the tissues of the gland, tightly fused to the skin and adjacent anatomical structures, felt upon palpation.
- Chest pain;
- Rapid development of a benign neoplasm in the gland.
Indications for the test may include:
- Early diagnosis of breast cancer.
- Determining the prognosis of the disease.
- The level of the body's susceptibility to drug therapy.
- Monitoring your health after surgery.
- The need to make changes to the chosen treatment tactics.
- Confirmation of the effectiveness of antitumor therapy.
Tumor markers for breast cancer necessarily require interpretation by a highly qualified specialist. The fact is that with values exceeding the norm, we are not necessarily talking about a malignant process - perhaps the problem lies in an inflammatory pathology of the breast, for example mastopathy. Therefore, you should not decipher the research results yourself. In addition to tumor markers, the oncologist will evaluate the size of the detected tumor, the fact of damage to the lymph nodes and histological data, that is, he will study the situation as a whole.
What other tumor markers are used by doctors to diagnose malignant neoplasms?
The remaining tumor markers have lower sensitivity and are not used in diagnostic programs for cancer screening. They are used by doctors only in specific clinical situations when it is necessary to confirm the diagnosis at one of the stages of examining the tumor process or in the process of monitoring the effectiveness of treatment after therapy for the cancer process.
These tumor markers include:
- Ca-15-3 – to assess the effectiveness of treatment and the course of the tumor process in breast cancer;
- Ca-19-9 – to evaluate the effectiveness of treatment for cancer of the pancreas, stomach, biliary tract and gall bladder;
- CEA (carcinoembryonic antigen) is a marker of the spread of colorectal cancer and recurrence of breast cancer;
- B2M – marker of multiple myeloma, some lymphomas, chronic lymphocytic leukemia;
- calciotonin – a marker of thyroid cancer;
- A(CgF) – marker of neuroendocrine tumors;
- BCR-ABL – marker of chronic myeloid leukemia;
- fragments of cytokeratin 21-1 – a marker of lung cancer;
- immunoglobulins – markers of multiple myeloma and Waldenström macroglobulinemia;
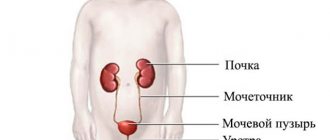
- UBC – bladder cancer marker;
- HE-4 – ovarian cancer marker;
- SCC – marker-antigen for squamous cell carcinoma of the cervix;
- NSE – marker for prognosis in small cell lung cancer;
- Cyfra 21-1 – a marker for prognosis in non-small cell lung cancer;
- Lactate dehydrogenase is a marker of germ cell tumors.
List of tumor markers
Several types of breast markers are used:
- whey;
- fabric;
- genetic.
Serum
The molecules have a protein-carbohydrate structure and are detected exclusively in human blood. Diagnostics consists of carrying out a binding reaction with monoclonal antibodies. Serum tumor markers for breast cancer are used quite often. These include:
- mucous or mucin glycoproteins of the MUC-1 group, for example CA 15-3, CA 125, CA 27.29, CA 549, M20 and SMA;
- CEA—carcinoembryonic antigen;
- cytokeratins - TPS, TPA.
In most cases, the doctor prescribes an analysis for one of the listed specific proteins of the MUC-1 group, usually CA 15-3 due to its high sensitivity. The information value of the study does not change if several antigens from this class are simultaneously assessed. In addition to CA 15-3, a breast tumor marker such as CEA is often studied.
Let's take a closer look at the main groups of serum markers.
Class MUC-1. In a healthy mammary gland, substances of this group are secreted into the ducts and enter colostrum or breast milk. The oncological process that affects the tissues of the organ leads to abnormal changes in their structure, so glycoproteins begin to be synthesized uncontrollably by the cells of the mammary gland and are found in the blood.
Among the antigens listed above, the specific proteins CA 15-3 and CA 125 are most widely used in research.
REA. One of the most common and studied tumor markers, which is predominantly produced by tumors such as adenocarcinomas of the intestine, pancreas and mammary glands. In combination with an analysis for CA 15-3, the CEA marker will help to diagnose breast cancer with a high probability.
Cytokeratins. Tumor markers such as TRA, TPS and Cyfra 21.1 belong to this class. Cytokeratins are present in every cell of the human body and consist of 20 protein regions closely associated with each other. In breast cancer, pairs CK 18/19 and CK 8/18 are often detected.
The TPA analysis allows us to determine all three peptides (8, 18, 19), TPS - 8 and 18, Cyfra 21.1 - 8 and 19.
Tissue tumor markers
Specific substances indicating the presence of breast cancer can be detected not only in the blood, but also when examining organ tissue. In this case, biological material obtained during a biopsy on a suspicious area of the breast or after surgery is used.
Tissue tumor markers help in selecting treatment tactics and predicting survival. The receptors sensitive to estrogen (ER) and progesterone (PR), as well as HER-2, are to be studied. But these indicators are not informative in the early diagnosis of cancer, since they can be present both in a healthy mammary gland and in atypically changed tissues of the organ.
In individuals without lymph node involvement, markers such as uPA and PAI-1 are tested.
Breast cancer is a heterogeneous disease, so genetic studies are used to classify it, aimed at studying four subtypes of pathology. They, in turn, differ in treatment approaches and prognostic data. Let's look at them:
- Basal. ER, PR and HER-2 are absent.
- Luminal A. ER is detected in small quantities.
- Luminal B. ER is diagnosed in high concentrations.
- HER-2. Positive.
ER and PR receptors play an important role in the development of breast cancer. Thanks to them, sex hormones can influence breast tissue. At any stage of the disease, the malignant process is better treated with hormonal drugs if the patient has ER-positive receptors. Therefore, such studies are prescribed to all women without exception.
The HER-2 receptor is the most sensitive tumor marker for breast cancer. It is detected in 15–30% of cases of the disease. If it is detected, aggressive development of the malignant process and the least favorable prognosis for survival are expected. Patients with HER-2 are prescribed immunotherapy with the drug Herceptin, and they have a weak response to chemotherapy.
Urokinase tissue tumor markers uPA and PAI-1 can predict the outcome of pathology in breast lesions. The first is involved in the growth and invasion of the tumor, the process of lymphogenous and distant metastasis, the second is involved in the progression of the oncological process. Repeated clinical studies have been conducted, which have been able to confirm that with low levels of uPA and PAI-1, the likelihood of the spread of metastases and the development of relapses of pathology is reduced.
There are other tissue markers that have diagnostic value, such as Ki-67.
Genetic tumor markers
Testing for mutations in the BRCA1 and BRCA2 genes allows us to assess whether a woman has a predisposition to developing breast cancer. Referral for this analysis is relevant for persons in whose family there have already been cases of the disease. These genes are responsible for the integrity of chromosomes and prevent mutational changes in cellular structures. With BRCA1 and BRCA2 pathology, the likelihood of encountering breast and ovarian cancer increases significantly.
Testing for genetic mutations of BRCA1 and BRCA2 also provides information necessary for early diagnosis of breast tumors.
Which tumor marker tests are used in screening examination programs?
The main tumor markers that are used in screening programs for examining patients with a high risk of cancer pathology are:
- PSA;
- hCG;
- AFP;
- Sa-125.
General PSA tumor marker analysis
This tumor marker is a precursor to prostate tumors. This test is included in the screening program for prostate cancer, and oncologists recommend that men undergo it annually after 40 years of age.
Normal total PSA test values vary depending on age. For men 40-49 years old they are 2.5 ng/ml, 50-59 years old - 3.5 ng/ml, 60-69 years old - 4.5 ng/ml, over 70 years old - 6.5 ng/ml. If the indicators of this analysis are moderately elevated, then the man needs to undergo a free PSA test, which is more specific.
One should also take into account the fact that PSA test results can be elevated not only with prostate cancer, but also with prostate adenoma, prostatitis, or even after a regular prostate massage. To clarify these diagnoses, the patient is prescribed other types of diagnostic tests that allow an accurate diagnosis.
