Everyone knows the phrase “probing the stomach.” It definitely causes unpleasant emotions, and sometimes even panic. But is gastric probing really that scary? What is it used for? Are there any contraindications? How does the procedure itself proceed? Let's try to deal with these questions in order.
Probing of the stomach is one of the safest and most informative medical procedures aimed at studying the inner surface and digestive secretions of the stomach. For this purpose, a thin rubber probe is inserted through the oral or nasal cavity into the stomach.
Who is prescribed
- Patients with abdominal pain of unknown etiology.
- For digestive disorders: heartburn, indigestion, bloating, nausea, colic, to establish the level of stomach acidity.
- If you suspect gastritis.
- If an ulcer is suspected.
- For gastric lavage and rapid removal of its contents in case of poisoning with food, drinks or medications.
- For feeding people in an unconscious state, coma.
- If you suspect neoplasms and tumors in the stomach.
To dispel anxiety and fear of the unknown, before starting the probing procedure, it would be good to talk with the doctor and medical personnel who will perform the manipulation. This will help to get a complete picture of how everything will go, and the patient will understand what is happening. Psychological attitude plays an important role in preparing for probing. Calm patients tolerate the procedure much easier.
https://youtu.be/b0NryRo4XmQ
Caring for the decompression tube
In order to prevent clogging of the catheter during the procedure, you should properly care for it and follow the rules for servicing the device:
- Each time before the procedure, you should wash your hands thoroughly.
- Check the position of the probe 3 times a day, monitor the acidity of the stomach.
- Rinse the tube thoroughly before and after administering food or medications. This must be done at least 3 times a day.
- To avoid mixing food, use new food sets each time.
- Take care of your nasal cavity every day, making sure that it is not damaged.
- The nasal mucosa should be treated with antiseptics.
- Carry out hygiene procedures in the mouth: rinsing, brushing teeth.
- Replace the tubes in a timely manner, avoiding their stay in the stomach for more than 30 days.
Types of gastric intubation
There are 2 main types of sounding:
- One-step. It is carried out with a thick (up to 13 mm in diameter) rubber tube. The gastric contents are pumped out only once. This type of research is no longer used as it is outdated and does not provide a detailed picture of the condition of the organ. The fairly thick tube caused severe discomfort and a pronounced gag reflex in patients.
- Fractional probing is more gentle and effective. It is carried out with a thin probe (up to 5 mm) in several stages. Duration 2-3 hours. This procedure gives a complete picture of the condition and functioning of the stomach.
Examination methods
Today, various methods have been developed to study the secretory function of the stomach. Each method has advantages and disadvantages. The probing method with further chemical, macroscopic study of the secretion is considered well-known and widespread in the world. Based on the obtained tests, the digestive ability of gastric secretions and the motor function of the stomach are assessed.
Simultaneous sensing
To perform this type of examination, a thick type of probe is used - a tube made of rubber material, 80-100 cm in length, approximately 10 mm in diameter. Now the method is practically not used as a diagnostic method, as it is considered uninformative. This type of sounding is carried out for therapeutic purposes. For example, for gastric lavage.
Multi-instant sensing
Multi-moment, or fractional, sounding is performed using a thin probe with a diameter of 4 mm and a length of 100-150 cm. A syringe attached to the tube periodically sucks in the contents of the stomach. With the type of examination described, the gag reflex, as a rule, does not occur. Fractional studies can be extremely informative and provide a comprehensive picture of gastric secretion.
The research algorithm involves 3 stages:
- Lean stage. Gastric juice is extracted after insertion of the tube.
- Basal stage. The liquid is sucked out over an hour.
- Stimulating stage. Stimulating drugs and products are administered. After 15 minutes, the gastric contents are suctioned.
Equipment
For the procedure you will need:
- a chair or couch to accommodate the patient;
- clean towel or napkin;
- medical probe;
- syringe, vacuum suction for attachment to the hose;
- medical tray or basin;
- test tubes for collecting tests;
- products, drugs that stimulate the production of gastric secretions.
How is the procedure performed?
The probing technique is as follows:
- Routine probing of the stomach is carried out in the morning. The patient is invited to the treatment room.
- The patient sits on a chair with a back or lies on his side on the couch.
- A towel is placed on the patient's chest and shoulders, as saliva may leak. Some patients experience vomiting.
- A tray is given to the hand or placed nearby to collect saliva (it must not be swallowed, but spat out).
- The pharynx is treated with a weak local analgesic to reduce sensitivity and pain threshold.
- The rounded end of a sterile probe (it may have holes or a miniature camera, depending on the purpose of the study) is placed on the root of the tongue. Then the doctor invites the patient to swallow, and he quickly moves the probe inside.
- Then the patient's nasal breathing is checked. He should breathe calmly through his nose.
- With each swallowing movement, the tube is moved deeper until the desired mark is reached. The depth is calculated using a special formula: human height minus 100 cm.
- Attach the hose to the patient’s clothing to secure it.
- At the next stage, a pump is put on the outer end of the probe or a syringe is attached and the entire contents of the stomach are aspirated.
- The basal (hungry) gastric secretion is pumped out in several stages, each of which lasts 5 minutes. Between them there are pauses of 10 minutes.
- Using a probe, a heated “test breakfast” (dried cabbage extract or broth) or special enzymes that stimulate the production of gastric juice (Insulin, Histamine or Pentagastrin) are injected into the stomach. These products and preparations act as a “breakfast” and help to get a complete picture of the functioning of the stomach after eating.
