How can I make the procedure easier?
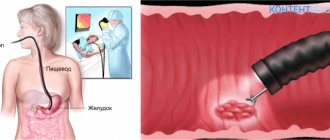
Fibrogastroduodenoscopy (FGDS) is a technique for endoscopic examination of the upper digestive system (stomach, duodenum, esophagus).
To carry it out, a special probe is used, which is equipped with a miniature camera and a manipulator. In modern endoscopy, the image is displayed on a special screen. Acidity is also constantly monitored. FGDS usually includes a test for the presence of Helicobacter pylori infection.
If necessary (for example, long-term existence of an ulcer, the appearance of neoplasms, chronic inflammatory processes), the examination is supplemented by a tissue biopsy with cytological examination in a specialized laboratory.
Reference
FGDS is the basis for diagnosing diseases of the stomach, duodenum or esophagus. It allows you to visualize changes in the mucous membrane that are difficult to see on CT or MRI.
It is based on the results of FGDS that gastritis, peptic ulcer or malignant process can be distinguished. The study is of particular importance for highly specific rapid diagnosis of Helicobacter pylori infection.
Fibrogastroduodenoscopy is prescribed if the patient has the following symptoms:
- aching pain in the upper abdomen, which intensifies after eating or drinking (especially alcoholic or carbonated);
- sensations of discomfort in the epigastrium;
- the occurrence of nausea, single vomiting;
- burning sensation behind the breastbone or heartburn;
- decreased appetite and subsequent loss of body weight;
- tendency to constipation or diarrhea.
Typically, FGDS is carried out after the patient is examined by a doctor and undergoes basic laboratory tests.
The correct approach to fibrogastroduodenoscopy can significantly improve the patient’s well-being during the procedure. Below are the main recommendations that make FGDS absolutely painless.
Choosing a qualified doctor with a friendly approach to his patients can significantly reduce anxiety before the procedure, as well as reduce the severity and frequency of side effects.
A good approach from a specialist relieves anxiety and helps the patient relax. This allows the procedure to be carried out without unnecessary trauma (for example, scratching the throat), since the probe advances more easily.
In clinical practice, there are situations when, due to low professionalism, the doctor applies the wrong or insufficient anesthetic. Also, some medical professionals do not explain the essence of the procedure, possible risks, and nuances of patient behavior.
Important
The doctor must carefully explain the nuances of preparing for the study, as well as select the most appropriate method of performing the procedure (nasal insertion of a probe, sedation or anesthesia) for a particular patient.
Many patients are scared and anxious; they do not know how to withstand a stomach examination. Some people generally cannot tolerate such procedures and do not know what to do or how to pass the FGDS.
It is usually scary to do research due to the lack of reliable information about FGDS, as well as reviews from friends. And if the patient is sure that he will be in pain during the procedure, then the risk of this complaint increases significantly, even if the study went without complications.
It is important to have contact between doctor and patient. This will help make the procedure easier. He must be ready to answer all questions that arise, as well as give truthful and objective information about why FGDS is performed, what its value is and how you can avoid the occurrence of side symptoms.
At the same time, there is no need to be afraid or ashamed if belching, increased salivation or an attack of nausea occur during the procedure.
These symptoms, to varying degrees of severity, bother most patients, but they are not a sign of the development of complications and quickly disappear after the diagnosis is completed. It is important to remember that medical staff encounter this every day, and therefore, for example, frequent belching does not bother them at all.
Before the procedure begins, the patient is given a small mouthguard that protects the probe from the teeth. In modern clinics, it is selected according to the diameter of the endoscope and the size of the patient’s oral cavity.
The procedure is performed with the patient lying on his side. During FGDS, the probe passes through the oral cavity, oropharynx, larynx, esophagus and enters the lumen of the stomach. The doctor examines the condition of the mucous membrane, takes measurements of acidity, and also tests for Helicobacter pylori infection. If necessary, a biopsy is performed.
note
The total duration of the procedure does not exceed 10-15 minutes (if the doctor collects tissue, it can take up to 20-30 minutes).
Herbal medicine or medications will help you tune in correctly to FGDS and eliminate anxiety.
Proper preparation for FGDS can significantly reduce the severity of side symptoms (especially vomiting) and increase information content. Therefore, on the day of the study, the patient should not eat. The last meal should optimally be no later than 10 hours before the test. For 2 hours, limit the intake of drinks - tea, coffee and even plain water.
To increase information content (especially if a Helicobacter pylori infection is suspected), special medication preparation is required.
It is necessary to discontinue medications that may affect the result - antisecretory agents, antacids, antibiotics, Bismuth preparations and some other medications.
Therefore, when prescribing a study, you should always warn the doctor about the presence of concomitant pathologies and medications taken.
Breathing feature
Before starting the procedure, the doctor must explain to the patient how to breathe correctly during FGDS. Breathing should be through the nose, deep and smooth. In this case (despite popular belief) there is no need to swallow while moving the endoscope through the oropharynx and larynx.
Following these recommendations will help the patient to adjust himself, promote calm and prevent sudden movements, therefore reducing the risk of injury and serious side effects.
