Transient ischemic attack is often a precursor to ischemic stroke. Some patients experience transient attacks over a long period of time, which, if not treated appropriately, can lead to death. Therefore, if a characteristic clinic occurs, you should definitely consult a doctor.
A transient ischemic attack (TIA) is an acute episode of temporary neurological dysfunction that results from focal cerebral, spinal cord, or retinal ischemia and is not associated with acute tissue infarction. Clinical symptoms of TIA usually occur for less than 1 hour and most often last no more than 30 minutes. In rare cases, prolonged episodes of seizure may occur.
A transient ischemic attack most often develops against the background of atherosclerotic occlusion of large vessels of the brain, that is, when atherosclerotic plaques completely block the blood flow at the branching site of the carotid arteries, the internal carotid artery or vertebral arteries.
The assessment of TIA is based on a neurological examination of the patient, which focuses on neurovascular diagnosis. The presence of other diseases that may complicate the course of TIA is also taken into account. Once intracranial hemorrhage has been ruled out, antithrombotic therapy begins.
Video TRANSIENT ISCHEMIC ATTACK - A PREDICT OF STROKE
Main reasons
Transient ischemic attack (TIA) is a reversible condition that does not lead to organic brain damage. Among the causes of its development are atherosclerotic lesions of cerebral vessels. Atherosclerosis of intracerebral and extracerebral arteries is detected in 50-60% of patients. Atherosclerotic plaques can independently block the lumen of the carotid, vertebral or cerebral arteries, and can serve as a source of thrombotic masses. The latter, entering the vessel, cause its persistent occlusion, disrupting the blood flow.
In 15-25% of patients, the cause is elevated blood pressure. Long-term hypertension causes structural changes in blood vessels. In some cases, high blood pressure and atherosclerosis are diagnosed in one patient, worsening his prognosis for recovery.
A common cause is cerebral thromboembolism. The source of blood clots is the heart. Thrombotic masses are formed in it during various types of arrhythmias, myocardial infarction, endocarditis, cardiomyopathy, congenital and acquired defects. With abnormalities in the development of the heart muscle, transient attacks of ischemic origin can be detected in childhood.
In addition to the above reasons, the following can lead to TIA:
- inflammatory arterial diseases: Takayasu's disease, antiphospholipid syndrome, etc.;
- dissection of the vascular wall as a result of head injuries and chronic inflammation;
- diabetes mellitus and other endocrine diseases;
- disorders of the blood coagulation system, etc.
In neurology, there are a number of risk factors that contribute to the occurrence of ischemic brain damage:
- high level of total cholesterol in a biochemical blood test;
- smoking and alcohol abuse;
- obesity of any severity;
- low physical activity;
- arterial hypertension;
- diabetes.
If one risk factor is present, the likelihood of a TIA increases by 10%. If there are two or more factors, the risk increases by 30-49%. In this regard, prevention of the development of ischemic attack is based on their correction.
Prevention
Although there is no reliable research demonstrating the effectiveness of lifestyle changes in preventing TIAs, many health care professionals recommend them. These include:
- No bad habits (smoking)
- Reducing fats to help reduce the amount of plaque formation
- Eating a healthy diet that includes plenty of fruits and vegetables
- Limiting sodium in your diet helps lower blood pressure
- Dosed consumption of alcohol, stimulants, sympathomimetics, etc.
- Maintaining a Healthy Weight
In addition, if you have cardiovascular diseases, it is important to keep them under control, especially if these are the following pathological conditions:
- High blood pressure
- High cholesterol
- Atrial fibrillation
- Diabetes
Classification of pathology
In neurology, 3 classifications of TIA are used: based on the location of the lesion, frequency of occurrence and severity. When examining the bloodstream, doctors distinguish the following types of disease:
- with damage to the carotid arteries;
- with damage to the vertebrobasilar arteries;
- with bilateral and multiple lesions;
- transient cerebral ischemic attack, unspecified.
Depending on the blockage of a particular vascular branch, this classification can be refined. Separately, transient blindness syndrome and transient global ischemia are distinguished.
Based on the severity of clinical signs, the following degrees are distinguished:
- mild - symptoms last less than 10 minutes;
- moderate severity - up to 2-3 hours;
- severe - up to 24 hours.
A common cause of transient ischemic attacks is cerebral thromboembolism.
The frequency of transient ischemic attacks affects the treatment and prevention of ischemic stroke. Therefore, all cases of the disease are divided into three options:
- rare - no more than 2 times a year;
- medium frequency - no more than 6 times a year;
- frequent - more than 6 times a year.
These classifications are used to diagnose the disease in each patient individually. Based on the identified pathology options, treatment and rehabilitation methods are selected.
Classification
TIAs with a clinical picture of vascular damage in the vertebrobasilar area account for about 70% of diagnosed attacks. Taking into account the duration of the attack, mild, moderate and severe forms are distinguished. In the first case, an ischemic attack lasts up to 10 minutes, in the second - up to several hours with the elimination of symptoms after the attack, in the third - several hours with the persistence of residual symptoms after the end of the attack. The diagnosis of TIA is made if the duration of the attack does not exceed 24 hours, and the neurological and autonomic disorders are reversible.
Clinical manifestations
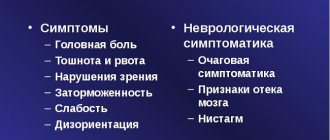
The main symptom of TIA is neurological impairment that lasts up to 24 hours. Doctors most often learn about the clinical signs of the disease from the patient’s words, since by the time he goes to a medical institution, the symptoms disappear.
