Pneumothorax is defined as the presence of air or gas in the pleural space, such as the space between the visceral and parietal pleura, which can impair oxygenation and ventilation in the lungs. Clinical results depend on the degree of lung collapse on the affected side. If the pneumothorax is significant, it may cause mediastinal shift and compromise hemodynamic stability. Air can enter the intrapleural space through a chest injury or from the side easily, which is observed in some complex pathologies.
- Causes of pneumothorax development
- How is the disease classified depending on the leading factor?
- Symptoms of pneumothorax development
- Surgical treatment for gas accumulation in the pleural cavity and possible complications
Causes of pneumothorox
Depending on the origin, spontaneous primary and secondary, traumatic, iatrogenic pneumothorax are distinguished.
Primary spontaneous
It forms without any apparent reason. His reasons:
- Congenital weakness of pleural tissues , rupturing when coughing, laughing, or increased stress;
- genetic defect – insufficient production of α-1-antitrypsin;
- a sharp drop in pressure (when flying on an airplane, diving).
Worried about possible complications from severe pneumonia? Choose the best antibiotic for pneumonia! Does your child have sinusitis that cannot be treated? What to do in this case can be found here.
Secondary
Develops more often in older people with lung diseases:
- Chronic and hereditary (bronchial asthma, cystic fibrosis, COPD);
- infectious (pneumonia, tuberculosis);
- oncological x (lung cancer).
Traumatic
The causes are injuries:
- Open - cut, stabbed, gunshot;
- closed - received during a fight, falling from a great height.
Iatrogenic
Formed during surgery:
- During ventilation;
- cardiopulmonary resuscitation and;
- puncture of the pleural cavity.
Causes of pneumothorax
The causes of pneumothorax can be divided into 2 groups:
Mechanical injuries of the chest and lungs:
- Open and closed injuries;
- Complications of diagnostic and treatment procedures, for example, insertion of a catheter and puncture;
- Artificially induced pneumothorax (this condition can be induced artificially for the purpose of diagnosing and treating tuberculosis).
Diseases of the chest cavity and lungs:
- of a specific nature;
- non-specific nature
Pneumothorax, the causes of which can be different, requires prompt and effective treatment.
Symptoms (signs) of pneumothorax
Depending on the volume of incoming air, the speed of its penetration and the amount of collapse of the lung, the magnitude of the manifestation of symptoms can vary significantly.
The most characteristic symptoms:
- Chest pain is sharp, unexpected, intensifies when inhaling. May spread to the abdomen, shoulder, neck;
- shortness of breath - sudden difficulty breathing;
- cardiopalmus;
- increased sweating – sticky, cold sweat;
- pale or bluish skin – due to insufficient blood circulation;
- cough - paroxysmal, dry;
- panic fear;
- emphysema under the skin is possible - as a result of air entering the subcutaneous tissue.
Symptoms
With intestinal pneumatosis, symptoms appear that are also characteristic of other diseases associated with the gastrointestinal tract. They depend on the number and location of cysts, stage and duration of the disease. In some cases, gases are dispersed throughout the intestines.
This disease is extremely rare, so it is quite difficult for specialists to recognize all its symptoms with maximum accuracy. Its main symptoms are pain and excessive bloating. An excess of gases in the stomach stretches its walls - after this colic or pain appears in the form of contractions.
Infants and young children with pneumatosis experience vomiting, diarrhea, flatulence, and poor health. Since the pressure in the peritoneum constantly increases, after some time the formed cysts begin to crack. This threatens intestinal rupture and the development of peritonitis. In this case, the symptoms are more pronounced:
- severe pain begins in the peritoneum;
- your health deteriorates sharply;
- blood pressure decreases;
- the skin turns pale;
- there is no peristalsis.
Then the patient is overcome by a state of shock, and if treatment is not started in a timely manner, even death is likely.