Indications
The gastroscopy procedure is prescribed if the patient has the following symptoms:
- difficulty swallowing;
- frequent vomiting for no apparent reason;
- admixture in vomited blood;
- constant pain in the stomach area, along the esophagus;
- vague abdominal pain;
- unexplained weight loss;
- sudden loss of appetite;
- untreatable anemia.
For a newborn child, gastroscopy is performed when:
- poor weight gain;
- refusal to eat;
- constant colic;
- other health problems.
Since FGDS is not only a diagnostic, but also a therapeutic procedure, it is prescribed for the following pathological processes:
- foreign body entering the stomach;
- polyposis of the stomach or esophagus;
- consequences of chemical burns of the esophagus;
- stomach bleeding;
- neoplasms of the esophagus or stomach.
For these diseases, the doctor uses a gastroscope to carry out the required medical manipulations.
The gastroscopy procedure is not performed for all patients - contraindications to FGDS are:
- scoliosis 3-4 degrees;
- severe chest deformities;
- obstructive pulmonary diseases;
- obesity 4 degrees;
- multiple strictures of the esophagus;
- large goiter;
- severe blood clotting pathology;
- cachexia - extreme exhaustion of the body;
- early period after a heart attack or stroke.
The following may also be contraindications:
- the patient’s categorical refusal to undergo the procedure (in this case, the study can be rescheduled);
- state of severe drug or alcohol intoxication;
- acute psychosis.
The endoscopic technique is not hazardous to health, but may cause discomfort to the patient. To minimize psychological discomfort, you should prepare for FGDS in advance. In addition to the patient’s psychological mood, there is a whole list of requirements for preparing for the study. Provided you follow all the doctor’s recommendations, the procedure will be quick, painless and successful.
The essence of the examination
An endoscopic examination is performed if there is a suspicion of peptic ulcer of the stomach, duodenum, gastritis, duodenitis and a number of other pathologies of the digestive organs. A routine examination using FGDS is carried out in the process of preparing a patient for a long-term surgical intervention, as well as in the presence of serious pathologies in the liver, gall bladder or pancreas.
The procedure is performed using special equipment. An endoscope is a flexible tube about ten millimeters thick. The end of the tube is illuminated. During the examination, it is inserted into the patient’s digestive tract, and the specialist can see the organs in detail. The procedure lasts on average ten minutes.
FGDS is carried out only after preparing the patient for the study. The presence of food or water in the digestive organs will make the procedure impossible. In addition, there are a number of contraindications to gastroscopy, so such a study is not suitable for every person.
Contraindications
For a number of diseases, FGDS is strictly prohibited. Patients with the following pathologies are not allowed to undergo the procedure:
- severe curvature of the spinal column;
- aortic aneurysm, tumor and other diseases that displace the esophagus;
- blood clotting disorder;
- esophageal stenosis;
- severe conditions after a myocardial infarction or stroke;
- bronchial asthma in the acute stage;
- enlarged thyroid gland;
- during and after a hypertensive crisis.
The procedure is performed in extreme cases if the patient has:
- enlarged cervical lymph nodes;
- angina pectoris;
- mental disorders;
- third stage hypertension;
- acute inflammation in the pharynx or larynx.
The presence of contraindications does not always prevent the procedure. FGS is done in cases where the importance of the examination outweighs the risks to the patients’ health. In this case, general anesthesia may be used to minimize the risk of accidental injury.
Fibrogastroduodenoscopy is prescribed in advance so that the patient has time to prepare for it. The doctor explains in detail to the patient how this needs to be done correctly and talks about the procedure itself.
Preparation for the FGDS includes general and private events.
General measures are aimed at the doctor identifying all possible complications that may arise during the procedure, and local measures concern the patient himself.
General preparation:
- The doctor identifies contraindications and corrects conditions that are dangerous for performing FGDS. If there is a need to conduct a study, despite contraindications, the patient is sent to a hospital, where the procedure is performed under general anesthesia. If there is inflammation in the esophagus or upper respiratory tract, the infection will need to be treated first and then tested.
- When interviewing the patient, the doctor identifies possible allergies to anesthetics and other medications that may be used during the procedure. The patient must be informed about all allergic reactions to medications.
- Preparation for FGDS includes the patient’s psychological attitude towards the procedure. Many people are afraid of it, so the doctor talks in detail about how this will happen and explains the importance of the study. If the anxiety state cannot be eliminated, the patient is prescribed sedatives.
Local preparation consists of following the doctor’s recommendations:
- rules for taking medications;
- rules for eating a few days before and the evening before the procedure;
- what you need to take with you to the study;
- what can and cannot be done directly on the day of the FGS.
In order for fibrogastroduodenoscopy to be successful, it is important to carefully follow all the doctor’s recommendations. If you treat them inattentively, this will complicate the procedure and reduce its quality and information content. Therefore, the question of how to prepare for EGD of the stomach should be studied carefully.