Analysis for the tumor marker hCG (human chorionic gonadotropin)
Normally, the levels of this tumor marker are less than 5.3 mIU/ml in non-pregnant women, and less than 2.5 mIU/ml in men. This test is often prescribed by oncologists in conjunction with an analysis for the tumor marker AFP to determine the likelihood of testicular and ovarian cancer. In testicular cancer, an increase in both tumor markers is observed, and in ovarian cancer, AFP increases significantly. The levels of this tumor marker may increase in other cancers (uterine cancer, stomach cancer, intestinal cancer, liver cancer), pregnancy, and in menopausal women who have uterine fibroids. That is why, to differentiate the diagnosis, this analysis is carried out in combination with other types of examination.
Alpha fetoprotein (AFP) test
This analysis is used by oncologists to diagnose and evaluate the effectiveness of treatment for liver cancer and germ cell tumors, and by obstetricians-gynecologists to identify developmental disorders and chromosomal defects in the fetus. Normally, AFP levels in men and non-pregnant women are less than 15 IU/ml, and during pregnancy, its normal levels depend on the duration of pregnancy.
An increase in AFP levels in men and non-pregnant women can be observed with malignant neoplasms:
- primary and metastatic liver cancer;
- ovaries;
- embryonal cancer;
- colon;
- pancreas;
- lungs;
- bronchi;
- mammary gland.
An increase in the level of this cancer marker can also be observed in the following benign diseases:
- acute viral and chronic hepatitis;
- cirrhosis of the liver;
- chronic renal failure.
To diagnose the fetus and pregnancy, obstetricians-gynecologists perform this test together with blood tests for estriol and hCG. An increase in AFP levels may indicate:
- multiple pregnancy;
- fetal malformations;
- cleft of the anterior abdominal wall in the fetus;
- fetal anencephaly;
- liver necrosis in the fetus, etc.
A reduced level of this tumor marker indicates:
- high risk of genetic pathologies in the fetus (for example, Down syndrome);
- false pregnancy;
- beginning miscarriage.
A slightly reduced AFP level indicates fetoplacental insufficiency.
Analysis for tumor marker Ca-125
This tumor marker is the main marker of ovarian cancer and its metastases. Normally, its levels do not exceed 0-30 IU/ml.
Due to the fact that an increase in the indicators of this tumor marker can occur in various diseases, it is not used as an independent diagnostic method, and its implementation is only the first step, which can indicate the development of a malignant neoplasm. If the level of Ca-125 increases, the patient is prescribed a more in-depth examination to identify the reasons for the deviation of its values from the norm.
An increase in the level of tumor marker Ca-125 can be detected in cancer:
- ovaries;
- uterus;
- mammary glands;
- stomach;
- pancreas;
- liver.
A slight increase in Ca-125 levels can be detected in the following benign diseases:
- endometriosis;
- ovarian cyst;
- peritonitis;
- pleurisy.
The level of Ca-125 can increase during menstruation, and this indicator will be physiological and not require treatment.
Norm
Let's look at the normal values of breast tumor markers in the following table.
| Tumor marker name | Norm IU/ml (U/ml) |
| SA 15-3 | 0–22 |
| REA | Up to 3 ng/ml for smokers, up to 5 ng/ml for smokers. |
| CA 125 | Up to 35 for women, up to 10 for men. |
| BR 27.29 (glycoprotein MUC1) | Up to 40 |
| HER-2 | It is used to monitor therapy; values above 450 ng/ml indicate ineffective antitumor therapy and a poor prognosis for survival. |
| TRA | Up to 75 |
If the analysis shows deviations from the norm, this does not indicate the presence of cancer in the body. With a malignant tumor, the listed figures increase tens and hundreds of times. The interpretation of the study must be carried out by a doctor, taking into account the available clinical and diagnostic data.
Mammary cancer
This malignant tumor occupies a leading place among female neoplasms. Such disappointing statistics are to some extent due to the low qualifications of doctors who perform unprofessional examinations of the mammary glands.
- Palpation of the gland allows you to identify lumps and swellings in the thickness of the organ and suspect a tumor process.
- Breast radiography (mammography) is one of the most important methods for detecting non-palpable tumors. For greater information, artificial contrast is used: pneumocystography (removal of fluid from the tumor and introduction of air into it) - allows to identify parietal formations;
- ductography - the method is based on the introduction of a contrast agent into the milk ducts; visualizes the structure and contours of the ducts, and abnormal formations in them.
| Research: | Risk factors: |
|
|
Decoding
Let's look at what the decoding of the main tumor markers looks like:
- CA 15-3 normally does not exceed the values of 0–22 IU/ml, characteristic of this breast tumor marker. At levels of 25–60 IU/ml we are talking about inflammatory processes in the mammary gland or benign neoplasms. If the CA 15-3 titer is above 60 IU/ml, breast cancer is highly likely.
- CA 125 at normal levels - up to 35 IU/ml in women and 10 IU/ml in men - does not pose a danger to humans. This marker slightly exceeds the norm - up to 100 IU / ml - in the fair sex during menstruation and pregnancy, as well as in liver cirrhosis, endometriosis, ovarian cysts, pleurisy and some other diseases. At levels above 100 IU/ml, an oncological process in the body is suspected.
- TRA should normally not exceed 75 IU/ml. A slight increase in the level of tumor marker is observed in inflammatory pathologies of the liver and kidneys, urogenital tract, lungs, etc. Values significantly higher than this indicator may indicate not only a malignant lesion of the mammary gland, but also tumors of the lungs, bladder, gastrointestinal tract, head and neck.
- CEA should normally not exceed 5 ng/ml; even a slight increase in the titer of this antigen may indicate a malignant process in the breast, reproductive system organs and other anatomical structures.
- BR 27.29 with values above 40 IU/ml may indicate the presence of a tumor in the mammary gland, early relapse of oncological pathology, or the ineffectiveness of antitumor therapy.
Reduced indicators of tumor markers against the background of the ongoing course of therapy for breast cancer indicate its effectiveness and regression of the disease. In 30% of patients at an early stage of the disease, antigens may not show deviations from the norm.
“Female” tumor markers
SA-125
A high molecular weight glycoprotein produced by epithelial cancer cells localized in the ovary, as well as other cells that originate from the Müllerian duct.
In healthy women, the concentration in the blood of this tumor-associated antigen almost never exceeds 35 U/ml, but in patients with ovarian cancer (especially serous ovarian adenocarcinoma), its content increases significantly.
An example of the ratio of CA-125 levels with different types of process in the ovaries:
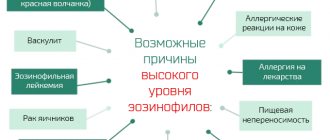
CA-125 exhibits positive associative connections with benign processes of the genital organs, as well as with tumors of other localizations: breast, lungs, liver, gastrointestinal tract. An increase in the level of tumor marker CA-125 is observed in some diseases of autoimmune origin and during pregnancy.
SA-15-3
A highly specific marker associated with breast carcinoma (BC), which, however, is not only located on the surface of cells in the area of malignancy, but (in much smaller quantities!) is synthesized by normal epithelial cells in the breast, lungs, pancreas, ovaries, urinary bladder, large intestine.
HE4
Glycoprotein, a protein inhibitor, is normally present on the epithelial tissues of the genital organs, pancreas, and upper respiratory tract.
The content of HE4 increases sharply during cancer processes localized in the ovary and endometrium. The sensitivity of this tumor marker is much higher for early stage epithelial ovarian cancer than CA-125 (in 50% of cases, HE4 was elevated, while CA-125 did not “feel” the appearance of the tumor and remained at normal levels).
Meanwhile, the use of these markers in combination with each other significantly improves diagnostic capabilities, including differential diagnostics (allows one to distinguish benign processes from malignant ones) and monitoring the effectiveness of therapeutic measures.