Types of pneumothorax
Depending on the communication with the external environment, the following types are distinguished:
- Closed – there is no communication with the environment, the amount of air entering is constant. The mildest type, often resolves spontaneously;
- open – there is a relationship with the environment. Lung functions are significantly impaired;
- valvular - characterized by the formation of a valve that allows air to enter the pleural cavity, but does not let it out. With each inhalation, the volume of air in the cavity increases. The most dangerous type is when the lung stops functioning, pleuropulmonary shock develops, blood vessels are compressed, the heart and trachea are displaced.
Complications
The prognosis for pneumothorax is favorable. The air in the pleural cavity resolves within 3-5 weeks, and complete recovery occurs.
Pneumothorax is often complicated by the development of exudative inflammation of the pleura with the accumulation of hemorrhagic and serous-fibrinous effusion.
The dangerous consequences of pneumothorax are: adhesions that disrupt the expansion of the lung; bleeding into the pleural cavity from the affected vessel; hemothorax; pyothorax; sepsis; rigid lung; purulent melting of the pleura.
Long-term pneumothorax often ends with the replacement of lung tissue with connective tissue, shrinkage of the lung, loss of elasticity, development of pulmonary and heart failure, and death.
Diagnostics
The possible rapid development of pneumothorax requires rapid diagnosis to provide timely assistance. Diagnostic methods:
- Clinical examination - identifying characteristic symptoms, listening with a stethoscope to identify the affected area;
- X-ray examination - on the X-ray, a clearly separated zone of clearing without a pattern of the lung is visible on the periphery. The heart, trachea, large vessels are shifted to the opposite side, and the diaphragm is shifted down;
- Computed tomography is more reliable than x-rays. Used to diagnose small lesions, identify the cause, and in differential diagnosis;
- blood test - hypoxemia is detected in 75% of cases.
X-ray for pneumothorax
Pathogenesis of pneumothorax
The pathogenetic classification identifies three groups of pathological conditions, which is based on the presence or absence of communication between the pleural space and the air environment:
- Closed (no message);
- Open (there is a message);
- Tense (message depends on inhalation and exhalation).
Each of these pneumothoraxes has its own pathogenesis (mechanism of formation).
The occurrence of closed pneumothorax
With a closed pneumothorax, air is sucked into the pleural space through a temporary defect in the pleura, after which it becomes blocked for various reasons.
The appearance of such a temporary defect can occur:
- If the outer (parietal) layer of the pleura is damaged.
Such pneumothorax occurs with penetrating chest injuries, when the defect is subsequently closed due to displacement and post-traumatic swelling of the soft tissues;
- If the internal (visceral) layer of the pleura is damaged.
This pathological process develops as a result of blunt trauma to the chest, when broken ribs during breathing injure the visceral layer of the pleura and lung tissue.
When the pathology is closed, as a rule, a small volume of air enters the pleural space, which often resolves on its own.
Pathogenesis of open pneumothorax
With open wounds of the chest or when the respiratory structures are damaged by a foreign body or during medical procedures, an open pneumothorax develops. Through the defect formed in the pleural layer, air freely enters the pleural space when inhaling and is pushed out of it when exhaling.
In this case, intrapleural pressure is compared with atmospheric pressure, so gas exchange in the alveoli of the lungs is sharply disrupted.
In this case, there is a decrease in the amount of oxygen (hypoxemia) and an increase in the amount of carbon dioxide (hypercapnia) in the blood. Thus, respiratory failure increases. Often such conditions are accompanied by significant hemorrhages into the pleural cavity - hemothorax.
The mechanism of development of valvular pneumothorax
In the development of valvular pneumothorax, the formation of a flap, which plays the role of a valve, is of primary importance: when inhaling, it allows air to pass in the direction of the pleural cavity, and when exhaling, it covers the defect of the pleural layer, preventing it from coming out.
Tension pneumothorax occurs:
- Internal (with the involvement of lung tissue as a flap);
- External (the flap is the parietal pleura or soft tissue of the chest wall).
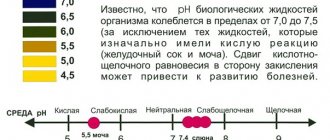
In the pathogenesis of pneumothorax, a sharp increase in intrapleural pressure is of great importance. Normally, when inhaling, it should be from -8.5 to 9 mm Hg, and when exhaling - from -3 to -6 mm Hg.