Basic Rules
- two days before the test, it is necessary to exclude fried foods, heavy foods, alcohol, and foods that cause gas formation from the diet;
- if you have gas in the intestines or other digestive problems, you need to take Espumisan, Festal and similar drugs approved by your doctor;
- the last meal should be taken at least twelve hours before the procedure, that is, the night before;
- on the day of FGDS, drink water or tea four hours before the procedure;
- in the morning you can brush your teeth, give an injection if necessary, or take lozenges;
- You should not smoke several hours before the test, as this stimulates the production of gastric juice and can cause a gag reflex.
Clothes should be comfortable and not brand name. It is not advisable to use cosmetics or perfumes that may cause allergies among medical staff. Your attending physician will explain in more detail how to prepare for an FGDS of the stomach during your consultation.
You must bring the following things to the office where the procedure is performed:
- replacement shoes;
- medical record, doctor’s referral and other necessary documents;
- towel or napkin.
On the day of the procedure, it is strictly forbidden to drink alcoholic beverages or take pills. Smoking is prohibited several hours before the test.
Tablets should not be taken because of the possibility of injuring the esophagus during swallowing of a solid substance. You can take absorbable medications or give an injection.
Often patients drink alcohol for courage, because they are afraid to undergo this test. However, a doctor may refuse to perform a gastroscopy on a patient who has been drinking.
The last meal is taken the night before, a few hours before bedtime. It is advisable to prepare a light dinner. Porridge and fermented milk products are well suited for this purpose. If a person does not have serious stomach problems, then you should not limit yourself too much, since by the time of the study it will already have time to be digested.
In the morning, three to four hours before the procedure, you are allowed to drink one or two glasses of tea or water. You can't drink anymore. If you feel thirsty, you can take water with you and drink it immediately after completing the study.
Many patients are afraid of fibrogastroduodenoscopy. In order to make it easier to endure FGDS, you need to relax, this way the procedure goes faster and the person experiences less discomfort. In fact, swallowing a tube does not cause pain, only discomfort from belching and gag reflexes. If you have a positive attitude, you can avoid worries.
- Trust the doctor. If the patient is confident that the procedure is performed by a competent doctor, then he is less nervous and tolerates FGDS more easily. There are many clinics offering such services. You can choose the best one, where experienced specialists work.
- Don't be ashamed. Regurgitation and salivation are a natural process in this study. If you try to hold back, it will complicate the procedure and cause muscle spasm.
- Positive attitude. After waking up, you need to set yourself up to the fact that everything will go well. Even if unpleasant moments arise, they are tolerable and will last only a few minutes.
- No pain. Local anesthesia is given before swallowing the tube, so there will be no pain. Awareness of this fact will help make it easier to endure FGDS.
- Medicines. If you still cannot overcome the attacks of fear and panic, then you can drink sedatives, for example, valerian.
Correct breathing
Some clinics teach patients how to make it easier to undergo an FGDS with the help of proper breathing. Experts recommend breathing only through your nose, slowly and deeply.
Inhaling air through the mouth will provoke a cough, as saliva can enter the respiratory tract. This, in turn, can trigger the gag reflex.
As a result, it will be difficult for the doctor to insert the tube into the digestive tract, and the procedure will be delayed.
Consequences
Complications after FGDS are not common. The following unpleasant phenomena may occur:
- In the first hours, nausea and discomfort in the stomach may persist.
- Since the tube mechanically affects the larynx, pain may occur when swallowing for some time.
- Sometimes injuries to the larynx and stomach occur. This happens when the patient behaves restlessly and twitches during the examination.
- When performing additional manipulations, for example, taking material for a biopsy, bleeding may occur.
- If the device is not handled properly, the walls of the organs may become inflamed due to infection.
https://youtu.be/QmCeXUabM9Q
Methods for painless gastroscopy
In modern medicine, there are a number of procedures that patients fear. One of them is fibrogastroduodenoscopy. FGDS, as experts abbreviately indicate in the referral, is considered the most accurate method of examining the gastrointestinal tract.
The procedure, performed using a flexible fiber-optic endoscope, consists of simple but rather unpleasant manipulations that cause panic.
However, there are a certain number of rules and tips on how to make it easier to undergo an FGDS, minimizing discomfort and obtaining a highly informative result.
- The nurse treats the root of the tongue with lidocaine to relieve pain and reduce the gag reflex.
- The patient lies on the couch and takes the correct position on the left side, straightening his back and pulling his knees to his chest.
- A special mouth guard with a hole in the center is inserted into a person’s mouth to insert an endoscope – a thin fiber optic tube with a small camera at the end.
- The tip of the probe is lubricated with a light gel to improve glide, and is inserted into the larynx through a hole in the mouthpiece. As directed by a specialist, it is necessary to periodically perform swallowing movements.
- Next, the probe enters the stomach or duodenum (depending on the purpose of diagnosis). The doctor begins to rotate it in different directions, examining in detail every centimeter of the mucous membrane. If necessary, air is supplied to the organ cavity to straighten internal folds and improve visual inspection.
- A biopsy sample (a piece of tissue) is taken using a special pin inserted directly through a video probe.
- Upon completion of the study, the fibrogastroscope is removed from the body, and the insert is removed from the mouth. If there are unpleasant symptoms: nausea, weakness, the patient is asked to lie down for some more time.
