Emergency care for pancreatitis will differ depending on the nature of the disease. In acute cases, assistance measures are carried out while waiting for an ambulance, and in chronic cases - at home to eliminate the symptoms of the attack and only after stabilization of the condition, the patient needs to contact a gastroenterologist or call him at home.
- First aid and acute pancreatitis
- First aid in cases of exacerbation
Characteristic symptoms
In cases of exacerbation of the pathology or its manifestation in an acute form, the main symptomatic sign is pain. They can appear in almost any part of the upper abdomen. In addition, the nature of the pain may also differ.
All these contradictory symptoms are united by a common “painful” symptom: special intensity. The pancreas contains many nerve endings. They take an “active part” in the process of inflammation, so the pain is so severe that without relief it leads to painful shock. The patient is unable to lie or move. Temporary relief occurs in the fetal position, which the patient unconsciously tries to assume. During an attack accompanied by severe pain, loss of consciousness is possible.
In severe cases, the symptoms of an attack are supplemented by the following signs:
- Nausea;
- Frequent vomiting, which begins with the release of undigested food and ends with bile;
- Bloating;
- Liquid, foul-smelling stool containing pieces of undigested food;
- Poor appetite;
- Increased body temperature;
- Stool disorders, manifested in alternating constipation and diarrhea;
- Belching;
- A white coating appears on the tongue;
- The elasticity of the skin decreases, it becomes gray in color;
- A sharp weight loss is recorded;
- Hiccups;
- Sometimes decreased blood pressure readings are recorded.
Such symptoms are reminiscent of food poisoning and gastrointestinal disorders. Therefore, an attack of pancreatitis can be diagnosed only after laboratory and hardware diagnostics.
Complications
Pancreatic necrosis is quite often accompanied not only by abscesses, but also by disruption of the functioning of neighboring organs and the development of various infections. Moreover, the latter are observed in every 3rd patient.
The likelihood of complications directly depends on the degree of neglect of pancreatic necrosis.
According to medical statistics, the first 3 weeks are the most dangerous for the development of complications of pancreatic necrosis. Moreover, over time, the risk of developing infection increases. Complications are observed:
- at 1 week - 25%;
- at week 2 - 40%;
- at 3 weeks - 60%.
At the end of this period, the risk of infection is sharply reduced, and by week 5 it is observed in only 3-5% of patients.
Pseudocysts
The formation of a false cyst is a common complication after pancreatic necrosis. Its main difference from the true one is that it can form without an epithelial lining. Only a doctor can diagnose the formation.
The most radical method of treating a false cyst in pancreatic necrosis is its complete removal.
Treatment of false cysts is complex and includes drug therapy, minimally invasive methods and surgical interventions.
External drainage is advisable if the pseudocyst is not connected by the pancreatic duct. Otherwise, internal drainage is performed, which is divided into several types: cystogastro-, cystoduodeno- or cystojejunostomy. The most radical method of treating a false cyst in pancreatic necrosis is its complete removal (extirpation). However, this operation is possible with a mobile small cyst that has well-formed walls.
Hemorrhages
Arrosive bleeding during pancreatic necrosis can be both internal and external. The former occur in the cyst cavity or directly in the gastrointestinal tract, the latter - in the postoperative wound. Most often, hemorrhages begin suddenly and are accompanied by tachycardia and a sharp decrease in blood pressure.
Most often, hemorrhages begin suddenly and are accompanied by tachycardia and a sharp decrease in blood pressure.
In most cases, bleeding recurs over time and can cause the patient's death.
Specifics of emergency care
It should be noted right away that in case of a pancreatic attack and inflammation of the pancreas at home, the use of medications is indicated only on the recommendations of a doctor. Only emergency physicians who respond to a call can administer certain medications to stop the symptoms of an attack.
After hospitalization, patients are examined using laboratory and hardware diagnostics. Only after a detailed examination and diagnosis is therapy prescribed. In this case, surgical intervention is often the basis of treatment.
However, before medical personnel arrive, the patient needs to be helped by reducing pain. First aid for an attack of pancreatitis at home includes the following actions:
- Place the patient in a position that is comfortable for him;
- Ensure free air circulation in the room;
- Relax or remove pressure from the patient;
- Give him a tablet of No-shpa or Drotaverine (if you have the opportunity and skills, it is better to administer the medicine intramuscularly).
Taking medications
The standard of medical care excludes the use of medications, since such actions can “blur” the clinical picture and harm the patient.
Medications are taken only as recommended by a doctor.
Medicines that help reduce inflammation of the gland and pain are nosh-pa or drotaverine. It is better to administer the drug intramuscularly, avoiding the digestive tract. But if this is not possible, take the tablet, first crush it in a spoon.
medications to help relieve pain in the pancreas
If pancreatic symptoms appear, you need to know about general actions in a hospital setting:
- taking antispasmodics is accompanied by the administration of an atropine solution;
- The outflow of bile often accompanies the symptoms of an “acute abdomen”, so it is advisable to take Allochol 2 tablets.