Intrabronchial pressure is positive during expiration (1-5 mm Hg), and can increase sharply when talking (up to 10 mm Hg), screaming or coughing (up to 70 mm Hg).
Thus, the difference between intrapleural and intrabronchial pressures during exhalation is up to 12-15 mm Hg. at rest and up to 80 mm Hg. when coughing or screaming. If a person has bronchial obstruction (narrowing of the lumen), this further increases the pressure gradient.
The valve mechanism increases intrapleural pressure, which as a result becomes the same as in the bronchi, or even exceeds it. It is in such cases that tension pneumothorax occurs, which is characterized by respiratory and hemodynamic disturbances.
The pathogenetic classification of pneumothorax is of great importance for determining the treatment tactics for a patient with this pathology. Pneumothorax is a life-threatening condition and therefore requires emergency surgical treatment in most cases.
Treatment
Therapy includes first aid and subsequent medical care.
Does your child have frequent, severe bronchitis? Then you should definitely find out how to treat bronchitis in a child correctly! Stuffy nose, night cough and headaches just don't go away? It could be sinusitis. Find out its signs and start effective treatment!
First aid for pneumothorax
Any pneumothorax requires emergency hospitalization in the surgical department.
A sudden pneumothorax requires emergency medical care, as it is a threat to human life. Not a minute of delay is acceptable!
An ambulance is called immediately when symptoms appear. While waiting for her, the patient is given first aid:
- Ensuring free air access;
- calming the patient;
- ensuring a semi-sitting position for the patient;
- in case of open pneumothorax , a sealed bandage is applied to the hole (from a sterile bag, adhesive plaster, rubberized fabric or polyethylene);
- in case of valve disease , a pleural puncture is urgently performed to eliminate trapped air using a needle and a large syringe.
Qualified medical care
Treatment is carried out in a surgical hospital and depends on the type and course of the pathology:
- A small, closed, limited pneumothorax most often does not require treatment. It resolves spontaneously after a few days without causing serious disorders;
- when closed - aspiration of trapped air is carried out using a puncture system;
- if open , first transfer it to closed, suturing the hole. Next, the air is sucked out through the puncture system;
- in case of valve disease , it is transferred to an open form using a thick needle and then treated surgically;
- for recurrent cases , surgical removal of its cause.
Flowchart of the organization of medical care based on the results of a clinical examination
Effective treatment of the disease
Pneumothorax is life-threatening. This applies to the valve shape and the open one. These options require immediate hospitalization. But, even before the medical team arrives, it is necessary to provide the patient with first aid.
Actions should be aimed at preventing further filling of the pleural cavity with air.
When the form is open, it is necessary to apply a compression bandage to prevent air from entering the injured area. To do this, cover the injury site with any material.
For better sealing, wrap the top with more plastic (bag, oilcloth). The patient must be seated to facilitate breathing, brought out of a state of fainting, and given an anesthetic.
In the hospital, a puncture is performed to remove accumulated air from the pleural cavity and to avoid the build-up of negative pressure in the pleural area.
Further treatment of pneumothorax will depend on its type. With a limited, closed form, conservative therapy is carried out.
It consists of providing the patient with rest and blocking severe pain syndromes with painkillers. According to indications, a pleural puncture is performed.
In case of a total variant of the disease, for normal expansion of the lung, drainage is placed in the pleural area and air is aspirated using a special apparatus.
To relieve cough syndrome, codeine or dionine is prescribed. All patients undergo oxygen therapy, which accelerates the resolution of pneumothorax several times. Pain relief is carried out with analgesics, sometimes even narcotics.
Surgery is required if most of the lung is damaged due to trauma. The defect in the lung tissue and soft tissues of the injured part of the chest are sutured, and a drainage tube is installed.
Measures are being taken to stop the bleeding. Surgical treatment will also be required in the absence of the effect of conservative measures. If the drainage has been in place for a week, and the lung has not expanded, then you can’t do without a surgeon.