SCC marker (SCCA – squamous cell carcinoma antigen)
It is considered an antigen for squamous cell carcinoma of any location (lungs, ear, nasopharynx, esophagus, cervix), that is, it is a glycoprotein that is produced by the tissue of any squamous cell. Physiological tasks are also not alien to SCC; for example, it takes part in the differentiation of normal squamous epithelium and is synthesized by the salivary glands.
Analysis for the SCC tumor marker is prescribed mainly to monitor the course of the pathological process and the effectiveness of treatment measures for all squamous cell cancers, but since carcinoma prefers the cervix more than other organs, material taken from women is more often examined. In addition, the marker has a very important prognostic value, since its content in the test sample corresponds to the degree of histological differentiation of cancer.
Normal SCC values do not exceed 2.5 ng/ml. High levels of this tumor marker can be found in the blood serum of pregnant women (from the end of the first trimester), with benign skin tumors, bronchial asthma and renal or liver failure.
Scheme for studying tumor markers
Let us highlight several points that relate to the mandatory aspects of studying breast tumor markers:
- Collection of information about the presence/absence of malignant processes in the body in addition to other diagnostic methods.
- Carrying out control tests before and after treatment to assess the effectiveness of the chosen therapy.
- Early detection of metastases and relapses of oncological pathology, that is, dynamic monitoring of the patient’s condition after therapy (as a rule, tests for CEA and CA 15-3 are used).
- Determination of ER and PR receptors for prescribing hormonal treatment.
- Determination of HER-2 for the purpose of Herceptin therapy.
- Genetic testing for tumor markers BRCA1 and BRCA2 in the case of “familial” breast cancer to identify predisposition to the disease.
Stomach cancer
Stomach cancer is the second most common tumor among the population (after lung cancer).
- Fibroesophagogastroduodenoscopy is the golden method for diagnosing gastric cancer and is necessarily accompanied by a large number of biopsies in different areas of the tumor and unchanged gastric mucosa.
- X-ray of the stomach using oral contrast (barium mixture) - a method that was quite popular before the introduction of endoscopes into practice, allows you to see a filling defect in the stomach on an X-ray.
- Ultrasound examination of the abdominal organs, CT, MRI are used to search for metastases in the lymph nodes and other organs of the digestive system (liver, spleen).
- Immunological blood test - shows stomach cancer in the early stages, when the tumor itself is not yet visible to the human eye (CA 72-4, CEA and others)
| Study: | Risk factors: |
| from 35 years of age: Endoscopic examination once every 3 years |
|
Reliability of research data
The reliability of the test results for any tumor marker for breast cancer or suspicion of it depends on the patient’s compliance with the rules for preparing for the analysis and the competent execution by the laboratory assistant of all manipulations for collecting biological material. Any violation is fraught with the appearance in the blood of a titer of additional specific proteins that have nothing to do with the terrible diagnosis.
For this reason, it is important for both the woman and the performing medical personnel to approach the study responsibly. In this case, you will not have to take the test twice or recheck it in other laboratories.
Sad story
St. Petersburg resident Ilya Fomintsev, an oncologist and executive director of the Cancer Prevention Foundation, through his blog addressed an open letter to commercial laboratories in the country calling on them to stop advertising tests for tumor markers for the early diagnosis of malignant tumors.
Ilya Fomintsev, oncologist. Photo from the-village.ru website
In the comments to the letter, readers quite rightly point out that such an analysis is not always the initiative of the patient himself; sometimes doctors refer it to it during a preventive examination, meaning the same thing - the possibility of early diagnosis in the absence of other symptoms. Yes, the analysis does not allow an accurate diagnosis, but what harm does it do?
“What is the harm from a false positive diagnosis of suspected cancer? - Fomitsev is surprised. - Yes, this is a huge psychological trauma. A person may rightly be outraged that this was offered to him.”
But it's not just about psychological trauma. Here's a sad story.
The patient has a number of signs of an oncological process: feces with blood, vasoconstriction, defecation disorders. He is tested for tumor markers of intestinal cancer, the indicators are normal, and the person calms down, attributing the symptoms to hemorrhoids, and after 9 months he dies from a malignant intestinal tumor with metastases to the liver.
However, here we are dealing with a patient who decided not to see a doctor based on a negative test result.
But complications also arise with false positive results, which in some cases lead to invasive diagnostic methods.
Ilya Fomintsev talks about a tragic case: the tumor marker was elevated, the patient’s intestine was pierced during fibrocolonoscopy, as a result of which fecal peritonitis developed, leading to the death of the person. As it turned out - unfortunately, too late - the patient did not have cancer.
Of course, death in this case is a tragic accident. But the costs associated with a false-positive result of tumor marker testing are high in any case.
Preparing for tests
To obtain the most accurate test results, it is important to follow the recommendations listed below:
- It is not recommended to drink alcohol or engage in significant physical activity 48 hours before taking blood.
- You should refrain from eating for 8 hours before the test.
- You should not smoke 3 hours before the test.
- You need to visit the laboratory in the morning, no later than 11 o’clock.
If a person is forced to constantly take any medications, he must inform the doctor about this before the study. There is also an opinion that you should not donate blood for tumor markers for breast cancer a few days before and during menstruation, but not all experts agree with this statement, so you need to consult your doctor.
If a tissue examination of the breast is planned, based on invasive techniques of biopsy and organ puncture, it is important for the patient to adhere to the recommendations listed above.
How to donate blood for tumor markers?
It is necessary to follow some recommendations, then the analysis for tumor markers will show an objective picture of the state of health:
Donating blood for tumor markers is allowed only in the morning, on an empty stomach. Three days before blood sampling, you need to stop consuming alcohol-containing products, tobacco, and fatty foods. It is also not recommended to consume smoked, pickled, spicy foods. Before the test day, you should avoid any physical activity. Stop taking medications other than those you need for your vital signs (consult your doctor). You may need to abstain from sexual intercourse. during some time.
The doctor may prescribe a specific blood test for cancer cells, or several tests at once to get more accurate data.
Important! All known and used markers for identifying tumor cells cannot be specific for a particular neoplasm with a malignant nature. It is worth noting that an acceptable (within normal) marker value does not exclude the development of a tumor in the body or its recurrence.
Tumor markers are used in medicine to track the progression of the disease and monitor the effectiveness of the treatment method used (surgery, chemotherapy, radiotherapy or hormone therapy). The most informative is the dynamics of the level of the research conducted, in comparison with a single result of the analysis.
Studying the dynamics of the marker makes it possible to differentiate diseases into malignant and benign based on changes in the level of the marker (in the case of a benign nature of the disease, the marker level increases to a minimum level and remains within these limits).
In some cases, a correctly assigned profile of tumor marker concentrations allows one to determine the onset of changes in tumor formation 1-6 months faster than using other diagnostic methods. With a regular decrease in the concentration of analysis parameters after the prescription and start of a course of chemotherapy, one can conclude that the treatment is effective.
However, if there are no changes or an increase in indications is observed, the therapeutic method should be adjusted due to the unresponsiveness of the treatment.
How are the tests done?
For the study, venous blood is taken in the morning strictly on an empty stomach. Before collecting biological material, the patient is not recommended to be nervous; ideally, 15 minutes before visiting the office, it is advisable to sit in a calm environment. After drawing blood, the laboratory technician signs the tube in the presence of the patient to avoid confusion.
The study must be carried out in the same laboratory recommended by the doctor. This is due to the fact that each clinic has different technical equipment and narrow reference values for tumor markers, which may vary depending on the test system used.
What types are there?