Symptoms of transient ischemic attack depend on the location of the lesion:
- TIA involving the carotid arteries most often manifests as visual impairment. The patient may notice a decrease in visual acuity, loss of individual visual fields, or complete blindness on one side. In addition, motor and sensory disorders of the arms and legs of a unilateral nature are often observed. In rare cases, unilateral convulsive syndrome is possible.
- TIA involving the vertebrobasilar region is characterized by disruption of the cerebellum. The patient exhibits a shaky gait, instability in a vertical position, and dizziness of varying severity. Speech disturbances are characteristic, as are motor and sensory disturbances in the legs and arms.
- When the arteries supplying the retina are damaged, a syndrome of transient blindness occurs. It is short-term and affects one eye. In some cases, loss of individual fields of vision is possible. Due to the small diameter of the retinal arteries, cases of TIA are common.
With transient global amnesia, the patient suddenly loses memories of the past. The localization of the ischemic focus is difficult to establish; apparently, a transient disruption of the blood supply occurs in the hippocampus and other subcortical structures. There is a characteristic connection between memory impairment and psycho-emotional stress and severe pain. Amnesia captures small fragments of the past, and after blood circulation is restored, memory is completely restored.
Differential diagnosis
Diagnosing this pathology is difficult for several reasons:
- Firstly, the disappearance of symptoms. A TIA attack lasts a maximum of a day, but can end in less than 10 minutes.
- Secondly, the manifestations of the attack are similar to the manifestations of other diseases, for example, epilepsy, migraine, multiple sclerosis, stroke, hypertensive cerebral crisis, hypertensive crisis, etc. Therefore, it often remains unspecified.
To clarify the diagnosis, neurologists resort to differential diagnosis.
Its principle is to compile a list of diseases that have similar symptoms and search for specific manifestations of any pathology in the patient.
If a TIA is suspected, use:
- collecting anamnesis (paying attention to diseases that manifested themselves in relatives);
- examination in otolaryngology and cardiology (symptoms may resemble hearing or heart diseases);
- blood tests (general, biochemical);
- blood clotting analysis (TIA pathogenesis is characterized by an increase in blood viscosity);
- instrumental diagnostic methods (ECG, EchoCG, computed tomography, duplex scanning, MRI).
MRI (if this method is not available, then computed tomography) is the most accurate way to differentiate this disease. In case of TIA, no focal changes should be detected on the transcript; if they appear on the images, then the pathology has already reached the stage of stroke.
Complications
In the absence of adequate first aid and subsequent treatment, the patient may develop the negative consequences of a transient ischemic attack. These include the following conditions:
- development of microstroke, characterized by organic damage to small areas of nervous tissue in the absence of clinical manifestations;
- ischemic stroke, which develops if the obstruction of a blood vessel is not eliminated or progresses, while organic changes occur in the brain - nerve cells die, swelling occurs and an inflammatory reaction develops;
- persistent neurological deficit, characterized by persistence of symptoms (the patient may experience impaired sensitivity or motor activity of varying severity);
- cognitive impairment: decreased memory, ability to concentrate, rapid mental fatigue, etc.
A transient ischemic attack increases the risk of developing an ischemic stroke in the future.
Complications can be prevented by promptly seeking medical help and starting complex therapy.
Consequences of TIA
The prognosis for TIA is favorable. Usually short-term failures are not life-threatening. Repeated attacks indicate the presence of provoking factors and indicate a high likelihood of a stroke. Statistics show that ischemic stroke is diagnosed in a third of patients who have suffered an acute attack of circulatory disorders.
Similar consequences of a transient (transient) ischemic attack occurring in the brain are observed within 1 month after the attack in 20% of patients. Within 1 year after the attack, stroke is diagnosed in 42% of patients. A person’s age and the frequency of attacks are decisive factors that determine the rate of onset of irreversible destructive changes in brain structures.
Diagnostic measures
The diagnosis of “Transient ischemic attack” is made according to a special algorithm and includes various diagnostic approaches:
- Collection of complaints available at the time of treatment, as well as symptoms that the patient noted in the past. These include headaches, dizziness, impaired coordination of movements, changes in speech, weakness and numbness in the arms and legs, etc. When collecting an anamnesis, it is necessary to find out what caused the clinical signs: heavy physical activity, drinking alcohol, emotional stress or the use of medications funds. Concomitant diseases are identified, primarily acute cerebrovascular accidents. Cases of TIA in the past, pathologies of the cardiovascular system and endocrine organs.
- Neurological examination, including the study of sensory, motor function, cognitive skills, etc.
- The list of laboratory tests consists of a clinical blood test, a biochemical blood test with determination of glucose levels, total cholesterol, low and high density lipoproteins, triglycerides, liver enzymes and bilirubin, urea, creatinine and blood electrolytes. According to indications, studies are carried out to identify rheumatic diseases: determination of autoantibodies, LE cells, etc.
- Electrocardiography with ultrasound of the heart in the presence of cardiac pathology.
- Ultrasound of extracranial vessels with Doppler sonography and duplex scanning can detect obstruction of the vertebral and carotid arteries. Methods are necessary to identify atherosclerotic plaques, thrombotic occlusions and vascular aneurysms. To clarify the diagnosis, it is possible to conduct cerebral angiography or MRI examination of the arteries of the brain.