To reduce the risk of recurrence of the disease, chemical pleurodesis is prescribed. Chemical pleurodesis is the filling of the pleural cavity with special chemicals that promote closure of the spaces between the pleural plates.
Prevention
There are no specific preventive measures in this case.
Primary
Based on maintaining the health of the whole body:
- Complete smoking cessation;
- regular long walks;
- performing breathing exercises;
- timely diagnosis of lung diseases and their treatment;
- avoiding chest injury.
Secondary
Its goal is to prevent the development of relapses:
- Fusion of pleural layers;
- removal of the cause of the disease.
How is the disease classified depending on the leading factor?
Spontaneous pneumothorax is usually studied in detail in search of a treatment approach that ranges from observation to active intervention. Primary spontaneous pneumothorax occurs due to the absence of underlying lung disease and provoking factors, among others. In other words, air enters the intrapleural space without prior trauma and without a basic history of the clinical form of lung disease.
However, many patients referred to as primary pneumothorax often have subclinical lung disease causing the presence of pleural blebs that can be detected by computed tomography (CT). The classic patient for this form of the disease is usually 18-40 years old, tall, thin, and often a heavy smoker.
Secondary spontaneous pneumothorax occurs in patients with a wide range of lung parenchymal diseases . Patients have an underlying pulmonary pathology that alters the normal structure of the lungs. Air enters the pleural cavity through stretched or damaged alveoli. The clinical presentation of these patients may include more severe symptoms and complications due to comorbidities.
Iatrogenic pneumothorax is essentially traumatic because it occurs due to damage to the pleura and is secondary to a diagnostic or therapeutic procedure. Half a century ago, iatrogenic pneumothorax was predominantly the result of deliberate injection of air into the pleural space to treat tuberculosis.
Traumatic pneumothorax from blunt trauma or penetrating injury results from disruption of the parietal or visceral pleura. The treatment steps for traumatic pneumothorax are similar to those for treating illness resulting from non-traumatic causes. If the injury causes communication of the pleural cavity with the external environment or leads to hemodynamic disturbances, drainage of the pleural cavity is performed to remove air, which allows the lungs to open.
There is a subset of traumatic varieties of pneumothorax classified as atypical - they may not be visible on x-ray, but can be distinguished on CT. In short, pathological processes of pneumothorax can be observed and treated if they manifest themselves symptomatically.
Tension pneumothorax
This type of pneumothorax is a life-threatening condition that occurs when air is trapped in the pleural cavity under positive pressure. Air masses displace mediastinal structures and damage cardiac function. Saving a patient's life is only possible in a modern intensive care unit. Because tension pneumothorax occurs infrequently and has potentially devastating results, a high index of suspicion, knowledge of basic emergency thoracic decompression procedures is important for all healthcare providers. Immediate chest decompression is mandatory if tension pneumothorax is suspected. The situation requires immediate radiographic confirmation.
Pneumomediastinum
Pneumomediastinum represents the presence of gas in the tissues of the mediastinum; it appears there spontaneously, after a medical procedure or injury. Pneumothorax may occur secondary to pneumomediastinum.
Forecast
The prognosis is significantly influenced by the type of pathology and the speed of assistance:
- In case of spontaneous uncomplicated pneumothorax , with timely assistance provided, the prognosis is favorable;
- in the presence of pulmonary pathology , frequent relapses are possible (in almost half of the cases);
- with traumatic pneumothorax - the prognosis depends on the injuries received;
- with valvular pneumothorax - the sooner the patient is in the hospital, the more favorable the prognosis.
Pneumothorax
– a serious, potentially fatal condition. In any case, emergency care and emergency hospitalization are required. If characteristic symptoms of pneumothorax develop, you should immediately call an ambulance, then treatment will be carried out by a thoracic surgeon and pulmonologist.
Clinical picture of pneumothorax
The diagnosis can be confirmed and treatment tactics determined only by taking an x-ray. But the symptoms of the disease are quite vivid; their severity is influenced by the causes of the disease and the degree of collapse of the lung.