There are several types of tumor markers that enable specialists to understand where exactly the tumor is developing. Cancer cannot be detected immediately in all organs. Tests for various tumor markers are prescribed even when you feel unwell, which makes it difficult to immediately treat this complex disease. Modern medical science has already come to the point that it can diagnose cancer of the lungs, stomach, rectum, ovaries, prostate, breast, cervix and some others in the early stages using tumor markers. They have their own code, which allows you to make a reliable diagnosis.
Conditions affecting blood marker levels
The following factors can affect the level of tumor markers in a person’s blood:
- pregnancy, lactation;
- menstruation;
- inflammatory diseases of the breast, ovaries, uterus, pancreas, stomach and intestines;
- cystic or benign neoplasms of the mammary gland and reproductive system of a woman;
- taking certain medications;
- drinking alcohol on the eve of the study or existing alcohol dependence;
- viral infections.
If the results of the analysis reveal that the tumor markers being studied are above normal, it is important to visit a specialist - a gynecologist, mammologist or oncologist - for a consultation and in-depth examination, since this is not always a malignant process in the breast. Quantitative changes in antigens in the blood must be deciphered by an experienced doctor who will take into account the factors associated with the test.
FAQ
When deciphering blood tests, patients often ask questions about how this or that indicator can change with cancer and what this can mean. Let's look at the most common of them.
Can a good blood test be detected in cancer patients?
Yes, it can if the disease is detected in the initial stages or at the compensation stage. In addition, do not forget that there are a huge number of types of blood tests and a situation may arise that there are no changes in the general analysis, and tumor markers were not detected.
However, the situation when a general blood test for cancer does not have any abnormalities does not occur so often
Is it possible to determine the stage of cancer using a blood test?
Oncology is staged based on many criteria, and most of them are purely clinical - the spread of the primary tumor, the presence of metastases in the lymph nodes and nearby organs, and so on. Therefore, if it is possible to draw a parallel with the stage using a blood test, then it is very approximately, and such an analysis should be highly specific, such as genetic tests or determination of tumor markers.
Is there a specific test to detect stomach cancer?
Stomach tumors cannot be detected by analyzing general blood tests. However, today there are innovative molecular tests that make it possible to determine gastric cancer and its antigenic set. This is the detection of PEA-1 tumor markers and the Foundation One genetic test, which completely determines the antigenic profile of a cancer cell. This test will show the cancer itself and determine its aggressiveness.
These tests are not carried out in all clinics in the world and are expensive. At the First Tel Aviv Medical Center, the patient has the opportunity to order all the latest genetic and molecular tests.
Can a blood test detect cancer?
Most often, even general and biochemical blood tests will show changes in indicators in the presence of cancer. However, this does not always happen and these changes may be associated with other reasons - infections, stress, and so on.
Identification of specific tumor markers is a more specific criterion, but they can also be elevated in related pathologies. But innovative genetic tests will always give an answer - what type of tumor led to the changes, whether it is treatable and show the degree of aggressiveness of atypical cells.
However, such tests are not performed in the CIS countries, so the answer to the question is no, there is no general test that determines cancer in the blood.
What tests should I take for blood cancer?
For hemoblastoses, the most effective will be a general blood test with a formula of cellular elements and a detailed biochemical analysis with the identification of tumor markers NSE and CEA-5
Deciphering a blood test for bone marrow cancer
In this situation, the general analysis will include immature cells and progenitor cells that are not normally found in the blood. During a tumor process in the bone marrow, they do not have time to develop to mature forms, enter the bloodstream and cease to perform their function
Features of testing for children, pregnant and lactating women, and the elderly
CHILDREN. Tumor markers in children, as in adults, provide an opportunity to conduct early examination to exclude cancer pathologies. Preparation for the study should comply with recommendations that are valid for adults, that is, blood from a vein should be donated on an empty stomach, exclusively in the morning and not while taking medications.
The results of the analysis can only be deciphered by the doctor who wrote out the referral for tumor markers. Since such a study is not common in pediatrics, self-diagnosis and interpretation of the data obtained at home is not recommended.
PREGNANT AND NURSING WOMEN. Increased levels of breast tumor markers are observed during pregnancy, especially in the last trimester, and during breastfeeding. For example, the CA 15-3 antigen increases to 50 IU/ml. Therefore, if a malignant process in the mammary gland is suspected in expectant and nursing mothers, it is important to use instrumental diagnostic methods. In any case, the opinion of the attending physician will have priority; self-diagnosis is unacceptable.
ELDERLY. The risk of developing cancer increases with age, so women of any age, including older ladies, are tested for breast cancer tumor markers. In their case, the likelihood of obtaining false-positive results increases, so most often it is recommended to take the test twice while carrying out other diagnostic methods.
Cervical cancer
Cervical cancer affects approximately 400,000 women per year worldwide. Most often diagnosed at very advanced stages. In recent years, there has been a trend towards rejuvenation of the disease - it more often occurs in women under 45 years of age (that is, before the onset of menopause). Diagnosis of cervical cancer:
- A gynecological examination in a speculum reveals only visible forms of cancer in an advanced stage.
- Colposcopic examination is an examination of tumor tissue under a microscope, carried out using chemicals (acetic acid, iodine solution), which make it possible to determine the location and boundaries of the tumor. The manipulation is necessarily accompanied by a biopsy of cancerous and healthy cervical tissue and cytological examination.
- CT, MRI, ultrasound of the pelvic organs - used to detect the spread of cancer to neighboring organs and the extent of its spread.
- Cystoscopy - used when cervical cancer invades the bladder, allows you to see its mucous membrane.
- Immunological analysis for cervical cancer - SCC, hCG, alpha-fetoprotein; It is recommended to study tumor markers over time
| Research: | Risk factors: | Risk factors for other gynecological oncopathologies: |
|
|
|
Where can tests be done?
Analysis for tumor markers can be done for a fee in independent laboratories, for example, “Invitro”, “Hemotest”, etc., state municipal medical institutions and private medical centers. Each institution has its pros and cons, but the optimal option remains independent laboratories, where, in addition to high-tech equipment and the absence of queues, test results are ready in the shortest possible time.
Let's consider which diagnostic institutions you can contact in Russia:
Center for Molecular Diagnostics "CMD", Moscow, st. Novogireevskaya, 3a.
Price:
- SA 15-3 - 780 rubles;
- REA - 780 rub.;
- CA 125 - 740 rub.
The duration of the study of the listed tumor markers is 1 day, and the analysis can also be carried out urgently - within 3-5 hours. In this case, the amount for each antigen is doubled.
Clinical diagnostic laboratory "LabStory", St. Petersburg, st. Furniture, 35/2.
Price:
- SA 15-3 - 824 rubles;
- CA 125 - 824 rubles;
- REA - 840 rub.
The Invitro network of independent diagnostic laboratories is widespread in the regions of Russia. Let's look at where you can conduct research on tumor markers using the example of individual cities:
- Ekaterinburg, st. Azina, 39;
- Voronezh, Leninsky Prospekt, 124B;
- Samara, st. Moskovskoe highway, 12.
The cost of research in the regions of the country differs slightly, since they are carried out within the same Invitro laboratory. Prices for tests will be as follows:
- SA 15-3 - 845 rubles;
- CA 125 - 735 rubles;
- REA - 825 rub.
Can cancer be detected by blood?
Unfortunately, a blood test for cancer does not 100% allow you to see cancer cells, but there is a certain degree of probability of identifying the diseased organ. Blood is precisely the liquid that interacts with all tissues and cells in the human body, and it’s clear that by changes in the chemical or biochemical composition one can determine what is wrong with a person.
The analysis gives a signal to the doctor that processes in the body are not proceeding correctly. And then he sends the patient for additional diagnostics of certain organs. Using blood, you can identify in which organ the tumor may live, at what stage and what size. However, if a person additionally suffers from any diseases, then the accuracy of this study will be lower.
What blood tests show cancer?
- Total (clinical) - shows the total number of red blood cells, platelets, white blood cells and other cells in the blood. Deviations from the general indicator may also indicate a malignant tumor.