- During the initial examination of the patient, a computed tomography scan of the head is performed to eliminate organic brain lesions (hematomas, intracerebral tumors, etc.). Also, CT can detect ischemic stroke, which can occur similar to TIA. To increase the accuracy of diagnosis and assessment of the condition of the brain, MRI is performed.
- PET (positron emission tomography) evaluates not only the structural integrity of the brain, but also the activity of metabolic processes in the nervous tissue. In specialized centers, this diagnostic method allows one to clarify the nature of ischemia and also identify micro-strokes.
Differential diagnosis of transient ischemic attacks is carried out with ischemic and hemorrhagic stroke, epileptic seizures and the onset of multiple sclerosis.
Diagnostics
The following vital signs are initially studied:
- Temperature
- Arterial pressure
- Heart rate and rhythm
- Breathing rate
- Oxygen saturation
In the process of assessing the general condition and appearance of the patient, his:
- Attentiveness
- Opportunity to interact with others
- Language and memory skills
- General hydration level
- General development
The purpose of the physical examination is to identify any neurological changes, evaluate cardiovascular risk factors, and look for a potential thrombotic or embolic source of the attack. Ideally, any neurological disorder should be recorded using locomotor tests (TWT, Hauser) and an integral scale (ADL, F1M).
During a neurological examination, the following will be examined:
- Function of cranial nerves
- Determination of somatic strength of the engine
- Somatic sensory testing
- Speech and language testing
- Evaluation of the cerebellar system (be sure to monitor the patient's progress)
It is important to exclude other causes, such as metabolic or drug-induced factors, which may present with signs similar to those of TIA.
Additionally, the following studies are prescribed:
- Blood glucose test
- General blood analysis
- The amount of electrolytes in the blood serum
- Coagulogram
- Standard electrocardiogram
The following tests may be performed urgently:
- Erythrocyte sedimentation rate
- Cardiac enzymes
- Lipid profile
If necessary, additional laboratory tests are carried out, which include:
- Screening for hypercoagulable states
- Serology of syphilis
- Antiphospholipid antibodies
- Toxicological factors
- Hemoglobin electrophoresis
- Serum electrophoresis
- Cerebrospinal fluid examination
Instrumental diagnostic methods allow you to obtain images of the brain, but they must be performed within 24 hours after the onset of symptoms:
- Magnetic resonance imaging (MRI) with diffusion-weighted imaging (preferred)
- Non-contrast computed tomography (CT, ordered if MRI is not available)
Imaging of the cerebral vasculature is often performed urgently, preferably in conjunction with brain imaging. Vascular imaging for TIA includes the following:
- Color Doppler ultrasonography
- CT angiography (CTA)
- Magnetic resonance angiography
Thus, timely and extensive diagnostics make it possible to make an accurate diagnosis and subsequently carry out highly effective therapy.
How to give first aid
First aid when symptoms of TIA occur is carried out by relatives or colleagues of the patient. First of all, you need to call an ambulance. Over the phone, you should describe in detail the symptoms that have arisen, as well as the reasons for their occurrence. The person is freed from tight clothing and belts, ensuring calm breathing. While waiting for an ambulance, the patient should lie on his back. Place a pillow or folded clothing under your head. It is not recommended to use medications on your own.
Emergency care for transient ischemic attack is provided only by doctors. It is based on eliminating the cause of the disease - lowering blood pressure, restoring respiratory function, etc.
Forecast of ischemic attacks
After a single transient ischemic attack, the consequences are unnoticeable and the symptoms disappear after a day, but the further prognosis is not always favorable - the tendency to re-develop TIA increases, and, under the influence of additional unfavorable factors, the following complications may occur:
- Transient ischemic stroke. The impaired blood flow is not restored after an hour and irreversible death of cellular structures occurs.
- Hemorrhagic stroke. If the wall is weak, a partially blocked vessel cannot withstand the increased blood pressure below the site of blood flow disturbance and it ruptures. The leaked blood permeates the brain structures, making it difficult for the cells to function.
- Visual impairment. If the lesion is localized in the vertebrobasilar system, then visual field impairment or a severe decrease in visual acuity may occur. When the disorder is located in the right artery basin, the SMA will be left-sided, but there is a high probability that visual function on the right will be affected and vice versa (vision in one eye will be preserved).
The prognosis is aggravated by the patient’s bad habits, the presence of concomitant diseases and risk factors, as well as old age.
Treatment approaches
Treatment of transient ischemic attack is a complex task aimed at preventing the development of stroke and restoring the functions of the nervous system. For this purpose, non-drug therapy and medications are used.
Various groups of drugs are used as drug therapy to eliminate the causes of TIA and prevent its complications. Treatment should be aimed at restoring blood flow through the cerebral arteries. It is recommended to use antiplatelet medications (Dipyridamole, Clopidogrel or Acetylsalicylic acid). In addition to antiplatelet agents, indirect anticoagulants (Phenindione, Ethylbiscoumacetate) can be used. The use of direct anticoagulants (Heparin, Fraxiparine, etc.) is contraindicated due to the risk of internal hemorrhages. Intravenous administration of glucose and combined saline solutions is necessary to improve the rheological properties of blood.
When the disease develops against the background of arterial hypertension, drugs that lower blood pressure come to the fore. The drug of choice is Captopril, which belongs to the group of ACE inhibitors. In addition, it is possible to use aldosterone receptor antagonists (Candesartan, Eprosartan), as well as beta-blockers (Esmolol, Propranolol). To improve cerebral circulation, Cinnarizine, Vinpocetine, Actovegin, etc. are prescribed.
