The appearance of growths on the intestinal walls is associated with the development of a tumor. At the initial stage, the neoplasm is benign, but due to provoking factors it becomes an oncological manifestation. If conservative treatment was not provided on time, then the patient needs surgery for rectal cancer. To remove a malignant tumor, there are several methods of performing a surgical procedure.
How are they treated?
The method of treatment for rectal cancer is determined depending on the patient’s condition, location and size of the tumor. The central method of treatment is surgery. But at stages 3-4 it is not enough, and an integrated approach is used:
- Radiation therapy before and after surgery;
- Surgical intervention;
- Polychemotherapy.
Comprehensive treatment greatly increases the chances of recovery.
On average, rectal cancer surgery costs:
- in Israel - from $20,000;
- in Germany - from € 15,000;
- in Russia - from 20,000 rubles.
Proctectomy
In some cases, the entire rectum and surrounding lymphoid areas must be removed. This procedure is called proctectomy. It ends with a colo-anal anastomosis - the end of the large intestinal tract is sutured to the anus.
Normally, the rectum acts as a container in which excrement accumulates. After proctectomy, this function will be performed by the final section of the colon. For this purpose, the surgeon is able to form an unnatural J-shaped reservoir and apply an anastomosis according to the “end to side” type, which will help reduce the frequency of bowel movements and guarantee stool density as close as possible to the standard one.
Preparing for surgery
Before surgery to remove rectal cancer is performed, the patient is examined by:
- Palpation;
- Ultrasound of the abdominal cavity;
- Endosonography;
- Chest X-ray;
- Blood and stool tests;
- Rectoscopy;
- Colonoscopy.
It is important to eat right before tumor removal.
Diet for rectal cancer before surgery:
- Fractional (5-6 times a day) diet;
- Low-fat fermented milk products (mashed fresh cottage cheese, 3-day kefir, fermented baked milk, yogurt);
- Vegetables (carrots, cauliflower, broccoli, tomatoes, beets, zucchini, spinach);
- Fruits (apples, plums, apricots);
- Berry purees and compotes;
- Cereals, bran, buckwheat, pearl barley and oatmeal;
- Lean beef, rabbit, chicken, turkey;
- Lean fish and seafood;
- Food is only boiled or steamed.
Before the operation (under general anesthesia), the patient's stomach is cleansed and an antibiotic is given.
Why is it better to perform anterior rectal resection at the Swiss University Hospital?
- The clinic was among the first to perform sphincter-preserving operations; to date, the number of surgical interventions on the intestines has exceeded 3,000 operations.
- We employ specialists of the highest category, many of whom, being authorities in surgery, are known not only in domestic but also in foreign clinics. Each of our specialists is fluent in all techniques and can perform more than 100 types of operations within their specific area.
- Every year we consult about 5 thousand people, including patients with proctological pathologies referred from other clinics.
- For diagnostics, our Center carries out almost all necessary studies: from laboratory tests to complex examinations using video endoscopic or computer technology. Thanks to the presence of a histological laboratory, the time for examining patients is minimal, which is extremely important for patients with cancer.
- If necessary, doctors of other specializations can be involved in the diagnosis and treatment of patients with concomitant diseases: endocrinologists, gynecologists, vascular surgeons, etc.
- We were one of the first to carry out simultaneous operations: during one anesthesia, the patient can get rid of other pathologies of the abdominal cavity or pelvic organs.
Types of operations
Operative surgery depends on the characteristics of the tumor and the patient's condition.
At stages 1-2, the tumor, affected tissues and lymph nodes, and nearby healthy tissues are removed to avoid the danger of metastases.
- Gentle local resection is most effective at stage 1 cancer. The tumor is removed using an endoscope.
- Open laparoscopy keeps pain and recovery time to a minimum. Used at stages 1-2.
- The non-contact operation begins with ligation of the blood and lymph vessels associated with the tumor. Then the affected area is cut off.
- Transanal excision eliminates small tumors in the lower segment of the intestine, preserving the sphincter and lymph nodes.
- An anterior resection is applied to a tumor in the upper part of the bowel. The lower abdomen is incised, the junction of the rectum and sigmoid colon is removed, and the ends of the intestine are sewn together.
- Low resection is used at stages 2-3. The rectum is removed, the sphincter is preserved. A temporary stoma (an opening in the abdominal wall to drain stool) may be needed.
- Abdominoperineal extirpation - removal of the rectum, sections of the anal canal and sphincter muscles to create a permanent stoma.
Sphincter-sparing operations minimize negative consequences and guarantee a significant length of life without reducing its quality.
Is it possible to do without surgery?
At this stage, treatment without surgery for rectal cancer is impossible.
Radiation and chemical therapy cannot replace surgery. They are only part of a comprehensive treatment.
Both types of therapy are used before and after surgery to shrink swelling, speed recovery, and reduce the risk of recurrence.
Classification
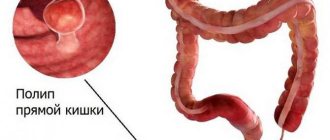
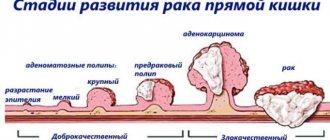
Rectal tumors can be benign or malignant. Benign neoplasms include epithelial, non-epithelial tumors and carcinoid. Epithelial neoplasms are represented by polyps, villous tumors and familial diffuse polyposis of the colon. The following types of rectal polyps are distinguished: glandular and villous-glandular (adenopapillomas, adenomas); miliary (hyperplastic); fibrous; juvenile (cystic-granulating). A submucosal carcinoid tumor of the rectum may be mistaken for a polyp. A villous tumor is characterized by multiple papillary growths of the rectal epithelium, represented either by a separate pedunculated node or by a fairly large area of neoplasia affecting a significant part of the rectum. Such a tumor has a very high potential for malignancy and therefore must be radically removed as soon as possible after detection.