- Biochemistry - usually shows the chemical composition of the blood. This analysis can more accurately determine in which place and in which organ a person develops cancer.
- Testing for tumor markers is one of the most accurate tests for oncologists. When a tumor develops in the body and cells in a certain place begin to mutate, then this thing itself releases certain proteins or tumor markers into the blood. This protein is foreign to the body, which is why the immune system immediately begins to try to fight it. The tumor markers for each tumor are different and can be used to determine in which organ the enemy has settled.
Complete blood count and cancer
A clinical blood test should be taken by men and women at any first incomprehensible symptoms of any disease. This can be done in almost any medical facility. As we have already found out, a complete blood count shows the condition of the blood based on the number of cells. Any change in the amount of hemoglobin, leukocytes, blood sugar and ESR for no apparent reason indicates a hidden disease.
What is diagnosed in this analysis? Usually these are the blood cells themselves and their number:
- Erythrocytes are red blood cells that deliver oxygen to all cells in the body.
- Platelets are cells that clog any wounds and clot blood.
- Leukocytes - roughly speaking, your immunity, cells that fight viruses, germs and foreign bodies.
- Hemoglobin is a protein that contains iron and is involved in the delivery of oxygen to tissues.
What could indicate cancer?
- ESR level (Erythrocyte Sedimentation Rate) - Usually, when this indicator is higher than normal, it indicates that an inflammatory process is occurring in the body. There are quite a lot of leukocytes, and they begin to attach to red blood cells and pull them to the bottom, which is why the sedimentation rate increases. in 25-30% of cases, when the ESR is elevated, it means that there is cancer in the body.
- Any change in the number of leukocytes due to oncology - there are two options. If there are very few of them, then in this case the organs that produce them are damaged and there is a suspicion of oncology in the bone marrow area. At elevated concentrations, it may also indicate a malignant tumor, as leukocytes begin to fight its antibodies.
- Decreased hemoglobin - usually accompanied by a decrease in platelet count. Then the blood clots poorly, and this indicates leukemia. Hemoglobin helps deliver oxygen to the cells of the body, and when there is less of it, then not enough oxygen reaches the cells, which causes some problems.
- A large number of immature cells - as the name suggests, these cells have not developed into a full-fledged healthy cell. For example, when they are just born, they are quite large, and after that they should acquire a normal size, but the problem with underdeveloped cells is that they live very little and then quickly die.
- The number of other cells also decreases.
- Many granular and immature leukocytes.
- Lymphocytosis is a huge amount of lymphocytes and lymph in the blood.
How long to wait for the result?
After what period of time the analysis for tumor markers will be ready depends on the laboratory or clinic where the study is carried out. In most cases this takes 1 day.
Blood donation for tumor markers used to search for breast tumors is carried out not only in women, but also in men. Thanks to this study, it is possible to diagnose a malignant process at its inception stage, which will significantly increase the chances of recovery.
Are you interested in modern treatment in Israel? Thank you for taking the time to complete the survey. Everyone's opinion is important to us.
Are tumor marker tests reliable?
If the results of tests for tumor markers are performed and interpreted in a high-quality manner, in most cases they are indicative. A significant excess of their norm indicates the development of a tumor in a particular organ in the human body. However, deviations from the norm do not always indicate the development of cancer.
In some cases, an increase in tumor marker levels may indicate the presence of disorders that are not cancer. Sometimes an increase in standards indicates the development of benign tumors, the treatment of which does not require “heavy artillery.” In addition, an increase in tumor marker levels can be detected in various viral and infectious diseases - in such cases they speak of a false result.
From all the information you received in this article, we can conclude that tests for tumor markers cannot be a panacea in diagnosing cancer, but they are an excellent addition to the early diagnosis of this disease and are actively used to assess the effectiveness of treatment of oncological pathologies. Their results should always be deciphered by experienced specialists, and to confirm such an ailment as cancer, a comprehensive and comprehensive examination of the patient should always be carried out.
Rating: (votes - 1 , average: 5.00 out of 5)
Diagnosis of gastrointestinal cancer, normal
The tumor marker CA 19-9 normally does not rise above 37 units per milliliter.
It is higher than normal in case of malignant pathology in the stomach, large intestine, often the rectum, bile ducts and bladder, and pancreas. But it can be increased during inflammatory processes in the biliary tract, colitis. A study of these SA tumor markers, the deciphering of which is of great importance in the diagnosis of malignant tumors of the gastrointestinal tract, is carried out with the exception of inflammatory processes in the intestines or common bile duct, otherwise the results may be false positive.
In case of malignant pathology of the gastrointestinal tract, CEA tumor markers may increase, the interpretation of which should take into account that the indicator is affected by smoking, inflammatory processes in the liver, pancreas, obstruction of the gallbladder and lungs. Also, its significant deviation from the norm may indicate cancer of the urinary system, a perirectal malignant focus.
general description
- CA 125
- CA 15-3
- CA 19-9
- CA 72-4
- Cyfra 21-1
- Alpha fetoprotein (AFP)
- Carcinoembryonic antigen (CEA)
Tumor markers are protein structures with carbohydrate or lipid components, which, when present in tumor cells or blood serum, serve as an indicator of a malignant process in the body.
The study of tumor markers allows us to obtain valuable diagnostic information that allows us to assume the presence of a malignant neoplasm and select the optimal sequence of examination of the patient. It should be remembered that a negative result when determining tumor markers cannot in all cases be considered a sign of the absence of oncopathology. A number of tumor markers can manifest themselves both in a specific cancer disease and in a number of others. Often, an increase in tumor marker concentration appears much earlier than the clinical symptoms of the disease itself. In practical medicine, tumor markers are used mainly to monitor the course of the disease and the effectiveness of its treatment. How is the procedure done?
Blood is drawn from the ulnar vein. Testing for on-comarkers does not require special preparation.
CA 125
Carbohydrate antigen 125 (CA 125) is a specific marker for ovarian tumors.
Indications for the purpose of analysis:
- prognosis of the course of the disease;
- timely detection of metastasis;
- assessment of the effectiveness of therapy for ovarian cancer.
| Norm CA 125 | |
| 4.0-8.8×109/l |
Interpretation of results
Increased Ca-125 levels
Malignant neoplasms:
- ovarian cancer;
- uterine cancer;
- endometrial cancer;
- fallopian tube cancer;
- mammary cancer;
- pancreas cancer;
- rectal cancer;
- stomach cancer;
- lungs' cancer;
- liver cancer;
- bronchial cancer.
Non-oncological processes:
- polycystic ovary syndrome;
- endometriosis;
- adnexitis;
- peritonitis;
- pleurisy;
- chronic hepatitis;
- cirrhosis of the liver;
- chronic pancreatitis.
CA 15-3
Carbohydrate antigen 15-3 (CA 15-3) is a specific marker of breast tumors. The appearance of this marker in tests significantly precedes the appearance of symptoms of the disease.
Indications for the purpose of analysis:
- prognosis of the course of the disease;
- detection of early relapses;
- detection of metastases;
- treatment effectiveness;
- distinctive diagnosis of breast cancer and benign mastopathy.
| Norm CA 15-3 | |
| in serum - 9.2-38 U/l |
Interpretation of results
CA 15-3 Level Up
Malignant neoplasms:
- mammary cancer;
- bronchogenic cancer;
- stomach cancer;
- liver cancer;
- pancreas cancer;
- ovarian cancer;
- cervical cancer;
- uterine cancer;
- endometrial cancer.
Non-oncological diseases:
- benign diseases of the mammary glands;
- cirrhosis of the liver;
- pregnancy in the third trimester;
- autoimmune diseases.
CA 19-9
Carbohydrate antigen 19-9 (CA 19-9) is a marker of malignant tumors of the gastrointestinal tract. Not having high specificity, it is most sensitive to pancreatic cancer (in 82% of cases), tumors of the liver and biliary tract (in 76% of cases).