An important stage of therapy is the prevention of the death of nerve cells associated with metabolic changes against the background of ischemia. The following drugs can be used as neuroprotective therapy:
- Magnesium sulfate;
- Glycine;
- Piracetam;
- Cytoflavin et al.
Treatment of TIA also includes symptomatic treatment. If vomiting develops, use Cerucal or Ondansetron. For headaches, Indomethacin, Ibuprofen, etc. are prescribed. Any medications should be used only after being prescribed by the attending physician, as they have contraindications. Otherwise, progression of the underlying disease or development of side effects of therapy is possible.
Non-drug methods
As a non-drug treatment, the patient must remain in the neurointensive care unit for 6 hours. During this period of time, he is under constant surveillance. The use of physiotherapeutic methods (oxygen barotherapy, electrosleep, microwave exposure) can improve metabolic processes in the body and have a positive effect on overall health.
In case of severe vascular occlusion, detection of large atherosclerotic plaques or aneurysms, surgical interventions may be performed to eliminate them. Operations are carried out after hospitalization and a comprehensive examination. Surgical interventions eliminate the cause of transient ischemic attacks, preventing their occurrence in the future.
Prevention of occurrence and recurrence of TIA
To prevent the development of transient ischemic attacks, you should follow the recommendations of specialists:
- take prescribed medications in accordance with the prescribed prescription;
- control blood pressure levels;
- monitor blood cholesterol levels;
- give up bad habits: alcohol and nicotine addiction;
- regularly take medications that prevent the formation of blood clots;
- be regularly checked by your doctor.
To prevent a transient ischemic attack from having consequences, you should lead an active and healthy lifestyle:
- eat on time and often;
- eliminate or reduce the consumption of fatty, smoked and salty foods;
- play sports: swimming, therapeutic exercises;
- spend more time outdoors.
If you adhere to all of the above, the prognosis for full recovery will be positive.
Author
Ekaterina Dmitrievna Abramova
Neurologist, director of the chronic pain clinic
Rehabilitation
Patients with TIA need rehabilitation measures aimed at restoring brain function. Rehabilitation is based on the following influences:
- Physiotherapy. The exercises are aimed at developing the motor functions of the arms, legs and facial muscles. Exercise therapy classes are conducted under the supervision of a specialist.
- Physiotherapeutic effects (electrophoresis, magnetotherapy, electrosleep, etc.) have a positive effect on the general condition of the patient.
- Massotherapy.
Long-term rehabilitation for transient ischemic attacks is not required, since brain functions recover independently. However, with frequent episodes, these rehabilitation measures can improve the patient’s quality of life.
General information about TIA
A transient attack is a short-term disruption of the blood supply to certain areas of the brain tissue, which leads to hypoxia and cell death.
Let's consider the main difference between a transient ischemic attack and a stroke:
- Development mechanism. With stroke lesions, there is a complete cessation of blood flow to the brain tissue, and during transient ischemia, insignificant blood flow to the brain area remains.
- Duration. Symptoms with TIA gradually subside after a few hours (maximum - a day), and if a stroke occurs, the signs of deterioration remain the same or progress.
- Possibility of spontaneous improvement of well-being. The ischemic attack gradually stops, and the function of the dead brain cells begins to be performed by healthy structures and this is one of the main differences from a stroke, in which, without medical assistance, foci of necrosis increase and the patient’s condition gradually becomes more severe.
It may seem that transient ischemic attack of the brain is less dangerous than stroke damage to brain tissue, but this is a misconception. Despite the reversibility of the process, frequent oxygen starvation of brain cells causes irreparable harm.
Preventive actions
Primary includes the elimination of correctable risk factors:
- Timely treatment of arterial hypertension using modern antihypertensive drugs.
- Quitting smoking, drinking alcohol and drugs.
- Therapy of diseases of the heart and blood vessels.
- Correction of lipid metabolism disorders with changes in diet and medications.
- Treatment of diabetes mellitus.
It is recommended to regularly engage in physical activity, normalize body weight and limit salt intake. Women with the above risk factors should not use oral contraceptives, which increase the risk of ischemic disorders.
Secondary prevention of TIA is aimed at preventing the recurrence of ischemic attacks. For this purpose, the patient must follow the doctor’s instructions for lifestyle changes, as well as use prescribed medications to correct concomitant diseases of the cardiovascular, endocrine and other systems. The patient is prescribed lipid-lowering therapy, antithrombotic and antihypertensive drugs.
Transient ischemic attack in the carotid vascular system
Most often, manifestations are associated with focal neurological symptoms and are often sensory disorders. It happens that the patient’s signs of a disorder are very minor, that he is not even aware of the existing problem:
- certain parts of the body become numb, as a rule, this is just one limb, but a hemianesthesia type occurs when the lower and upper limbs, located on the same half of the body, go numb;
- disturbances of motor function develop in the form of hemiparesis or monoparesis (when disturbances are determined in one limb or in two, located on the left or right half of the body);
- the development of speech disorders (cortical dysarthria, aphasia) is associated with damage to the hemisphere located on the left side;
- seizures are observed;
- Blindness in one eye may develop.
Forecast
The prognosis is determined by the severity and frequency of transient ischemia. If the symptoms are mild and occur up to 2 times a year, then the pathology does not have a significant impact on the duration and quality of life. With more frequent TIAs and attacks of moderate severity, the patient's risk of developing organic brain damage increases significantly. In this case, a person needs a comprehensive examination to identify the causes of ischemia (atherosclerotic plaques in the cerebral vessels, congenital malformations of the arteries, etc.) and their elimination.