It is difficult to confuse an open pneumothorax - a person is forced to lie down on the injured side, air is noisily sucked in through the wound while inhaling, and foamy blood comes out when exhaling.
Symptoms of the spontaneous development of the disease are pain on the side of the chest where the lung is damaged, paroxysmal cough, shortness of breath, tachycardia, cyanosis.
The patient characterizes the pain as dagger-like, piercing. It radiates to the neck and arm and intensifies with inhalation. Sometimes symptoms such as sweating, drowsiness, anxiety, and fear of death occur.
When examining the chest, a lag in breathing on the damaged side is visible. During auscultation on this side, breathing can be heard weakly, or not at all.
Symptoms of the presence of air in the pleural cavity in newborns and babies up to 12 months are anxiety, difficulty breathing, puffiness of the face, shortness of breath, cyanosis, sudden deterioration in condition, refusal to eat.
The closed form of the disease is sometimes asymptomatic.
Helping patients with open pneumothorax
First aid for open pneumothorax is to prevent air from entering the chest. In order to stop this process, an occlusive bandage is applied to the area of injury - a sealed bandage that does not allow air to enter.
To apply it, you need sterile napkins, a bandage, airtight material (oilcloth, cellophane), and an antiseptic solution.
Rules for effectively applying an occlusive dressing:
- Make the victim sit facing you, calm him down and explain your further actions.
- Wear gloves, conduct a visual inspection of the injury site, determine where air enters the pleural cavity.
- Treat the skin with an antiseptic.
- Place sterile wipes and secure them with an adhesive plaster or bandage.
- Cover the injury site with oilcloth or plastic wrap.
- Finish bandaging.
To prevent the development of painful shock, subcutaneous or intramuscular injections of painkillers are given. To support the heart - adrenaline, atropine. To replenish blood loss, a drip with special infusion solutions is connected to replenish the BCC (circulating blood volume). To ensure airway patency, the victim is given oxygen therapy (oxygen supply) or artificial ventilation.
The victim is urgently hospitalized in an upright position (sitting).
In a hospital setting, first aid for pneumothorax is aimed at removing air from the chest.
First, the person undergoes primary surgical treatment of the wound surface - the edges of the wound are excised, damaged and dead areas are removed, if there are foreign bodies, they are removed. This manipulation performs three functions:
- ensures asepsis (sterility) of the wound;
- promotes rapid healing;
- prevents the development of infectious complications.
Then they begin decompression of the pleural cavity - elimination of the air cushion. To do this, drainage is carried out according to Bulau.
If the lung is mechanically damaged and its anatomical integrity is compromised, the patient undergoes surgery - thoracotomy . This is a surgical opening of the chest for the purpose of a detailed examination of the organs of the chest cavity. If the lung is damaged, resection or suturing of the wound is performed.
Thoracotomy leads to complications in 10% of cases. Patients develop severe pain, requiring the use of narcotic painkillers to relieve pain. In the postoperative period there is often bleeding and suppuration.
Suturing the wound
Suturing a lung wound is a surgical operation to restore the integrity and functionality of the lung. To carry it out, there are some difficulties associated with suturing the pulmonary parenchyma. A weak connective tissue frame leads to the fact that after a needle puncture, the wound channel around the suture thread increases in diameter and fills with air and blood. Additional damage is caused when attempting to tie a knot. The thread cuts into the lung tissue, causing trauma.
The purpose of the operation is to ensure the tightness and physiological constancy of the lung . To do this, the seam is placed deep. It is better if the sutures are applied to the still compressed and collapsed organ. To do this, use an atraumatic needle and silk thread.
Lung resection
Traumatic damage to the parenchyma leads to its enlargement and destruction. To stop this process, surgical intervention is required. Lung resection is the excision and removal of part of an organ . Part of the lung is removed in lobes (lobectomy) or segments (segmentectomy). You can delete multiple beats or segments at once.
If at the time of injury the affected area is small, marginal resection is performed. The affected tissue is removed from the outer surface of the lung.
The operation can lead to complications, although they are not common. During surgery, there is a risk of severe bleeding associated with the dense blood network in the lung parenchyma .