Indications for the purpose of analysis:
- monitoring the course of pancreatic cancer;
- timely detection of metastasis;
- assessing the effectiveness of pancreatic cancer treatment;
- observation of patients with probable recurrence of stomach cancer - in combination with CEA;
- CEA-negative colon tumors.
| Norm CA 19-9 | |
| in serum - 0-37 U/ml |
Interpretation of results
CA level increase 19-9
Malignant neoplasms:
- pancreas cancer;
- cancer of the gallbladder and bile ducts;
- bladder cancer;
- primary liver cancer;
- stomach cancer;
- rectal cancer;
- sigmoid colon cancer;
- mammary cancer;
- ovarian cancer;
- uterine cancer.
Non-oncological pathology:
- cirrhosis of the liver;
- cholecystitis;
- cystic fibrosis;
- hepatitis;
- cholelithiasis.
CA 72-4
Carbohydrate antigen 72-4 (CA 72-4) is a marker for stomach, ovarian and lung tumors, but is most sensitive to stomach tumors.
Indications for the purpose of analysis:
- timely diagnosis of stomach and ovarian cancer;
- assessment of the effectiveness of surgical treatment;
- prognosis for stomach, ovarian, and colorectal cancer.
| Norm CA 72-4 | |
| in serum - less than 6.9 U/ml |
Interpretation of results
CA 72-4 Level Up
Malignant neoplasms:
- stomach cancer;
- colon cancer;
- ovarian cancer;
- breast cancer;
- lungs' cancer;
- endometrial cancer;
- pancreas cancer.
Non-oncological diseases:
- pancreatitis;
- cirrhosis of the liver;
- pulmonary pathology;
- ovarian cysts;
- autoimmune diseases;
- gynecological diseases.
Cyfra 21-1
Cytokeratin 19 fragment (Cyfra 21-1) is the most specific marker of bladder cancer and non-small cell lung cancer. Particularly informative when simultaneously determined together with REA.
Indications for the purpose of analysis:
- timely detection of lung cancer;
- lung cancer prognosis;
- bladder cancer prognosis;
- monitoring the effectiveness of surgical treatment.
| Cyfra Standard 21-1 | |
| in serum - up to 3.3 ng/l |
Interpretation of results
Cyfra boost 21-1
Malignant diseases:
- bladder cancer;
- lung cancer;
- cervical cancer;
- malignant tumors of the head and neck;
- esophageal carcinoma.
Non-oncological diseases:
- chronic renal failure;
- chronic hepatitis;
- pneumofibrosis.
AFP (alpha fetoprotein)
Alpha-fetoprotein (AFP, alfa-Fetoprotein) is a marker of primary liver cancer in oncology.
Indications for the purpose of analysis:
- monitoring the course of the disease;
- timely detection of metastasis;
- assessment of the effectiveness of treatment;
- detection of metastasis in the liver;
- examination of risk groups of patients with liver cirrhosis, chronic HBs-positive hepatitis, α1-antitrypsin deficiency.
| AFP norm | |
| Adult men and non-pregnant women: 0.90–6.67 U/ml |
Interpretation of results
Increase in AFP indicators
Oncological pathology:
- primary liver cancer;
- teratoblastoma of the testes and ovaries;
- pancreas cancer;
- stomach cancer;
- colon cancer;
- lungs' cancer.
Somatic pathology:
- chronic hepatitis;
- cirrhosis of the liver;
- alcoholic liver disease.
Decrease in AFP indicators
- tumor removal;
- adequate antitumor therapy.
A repeated increase or insufficient decrease in AFP may indicate relapse of the disease or the onset of metastasis.
CEA (carcinoembryonic antigen)
Carcinoembryonic antigen (CEA, CEA, antigen CD66E) is a nonspecific tumor marker. It is practically not detected in the serum of healthy adults, including pregnant women. But in the presence of a tumor process, the concentration of CEA in the blood increases significantly. Marker of tumors and their metastases.
Indications for the purpose of analysis:
- timely detection of tumors during examination of risk groups;
- monitoring the course of the disease;
- detection of early relapses and monitoring the effectiveness of surgical treatment of colorectal cancer, tumors of the breast, stomach, and lung.
| REA norm | |
| from 0 to 6.3 ng/ml |
Interpretation of results
Increasing REA indicators
CEA indicator 20 ng/ml and above:
- colon cancer;
- rectal cancer;
- stomach cancer;
- lung cancer;
- mammary cancer;
- malignant tumors of the pancreas;
- metastases to the liver, bone tissue;
- tumors of the prostate, ovaries.
CEA indicator within 10 ng/ml:
- cirrhosis of the liver;
- chronic hepatitis;
- colorectal polyps;
- ulcerative colitis;
- chronic pancreatitis;
- tuberculosis;
- pneumonia;
- cystic fibrosis;
- renal failure;
- Crohn's disease;
- autoimmune diseases;
- heavy smoking;
- malignant tumors of the rectum;
- distant metastases after tumor surgery.
Tumor markers: decoding, norm for other substances in the blood
An increase in tumor markers is not always interpreted as a bad result. Sometimes this occurs due to increased decay of the malignant focus after treatment. This is a good indicator, as it indicates that the tumor is treatable.
The diagnosis is established only after a confirmatory biopsy from the relevant organ. The diagnosis is also confirmed by clinical and biochemical blood tests, X-ray and other types of examination. For example, lung cancer can be confirmed using fluorography or x-ray examination. Stomach cancer is obvious on gastroduodenoscopy. Malignant pathology of the kidneys and ovaries can be detected by ultrasound. Degeneration of the cervix is determined by vaginal examination. Cancer of the rectum and lower intestine can be confirmed by sigmoidoscopy.
As we see, tumor markers only help to identify malignant pathology, and in the early stages, but in no case are they a verdict. The diagnosis is made on the basis of many data, so you should not draw hasty conclusions on your own.
Brain
The most problematic area and a fairly rare type of cancer. The fact is that there is no specific tumor marker for the brain yet, and that is why all tests are carried out together for different types of antibodies - AFP, Ca 15-3, CYFRA-21.1, PSA. All these markers may belong to other organs, and therefore, after positive tests, it is worth turning to other research and diagnostic options.
In this case, a professional oncologist should decipher the analysis. It is also better to get tested several times to understand how the concentration of antigens has changed since the last time and to understand how the disease is progressing.
- What increases hemoglobin? List of foods that increase hemoglobin in the blood
- Increased heart rate during a cold – Treatment of hypertension
Reasons for an increase or decrease in the CYFRA 21-1 tumor marker
The question of what causes the deviation from the norm of this marker interests many. In clinical practice, the tumor marker cyfra 21-1 is most often elevated due to the development of the diseases listed above.
In addition, the appearance of elevated values may be influenced by a common cold or the patient’s violations in preparation for this test. It is considered more dangerous if the patient underwent surgery to resection an organ affected by cancer and cyfra 21-1, a tumor marker of epithelial tissues, decreased to reference values, and after a short time the antigen levels suddenly began to increase again. This situation indicates the beginning of a relapse of the disease.
What do blood tumor markers show?
Most often, tumor markers are used to monitor the effectiveness of treatment for an already detected tumor. If after surgery, chemotherapy or radiation the concentration of the tumor marker decreases, it is concluded that the treatment was successful. Sometimes the doctor recommends taking tumor markers at certain intervals. If their concentration begins to increase compared to the original, even remaining within normal limits, there is a possibility of tumor regrowth or metastases. Thus, based on the level of tumor markers, it is possible to individually select treatment and monitor relapses several months before their visualization using instrumental diagnostic methods: ultrasound, CT, MRI, etc.
There are about 20 cancer markers that doctors use in difficult diagnostic cases: when there are suspicious symptoms or when it is necessary to determine the “evil” or “good” nature of a hard-to-reach tumor. However, these tests are prescribed only if the possibilities for more reliable cancer diagnosis have been exhausted.