With severe severity of transient ischemic attacks or frequent disorders of moderate severity, life expectancy is reduced due to the risk of developing ischemic stroke. It is important to note that in each case of a transient attack, the doctor must determine whether it is a microstroke or not. Micro-strokes lead to impairments in a person’s personality and intelligence, and are also a risk factor for stroke.
Treatment
Before prescribing appropriate treatment for patients with TIA, the following should be done urgently:
- Assessment of the patient's general condition
- Risk stratification
- Initiating stroke prevention
In patients with a recent (≤1 week) TIA, immediate hospitalization is recommended, especially if the following conditions are present:
- Symptoms last longer than 1 hour
- There are signs of carotid artery stenosis of more than 50%
- There is a credible source of embolus (eg, atrial fibrillation)
- Hypercoagulable state determined
Due to the high short-term risk of stroke after TIA, antithrombotic drugs are prescribed only after the intracranial hemorrhage has resolved. Suitable first-line option for initial therapy:
- Aspirin
- Aspirin plus extended-release dipyridamole
- Clopidogrel
The treatment regimen for stroke prevention is usually recommended for cardioembolic TIAs and is as follows:
- Patients with atrial fibrillation after TIA are prescribed long-term anticoagulation with warfarin and aspirin if one cannot take oral anticoagulants
- In acute myocardial infarction and left ventricular thrombus, oral anticoagulation with warfarin in combination with aspirin is prescribed
- For dilated cardiomyopathy, oral anticoagulation with warfarin or antiplatelet therapy is performed
- For rheumatic mitral valve disease, oral anticoagulation with warfarin is performed
For patients with TIA due to 50-99% stenosis of the main intracranial artery, the following is recommended:
- Aspirin, not warfarin
- Maintaining blood pressure below 140/90 mm Hg. Art. and total cholesterol levels below 200 mg/dL
Surgery
If a patient is considered at increased risk (for example, if the carotid artery is narrowed by at least 70%), surgery to widen the artery (called a carotid endarterectomy) may be performed to improve the patient's condition.
Carotid endarterectomy usually involves removing fatty deposits (atheroma or plaque) formed due to atherosclerosis and clots in the internal carotid artery. However, the surgery can cause a stroke because it often displaces clots or other material that can then travel through the bloodstream and block the artery. However, after surgery, the risk of stroke decreases for several years than with drugs.
Stents
If the patient is contraindicated for surgery, angioplasty with stenting may be required. For this procedure, a catheter with a balloon at its tip is inserted into the narrowed artery. The balloon is then filled with air and inflates within a few seconds, which helps dilate the artery. To prevent the vessel from becoming stenotic, doctors insert a wire mesh tube (stent) into the artery.
Symptoms and signs
An ischemic attack, the symptoms of which are similar to those of other diseases, causes panic in the victim. He cannot understand what happened to him. Symptoms of an attack vary depending on the area in which the disruption of blood flow to the brain occurs. These areas are called vascular territories. There are two main vascular regions - vertebrobasilar and carotid (or the area of the carotid arteries).
Impaired blood flow in the vertebrobasilar region of the brain is characterized by the following symptoms:
- dizziness;
- gag reflex and attacks of nausea;
- speech dysfunction;
- minor spasms of the facial muscles causing facial hardening;
- short-term visual impairment (fogginess and darkening of the eyes, inability to focus);
- decreased sensitivity of the skin;
- motor dysfunction;
- loss of orientation in time and space;
- panic attacks;
- short-term memory lapses, which are expressed by the inability to remember your name, age, place of residence.
If there is a circulatory disorder in the carotid region of the brain, the patient will experience the following symptoms:
- deterioration of skin sensitivity;
- violation of speech function (it becomes incoherent and incomprehensible);
- numbness and loss of mobility of the upper and lower extremities, sometimes numbness occurs on one side of the body;
- apathy;
- drowsiness;
- panic attacks.
Sometimes with both types of ischemic attack there is a severe headache. The patient panics, declaring that his head will explode from the pain.
An ischemic attack passes in a few minutes, but you should not relax, because it can recur soon and cause various consequences: in 15% of patients after the first attack of an ischemic attack in the first three months, and in 25% within a year, an ischemic stroke occurs. In 20% of patients who have had an ischemic attack, it does not recur for several years or never.
Symptoms of an attack disappear within 10-15 minutes, so it is recommended to remember most of the symptoms before the ambulance arrives or the victim is transported to the hospital independently. This will help the doctor make the correct diagnosis.
Causes
The main causes of this disorder:
- The presence of atherosclerotic plaques that disrupt the blood supply to large vessels.
- Disease of the cardiovascular system.
- Diabetes.
- Blood clot formation.
- Chronic increase in blood pressure.
- Aplasia.
- Osteochondrosis of the cervical segment.
- Hereditary predisposition.
- Atrial fibrillation.
- Having unhealthy habits.
- Age-related changes.
- Fabry disease.
When the first signs appear in the form of loss of consciousness, impaired communication, or paralysis of the limbs, it is necessary to immediately call a team of doctors to provide the patient with first emergency medical care.
Main features
You can understand that a transient ischemic attack has begun by the characteristic signs. Some people may confuse the symptoms with those of an ischemic stroke. But, again, let us remind you that the main difference between TIA is the rapid disappearance of negative signs.
Symptoms:
- Incessant noise in the ear.
- Glare in the eyes, bright spots.
- Feeling of nausea, vomiting is rarely possible.