Non-epithelial neoplasms of the rectum are extremely rare; they develop from muscle, fat, nervous and connective tissue, vessels of the blood and lymph circulatory system. These neoplasms are usually localized in the submucosal or muscular layer, under the serous membrane, and in those areas where it is absent, they spread to the surrounding perirectal tissue. Among benign rectal tumors of non-epithelial nature, fibromas, myomas, lipomas, cavernous angiomas, neurofibromas, and lymphangiomas are most often diagnosed.
Carcinoid is a neuroendocrine neoplasm that produces hormone-like substances (serotonin, prostaglandins, histamine and others). The clinic is determined by the substance that the tumor secretes and its concentration. Carcinoid requires surgical treatment.
Malignant tumors of the rectum are also divided into epithelial (cancer: glandular - adenocarcinoma, squamous cell, signet ring cell, solid, scirrhus, mixed; melanoma, melanoblastoma) and non-epithelial (leiomyosarcoma, lymphoma, angiosarcoma, neurilemmoma, rhabdomyoma and unclassified tumors). About 70% of rectal tumors are cancer. Based on the growth pattern of the tumor node, endophytic, exophytic, diffuse tumors and squamous cell carcinoma of the skin of the anus and anus are distinguished. In 85% of cases, cancer is localized in the ampullary part of the rectum.
Consequences of the operation
Any surgical intervention may involve risks.
Unpleasant consequences may include:
- Bleeding into the peritoneum;
- Infections;
- Long healing period;
- Rupture of the stitched ends of the intestine and inflammation (peritonitis);
- Digestive disorders;
- Fecal and urinary incontinence;
- Sexual dysfunction (impotence);
- Fusion (adhesions).
After surgery, rectal cancer may return within 2 years. In order to detect metastases in time, you need to constantly see a doctor (every 3-6 months), undergo a colonoscopy and examinations, and do a blood test.
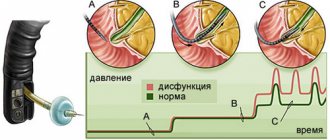
Diagnosis before resection
Malignant tumor is the main disease. which may lead to the need for rectal resection. Signs of cancer most often make themselves felt in the later stages, the symptoms are as follows:
disturbances in the regularity of bowel movements; pain that is felt during defecation; the presence of pus, mucus and blood in the stool; tenesmus, or false and painful urge to defecate.
As the disease progresses, it becomes difficult to pass stool, constipation and serious bowel dysfunction occur. A blood test determines the presence of anemia, which is a low concentration of red blood cells.
Diagnostic procedures used to detect cancer:
examination by a proctologist; anoscopy; sigmoidoscopy; MRI; ultrasonography.
How to eat?
Nutrition after surgery may be the same as before the illness. Regulating your bowel movements will help you avoid stomach upsets, bloating and unpleasant odors.
The recommended diet after surgery is the same as before:
- You need to avoid fatty, spicy and fried foods - it is better to stew, boil or steam.
- Drink at least 2 liters of fluid per day between meals.
- Eat small meals (5-6 times a day) and chew your food thoroughly, do not eat very hot or cold foods.
Preparatory stage
The day before the resection, it is necessary to clear the intestines of feces. For this purpose, enemas and special laxatives are prescribed. Thorough bowel cleansing significantly reduces the risk of complications. You are not allowed to eat solid food the entire day before surgery. Only water, broth, teas, compote are allowed.
You should also take all medications prescribed by your doctor strictly according to schedule. It can be:
beta blockers - reduce the risk of heart complications in patients with vascular atherosclerosis; diuretics – reduce the risk of a heart attack that can occur due to excess fluid in the body; Antihypertensive drugs help stabilize blood pressure during surgery.
It is prohibited to take medications that affect blood clotting before surgery. These are NSAIDs (in particular ibuprofen and aspirin), anticoagulants. Taking medications for diabetes must be discussed with your doctor.
How long do they live after surgery?
Life expectancy after tumor removal depends on several factors:
- The stage at which the disease was diagnosed. After surgery at stage 1, 90-95% of patients survive, at stage 2 - 75%. At 3 up - 50%, and at 4 - 5-8%.
- The size of the tumor seriously affects prognosis after surgery. With superficial lesions, 85% of patients survive, with muscle lesions - 67%, expanded metastases reduce the chances to 49%.
- Patient's age: among patients under 30 years of age, the survival rate is significantly lower than among older people.
- Level of resection: resection at the tumor border gives a chance of 55% of patients. For resection at a greater distance - 70%.
At the same time, patients with rectal cancer live without surgery for no more than a year. Therefore, it is a timely visit to a doctor that can save a life.
Causes
The main causes of the development of rectal tumors are precancerous diseases, single and multiple intestinal polyps, chronic constipation, bedsores and rectal ulcers, disorders of the immune system, the negative influence of carcinogens and genetic factors. Most patients with cancer of this localization experience an immune imbalance, in which antitumor immune cells cease to function properly. As a result, the formation and further proliferation of tumor cells occurs. The immune mechanism for the development of rectal tumors is usually combined with other mechanisms of carcinogenesis. In particular, chronic intestinal inflammation plays a large role in the formation of the oncological process.
Precancerous intestinal pathologies include such common diseases as proctitis, hemorrhoids, anal fissure, paraproctitis, proctosigmoiditis, ulcerative colitis and Crohn's disease. Carcinogens such as nitrites, industrial poisons, chemicals, radiation, saturated fats, various viruses, and so on play an important role in the development of tumors. One of the most important factors in the appearance of rectal tumors is hereditary predisposition: an increased risk of incidence is observed in people whose immediate relatives have colorectal cancer.