If the study is performed correctly, it does not cause severe discomfort or pain, as a result of which many people tolerate it well. An experienced doctor helps you tune in psychologically, which makes the procedure easy and as fast as possible.
Some people worry about the occurrence of a gag reflex and excessive salivation, but these natural manifestations are considered secondary. The main thing that is required of the patient is to follow the advice of the gastroenterologist.
General recommendations
As you can see, performing the study is not difficult for both the doctor and the patient. But to make it easier to bear, you need to adjust accordingly. Preparation usually takes place at home, and consists of correcting nutrition, emotional relaxation, and training in proper breathing.
Nutrition correction
The endoscopic procedure is scheduled in advance with the calculation of the availability of time for full preparation. A week before the specified date, you need to adjust your diet, replacing regular meals with lighter and more quickly digestible ones. To do this, you should exclude certain products:
- fatty meats, poultry, fish;
- sausages;
- hot and spicy spices, seasonings;
- seeds, nuts;
- baked goods;
- legumes;
- heavy mayonnaise-based sauces;
- canned preparations and smoked meats;
- cream, milk;
- carbonated drinks, coffee, alcohol.
You should also limit the consumption of bread, sweets, chocolate, fresh vegetables and fruits, and strong tea as much as possible.
Refusal of medications
It is not recommended to take any medications specifically to alleviate the condition and relieve anxiety.
The exception is medications that were prescribed before diagnosis for health reasons.
In this case, to minimize the risk of complications, the gastroenterologist should be notified, and the drug should be kept in the mouth until it is completely dissolved, and not swallowed as usual.
If there is increased psychological discomfort, immediately before the start of the process, the patient is asked to take a medicine with a sedative effect.
To give up smoking
There is no strict ban on smoking, however, everyone knows that it is a bad habit. Some people try to take a long drink for the purpose (as it seems to them) of relaxation and calm.
But studies confirm that the entry of smoke and harmful substances into the respiratory tract causes vasospasm, the formation of mucus and, oddly enough, provokes excessive nervousness.
In addition, nicotine consumption promotes the secretion of digestive juice, and since it remains unspent in an empty organ, the results may be distorted.
Therefore, an experienced specialist insists on this restriction and advises to refrain from the addiction for at least a day.
In the last decade, techniques have begun to be actively used that can significantly reduce discomfort or even painlessly undergo gastroscopy of the stomach:
- Sedation. Sedation will help you survive FGDS calmly without fear. The patient is injected intravenously with a drug from the group of benzodiazepines, after which he falls asleep. The procedure is widely carried out and makes it easier to endure unpleasant sensations and painlessly perform FGDS of the stomach for adults and children. A few minutes after completion of the study, the patient wakes up. In an hour he can go home. The risk of side effects is low.
- Anesthesia (general anesthesia). Used more rarely under the supervision of an anesthesiologist. The patient is given several drugs for pain relief, but mechanical ventilation is not required. Usually performed before planned surgery.
Capsule endoscopy. This is an innovative technique in which the patient does not have to swallow the tube. Instead, it swallows a small capsule-shaped chamber that travels all the way through the digestive system. The image is recorded and then viewed by a doctor without any problems. Among the disadvantages of capsule endoscopy is the impossibility of a more thorough examination of the changed area of the mucosa, conducting a Helicobacter test or biopsy. Helps those who cannot undergo the standard FGDS procedure.
Insertion of a probe through the nose (transnasal technique) is also used. This technique provides a more comfortable FGDS, since it causes nausea much less often and does not affect hemodynamic parameters (which is important for patients with cardiovascular diseases). A probe with a significantly smaller diameter is used - 5.4 mm (standard - 11 mm). When asked whether it is painful to do gastroscopy of the stomach in this way, many patients answer negatively.
Some diseases can be diagnosed using less unpleasant procedures: x-rays of the stomach and ultrasound of the abdominal cavity.
The leaflet given to patients provides the following advice:
- Fast 12 hours before the actual examination. You can't drink either. Dinner should include foods that are easily digestible and do not irritate the gastric mucosa. If you break this rule and eat spicy, sour or pickled foods and foods, you can distort the results of the study.
- Nuts and chocolate should not be consumed. Particles of these products may remain in the folds of the mucous membrane, which also interferes with normal gastric gastric gastroscopy. It is better to eliminate them within 2 days. Also remove foods that cause gas from your diet.
- Only essential medications are allowed. It is better to exclude others. And those that need to be taken should be dissolved rather than swallowed whole, and you should definitely warn your doctor about this.
How to behave during the procedure:
- Calm down and relax. Fear causes excessive tension in the muscles of the esophagus, which interferes with the free passage of the gastroscope. The more afraid you are, the longer the procedure will take. Patients should understand that drooling and belching during FGDS are normal manifestations. Doctors do not want to hurt the patient; on the contrary, they try to carry out the manipulation as painlessly as possible. But not everything depends on them. If you are tense, gastroscopy will not be easier. Some patients say, “I'm afraid to do a biopsy.” But it's not scary at all. The material is collected under local anesthesia.
The patient who comes to the FGDS must be ready to interact with the doctor
- Smoking and drinking alcohol is prohibited. Strictly speaking, smoking is not absolutely prohibited, but it causes vasospasm and excessive nervousness. It is better to put off cigarettes before doing FGDS.