- After 10 minutes, a sample of gastric juice is taken again.
- After another 15 minutes, another portion of the stomach contents is taken.
- So within an hour they take gastric juice 7 times.
- The probe is removed, the patient is allowed to rinse his mouth and rest.
All portions of the secret are numbered, signed and sent to the laboratory for study.
How much does the FGDS procedure cost?
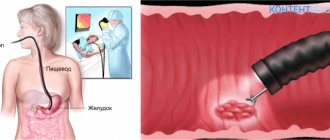
The abbreviation FGDS in medicine refers to one of the most common methods for studying the upper parts of the digestive system. It stands for fibrogastroduodenoscopy - examination of the mucous membrane of the stomach and duodenum using an endoscope (gastroscope).
Sometimes the procedure is called EGD. The letter E in the name means “esophagus” - esophagus. However, this abbreviation is used less frequently, since FGDS itself already implies examination of the esophagus; the endoscope passes into the stomach through it.
The essence of the technique is that the patient swallows a probe, which, after passing through the mouth, enters the stomach and the initial part of the intestine. At the end of this probe is a miniature light bulb and a camera. The image from the camera is transmitted to a computer screen, after which it is deciphered by a gastroenterologist.
| View | Description |
| Classical | It is carried out without anesthesia; the patient swallows a tube after applying an anesthetic spray to the pharyngeal mucosa. Used in most subjects |
| With anesthesia support | Some categories of patients require anesthesia in order to be able to fully carry out the manipulation. A short-term general anesthesia is used, during which the muscles of the pharynx and esophagus relax, allowing the doctor to insert the endoscope |
| Planned | It is carried out by appointment, for patients who do not require an urgent diagnosis. |
| Emergency | It is carried out for vital indications, when it is urgently necessary to determine what happened to a person. The risk of complications increases due to lack of proper preparation |
| Diagnostic | Used only for examining the mucous membrane of the esophagus, stomach and intestines, identifying pathological changes |
| Medical | In addition to the examination, the doctor can carry out the required treatment measures:
|
Using gastroscopy, a doctor can diagnose the following diseases:
- various tumor neoplasms - polyps, cysts, cancer of the esophagus or stomach;
- gastritis - erosive, atrophic, hypertrophic;
- gastroesophageal reflux disease;
- Barrett's esophagus;
- Mallory-Weiss syndrome;
- ulcers of various parts of the digestive tract;
- wounds to the mucous membrane.
With the help of endoscopic equipment, dilation of the esophageal veins can be detected, which is one of the signs of liver cirrhosis.
Contraindications for probing
Despite the fact that this procedure is common throughout the world and is considered safe, there are categories of patients for whom it is contraindicated:
- Heart failure.
- Hypertonic disease.
- Kidney failure.
- Severe forms of diabetes.
- Allergy to drugs that stimulate secretion.
- Severe hypotension.
- Some mental illnesses.
- Impaired nasal breathing.
- The patient has a severe cough.
- Pregnancy.
- Varicose veins of the esophagus.
- Stomach bleeding.
About the probing procedure
This examination is carried out on an outpatient basis by a gastroenterologist. A probe is inserted through the mouth or nose into the esophagus and advanced into the stomach. Using a specially developed algorithm, the doctor performs diagnostic manipulations to study indicators such as:
- composition of gastric juice taken in several stages;
- secretory function of the mucous membrane;
- acidity level;
- the presence or absence of food residues in the mucous membrane;
- the volume of fluid pumped out of the stomach.
The examination causes virtually no discomfort, despite the fact that it is carried out without anesthesia or pain relief. The position of the tube in the patient's stomach is monitored using an X-ray machine.
The use of modern materials makes it possible to conduct research using a very thin probe with a diameter of 0.4-0.5 cm. The minimum possible dimensions will help avoid gagging and do not create unpleasant sensations.
Modern medical technology has further improved and simplified gastric probing. An exceptionally thin probe can now be equipped with a miniature video camera that transmits an image of the internal contents of the organ and its structural features to a computer screen. Based on the data obtained, the doctor will be able to confirm or refute the alleged diagnosis, differentiate it from similar pathologies, and promptly detect the onset of cancer damage to the mucous membrane and muscular wall of the organ.
Evaluation of test results
Signed beakers with analyzes are sent to the laboratory. To make a diagnosis, such indicators as color, quantity, and nature of the secretion are important. The doctor will pay attention to the following points:
- The liquid should be colorless, moderately fluid, and not contain inclusions of a different color.
- Abundant secretion indicates hyperfunction of gastric juice and a shift in acidity in one direction or another.
- A yellowish-green color indicates the presence of bile from the intestines. Reddish-brown spots indicate the presence of blood.
- In a healthy stomach, gastric juice has no odor or is sour. The smell of rot may indicate the development of a cancerous tumor.
- In addition to physical indicators, the chemical composition of liquids is also studied.
Depending on the test results, the necessary treatment is prescribed.
Typically, gastric intubation does not cause any side effects in patients. During the day, you may experience slight malaise and stomach upset. This condition does not require special treatment. Doctors advise not to overeat or burden your stomach on this day. At first, crackers and tea with sugar are recommended; in the evening, when the condition improves, you can eat a light dinner. Many patients tolerate the procedure well and immediately after it go to work and do their daily activities.