In a hospital setting, the pancreas is treated with the following medications:
- Antispasmodics.
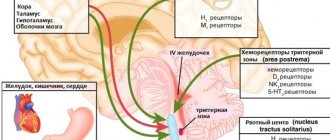
- H2 blockers, which inhibit pancreatic secretion.
- Enzymes.
- Antacids to reduce stomach acidity.
- Antibiotics to reduce inflammation and as a means of preventing the spread of infection.
The drugs are prescribed by a doctor after diagnosing the disease.
Differences in the chronic course of the pathology
Chronic inflammatory disease of the pancreas has the same symptoms as acute one. However, the symptoms are less intense.
The disease “manifests itself” after a violation of dietary nutrition, intensive and prolonged consumption of alcohol, and severe stress. At the same time, the patient should know that a suddenly stopped attack is evidence of extensive necrosis of pancreatic tissue. Therefore, medical consultation is necessary for such patients.
Providing emergency care during an attack of chronic pathology does not differ from the acute form. However, the patient already knows about his illness, he has been examined and has certain medical prescriptions. Therefore, the patient can take analgesics that are approved by the attending physician. Taking 2 tablets of Allochol is also indicated. The drug will help bile and pancreatic juice to “leave” the pancreas.
You can take Allochol only together with medications that relieve spasms! Use of the medicine during an attack is indicated only in chronic cases of the disease and strictly as prescribed by the doctor.
After hospitalization and an objective assessment of the patient’s condition, treatment tactics are determined individually.
Antispasmodics and analgesics
Painkillers “No-shpa”, “Papaverine”, “Baralgin” are welcome and considered necessary in the home medicine cabinet. The drugs are effective and safe. They eliminate spasm of smooth muscles and reduce pain. Sometimes they take analgesics: Paracetamol, Aspirin. In some cases, to prevent the development of allergic reactions, antihistamines are used: Atropine, Platifillin, Diphenhydramine.
H2 blockers
H2 blockers (Famotidine, Ranitidine, Cimetidine) are used to suppress pancreatic secretion. Sometimes hormones are prescribed that inhibit the acid-forming function of the stomach (Somatostatin, Glucagon). The use of such drugs is justified in pancreatic shock.
Enzyme preparations
To normalize digestion and better assimilate proteins, fats and carbohydrates, enzyme substances are used, including amylase, lipase, protease. Enzyme preparations are available without a doctor's prescription; popular products are: “Creon”, “Pancreatin”, “Festal”.
If a person is allergic to pork protein, herbal preparations are used: Somilase, Pepfiz. Enzymes are prescribed by your doctor and taken after meals. The duration of treatment depends on the form and degree of development of the inflammatory process, the age of the patient, and concomitant diseases.
Antacids
Antacids are used to neutralize and reduce the production of hydrochloric acid. The most commonly used are Almagel, Phosphalugel, Gastrozol, and Controloc. The medication is taken 1 hour after meals. It is not advisable to use it together with other medications.
Classification
AP classification is carried out taking into account the degree of progression of the inflammatory process, the presence or absence of complications. According to the form of the disease, it can be edematous type, sterile pancreatic necrosis and infected pancreatic necrosis. Sterile AP is further classified into limited and widespread type, and according to the nature of the lesion, the pathological process can be mixed, fatty and hemorrhagic.
Classification by severity:
- mild form (the disease is characterized by minimal damage to the pancreas and mild symptoms);
- severe form (extensive damage to the pancreas, severe symptoms, the presence of complications in the form of abscesses, necrotic areas).
Pancreatitis: emergency call card
Woman, 52 years old. The reason for the call was acute abdominal pain, a history of pancreatitis, and no appendectomy.
According to the patient, she has been sick for 1 day, but such attacks have happened before. Complaints of sudden onset of severe “girdling” pain of a spastic and increasing nature in the upper abdomen, radiating to the left clavicle and the posterior sections of the lower ribs on the left.
- In this article you will find only a few ready-made samples and templates. In the Consilium System they more than 5000
.
Main clinical symptoms
- Pain syndrome (intense constant pain localized in the right hypochondrium and epigastric region, possibly radiating to the right supraclavicular region, shoulder and scapula, sometimes to the sternum);
- Nausea, vomiting;
- Hyperthermia, chills;
- Palpation: local defence;
- Positive symptoms of Ortner, Georgievsky-Mussi (phrenicus symptom), Kera, Murphy, etc.
- of acute cholangitis is possible (pain in the right hypochondrium + itching, yellowness of the skin, discoloration of feces + hectic fever).