Breath
You only need to breathe through your nose. If you try to breathe through your mouth, the saliva that is released abundantly during gastroscopy can enter the respiratory tract and cause a cough.
Inhalation and exhalation should be slow and deep. If you do the opposite, it will obstruct the passage of the gastroscope and can lead to injury to the esophagus.
Modern gastroscope
The following arguments can be given to fearful patients:
- If the patient is calm and breathes correctly, then he will only have to endure a few unpleasant moments while the doctor inserts the gastroscope.
- The doctor uses a mouthguard that prevents the teeth from clenching.
- Deep breathing quickly relieves the gag reflex. The patient will only experience discomfort from a foreign body in the esophagus, and then in the stomach.
The patient lies on the couch on his left side. For the correct position, you need to bend your knees to your chest and straighten your back. The root of the tongue is sprayed with lidocaine to relieve pain and relieve the gag reflex, which makes it possible to easily and quickly insert the endoscope into the stomach.
What is fibrogastroduodenoscopy?
The purpose of the procedure is to examine the surface of the stomach and duodenum from the inside.
To do this, a tube with a special device (endoscope) at the end is inserted into the patient’s esophageal passage through the oral cavity, with the help of which the internal organs are visualized. FGDS, scheme
https://www.youtube.com/watch?v=QmCeXUabM9Q{amp}amp;modestbranding=0{amp}amp;controls=1{amp}amp;rel=0{amp}amp;showinfo=1{amp} amp;enablejsapi=1{amp}amp;origin=
FGDS makes it possible to accurately assess the functioning of the gastrointestinal tract and its anatomical structure, detect changes, determine the location and scale of pathological processes (hemorrhages, benign and malignant tumors) and begin treatment in a timely manner.
Carrying out FGDS
Indications for performing FGDS include digestive disorders, manifested by heaviness in the epigastric region, nausea, heartburn, pain, bloating and other symptoms.
The study is recommended for patients with suspected peptic ulcers, gastritis, tumors in the stomach and esophagus, bleeding from the digestive tract.
FGDS allows not only to diagnose diseases and pathologies, but also, if necessary, to take tissue samples for biopsy.
How is a biopsy performed?
Since fibrogastroduodenoscopy is considered a rather complex diagnostic procedure, the patient’s consent is required for its implementation (if a person categorically refuses diagnosis, FGDS is not performed).
FGDS is carried out only with the consent of the patient
In addition, there are a number of pathologies and diseases in which its implementation is prohibited:
- myocardial infarction in the acute stage, any disturbances of cardiac activity;
- severe pathologies of the respiratory system;
- diseases that can provoke displacement of the esophagus (aortic aneurysm, tumors);
- esophageal stenosis;
- curvature of the spinal column;
- stroke;
- enlarged thyroid gland;
- severe bronchial asthma;
- bleeding disorders;
- pregnancy.
FGDS is not performed during pregnancy
Relative contraindications include acute inflammatory processes of the pharynx and larynx, enlarged lymph nodes in the cervical region, hypertension and angina pectoris, as well as some mental disorders when the patient is unable to control his body.
Before performing an FGDS, the individual characteristics of the body and the presence of factors that can cause complications during gastroscopy are taken into account.
Contraindications to FGDS are relative - in emergency cases (a foreign object entering the esophagus, posing a threat to the patient’s life, severe bleeding), the procedure can be performed in the presence of serious diseases. The attending physician can correctly weigh the risks and benefits of diagnostics.
Carrying out FGDS in special cases
Preparation for FGDS
In order for the procedure to cause a minimum of discomfort and give accurate results, the patient needs to properly prepare for it.
A week before diagnosis, it is necessary to exclude from the diet all foods that can cause irritation of the mucous membranes, avoid drinking alcohol and not smoking. This allows you to achieve a normal level of acidity and will facilitate the implementation of FGDS.
Before FGDS you need to give up bad habits
Some medications can negatively affect the gastrointestinal tract and distort diagnostic results, so you should, if possible, stop taking medications or replace them with others after consultation with your doctor. You can give injections or take medications in the form of drops.
It is better to consult your doctor about taking medications
You should not eat food on the eve of the study. Normally, it is cleared from the stomach within 8 hours, but seeds, oatmeal, nuts, chocolate and other indigestible foods remain in the cavity for several days, which makes diagnosis difficult.
Oatmeal and chocolate are foods that should be excluded from your diet a few days before the FGDS
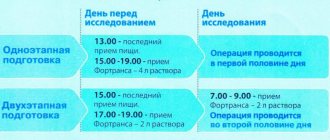
If FGDS is scheduled for the morning, you can have dinner no later than 18-20 pm, and the dishes should be light and nutritious (buckwheat porridge, chicken, stewed vegetables).
Buckwheat with chicken is the optimal dish for dinner before the procedure
Sometimes the diagnosis is scheduled for the second half of the day - then the patient can eat a light breakfast, but the interval between the meal and the procedure must be at least 8 hours. Drinking any drinks, including water, is also prohibited: the recommended interval between drinking and FGDS is 5 hours.