There is no need to be afraid of the gastric intubation procedure. Nowadays, probing is much more painless and comfortable than it was several decades ago. The main thing is to remember that it will help make an accurate diagnosis, therefore, restore lost health, and maybe save a life.
Comments:
- Probing methods and methods
- Preparation for the procedure and evaluation of research results
Probing of the stomach is necessary for diagnosis in case of suspected peptic ulcer, chronic gastritis and functional diseases of the digestive system. Without assessing the clinical picture and determining the state of gastric secretion, it is almost impossible to choose the right treatment.
Probing the stomach is one of the safest and most effective procedures, but it has some contraindications.
These include:
- pregnancy;
- diseases of the cardiovascular system;
- stomach bleeding.
Preparation
Probing the liver or stomach is a lengthy procedure with unpleasant sensations. To carry out the manipulation, the doctor requires a stool on which the patient will sit, a special container-basin, a thin sterile probe, a syringe or pump for the hose, a towel, and sterile jars for tests. The patient undergoes training:
- during the day before the study, refrain from smoking and taking medications;
- does not consume foods that increase the accumulation of gases and the secretion of gastric juice;
- 14-16 hours before the test, does not eat anything, drinks only clean water, with the exception of soda;
- improves his psychological state, tries to avoid stress (otherwise the secretion of gastric juice increases);
- removes inserted dental structures, if any.
- Ticks on a dog - what to do
- How to feed strawberries during flowering
- Potato cookie cake - recipes with photos. How to make homemade potato cake, like in childhood
Probing methods and methods
Probing of the stomach is carried out in 2 ways.
- One-step. The probe is thick - the internal lumen is 8 mm, length - 80-100 cm. The procedure is practically not used for diagnostics; it is performed when food is introduced into it.
- Factional. It is carried out with a thin probe, which is a rubber tube with a lumen of 2-3 mm, a length of 1.1-1.5 m. The end lowered into the stomach without an olive, there are 2 holes on it. The hose is marked at a distance of 50 and 70 cm from the lower end. At the outer end there is a syringe through which the contents of the stomach are sucked out at certain intervals.
During fractional sounding, the doctor requires the patient's assistance.
The algorithm for performing the procedure is a standard scheme:
- First, all the contents of the stomach are pumped out.
- Then, every 10 minutes, portions of fresh basal secretion are sucked out - this is the name of the gastric juice that is produced on an empty stomach. This stage takes about an hour.
- Then a secretion stimulant or a test breakfast is administered through a probe. Broth is most often used as a test breakfast. Insulin, pentagastrin or another drug is used as a stimulant. The choice of stimulant depends on the history of chronic diseases.
- The secretion irritant begins to act within 30 minutes. Gastric juice, which was released under the influence of the irritant, is withdrawn at intervals of 15 minutes.
In order for the probe to be inserted successfully, the patient is seated on a chair: the back must be kept straight. The doctor inserts a flexible hose into the throat by the root of the tongue, and the patient makes swallowing movements. Thanks to them, the probe moves to the required distance.
When the hose is inserted to the required length, it is fixed - secured with a clamp to the patient’s clothing. A clamp is also installed at the end to prevent gastric contents from leaking out randomly.
The procedure requires at least 2-2.5 hours.
The procedure technique may vary. Sometimes a mouthpiece is inserted into the patient’s mouth to fix the jaws in the desired position and prevent the hose from being bitten; the larynx area is anesthetized with an anesthetic, the patient does not need to sit - he is placed on his left side, and gastric secretions are collected with a special pump.
» What is Duodenal sounding? How and when is it done?
Not everyone can undergo duodenal intubation; for example, the procedure is contraindicated for patients suffering from acute cholecystitis, exacerbation of cholelithiasis, ulcers during an exacerbation, narrowing of the esophagus, dilation of the esophageal veins, angina pectoris and heart attack.
When is duodenal intubation done?
Indications for duodenal intubation:
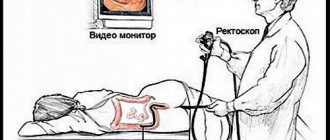
Duodenal sounding is carried out using a duodenal probe, which is a kind of tube, the diameter of which is no more than 5 mm and the length is one and a half meters. The end inserted into the stomach has a metal olive with holes. There are several distance markings on the probe itself.
A very important place is occupied by the preparation of the patient before performing duodenal intubation. A few days before the procedure, it is necessary to exclude from the diet foods that contribute to gas formation, namely milk, brown bread, confectionery, and legumes. In addition, the doctor prescribes atropine. Dinner the night before should be light no later than six o'clock in the evening. The procedure itself is carried out on an empty stomach.
Duodenal intubation is performed in a sitting position, the head is slightly tilted forward, the patient holds a container with a probe. Breathing should be deep, the probe is swallowed along with saliva, which manages to accumulate in the oral cavity. The probe with the tip is placed deep on the tongue, then several swallows must be taken, while the mouth must be closed. Markings on the probe help determine where the olive is located. The first mark indicates that the probe is already in the stomach, the insertion is temporarily stopped and the patient lies down on the couch on the right side, with a bolster under the pelvis and a heating pad under the hypochondrium. Next, swallowing the probe is resumed until the second mark is reached. To avoid the tube from coagulating in the stomach, it is necessary to swallow it gradually.