- Pain in the head, with the symptom affecting mainly the back of the head.
- Problems with coordination.
- Intense dizziness.
- Changes in blood pressure.
- Memory problems are usually minor.
When a person has a transient ischemic attack, their skin becomes excessively pale. If you ask a patient with closed eyelids to touch his nose with his finger, the person will miss. People often complain of general weakness, as well as deterioration in the sensitivity of the limbs. In severe cases, a transient ischemic attack can lead to vision loss, speech impairment and seizures.
If symptoms of an ischemic attack of the brain appear, you should consult a specialist. He will conduct a professional diagnosis and, if necessary, send you for examinations. After them, it will be possible to unambiguously determine what kind of problem the patient had to face.
What is a transient ischemic attack of the brain? This condition is associated with a decrease in blood supply to the brain tissue. The flow of red blood cells does not stop completely, but is significantly limited. The location of the outbreak affects subsequent manifestations of the attack.
Common signs of a TIA include:
- severe tinnitus;
- flashes of light in the eyes;
- severe hiccups;
- nausea or vomiting;
- speech problems;
- pain in the back of the head;
- dizziness;
- severe headaches;
- coordination problems;
- convulsive state;
- blood pressure surges;
- transient amnesia.
Patients experience pale skin, absent-mindedness, and inability to concentrate. If the pathology is localized in the cervical region, then situational attacks cause the appearance of severe muscle weakness - the patient may fall, lose the ability to freely move the limbs, most often the victim is fully conscious. In severe cases, a person requires immediate emergency care.
The following symptoms are not typical for TIA:
- disturbance of consciousness;
- isolated deafness;
- fainting;
- flickering scotoma;
- isolated ringing in the hearing organs;
- acute behavioral changes;
- progression of sensory disorders.
A suspected diagnosis of transient ischemic attack requires taking appropriate measures to prevent further unwanted complications.
Prognosis for TIA
If you quickly respond to the symptoms, call an ambulance and perform timely therapy, TIA will have a regressive course and after a short time the person will return to normal life.
If you delay seeing a doctor, a TIA can develop into a heart attack or stroke. This worsens the prognosis, and there is a risk of disability or death. Advanced age, harmful habits and somatic disorders worsen the prognosis for recovery and increase the duration of the attack.
Blood supply to the brain
Blood supply to the brain
Anatomically, a special vascular “formation” is responsible for the blood supply to the brain - the Circle of Willis, from which all areas of the brain receive blood.
Clinically, the brain receives blood through two main vessels - the carotid and vertebral arteries. The carotid artery, for the most part, supplies blood to the tissue of the hemispheres and cortex. The vertebral artery basin (vertebrobasilar) carries blood primarily to the base of the brain and some components of its trunk (in particular, the cerebellum).
Thanks to this division, a transient ischemic attack can develop in any of these areas, leading to the development of a clinical picture typical for each type of attack.
The essence of the disease
There are several mechanisms for the development of acute cerebrovascular accidents and TIA in particular. But the most common is the following.
Microemboli and atheromatous masses that form in the carotid and vertebral arteries (they are the result of the disintegration of atherosclerotic plaques) with the blood flow can move into smaller vessels, where they cause blockage of the arteries. Most often, the terminal cortical branches of the arterial vessels are affected.
Atherosclerosis affects all vessels in the body, including cerebral arteries, which leads to TIA or ischemic stroke
These platelet and atheromatous masses are very soft in structure and therefore quickly dissolve. After this, the spasm of the artery is eliminated and blood flow in this area of the brain is normalized. All symptoms go away. Also, these microemboli may be of cardiogenic origin or be the result of problems in the blood coagulation system.
This process itself lasts only a few seconds or minutes, but pathological signs sometimes last up to 24 hours. This is due to swelling of the vascular wall due to its irritation, which disappears within a few hours after the acute period.
But, unfortunately, the development of the disease is not always so favorable. If the dissolution of blood clots and vascular spasm is not eliminated on its own within 4-7 minutes, irreversible changes occur in neurons that are under hypoxic conditions and they die. A stroke develops. But, fortunately, such strokes have a relatively favorable prognosis, since they are never extensive.
Recommendations
If the patient often has a transient attack, then you should not rely on drugs. It is imperative to follow the rules of protection. Much more depends on the lifestyle that the patient leads than on the use of medications.
It is recommended to follow the following rules:
Special diet
- Stop drinking alcohol and smoking.
- Nutrition should be anti-atherosclerotic. To do this, the doctor selects a special diet that you will have to follow for the rest of your life. It involves strictly limiting the consumption of foods with animal fat. All high-calorie foods are also prohibited. It is necessary to switch to vegetable oils. It is beneficial to eat lean fish and dairy products. You should always use more fruits and vegetables.
- Physical activity is mandatory. Of course, strenuous sports are not suitable, but you can do fitness, swimming, yoga, cycling, walking.
- You should always monitor your blood pressure. If you control it, you can avoid an ischemic attack. Indicators should be maintained at 120/80 mm Hg. If necessary, you need to take medications with antihypertensive properties, but a healthy lifestyle also plays a big role.
- Normal blood cholesterol levels should be maintained. To do this, you need to eat right, lead an active lifestyle, and take medications with lipid-lowering properties.
- If necessary, you should take medications that prevent the formation of blood clots. For example, Aspirin will do. However, you can start using it only after your doctor’s permission.
- It is necessary to carry out therapy against pathologies that are risk factors for ischemic attacks.