Postoperative complications:
- pneumonia;
- atelectasis - compression of the walls of the organ;
- respiratory and heart failure as a consequence of decompensation of the body and its adaptation to new conditions.
Diagnosis of pneumothorax
To diagnose the disease, special instrumental studies are carried out, which include:
- chest x-ray (to detect pneumothorax and determine the degree of lung collapse);
- puncture of the pleural cavity (to detect sealing and lung compression syndrome);
- thoracoscopy (to indicate the cause of the disease).
When examining the patient, characteristic signs of pneumothorax may be revealed, such as:
- decreased blood pressure, displacement of the heart border to the healthy side, tachycardia;
- expansion of the chest and spaces between the ribs, limitation of chest excursion on the affected side;
- cold sweat, cyanosis, shortness of breath.
When diagnosed, the patient usually takes a forced semi-sitting or sitting position, which is also a symptom of pneumothorax.
Clinic
When interviewing and examining the patient, the doctor pays attention to sudden chest pain, shortness of breath, rapid breathing and heartbeat, and dry cough. Acute attacks of fear can also be a consequence of pneumothorax. The types of injuries and the nature of the damage, sometimes even detected visually, will help to finally determine the diagnosis and refer the patient for treatment. This can be either a surgical or a therapeutic hospital or an intensive care unit. It all depends on the severity of the condition and the specifics of the damage.
Causes
Rupture of pulmonary or bronchial tissues occurs for the following reasons:
- Mechanical injuries
are the main cause. Injuries can occur in a car accident, hitting the ground during a fall, or during a fight; - chronic lung diseases
– , COPD, ; - congenital pathologies of the lungs and pleura
- leading to their ruptures during intense physical and respiratory stress; - surgical procedures
- ventilation.
Diagnosis of pathology
Most often, diagnosing pneumothorax is not difficult. For pneumothorax, the following diagnostic methods are particularly informative:
laboratory blood tests;
- radiography;
- electrocardiography;
- ultrasonography;
- CT scan.
A general blood test does not reveal any special pathological changes in this disease. In the presence of concomitant bleeding in the peripheral blood, a decrease in the number of all blood cells and a drop in hemoglobin levels can be detected, which indicates blood loss.
The greatest changes are detected when studying the gas composition of the blood. In 75% of patients, pathological changes in blood gases are observed: hypoxemia (a drop in the partial pressure of oxygen in the blood below 80 mm Hg) and hypercapnia (an increase in the partial pressure of carbon dioxide above 50 mm Hg).
Pathological changes in the gas state of the blood are directly proportional to the volume of air accumulated in the pleural cavity and the degree of collapse of the lung. A critical decrease in oxygen content in the blood indicates a severe degree of acute respiratory failure, which can lead to the development of hypoxic coma.
Radiological signs of pneumothorax, identified on a plain x-ray, are:
- Detection of the air gap between the layers of the pleura.
Absence of a lung pattern on the affected side of the chest.
- Displacement of the shadow of the mediastinal organs (heart, bronchi, large vessels) to the healthy side.
- Fluid level (effusion) in the lower parts of the pleural cavity.
- When performing radiography with the patient lying down on the affected side, a deep costophrenic groove is determined.
X-ray examination can be supplemented with computed tomography.
In case of severe hemodynamic disturbances, an electrocardiographic study is required. The ECG will show signs of overload in the right side of the heart.
Classification
Depending on the causative factors, pneumothorax is divided into:
- Post-traumatic
- is a consequence of traumatic injuries to the chest. - Spontaneous
- develops independently in healthy people or those with a history of chronic pulmonary pathology: abscess, gangrene, emphysema, or. - Iatrogenic or artificial
pneumothorax is the result of medical procedures.
Pathogenetically, the disease is classified into forms:
Tin disinfection of the area around the drainage tube. The thread cutting of the waiting thread is composed by the waiting node. The patient requires forced removal. Draw the drainpipe quickly while helping the waiting thread. In case of pneumothorax, the drain tube is suppressed when the lung is dilated and there is no loss of air, and for hemotaxis or empyema, the drain tube will be withdrawn when no more blood or pus has been removed and there is no loss of air.