The contents of the stomach are aspirated using a syringe. That penetration of the probe into the intestine is possible only when the pylorus is opened. If the opening of the pylorus is delayed, the patient is given atropine, papaverine, or given a sodium bicarbonate solution to drink. The fluid that is sucked out helps determine where the probe is located. Portion A begins to be released after the probe penetrates the duodenum. To obtain portion B, it is necessary to introduce an irritant and close the probe for five minutes, only after which bile begins to be released. Portion C is a clear liquid that is released when the gallbladder is completely emptied.
To remove the probe, the patient is seated. After removal, you must rinse your mouth.
The results of the study of the secretions of the digestive organs make it possible to see the presence of pathologies in the bile ducts, pancreas, and liver. The study is carried out if gastroenterological diseases and the development of liver pathologies are suspected. It shows the presence of foci of inflammation and helminths in the organs of the digestive system.
- accumulation of sputum in the gallbladder;
- bitter taste in the mouth;
- frequent attacks of nausea of unknown etiology;
- pain near the right hypochondrium;
- increase in urine concentration.
Important! For helminthic infestations, duodenal examination is prescribed if giardia cholecystitis, feline or liver fluke infection is suspected.
The procedure for duodenal examination for children does not differ from probing for adults. But the child needs to be mentally prepared for the study.
Preparation for duodenal examination begins 5 days in advance. In order for the analysis results to be reliable, it is necessary to exclude the use of certain pharmaceutical drugs:
- choleretic;
- antispasmodics;
- vasodilators;
- laxatives
- medications that improve the digestion process.
24 hours before the study, the patient is shown atropine - a 0.1% solution is administered subcutaneously. Or take a mixture of 8 drops of the drug, 30 g of xylitol and a small amount of warm water.
Before a chromatic duodenal examination, you must take methylene blue in a gelatin capsule. The product should be consumed 3-4 hours after dinner.
Important! The evening meal should be light, you need to completely eliminate foods that cause gas formation - milk, brown bread, legumes, potatoes.
At the preparatory stage, a throat smear is taken from the patient on the eve of probing. This procedure is done in order to see the presence of pathogenic microflora and prevent its penetration into the bile samples being studied.
The procedure is carried out in the morning, on an empty stomach. Before probing, the pharynx and oral cavity are treated with antiseptic agents.
Duodenal intubation is a complex and not very pleasant procedure. For research, use a probe with a tip made of plastic or metal (olive). The olive has holes into which samples of the material being tested penetrate.
Before starting the diagnosis, marks are applied to the probe that will help determine the location of the probe. The distance between the start and end marks is equal to the length between the front teeth and the navel.
How it is carried out:
- The tip of the probe is lubricated with glycerin and placed as close as possible to the root of the tongue.
- The patient should breathe calmly and make uniform swallowing movements.
- The first mark was at the level of the teeth - the probe reached the stomach.
- The person needs to lie on his right side and continue to swallow the probe until the second mark.
- The second mark means that the tip has reached the pylorus - after opening it will be able to penetrate the duodenum.
- The third mark indicates that the olive has penetrated the duodenum - a golden liquid appears from the hose.
On average, the examination takes approximately 1.5 hours.
Duodenal intubation can be classical or fractional. The classical method is somewhat outdated, since it allows you to take only samples of duodenal, cystic and hepatic bile.
Important! Fractional research consists of 5 phases, which are taken after a strictly defined time.
Portion A appears immediately after the tip of the probe penetrates the duodenum and is released within 20 minutes. After this, magnesium sulfate is administered - bile from the spasm of the sphincter of Oddi ceases to be released, the phase lasts about 5 minutes.
In the third phase, the contents of the extrahepatic bile ducts are released within 3–4 minutes. In the next phase, portion B of bile is released directly from the gallbladder; the thick liquid is dark yellow or brown. This type of biomaterial is the most important for research.
Portion C includes light bile, which appears after the gallbladder is completely empty.
Due to the complexity of the procedure, probing is not performed on children under 3 years of age. The main contraindications are asthma, jaundice, hypertensive crisis, varicose veins of the esophagus. Duodenal examination is not performed in case of gastric bleeding, peptic ulcer in the acute stage, or the presence of stones in the gall bladder. This type of examination is contraindicated for expectant and nursing mothers.
Diet before gastroscopy of the stomach: how many hours before you can’t eat, what you can eat and drink
Gastroscopy of the stomach is one of the modern diagnostic procedures that allows one to obtain reliable information about the condition of this organ. To carry it out, a special device is used - a gastroscope, which resembles a flexible tube equipped with a fiber-optic system connected to the monitor screen.
An endoscopist conducting an examination and having the opportunity to see the inner surface of the stomach, if inflammation, neoplasms and any changes are detected on the surface of its mucous membranes, receives important information that allows making an accurate diagnosis.
In order for the results of an endoscopic examination of the stomach to be reliable, before it is performed, the patient must undergo certain comprehensive preparation, in which adherence to a special diet plays an important role.
In order for the discomfort experienced by the patient during gastroscopy to be minimal, and for any interference that prevents the examination of the walls of the stomach to be completely absent, the organ being examined must be freed from particles of undigested food.
A special diet that contributes to the implementation of this important task should be followed for 48 hours preceding the gastroscopy procedure. Compliance with all its requirements will allow the patient not only to tolerate the process of diagnostic examination of the stomach well, but also to quickly get rid of irritation of its mucous membranes.