Tumor markers are sometimes used for screening, but only among people at high risk of cancer. For example, the CA 125 tumor marker is used for the primary diagnosis of ovarian cancer in women at risk: those who have a genetic predisposition. In this case, a CA 125 test is prescribed annually in combination with ultrasound and monitored over time. The analysis can be positive for uterine fibroids, ovarian cysts, inflammatory processes in the pelvis and abdominal organs, at the beginning of pregnancy and in some other cases. However, it is worthwhile in women at high risk of cancer, although it is not useful in the general population.
A serious problem in oncology is intestinal cancer - this is one of the most common types of malignant neoplasms, the early stages of which are asymptomatic. There is a great temptation to use tumor markers for early diagnosis of this disease. However, all existing tumor markers for colon cancer give an unacceptably high number of false-positive results. They are used only to monitor treatment, monitor patients in remission, and track relapses. To screen for intestinal cancer, a simple and cheap stool test for occult blood (not a tumor marker) is currently used. According to studies, this measure reduces the risk of death from colorectal cancer by a third, as it allows the tumor to be suspected at a time when it can be cured.
The only blood test for cancer that can be taken as part of screening is a test for prostate cancer - the PSA tumor marker.
Pancreas
Tested for two types of tumor markers:
- Calcitonin - with elevated levels indicates medullary cancer. By the excess of this marker, you can see both the size of the tumor and the approximate stage of development.
- Thyroglobulin - Does not show exactly what stage the tumor growth is in the human body - relapse or metastasis, but it already determines problems with the thyroid gland even in the early stages.
Subsequence
- We donate Ca242 and Ca19-9 (released in the bronchi). Previously, they tested only the first one, but then it turned out that an increase in this marker could be due to a cyst, pancreatin, or other non-cancerous formations in this area.
- If the previous markers are elevated, then you need to donate blood for CA 72-4.
- For an even more accurate analysis, CA 50 is taken; it is more sensitive than the previous ones, and is also specific only for the pancreas.
Tumor markers for women
Among the many tumor markers, the norm for the female half of humanity is to check only a few of them - specific to their body.
For example, marker HE 4 is a special “flag” for malignant lesions of the ovarian and endometrial structures. In addition, its concentration will not increase with endometriosis and other gynecological pathologies, as well as benign neoplasms, for example, cysts.
If the tumor marker is elevated, in 80-90% of cases, ovarian cancer is then diagnosed at an early stage of its formation. In addition, the parameter is important for monitoring anticancer therapy for pelvic epithelial tumors and their relapses diagnosed at the preclinical stage.
With regard to atypia in breast tissue, CA 15–3 has the greatest specificity. However, for confirmation, information is also taken from other studies, for example, ultrasound, mammography, CEA marker. In practical medicine it is recommended to use it for the following purposes:
- assessment of the effectiveness of antitumor therapy for breast carcinoma;
- early diagnosis of metastases;
- differential diagnosis with mastopathy.
And a few more important tumor markers
What other tumor markers there are and what they mean is extensive material for study. Not all of them are used in the practice of oncologists.
Squamous cell carcinoma antigen is a marker of cancer at various locations. For example, it must be included in a set of diagnostic procedures when differentially distinguishing the benignity or malignancy of an identified lesion. In the absence of cancer, its high concentration may indicate insufficiency in the renal structures, asthma, and disruptions in the functioning of the biliary tract. Normally, parameters in people of different ages and genders should not exceed 1.5 ng/ml.
A marker with a similar focus - to identify alarming conditions in organs, an oncological tendency in them - is Cyfra CA 21-1. It is recommended for examination if a squamous cell carcinoma is suspected in the respiratory, urinary or gynecological systems. It helps in differential diagnosis and monitoring of ongoing antitumor treatment, but is not at all specific. You should focus on its normal indicators not exceeding 3.3 ng/ml.
The level of markers of neuroendocrine origin, for example, neuron-specific enolase, can increase both during inflammatory processes in the structures of the central nervous system, and after trauma and oncopathology. Significant numbers can help monitor the effectiveness of treatment measures for diagnosed small cell lung carcinoma or suspected neuroblastoma in children. Concentrations up to 16.3 ng/ml are considered not elevated.
However, with all the diversity, only a specialized oncologist should decide what tumor markers show and what the final diagnosis will be. Self-diagnosis is not acceptable.
What are tumor markers?
The formed cancer focus does not pass without leaving a trace for the full functioning of the human body. Cancer cells necessarily produce specific proteins. They will be shown by a study prescribed by a specialist - donating blood for tumor markers.
This analysis is a kind of express method that allows you to make a preliminary diagnosis. If a failure actually occurred in any organ, as indicated by the parameters of the analysis performed, the specialist will recommend more specific examination methods, for example, tissue biopsy.
Therefore, when asked by an anxious patient what a tumor marker is and for what purpose it was prescribed, specialists explain everything in detail during a preliminary consultation.
Tumor markers are proteins and other tumor waste products that arise as a result of the formation of cancer and tumors in various tissue areas. In fact, tumor markers are also present in the body of a healthy person, although their level always fluctuates within a certain healthy range.
But here it is necessary to emphasize that it is in a healthy person, since it happens that the level of these markers increases with other diseases, or with exposure to various chemicals and medications.
So this analysis does not always provide exact certainty that the patient has cancer, and it happens that the analysis is either false negative or false positive. But at the moment, this is the only method that is used to diagnose tumors in the first stages.
How does the analysis determine where the focus is? We will try to explain more clearly. As you probably know, all cancerous malignant or benign tumors can be located on almost any tissue: skin, brain, pancreas, etc.
Mutation of cells on each type of tissue gives rise to its own tumor. This tumor begins to grow and releases certain hormones and tumor markers, as well as waste products, into the blood. From the composition of these products, laboratory doctors can understand where the cancer appeared.
The tumor itself secretes several substances:
- Antigens
- Enzymes that are produced as a result of the growth and activity of cancerous tissues
- Blood plasma proteins and breakdown products of cancer cells, as well as other nearby cells.
The presence of all these antigens will indicate the presence of a tumor in the body.
Be healthy!
Thyroid cancer
As already mentioned, a tumor marker is a protein secreted by cancer cells and some healthy cells. It is found both in urine and in the blood. For thyroid cancer, blood is donated for the following tumor markers:
- “Calcitonin”—can be found in the patient’s blood or urine. Used in the diagnosis of modular cancer. Its concentration depends on the formation and period of the pathological process.
- “Thyroglobulin” is a protein that collects in the follicles of the thyroid gland. It is the main marker in the diagnosis of relapse of malignant tumors.
- “CEA” (carcinoembryonic antigen) – with thyroid disease, the tumor marker increases. It is determined only in blood serum.
How is this analysis carried out?
Testing for tumor markers is indicated to detect or rule out cancer in the human body.
The most accessible biological media for analysis are blood and urine. They are most often taken to identify cancer markers. The list of them is large and varied, therefore, the conditions for conducting analyzes have their own characteristics. Sometimes pleural fluid, prostate juice, punctate from the abdominal cavity and other body media are used. The study is carried out using special equipment using specific reagents at a certain temperature. Methods for conducting analysis for tumor markers and deciphering its results are available only to specialists. Patients only need to comply with the conditions for submitting it correctly and entrust the interpretation of the data to a competent doctor.
Test cost
You can also take in vitro tests in private clinics that provide this service. The average cost of analysis is about 3,000 rubles. Some laboratories offer comprehensive reference tests for men and women, where several types of tumor markers are compared.
All tumor markers known today can be divided into two groups:
- Specific. They indicate that an oncological process is definitely present in the body and help determine its type.
- Nonspecific - show the possible presence of an oncological process, but may also indicate that there is inflammation of an organ in the body in the absence of oncology.