You can drink water 5 hours before the procedure
The psychological attitude also plays an important role - FGDS is an unpleasant procedure, but it should be endured for the sake of your own health.
You need to mentally prepare for the procedure and calm down as much as possible.
Fibrogastroduodenoscopy (FGDS, gastroscopy) - review
| View | Description |
| Classical | It is carried out without anesthesia; the patient swallows a tube after applying an anesthetic spray to the pharyngeal mucosa. Used in most subjects |
| With anesthesia support | Some categories of patients require anesthesia in order to be able to fully carry out the manipulation. A short-term general anesthesia is used, during which the muscles of the pharynx and esophagus relax, allowing the doctor to insert the endoscope |
| Planned | It is carried out by appointment, for patients who do not require an urgent diagnosis. |
| Emergency | It is carried out for vital indications, when it is urgently necessary to determine what happened to a person. The risk of complications increases due to lack of proper preparation |
| Diagnostic | Used only for examining the mucous membrane of the esophagus, stomach and intestines, identifying pathological changes |
| Medical | In addition to the examination, the doctor can carry out the required treatment measures:
|
Using gastroscopy, a doctor can diagnose the following diseases:
- various tumor neoplasms - polyps, cysts, cancer of the esophagus or stomach;
- gastritis - erosive, atrophic, hypertrophic;
- gastroesophageal reflux disease;
- Barrett's esophagus;
- Mallory-Weiss syndrome;
- ulcers of various parts of the digestive tract;
- wounds to the mucous membrane.
With the help of endoscopic equipment, dilation of the esophageal veins can be detected, which is one of the signs of liver cirrhosis.
Photo gallery
The photo shows the main nuances of the implementation of FGDS and the detected pathologies
Location of the endoscope in the stomach Scheme of FGDS Types of pathologies Biopsy using an endoscope
During the FGDS, the doctor evaluates the following parameters:
- color of the mucous membrane throughout the examined area of the gastrointestinal tract;
- the presence of folds of the mucous membrane;
- integrity of all shells;
- the presence of inflammatory changes and neoplasms;
- severity of peristalsis.
If there are pathological changes for each item, they are described in the conclusion.
The video describes the FGDS procedure. Filmed by TNT channel.
Indications
The gastroscopy procedure is prescribed if the patient has the following symptoms:
- difficulty swallowing;
- frequent vomiting for no apparent reason;
- admixture in vomited blood;
- constant pain in the stomach area, along the esophagus;
- vague abdominal pain;
- unexplained weight loss;
- sudden loss of appetite;
- untreatable anemia.
For a newborn child, gastroscopy is performed when:
- poor weight gain;
- refusal to eat;
- constant colic;
- other health problems.
Since FGDS is not only a diagnostic, but also a therapeutic procedure, it is prescribed for the following pathological processes:
- foreign body entering the stomach;
- polyposis of the stomach or esophagus;
- consequences of chemical burns of the esophagus;
- stomach bleeding;
- neoplasms of the esophagus or stomach.
For these diseases, the doctor uses a gastroscope to carry out the required medical manipulations.
Contraindications
The gastroscopy procedure is not performed for all patients - contraindications to FGDS are:
- scoliosis 3-4 degrees;
- severe chest deformities;
- obstructive pulmonary diseases;
- obesity 4 degrees;
- multiple strictures of the esophagus;
- large goiter;
- severe blood clotting pathology;
- cachexia - extreme exhaustion of the body;
- early period after a heart attack or stroke.
The following may also be contraindications:
- the patient’s categorical refusal to undergo the procedure (in this case, the study can be rescheduled);
- state of severe drug or alcohol intoxication;
- acute psychosis.
Preparation
In order for the patient to endure the procedure easily psychologically and physically, the doctor tells how to prepare for it.
Nutrition
A person is warned about a planned FGDS 2-3 days in advance. At this time, he follows a special diet and prepares himself mentally for the procedure.
It is recommended to temporarily exclude the following foods from the diet:
- fatty meat and fish dishes;
- mushrooms;
- baking;
- seasonings and spices;
- sausages;
- fatty cheese, milk;
- legumes;
- sweets;
- bread;
- cabbage;
- coffee;
- alcohol.
A person’s menu before an FGDS consists of:
- chicken meat;
- lean fish;
- stewed vegetables;
- porridge with water;
- weak tea.
On the eve of the study, you can eat a light dinner. Since FGDS is usually done in the morning on an empty stomach, you can drink water no later than three hours before the procedure.
General recommendations
Additional proper preparation is carried out taking into account the following nuances:
- a few days before the procedure, it is recommended to quit smoking (or reduce the number of cigarettes as much as possible);
- if a person is forced to take any medications for medical reasons, the doctor who will conduct the FGDS should be notified about this;
- If the tablet needs to be taken in the morning, it is not swallowed, but dissolved in the mouth.
The moral preparation of the patient is of great importance, because if a person has a strong fear of the upcoming procedure:
- the patient will be nervous, which will prevent him from swallowing the probe;
- the doctor will not be able to fully examine the stomach.
The patient needs to understand that the procedure is painless, so the better the person relaxes, the easier it will be for him to survive the manipulation.