- chocolate;
- strong fish and meat broths;
- fast food (fast food);
- marinades and pickles;
- fatty fish and meat;
- any smoked meats and lard;
- all types of canned food;
- hot sauces and seasonings (adzhika, ketchup, mayonnaise, mustard, table horseradish) homemade and industrial;
- bread and bakery products of dark varieties;
- mushroom dishes (including mushroom broths);
- seeds and any nuts;
- animal fats.
The above dishes and products are poorly absorbed by the human body, change the acidity of gastric juice and contribute to the occurrence of intestinal flatulence.
Requiring long-term digestion, they overload the stomach and irritate its mucous membranes, so even a short exclusion of them from the daily diet is beneficial for the gastrointestinal tract.
In anticipation of undergoing gastroscopy, the patient is advised to significantly limit the consumption of table salt. In order to remove excess fluid from his body, he is recommended to gradually add salt only to ready-made dishes.
The day before the scheduled gastroscopy, the patient is prohibited from consuming:
- whole grains;
- fat cottage cheese;
- flour and pasta products;
- baked goods;
- legumes;
- whole milk and heavy cream;
- tomatoes;
- citrus fruits (tangerines, lemons, oranges);
- plum, kiwi, quince, grapes;
- jam with any (even small) seeds, including raspberry and currant.
- White poultry and lean fish (blue whiting, hake, pike, pike perch, pollock, perch, ice fish, roach, cod) boiled or in the form of steam cutlets. As a side dish, you can serve them with omelette, buckwheat porridge, rolled oats or mashed potatoes.
- Fermented milk products (yogurt, acidophilus, kefir) with a low fat content. Doctors also recommend eating low-fat cottage cheese and dishes made from it.
- Soups made from milk half diluted with water (with the addition of small noodles or ground boiled cereal).
- Weak fish and meat broths.
- Light vegetarian soups that do not contain seasonings and fried vegetables, seasoned with a small spoon of low-fat sour cream. You can add some finely chopped greens to the plate. It is advisable to avoid eating borscht.
- A small amount of butter.
- Unsalted low-fat cheeses (preferably grated).
- Vegetables (pumpkin, carrots, potatoes, cauliflower, beets), especially boiled and baked.
- White bread or crackers made from it.
- Cookies.
- Soft-boiled eggs.
- Steamed omelettes.
- Sweet apples, pureed using a grater. You can bake them with pumpkin slices, sweetening them slightly with sugar or honey.
- Pears and bananas.
The optimal way to cook food is boiling, stewing, and steaming. Baking dishes in the oven is allowed, but without the use of fat and oil. Frying foods should be completely avoided.
To ease the work of the stomach, it is better to grind cooked food or puree it.
The temperature of the food consumed is no less important: it should not be too hot or too cold, since sudden temperature changes at the time of eating contribute to irritation of the mucous membranes of the stomach.
Here's what a patient's daily diet might look like on the day before gastroscopy.
Breakfast:
- steamed cheesecakes;
- weak tea (black or green), 200 ml.
- a small portion of light vegetable soup with small noodles or grated cereal;
- a piece of steamed veal;
- boiled Brussels sprouts, seasoned with a small amount of vegetable oil;
- rosehip decoction.
Afternoon snack:
- baked apple (the peel must be cut off before eating).
- a small portion of steamed pike perch fillet;
- several slices of boiled or baked vegetables;
- low-fat kefir.
What can you drink?
The patient is allowed to use:
- decoctions of blueberries or rose hips;
- herbal teas with anti-inflammatory effects;
- compotes made from both fresh and dried fruits;
- mineral table waters that do not contain gas;
- weak black or green tea;
- fruit juices;
- berry fruit drinks.
The temperature of drinks that we are used to drinking cold should be close to room temperature, and tea should not be too hot. It is better to use honey to sweeten tea. The amount of sugar added to drinks should be moderate.
Patients should avoid drinking alcoholic beverages of any strength (including beer with low alcohol content) at least 24 hours before the scheduled examination.
The main condition for a successful gastroscopy procedure is complete emptying of the stomach, since this is the only way to prevent the gag reflex, which is a natural reaction of the body to the insertion of a gastroscope.
Neglect of this condition can cause:
- the occurrence of vomiting, which significantly complicates the process of both insertion and removal of the gastroscope from the patient’s body;
- serious damage to the mucous membranes of the stomach and larynx by the edges of the already inserted device at the time of vomiting, as a result of which its re-insertion may become impossible.
To eliminate the possibility of such undesirable events, it is necessary to carefully calculate the time remaining before the start of gastroscopy:
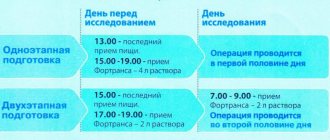
- Patients complaining of poor stomach function should ensure that their last meal takes place twelve hours before (the extra time is also necessary because at night the speed of the digestion process decreases significantly). Fasting for 10-12 hours is also required in cases where the procedure will be performed under general anesthesia.
- Those with a completely healthy stomach that can quickly digest food can have dinner nine to ten hours before the scheduled procedure.
Most medical sources say that before a gastroscopy scheduled for the morning, the last meal should take place no later than 19-00. If the procedure is carried out in the afternoon, the patient is allowed a light breakfast, which should take place approximately eight hours before the procedure begins.
If this condition is not met, particles of undigested food will either interfere with the advancement of the gastroscope, or, by forming a thin layer on the walls of the stomach, may prevent the timely identification of problem areas on their surface.