The specific ones include:
- CEA is a tumor marker used to diagnose problems in the large intestine and rectum. If it is present in the analysis, it is possible to predict the further dynamics of the tumor, obtain the necessary information about the parameters of the malignant neoplasm and establish the period of growth.
- “CA 242” indicates pathology of the large intestine, pancreas and rectum at fairly early stages. Based on the results of this examination, tumor formation can be predicted 3–5 months in advance.
- “CA 72-4” is a tumor marker whose name is known to many laboratory technicians. It is surrendered together with REA. If antibodies are present, this indicates damage to the cells of the lungs and colon during the formation of small cell cancer.
- “M2-RK” this marker reflects metabolic processes in cancer cells. Its main feature is the lack of specificity when examining organs, which is why it is called a “marker of choice.” The test is used as a special metabolic indicator, since this tumor marker for intestinal cancer indicates the disease in the early stages.
Non-specific ones include:
- "AFP" (alpha fetoprotein) - demonstrates the presence of a neoplasm in the sigmoid and rectum.
- “CA 19–9” - (carbohydrate antigen) identifies pathology that is located in the pancreas, esophagus, gall bladder and ducts of the large intestine.
- The interpretation of the tumor marker “CA 125” in this case indicates the presence of an oncological process in the sigmoid colon. It should be noted that this marker is more often used for female ailments. It is often detected during inflammation in the peritoneum, in the presence of ovarian cysts, and during menstruation.
- “CYFRA 21-1” - an increased amount of this protein indicates problems in the rectum.
- “SCC” is an indicator indicating damage to the rectal canal by an oncological tumor.
- “LASA-P” - the presence of an increased number of this marker notifies about a malignant neoplasm in the intestinal organs.
In fact, in public clinics you can take it for free under your policy. But recently they have often started asking for money. Typically the price varies from 300 to 1000 rubles per analysis.
How many days does the analysis take? On average from 1 to 2 days. If the laboratory itself is located at the clinic of your attending physician, then in certain situations they can do it faster.
DETAILS: What to take if you have high blood sugar
How much can you trust tumor markers? You must understand that there is no 100% accuracy here, and tests may give different results depending on the equipment. Plus, this is influenced by a large number of factors from the person himself: alcohol, smoking, etc. So this is of course a great way to check, but it must be comprehensive with other diagnostic methods.
How often should I get tested? Once a year for ordinary patients and patients with other diseases. Once every six months for prevention, for those who are at high risk of cancer.
Varieties
Usually, when taking tests, the doctor prescribes several tumor markers at once. The fact is that several antigen indicators can indicate one disease at once, just as one marker can be isolated from cancerous tissues of different organs.
- The main one is a tumor marker, which is highly sensitive and can detect a tumor in the early stages, but can belong to different tissues.
- Secondary - a marker with low sensitivity, but a narrower specialization. Usually, several secondary markers are used at once along with the main one for more accurate results.
Mainly used are oncofetal tumor markers or proteins that are mostly found in the tissues of the embryo. They are necessary for the normal construction of internal organs and the growth of the child in the womb. An adult should have less of these proteins.
| Tumor location | Onomarkers |
| Brain | NSE, protein S100 |
| Nasopharynx and ear | SCC,REA |
| Lungs | NSE, CYFRA 21-1, REA, SCC |
| Liver | WUA, CF 19-9 |
| Pancreas | Tumor marker CA 19-9, CA242, CEA |
| Colon | REA, SA 242, SA 19-9, Tumor M2-PK |
| Multiple myeloma | B-2 Microglobulin, Immunoglobulins (igG, igM, igA, igE) |
| Prostate | PSA, Free PSA |
| Testicle in men | Tumor marker AFP (AFP), tumor marker hCG, CA 125 |
| Bladder | Bladder Cancer Marker - UBC, Cyfra 21-1 |
| Lymphoid system | B-2 microglobulin, firritin |
| Thyroid | Calcitonin, Thyroglobulin, CEA |
| Esophagus | SCC, REA |
| Breast | SA 15-3, REA |
| Stomach | Antigen Ca-72-4, REA, CA-19-9 |
| Adrenal glands (Pheochromocytoma) | Catecholamines (adrenaline, norepinephrine, dopamine) |
| Bud | Tumor M2-PK |
| Ovaries in women | SA 125, NE-4, SA 72-4, REA |
| Uterus (Endometrium) | CA 125 |
| Cervix | SCC, REA |
| Skin (Melanoma) | Protein S-100 |
| Gallbladder | SA 19-9 |
What are the most common types of cancer and tumor markers?
| Name | Most specific marker | Other markers | Purpose of the study | Use for early stage/screening diagnostics | The need for additional diagnostic methods |
| Bladder cancer | BTA, NMP22 | CEA, CA 125, CA 19 9 | Monitoring treatment, detecting relapses | No | + (cystoscopy, biopsy, cytological examination of urine) |
| Breast cancer | CA15 3, CEA | CA 27.29 | Treatment control | No | + (mammography, tomography, biopsy) |
| Rectal cancer | SEA, SA 19 9 | — | Monitoring treatment, detecting relapses, assessing prognosis | No | + (colonoscopy, sigmoidoscopy, feces for occult blood) |
| Liver cancer | AFP | — | Diagnostics, treatment control | No Yes | + (biopsy, ultrasound, tomography) |
| Lungs' cancer | CEA, NSE | TPA | Monitoring treatment, detecting relapses | No | + (X-ray studies, tomography) |
| Melanoma | TA 90, SU 100 | — | Metastasis, progression | No | + (biopsy) |
| Ovarian cancer | CA 125 | SA 72-4, LASA-P, AFP | Monitoring treatment, detecting relapses | No/screening for high-risk groups | + (ultrasound, biopsy) |
| Pancreas cancer | SA 19 9 | PAP, PSMA | Monitoring treatment, detecting relapses | No | + (ultrasound, tomography) |
In 2/3 of patients, AFP alpha-fetoprotein often increases, which is a tumor marker of liver cancer and increases as the tumor process grows. In addition, this liver tumor marker increases in acute and chronic hepatitis, and sometimes in ovarian or testicular cancer, but this category of patients accounts for no more than 5%.
With the development of multiple myeloma or lymphomas, beta - 2 - microglobulin is determined and it is this tumor marker that is prognostic for survival.
The presence of CA 15 3 and CA 27.29 indicates breast cancer, but at the initial stage of the disease they exceed the norm slightly. As it progresses, the rate increases.
CA 125 indicates ovarian cancer and is elevated in most patients; it is this tumor marker of ovarian cancer that allows a preliminary diagnosis to be made at the stage of medical examination. But it can also be elevated in other gynecological diseases or lung cancer, as well as in cancer survivors. CA 72-4 and LASA-P are also detected as a marker of ovarian cancer, but they can also be present in gastrointestinal oncology.
CA 19 9 is characteristic of damage to the pancreas, as well as with the effectiveness of treatment. This marker may increase in cases of intestinal or bile duct cancer.
Indications of tumor markers and diagnosis of the disease
What does a tumor marker blood test show and how much can you trust it? Of course, this analysis will not show the complete picture of the disease, but an increased level of tumor markers gives reason to suspect the development of pathology in the body and prescribe specialized types of tests, as well as the necessary examination (ultrasound, MRI and others).
Localization of tumors and corresponding markers
Note. More often, a tumor marker is used to monitor an already developed disease and to monitor ongoing treatment. Increased or decreased levels of tumor markers may indicate progression or, conversely, attenuation of the process.
If the level of tumor markers is elevated in a blood test taken during a medical examination, what does this mean? The presence of a cancerous tumor is not at all necessary; an increase can occur with a benign neoplasm, with some pathological processes in the pancreas and liver. There are other situations when the analysis shows a good tumor marker, but cancer develops in the body.
Important! A blood test for a tumor marker is not 100% proof of the presence of cancer; it is only a reason for further action.