If you ignore the pathological condition, the situation will worsen over time. If you hospitalize the patient in time and carry out competent emergency therapy, the attack will gradually pass, and the person will be able to return to a normal lifestyle. However, in some cases the prognosis is disappointing. The pathology often leads to disability, as it causes ischemic stroke and cerebral infarction. In addition, there is a possibility of death.
Causes and factors contributing to temporary ischemia
If a person has had a transient ischemic attack, then it is worth thinking about improving their health. Otherwise, there is a risk of having a stroke, which can even be fatal. The doctor will need to understand why the person had an attack, because treatment will be aimed at eliminating the cause. Patients are also advised to reconsider their lifestyle in order to normalize their health.
Treatment for TIA can be gentle and is suitable in the absence of significant symptoms. The doctor may advise the patient to go for acupressure, as well as perform special physical exercises. These measures will improve your well-being, especially if you also undergo microwave therapy and electrophoresis.
Medicines are often used to treat the cause of a TIA. The doctor determines specific medications based on the patient’s characteristics. Antiplatelet agents such as aspirin and warfarin may need to be used.
Vasodilators such as cinnarizine and ticlopedine are effective. If there are deviations in the level of cholesterol, then Lopid or Nicolar is prescribed. The doctor may also prescribe clonidine as an antihypertensive medication.
If medications and strengthening procedures do not help and the person continues to suffer from transient ischemic attacks, then surgery will be required. This decision can be made by the doctor after analyzing the patient’s condition.
The essence of the procedure is that it is necessary to excise the fatty plug, which puts pressure on the artery. In addition, it is necessary to eliminate the affected area of the vessel. After these manipulations, angioplasty is performed.
Diagnostic methods
The most effective methods for identifying the current lesion should be considered magnetic resonance imaging, electrocardiogram, echocardiography - all these methods help to find the damaged area and detect even the early stages of vascular thrombosis.
If the diagnostic indicators are not satisfactory, the cardiologist may prescribe an additional study, which is carried out by more specialized specialists. In addition, one should take into account the fact that some external manifestations of the pathological condition in question may in many ways resemble the symptoms of organic and functional lesions. For example, diabetes mellitus and Meniere's disease have similar manifestations, which can reduce the effectiveness of the diagnosis. Therefore, after a course of general diagnostics, it is recommended to carry out a number of additional manipulations to make a more accurate diagnosis.
Which doctor should I contact?
If a TIA occurs, the patient must be hospitalized. The specialized department will be neurological.
After the main crisis period is over, the primary treating physicians for a patient who has had an attack will be a cardiologist and a neurologist.
Since solving the problem requires treatment of blood vessels and accompanying possible neurological consequences. Also, it is the cardiologist who gives recommendations on how to prevent possible recurrences of such conditions.
Transient ischemic attack in the carotid artery system
Symptoms of an ischemic attack develop within 2–5 minutes. If there is a disturbance in the blood flow in the carotid artery, then characteristic neurological manifestations appear:
- a feeling of weakness, movement of the arms and legs on one side becomes difficult;
- the sensitivity of the left or right side of the body decreases or is completely lost;
- slight speech impairment or its complete absence;
- sudden partial or complete loss of vision.
Most often, the development of TIA in the carotid artery system has objective signs:
- weakened pulse;
- when listening to the carotid artery, a murmur is noted;
- there is pathology of the retinal vessels.
Pathology of the carotid artery is characterized by symptoms of brain damage that are focal in nature. The manifestation of TIA is associated with certain neurological symptoms:
- the face becomes asymmetrical;
- sensitivity is impaired;
- pathological reflexes are noted;
- then an increase, then a decrease in pressure;
- the vessels of the fundus narrow.
Other signs of the development of such a TIA are interruptions in the functioning of the heart muscle, tearfulness, a feeling of heaviness in the chest, suffocation, and convulsions.
Consequences
The occurrence of a transient ischemic attack does not pose a particular threat to the patient’s health, but it signals many dangerous diseases.
After two or three attacks of TIA without proper treatment, an ischemic stroke most often develops, which is truly extremely dangerous not only for the patient’s health, but also for his life.
Approximately one patient out of ten experiences a cerebral stroke or heart attack after experiencing a transient ischemic attack. Many people, after suffering a TIA, especially a short-term one (if it lasted a few minutes), postpone a visit to specialists, which is extremely dangerous for their health.
Symptoms
Depending on the vascular basin where ischemia manifests itself, transient ischemic attacks occur in the carotid and vertebrobasilar basins (VBB).
Carotid and vertebrobasilar basin
Depending on the affected area, the location of the brain that lacks blood supply is determined.
And here neurologists divide symptoms into two types:
- General – nausea, pain and weakness, dizziness and loss of coordination, short-term loss of consciousness;
- Local – individual, depending on the affected area.
Based on local manifestations, the area affected by the thrombus is determined.
TIA in the VVB is the most common occurrence of short-term ischemia (occurs in 70 cases out of 100).
Accompanied by:
- Vestibular ataxia (imbalance of stability and coordination);
- Noises and spasms in the head;
- Increased sweating;
- Vomiting, nausea;
- Short-term amnesia;
- Visual dysfunction;
- Sensory disorders;
- Increased blood pressure;
- Very rarely - the onset of dysarthria.