No less important is the question of whether you can drink water before the gastroscopy procedure. Its last use (in a volume not exceeding 100 ml) is permissible no later than four hours before. People suffering from chronic diseases and forced to take pills are allowed to take them with a small amount of water.
- For patients with diabetes, the procedure is usually prescribed in the morning, so that half an hour after its completion they can take vital medications and have a snack with food they brought with them.
- A special diet before gastroscopy of the stomach, which has virtually no contraindications (except for individual intolerance to certain foods) and is useful for people of any age, is tolerated by patients quite easily, given the wide variety and nutritional value of the dishes allowed for consumption.
- The need to adhere to a special diet is 72 hours: 48 hours before the examination and 24 hours after the procedure.
- The only drawback of the diet described above is the need to prepare food yourself, since the menus of canteens, restaurants and cafes do not always include dishes prepared in full accordance with the requirements of therapeutic nutrition.
The diet that should be followed before undergoing gastroscopy is based on the principle of proper nutrition with exclusively healthy foods, so you can stick to this regimen even after completing any medical procedures and examinations. By following it, every person can avoid digestive problems.
As the results of gastroscopy of the stomach and reviews of patients who strictly followed the rules of a special diet before performing it show, during the medical procedures consisting of inserting and removing a gastroscope, they experienced almost no discomfort.
Gastroscopy is an effective endoscopic diagnostic method that allows you to examine the condition of the gastrointestinal tract.
For this type of examination, a special device called a gastroscope is used, which is a flexible tube with fiber optics.
A medical video endoscope equipped with an electronic sensor is also used, using the device to obtain an image on the screen.
There are a number of types of endoscopic examination:
- Fibrogastroscopy, gastrofibroscopy, gastroendoscopy or gastroenteroscopy (abbreviated name - FGS) is used when examining the stomach to evaluate the mucous membrane of the organ and identify diseases.
- Esophagoscopy involves examining the mucous membrane of the esophagus.
- Esophagogastroduodenoscopy (abbreviated as EGDS). With this type of diagnosis, the esophagus, stomach and duodenum are examined.
- Fibrogastroduodenoscopy, gastroduodenoscopy (abbreviated as FGDS). During this procedure, the stomach and duodenum are examined.
Complications during the procedure and research results
Duodenal examination is extremely unpleasant for people. The main problem is the occurrence of strong urges of nausea when swallowing the probe and tip. In some people, the gag reflex is so strong that muscle spasm occurs and it is impossible to conduct an examination.
Important! Throughout the procedure, increased salivation is observed - saliva cannot be swallowed, it must be spat into a special tray.
If magnesium sulfate is used as an irritant, severe diarrhea may occur. When using xylitol, sorbitol, or glucose solution, the patient's condition may worsen if there were strong fermentation processes in the intestines.
In people who undergo probing, blood pressure often drops and changes in pulse rhythm are observed. After completing the procedure, you should not jump up suddenly; you must lie down for at least an hour under the supervision of a doctor.
All portions of bile undergo microscopic and bacteriological examination.
Duodenal diagnostics is one of the most informative types of research for many diseases of the gastrointestinal tract and helminthic infestations. The procedure requires preliminary preparation; all doctor’s instructions must be strictly followed.
Have you even read anything about medicines designed to defeat the infection? And this is not surprising, because worms are deadly to humans - they can reproduce very quickly and live for a long time, and the diseases they cause are difficult, with frequent relapses.
Bad mood, lack of appetite, insomnia, immune system dysfunction, intestinal dysbiosis and abdominal pain... Surely you know these symptoms firsthand.
Answers to your questions
Classical and fractional duodenal intubation are procedures in which bile secretions are taken from the patient for analysis using a probe. Proper collection of fluids helps to identify pathologies and detect helminthiasis inside the gallbladder and liver with an accuracy of 90%. The probing procedure for the patient involves a number of uncomfortable sensations, so you need to strictly follow the doctor’s instructions.
Complications
When performing multi-stage gastric intubation, the following complications may occur:
- Stomach bleeding;
- Collapse (a serious condition in which blood pressure drops sharply, the pulse quickens, the skin becomes cold, cold, sticky sweat appears, the skin turns pale);
- Fainting (short-term loss of consciousness);
- Injury to mucous membranes;
- Profuse vomiting.
What is duodenal intubation
The duodenal sounding procedure is a diagnostic method that is used to examine the liver and biliary tract. For medicinal purposes, a medical measure is used to remove the contents of the gallbladder. Carrying out such a diagnostic manipulation becomes possible thanks to special equipment - a duodenal probe, which in appearance is a tube made of flexible material 150 cm long and 3-5 mm in diameter. At the tip of the device there is a metal olive with holes on the surface.
A duodenal tube can enter the body through the digestive system, so the tube and other parts must be absolutely sterile. Using the device, doctors select the required amount of bile, gastric, intestinal and pancreatic juice from the duodenum. The duodenal diagnostic method is required if it is necessary to obtain information about the activity of the pancreas, the condition of the liver, biliary tract and gallbladder capacity.
Necessity of application
Gastroscopy is prescribed in the following cases:
- If necessary, search for pathologies of the upper digestive organs, namely inflammation of the esophagus or esophagitis, reflux astroesophageal disease or GERD, as well as narrowing of the esophagus or structure.