Spontaneous general right pneumothorax. The appearance of correct post-plurotomy is expansive lungs. Direct thoracic trauma with fractures C2 - C6. Correct aspect of vision. Expansive lungs. Horvath T. - Elements of surgical pathology - Notes for the course at the Faculty of Medicine, Ed.
- Closed
is the mildest type of pneumothorax, in which there is no communication with the external environment. - Open
– characterized by depressurization of the respiratory system. Air enters the pleural cavity during inhalation and is removed during exhalation, without accumulating in the body.
Other medical products about: Surgery
Medical information is for informational and educational purposes only.
They cannot replace a doctor's consultation or a diagnosis established after research and medical tests by a specialist. It is often ineffective and has disadvantages: the possibility of pleural infection. Risk of lung damage and relapse. Pleural catarrh through the intercostal space or bed after resection of the coastal fragment. Suction drainage can be passive or active. Accidents and accidents are more common after pleurotomy:. - pleural shock; - anaphylactic shock; - parietal bleeding; - long-term damage with hemorrhage and vectors; - injuries of the mediastinal organs; — penetration of the diaphragm with subfrene; - subcutaneous emphysema. Open pneumothorax
- Valve
- air enters the pleural cavity through the wound and does not leave it.
It is concentrated between the pleural layers, intrapleural pressure increases rapidly. Further progression of the pathology ends with damage to the neurovascular bundles and compression of the second lung. Valvular pneumothorax turns into tension pneumothorax - the most dangerous type of pathology, leading to the death of the patient.
Intercostal neuralgia; - insufficient drainage; - unilateral pulmonary edema through severe re-interpretation of the lung. Pulmonary remission edema is a very rare complication, the pathogenesis of which has not yet been published, and the evolution is impressive. The indicated treatment is intubation of the patient, bronchospasm, and concomitant administration of steroidal anti-inflammatory drugs. Surgical treatment itself is practiced when: constant loss of air; Surgical techniques used: Excision or ligation at the base of the blisters, whether or not associated with apical pleunectomy.
Tension pneumothorax
According to localization, pneumothorax can be unilateral (left- or right-sided) and bilateral.
According to the degree of collapse of the lung:
- Partial or limited collapse
- the lung collapses by 1/3, - Subtotal collapse
- the lung collapses by ½, - Total collapse
- the lung collapses by more than ½ or is completely compressed by air.
If the pleural cavity contains blood in addition to air, then they speak of hemopneumothorax, if pus - pyopneumothorax.
Abrasion, including the diaphragmatic pleura, other than the mediastinal pleura, with or without sympathetic agents. Atypical resections of the affected area of the lung. Surgical interventions can be performed either by classical thoracotomy, sternotomy, or minimally invasive methods.
As risk factors for recurrence we recall: more than one episode in the past. Loss of air for more than 48 hours before the first episode. Radical air cysts. To reduce the risk of recurrence, in addition to the abrasion and pleurectomy techniques indicated in open thoracic surgery, in the case of tube drainage, autologous intrapleural autologous instillation may be used in addition to heterologous syphilis agents.
Mechanism of occurrence
The natural state of the slit-like space near the lungs implies the presence of negative pressure. This condition is necessary for the functioning of the respiratory system.
After damage to the layers of the pleura, internal (bronchus or lung rupture) or external (chest injury), air fills the pleural cavity. This leads to the fact that the pressure inside the slit-like space increases, that is, one of the following situations arises:
- pleural pressure comes into line with atmospheric pressure;
- pleural pressure is higher than atmospheric pressure.
These circumstances lead to the fact that air entering the pleural zone compresses the lung. A similar effect causes respiratory dysfunction. If the volume of compression is large, then both lungs are affected - the damaged and the healthy.
The influence of air on the lungs entails displacement of the mediastinal organs (a complex of organs located in the area between the right and left pleural cavities). This means that the heart and large blood vessels can become dislodged, affecting circulation.