TIA in the carotid region occurs:
- With visual impairment, monocular blindness (in the right or left eye) and goes away as the attack disappears (lasts a few seconds);
- With paroxysmal vestibular and sensory disorders - it is impossible to control the body due to loss of balance;
- Vascular visual disorders - occur in the form of decreased sensitivity or complete paralysis of one side of the body, and warns of a micro-stroke in this area;
- With convulsive syndromes, during which convulsions in the limbs, without loss of consciousness, independently bend and straighten the arms and legs.
TIA in the local area of the blood flow of the retinal artery, ciliary or orbital artery is prone to stereotypical repetition and is accompanied by:
- Transient blindness - visual acuity suddenly decreases, clouding occurs, colors are distorted, and a veil appears on one eye.
- Hemianesthesia , decreased muscle tone, the occurrence of convulsions, paralysis, which indicates a transient ischemic attack of the carotid arteries.
- Transitional global amnesia - occurs after a strong nervous shock or painful sensation. There is short-term amnesia of new information in the presence of very old information, absent-mindedness, a tendency to repeat, vestibular ataxia. TGA lasts up to half an hour, after which memories are fully restored. Similar attacks of TGA may recur several years later. A patient in a coma may experience the sail sign, which is so called because of the external resemblance to the swelling of the cheek on the side opposite the paralyzed one during breathing.
Article on the topic: Arterial hypertension against the background of thyroid pathologies
The difficulty in determining the diagnosis is that the symptoms of the attack are short-lived and the neurologist is forced to diagnose TIA only from the patient’s words , which will depend on the pathological zone of cerebral blood flow.
Despite the reversibility of the symptoms, it must be remembered that at the moment of the onset of spasm, the arteries carrying oxygen and vital substances stop the processes.
Energy is not produced, and the cells suffer from oxygen starvation (temporary hypoxia is observed).
Symptoms in humans with brain hypoxia
Damage to the body from an attack will depend on the area of the affected area, but even small local attacks will cause considerable harm to health.
Signs of aortic cerebral attacks
The occurrence of pathological processes in the blood circulation in the aortic area before the bifurcation of the carotid and vertebral vessels is marked by symptoms:
- Photopsia, diplopia;
- Noise in the head;
- Vestibular ataxia;
- Drowsiness and decreased physical activity;
- Dysarthria.
The disorder may occur with congenital heart disease.
And if there is an increase in blood pressure, then the following are observed:
- Headache;
- Vestibular ataxia;
- Weakness in the limbs;
- Nausea and vomiting.
Symptoms of an attack become more pronounced if the patient begins to change head positions and the risk of TIA increases (Table 1).
| Risk of ischemic stroke after TIA (according to the AVSD scale) | ||
| Index | Signs | Grade |
| HELL | above 140/90 Hg. | 1 |
| Age | over 65 years old | 1 |
| Manifestation | weakness, numbness of one of the limbs | 2 |
| dysarthria without limb impairment | 1 | |
| other | ||
| Duration of symptoms | over 1 hour (severe, occurs due to irreversible cerebral deformation) | 2 |
| up to 1 hour (moderate, in the absence of any residual effects after the paroxysm) | 1 | |
| less than 10 minutes (mild) | ||
| For a patient who has previously been diagnosed with diabetes mellitus | 1 | |
| Maximum number of points on the scale: 7 points. | ||
Effective treatment
As soon as symptoms characteristic of ischemic attacks appear, you must immediately call an ambulance and tell them about the patient’s complaints. If the symptoms are mild, you can seek advice from a neurologist, but this should be done as early as possible, because there is a possibility that attacks will intensify and reoccur frequently. In an inpatient setting, the patient will be examined additionally by a cardiologist, a vascular surgeon and an ophthalmologist. After an attack, you need to visit an endocrinologist to rule out the development of diabetes. It is imperative that you consult a nutritionist to choose the right treatment.
For transient ischemic attacks, therapy is aimed at preventing stroke. Therefore, it is necessary to go to the hospital as early as possible, and not wait until a severe form of the attack appears, its recurrence, or even the stroke itself.
Hospitalization is required only if the attacks become more frequent, due to which the patient’s ability to work is sharply impaired. If an examination has been carried out, and attacks occur rarely, then you can be treated at home, but you need to constantly visit the hospital, as the doctor will monitor the process.
Treatment of transient ischemic attack involves the following:
Tromboass
- It is necessary to thin the blood. For this purpose, drugs such as Cardiomagnyl, Thromboass, Aspirin are prescribed. Sometimes these medications are difficult to tolerate, which is usually due to problems with the stomach. In this case, it is best to take Ticlopedine.
- Reopoliglyukin is prescribed. It is administered by drip through a vein. The procedure is carried out in a hospital setting.
- Statin drugs are used. They reduce the concentration of cholesterol in the blood and prevent the development of atherosclerosis. These drugs include: Pravastatin, Simvastatin, Atorvastatin.
- To relieve spasms of blood vessels, drugs that belong to the group of coronary lytics are used. For example, Nikoverin and Papaverine are used. In addition, nicotinic acid will do.
- Medicines are prescribed that will restore blood microcirculation in the brain. These include: Vinpocetine and Cavinton.
- To support the functioning of neurons and maintain their integrity, nootropic drugs are prescribed. For example, Cerebrolysin, Nootropil, Piracetam are used. These medications also provide additional energy to the cells of the central part of the brain.
There is currently debate about whether it is advisable to use statins in treatment for transient ischemic attacks, since their frequent use can lead to mental problems. Typically, such drugs are prescribed only if a special anti-cholesterol diet has not helped within two months and the level of cholesterol concentration in the blood has not decreased. If the lipoprotein content is normal, then static agents are not used.