- Hiatal hernia or hiatal hernia.
- The presence of Barrett's esophagus or a condition that increases the risk of developing esophageal cancer due to pathological changes in the mucous membrane that indicate a precancerous condition.
- Ulcerative diseases.
- Cancer.
- The need to determine the cause of vomiting with bloody splashes, as well as to clarify the nature of blood formations.
- Finding out the causes of pain in the upper part of the stomach, bloating, dysphagia or difficulty swallowing, vomiting, unexplained weight loss.
- Finding the source of infection.
- Monitoring the healing process of ulcers;
- The need to monitor the state of the digestive organs in the postoperative period.
- Determining the causes of disturbances in the processes of food movement, passage from the stomach cavity into the space of the duodenum or stenosis of the gastric outlet.
In other cases, gastroscopy is done for:
- diagnosing the degree of chemical damage to the esophagus in a patient in critical condition due to poisoning with toxic substances;
- removal of pathological formations in the esophagus and other digestive organs, gastrointestinal polyps;
- performing medical procedures in cases of intra-abdominal bleeding associated with the digestive organs, including from the dilated veins of the esophagus;
- removal of foreign bodies that entered the gastrointestinal tract or gastrointestinal tract during swallowing;
- identifying the causes of chronic bleeding, which manifests itself in cases of prolonged anemia caused by impaired oxygen-binding functions of red blood cells.
Indications for duodenal intubation
The main indications for probing the liver and gallbladder are the following symptoms:
Proper preparation of the patient for duodenal intubation is very important. The process is a set of measures consisting of the following actions:
- discontinuation of choleretic, laxative, antispasmodic and enzyme medications 5 days before the expected sounding;
- a diet that you need to start following 2-3 days before the study;
- refusal to eat 12 hours before the procedure - probing is carried out on an empty stomach;
- bowel cleansing in the evening before duodenal examination.
Diet before probing
Preparation for duodenal intubation involves following a diet. Dietary restrictions are not strict - on the eve of the study, the patient is allowed to eat his usual food. Experts recommend limiting the consumption of large amounts of foods that stimulate the biliary system. You should eat less fatty and fried foods, vegetable oil, dishes containing eggs, soups based on rich fish and meat broths, sour cream, cream, and sweets.
It is not recommended to drink strong tea, coffee, carbonated drinks, or alcohol. Fruits, vegetables and berries have a strong stimulating effect on the gallbladder. When consuming these products, the secretory function of the organ is significantly enhanced. You should not combine vegetables with vegetable oils. Such a union provokes bile secretion. The diet must be followed by the patient for 2-3 days before duodenal examination.
Nutrition after the procedure
After completing the manipulation, the patient has a question: what can you eat after duodenal intubation?
After 20-60 minutes. After the procedure is completed, you can eat. Food should be light, and food throughout the day should not contain spicy, fatty or fried foods. Next, it is recommended to stick to the diet for several days.
The nutrition menu after duodenal intubation for the first 3 days should consist of properly selected dishes that will not create additional stress on the gastrointestinal tract. After all, before the procedure, the patient followed a diet for some time, which helped the stomach prepare for the upcoming test.
Therefore, it is necessary to avoid heavy foods and give priority only to dietary dishes, which should be at room temperature and low in fiber.
Examination for opisthorchiasis using duodenal intubation, although it causes a person some discomfort, is safe, and if you follow the doctor’s recommendations, no side effects occur. This method has a number of advantages that help to identify a reliable picture of the state of the gastrointestinal tract in a person and the presence of helminths in it.
Duodenal intubation is a method of examining bile with a special tube inserted into the duodenum. The accuracy of diagnosis is influenced by nutrition before the procedure and compliance with recommendations for cleansing the body. The reliability of the result depends on whether the preparation for duodenal intubation was correct.
Execution technique
Duodenal examination using a probe can be carried out in two versions: classical and fractional. The first technique, consisting of three phases, is practically not used because it is considered obsolete. As a result of the procedure, the specialist receives three types of bile for study: duodenal, hepatic, and cystic. These fluids are taken from the duodenum, bile ducts and bladder, and liver.
The fractional technique of duodenal intubation consists of 5 phases of pumping out bile secretion, which change every 5-10 minutes:
- The first phase is the release of portion A. Liquid is taken at the stage of the probe entering the duodenum before the use of cholecystokinetic agents. The duration of the probing phase is 20 minutes, during which the duodenal contents, consisting of pancreatic, gastric and intestinal juices, and bile, are pumped out.
- At the second stage of duodenal examination, the specialist introduces magnesium sulfate, the release of bile from the spasm of the sphincter of Oddi stops. The duration of this phase varies between 4-6 minutes.
- The third stage of probing is characterized by sampling the contents of the extrahepatic bile ducts and lasts 3-4 minutes.
- The fourth phase of the duodenal examination consists of isolating portion B: the contents of the gallbladder, the secretion of thick bile of a dark yellow or brown hue.
- At the final stage of probing, specialists begin to pump out bile, which has a golden hue. The process takes about half an hour.
Algorithm
Duodenal examination by probing involves a sequential algorithm:
- The patient should assume a sitting position with his back straight. The specialist places the tip of the probe, on which the olive is located, into the oral cavity of the person being examined - it must be swallowed.
- The umbrella then begins to sink deeper through slow swallowing.