It is important not to be afraid of the upcoming procedure and to set yourself up positively - for this you can:
- meditate on the eve of the study;
- take a sedative;
- talk to a psychologist.
Sometimes gymnastics helps you get into the right mood.
During FGDS, the patient is only required to lie still and breathe correctly, while:
- breathing should be carried out only through the nose, without using the intercostal muscles and diaphragm;
- you need to inhale the air slowly and deeply, measuredly;
- It is best to mentally count the rhythm while breathing.
Deep breathing helps you calm down, especially if you are very afraid of pain.
To reduce or alleviate the severity of the gag reflex, first of all, you must strictly follow the doctor’s recommendations.
The urge to vomit during FGDS occurs in a person due to irritation of the root of the tongue with the gastroscope hose, therefore:
- to reduce the sensitivity of nerve endings, this area is irrigated with an anesthetic - lidocaine or ultracaine;
- reduction of muscle tension is achieved by administering muscle relaxants;
- During insertion of the tube, the person must actively swallow the probe - this will reduce the pressure on the root of the tongue.
Description of the procedure
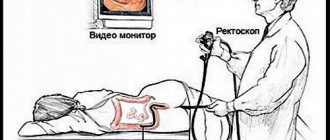
Planned FGDS is prescribed in the morning. The procedure is carried out in an equipped endoscopy room.
Before manipulation, it is necessary to remove objects squeezing the body:
- belts;
- chains;
- tight clothes.
Step-by-step process of the procedure:
- An hour before gastroscopy, the patient is given premedication - 1 ml of atropine and 1 ml of trimeperidine are administered intramuscularly.
- The person is placed on the couch on his left side. You can bend your legs slightly and wrap your arms around yourself at elbow level. Place a tray in front of your face. During the examination, you need to behave correctly - you cannot move, turn your head, swallow saliva, or talk.
- The patient is given a silicone insert to clamp between the teeth, through which the probe is inserted. It is necessary to prevent damage to the gastroscope. If it is impossible to perform the procedure due to the person’s strong tension or a pronounced gag reflex, anesthesia is performed - then it will be painless.
- Next, the doctor inserts a tube into your throat. You need to swallow it while taking a deep breath. When the tube passes through the pharyngeal ring, the discomfort stops.
- The endoscopist examines the internal organs. Sometimes it is possible to go through the intestine completely and examine the place of its transition to the next section.
- After this, the doctor carefully removes the gastroscope tube.
Photo gallery
Complete insertion of the probe Inspection directly through a gastroscope Inspection on the screen Gastroscopy under anesthesia
The gastroscope probe has a diameter of 1.5-2 cm, so it does not cause pain when swallowing. Only discomfort appears from the presence of a foreign object in the throat.
The thickness of the tube for small children is even smaller - 5-10 mm. Therefore, there is no need to worry about pain, because the diameter of the esophagus is much larger and the tube will pass through it absolutely freely.
Initially, healthy people do not often need to undergo gastroscopy. FGDS is carried out only according to indications, on which the regularity of the manipulation will depend. It is prescribed when appropriate symptoms appear; the further number of examinations depends on the established diagnosis.
If you have uncomplicated gastrointestinal diseases, the test can be taken once a year. Severe pathologies - with complications, rapidly progressing - require gastroscopy every 3-6 months. In most cases, the frequency of FGDS is determined individually.
If it is absolutely impossible to perform a classic gastroscopy, if the patient has contraindications, there is an alternative method of visual examination of the gastrointestinal tract.
This is a capsule FGDS - the patient swallows not a tube, but a small chamber in the form of a capsule. It sequentially passes through all parts of the gastrointestinal tract and leaves the body naturally.
The data recorded by the camera is then transferred to a computer where the doctor can study it.
As with classical gastroscopy, there are several contraindications:
- swallowing disorder;
- installed pacemaker;
- epilepsy;
- intestinal obstruction.
The preparation required is the same as for conventional FGDS. The capsule passes through the entire gastrointestinal tract in 12-14 hours, so the test result is issued the next day.
Capsule FGDS
Fibrogastroscopy has a number of positive and negative aspects, taking into account which the need for it is determined.
| Advantages | Flaws |
|
|
Features of FGDS and expert advice
Diagnosis is most often carried out in the morning. The person being examined takes a position on his left side, on a special table. You should first get rid of items of clothing that put pressure on the body (belts, narrow collars, and jewelry).
Following the advice of doctors will allow you to undergo the procedure without pain.
The nurse treats the patient's throat and mouth with a spray solution that reduces sensitivity (anesthetic). In the presence of allergic reactions, treatment is not performed. The patient must inform in advance about chronic pathologies and allergies.
With his teeth, a person clamps a special insert through which the tube of the device is inserted. While taking a deep breath, the tube is passed into the throat. This is the most unpleasant moment of the procedure, which should be endured calmly. Vomiting, a characteristic sound and salivation are a normal reaction. You shouldn't be afraid or embarrassed about this.