- When the hose for duodenal examination drops inward by 40 cm, it is necessary to advance it another 12 cm. At this stage, a syringe is attached to the device, which helps to collect gastric juice.
- The next step is to swallow the rubber tube for probing to the 70 cm mark.
- When the duodenal tube is immersed to this depth, the patient should lie on the right side. In this case, the specialist places a pillow under the pelvis of the person undergoing probing, and a warm heating pad is placed under the ribs.
- The outer free end of the duodenal hose is lowered into a test tube on a stand designed to collect secretions.
- Immersion of the probe continues until the 90 cm mark. From 20 to 60 minutes are allotted for this stage of duodenal sounding.
- After the olive enters the duodenum, the tube is filled with yellow duodenal fluid;
- When all phases of the procedure have completed, the probing hose is removed with gentle movements.
Carrying out diagnostics
The probing procedure can take up to 2.5 hours, depending on the technique used and the patient’s condition. A lot of probing techniques have been developed; most often the procedure is carried out according to the standard scheme:
- All its contents are pumped out of the stomach;
- Within an hour, the basal secretion is pumped out - the fluid produced by the stomach on an empty stomach. The liquid is withdrawn in 5-minute portions every 10 minutes. It turns out 4 portions of secretion for every hour, each of them is poured into a separate jar and marked;
- Then a test breakfast or a secretion stimulant is administered. A test breakfast is broth, cabbage broth, or one of the options offered by other methods. The secretion stimulant is gestamine, pentagastrin or insulin. Gestamine and insulin are not used if the patient suffers from cardiac, hepatic, renal or pulmonary failure, hypertension, or diabetes. Pentagastrin also has a number of limitations: stage 2 or 3 circulatory failure, cardiac arrhythmias and hypotension. The trial breakfast is now used less and less: it gives a less pronounced stomach reaction;
- After half an hour (during this time the stimulus has time to fully act), the secretion produced in response to the stimulus is also taken in 15-minute portions.
Each portion of the secretion is studied in the laboratory, based on the results an acidity curve is constructed, the content of peptides, hydrochloric acid and impurities (bile, blood, starch, muscle fibers, blood and others) is assessed. The specialist also evaluates the appearance, smell and consistency of the secretion. The total amount of liquid pumped out also matters.
How to swallow a tube correctly
Probing of the liver and gallbladder will be successful if the patient can swallow the tube correctly. The doctor must carefully move the device through the esophagus and stomach to the required marks that are on the hose. Sudden swallowing can cause the probe to curl up, requiring repeated immersion, so the process must be carried out progressively. As the tube is inserted into the digestive system, the patient should breathe through the nose to relieve discomfort.
What is the difference between a pediatric nasogastric tube and an adult one?
Feeding through a catheter is used in children and infants who cannot feed on their own. The structure of a children's catheter is no different from a probe for adults, only it is smaller in size.
Some pediatric models are equipped with a syringe adapter and a radiopaque strip. Pediatric tubes should not be used for more than 2 weeks. Installation is carried out in the same way as for adults, with the difference that the tube is attached to the child’s cheek using a patch, and not to clothing.
Contraindications
It is prohibited to prescribe the procedure if there are the following contraindications:
- diseases of the digestive system of a chronic nature;
- cholecystitis (acute or during exacerbation);
- dilation of the veins of the esophagus;
- heart attacks and angina pectoris of any nature;
- tumors in the gastrointestinal tract of a chronic nature;
- narrowing of the esophagus;
- pregnancy and lactation;
- nervous and mental disorders;
- child's age up to 3 years;
- ulcer of the duodenum and stomach;
- internal bleeding;
- inflammatory processes of the gallbladder;
- abnormally formed oropharynx and esophagus;
- bronchial asthma;
- severe diabetes mellitus.
How is the result assessed?
The obtained data are compared with the average normative values. If they are lower or higher, they need to be assessed together with clinical data.
Gastric juice is also assessed visually (normally it is transparent). A yellow or brownish color indicates bile ingestion, which is associated with reflux. If there is gastric bleeding, the color of the secretion is brown, reminiscent of coffee grounds.
If red blood appears, the study should be stopped. This indicates developed gastrointestinal bleeding. A large volume of fluid received indicates increased secretion or a violation of the movement of food.
Caring for a Patient with a Gastric Tube
A nasogastric tube, the placement algorithm of which is followed by a medical professional, for intubation of the stomach, artificial nutrition, and lavage requires careful care. Just like feeding through it requires a careful approach.
Before feeding, the stomach should be rinsed with saline solution to remove accumulated mucus and food debris. After finishing feeding, the tube is clamped for 1 hour. After this, its end is lowered into a container for the outflow of food. Catheters should not be changed frequently because this may increase intracranial pressure.
In case of weakened peristalsis and absence of stool, cleansing enemas are performed, but not more than once every 2 days. After the swallowing reflex is restored, the patient is transferred to a normal diet. Liquid food is started to be given from a spoon or from a sippy cup only if the patient is able to swallow on his own.
Otherwise, food entering the trachea can lead to the development of severe pneumonia. Plaques formed on the tongue during feeding are removed with a spoon. After feeding, lips should be lubricated with a special cream.
Nutritional therapy for surgical diseases is an important part of the body’s recovery. In this case, a nasogastric tube will be a good helper, and the correct algorithm for placing it will ensure the patient’s safety.
Article design: Mila Friedan
https://youtu.be/B4wiTD4Tu4U