The gastroenterologist examines the stomach in detail, turning the tube of the device in different directions. Tissue collection for analysis is carried out with special forceps, which are inserted into the tube. There is usually no pain during this manipulation. The movement of the fiber gastroscope tube along the esophagus and its subsequent rotation directly in the stomach does not cause pain symptoms. The patient feels only discomfort from the presence of a foreign object in the internal organs.
The main recommendation is the ability to breathe correctly during FGDS. Only the nose is involved in the process. Inhalations and exhalations should be slow and deep. It is necessary to concentrate as much as possible so that your breathing is smooth and rhythmic.
FGDS - does it hurt?
During the diagnosis, it is prohibited to: swallow air, talk, swallow drool, move your body and jerk your head. In order for the procedure to go smoothly, you must strictly follow the instructions of medical specialists, breathe correctly, do not be nervous, and try to relax all your muscles.
If you cannot get rid of excessive tension on your own, you can take a sedative an hour before the examination, and inform the medical specialist conducting the examination. In cases where the patient cannot endure stress, the doctor can perform an FGDS under general anesthesia.
You should not strive for this, as general anesthesia harms the body. When the gastroenterologist considers the procedure complete, he smoothly removes the tube of the device. The extraction process is easy, without causing inconvenience or pain. Do not suddenly move to a vertical position.
The rise should be slow, without vigorous movements. If you feel dizzy, you should tell the doctor about it and spend some time in the office.
Possible consequences
After completion of the procedure, patients may have the following complaints:
- aching pain in the epigastrium (upper abdomen), neck or behind the breastbone, which may intensify after swallowing;
- weakness, dizziness, headaches, drowsiness (if drug sedation was used);
- cough (entry of stomach contents into the respiratory tract due to improper preparation of the patient);
- allergic reactions (to anesthetic);
- heartburn or burning sensation;
- increased saliva production;
- decreased appetite;
- palpitations or increased blood pressure (due to activation of the sympathetic nervous system);
- nausea that gets worse when eating or drinking water.
Important
The severity of these complaints greatly depends on the qualifications of the doctor, as well as on the method of conducting the diagnostic procedure. They usually go away completely within a few hours.
Recommendations after the procedure:
- Diet. After completing the FGDS, you cannot eat for another 30 minutes (and if a biopsy or sedation was performed, then 2 hours). The first meal should consist of simple foods and dishes: porridge, lean meat or fish, yesterday's bread, dry cookies, hard cheese, honey.
- Peace. Avoid increased physical and emotional stress during the day.
How to do an FGD with a strong gag reflex
Reactive gag reflex is the most common problem during gastric gastroscopy. It is impossible to completely eliminate it, since it is a natural protective reaction of the body to foreign objects entering the throat. To undergo gastroscopy as comfortably as possible, you should pay special attention to preparing for diagnosis and carefully listen to the advice and instructions of the doctor performing FGDS.
Important! With proper preparation for gastroscopy, vomiting is virtually excluded, even if the patient is very nauseous. However, the urge may be so intense that the contents of the duodenum may enter the esophagus and throat.
To weaken the gag reflex during FGDS, it is necessary to reduce the pressure on the root of the tongue. To do this, the patient must actively swallow the gastroscope tube. In addition, local anesthetics and muscle relaxants are used to reduce the sensitivity of receptors and relieve spasm. If they do not help, the procedure is performed under general anesthesia. To prevent respiratory arrest and the entry of digestive tract contents into the respiratory tract, an endotracheal tube is used.
SOURCES: https://diagnozpro.ru/skopiya/gastroscopy/kak-legche-perenesti-fgds https://diagnostinfo.ru/skopiya/gastroscopy/kak-legche-perenesti-fgds.html https://apkhleb.ru/ endoskopiya/kak-legko-proyti-proceduru-fgds
FGDS under anesthesia: painless and fast
Is it possible to perform FGDS without pain? Recently, the method of gastroscopy during sleep has been gaining popularity. This is a completely similar study as described above, only in this case the person sleeps and does not feel anything. A person falls asleep under the influence of special anesthetic drugs. This is a kind of anesthesia, only short-term (from 5 to 15 minutes).
The advantage of FGDS under anesthesia is the fact that the person sleeps and does not feel everything that is felt with the traditional research method. Gastroscopy during sleep differs from the traditional method not only in the absence of unpleasant sensations, but also in cost. For comparison: the traditional method will cost 500-1000 rubles, depending on the duration, and gastroscopy in a dream will cost from 3000 to 9000 rubles. Therefore, not everyone, even the most suspicious person, can afford such luxury. With FGDS, a person does not feel anything during sleep, but after waking up, a sore throat occurs, which can last no more than 1 day.
It is important to know! During gastroscopy without anesthesia, a person experiences not only gagging, but also a feeling of shortness of breath. Shortness of breath occurs if the patient does not listen to the doctor and does not follow his instructions.
In conclusion, it should be noted that although the FGDS procedure is an effective research option, it also has its contraindications. Gastroscopy is prohibited for the following diseases:
- inflammatory processes in the mouth and pharynx;
- myocardial infarction;
- disruption of cerebral circulation;
- other types of disorders.
FGDS during pregnancy is permitted only on the recommendation of the attending physician. A timely detected disease is much easier to cure than in an advanced stage.