Causes of anal fissures
Reasons why anal fissure may occur:
- Constipation. During chronic constipation, hard stool constantly forms, which leads to microcracks and damage to the tissues of the anus. In addition, straining performed by a person increases pressure in the rectal area - this can lead to tissue rupture and the appearance of a crack.
- Inflammatory processes in proctitis. With inflammation, the strength of the tissues of the anus decreases, which leads to their damage by feces.
- Poor nutrition, poor chewing of food. Undigested sharp pieces of food (nuts, seeds) can damage tissue during bowel movements.
- Childbirth. A rupture of the mucous membrane may occur with strong straining, as well as when applying forceps or using a vacuum.
- Strong physical activity.
- Intestinal examinations.
- Rapid, incorrect administration of an enema.
- Anal sex.
- Prolonged sitting.
- Wrong diet: spicy food, alcohol.
Causes
Cracks can be located both on the back (80% of cases) and on the front wall of the canal mucosa (about 10-12%). When defecating, they remain practically motionless, while the rest move down and then return back. If you imagine the mucous membrane of the anal passage on a conventional dial, then at 6 and 12 o’clock the motionless walls are precisely the areas with insufficient blood circulation and the risk of injury during defecation.
Proctologists consider the inflammatory process in the pockets of the Morganian crypts to be one of the factors in the formation of injury. It develops when excrement accumulates in them. Due to inflammation, the mucous membrane first loses its elasticity, and then becomes injured and ruptured. Thus, the main causes of mucosal tear are:
- Damage to the canal by “heavy” coarse stools, which is caused by excessive consumption of coarse fiber and insufficient amount of fluid.
- Severe straining during defecation.
- Rupture of the meatus during childbirth. It is observed in primiparous women; it is provoked by excess tension in the anal area.
- Concomitant diseases: irritable bowel syndrome, ulcerative colitis, proctitis, Crohn's disease, pancreatitis.
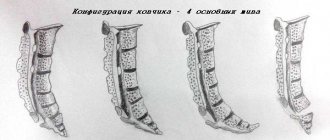
- Damage to the mucosa associated with the anatomical features of the structure of the intestinal canal (sacrococcygeal curvature).
- Damage to the canal by proctological instruments during diagnostic procedures, anal sex, injury from foreign objects contained in feces.
- Impaired blood flow and blood stagnation caused by thrombophlebitis, aneurysm, hemorrhoids, atherosclerosis.
- Pressure surges in the rectum. They can be caused by heavy lifting.
- Neurocirculatory disorders. Promote the development of sphincter spasm.
The study of the mechanisms of problem occurrence continues today. Thus, thanks to research, doctors were able to relieve sphincter spasm with nitro drugs, which significantly improved the effectiveness of treatment.
Symptoms of this disease
There are three main signs that make it easy to diagnose an internal anal fissure. Typically, patients experience the following symptoms:
- Acute pain during bowel movements, which patients describe as a “burning” sensation, a feeling of “broken glass”. Such pain occurs in the anus, radiating to the anus, groin, and lower abdomen. The syndrome may last for some time after defecation.
- Light bleeding during bowel movements. May appear as a streak of blood on the surface of the stool. In some patients, the fissure bleeds between bowel movements.
- Spasm of the anal sphincter, which may be accompanied by severe pain.
Some patients may experience characteristic symptoms only for a short time, which will lead to misconceptions about the healing of the fissure, but this happens extremely rarely. Without compliance with certain treatment measures, it is difficult to achieve the desired result, and the possibility of relapse is extremely high.
Diet for rectal fissure
For rectal wounds, great importance must be given to proper nutrition. This is especially true for people whose pathology is caused by constipation. To cure an anal fissure, it is necessary, first of all, to establish a drinking regime. For the normal functioning of the human body, it is necessary to drink up to 3 liters of fluid per day.
Positive results for constipation are obtained from a diet that includes fermented milk products. The substances contained in this food allow you to dilute stool and increase the number of trips to the toilet. In addition, permitted nutrients include prunes and vegetables that contain large amounts of easily digestible fiber.
It is important to regularly consume protein products - meat broths, dairy dishes. They are essential for maintaining immunity and energy. In addition, protein has a good effect on the functioning of the muscular system. At the same time, proctologists recommend giving up rye and wheat bread, marinades and smoked foods, so as not to overload the intestines with unnecessary substances.
It is important to limit your consumption of fatty, spicy foods to a minimum - they can cause irritation in the gastrointestinal tract. Some proctologists for fissures advise drinking a few teaspoons of olive or vegetable oil in the morning to induce bowel movements and empty the intestines without problems.
Features of treatment of acute anal fissure
Features of the treatment of this disease depend on its form, which can be acute or chronic. An acute anal fissure is a defect that is present during the first month. Such a crack looks like a small tear without clear boundaries, from where red muscle tissue is visible. If the gap does not heal within 6 weeks, and the edges acquire clear boundaries, the anal fissure becomes chronic.
It is important that the patient consult a doctor during the acute period - in this case, the likelihood of non-surgical cure is high. As a rule, doctors treat using conservative medicine methods: thermal procedures, pain relief, prescribing ointments, creams, suppositories, enemas, baths, medications, cauterization. As a last resort, they resort to using novocaine blockades and stretching the sphincter.
Laser surgery is also an effective method (laser is effective only during the acute period). If conservative treatment methods do not lead to a noticeable result, and the anal fissure becomes chronic, surgical intervention is required.
- Blood from the anus - causes of symptoms, diagnosis of diseases and how to stop bleeding
- Hemorrhoids 1st degree - symptoms and signs of the disease, diagnosis and treatment
- How to get rid of itching from hemorrhoids: causes and treatment of the disease
Diagnosis of the disease
Acute and chronic anal fissure are diagnosed using the same medical tests, which can only be performed by a proctologist.
External inspection
In most cases, an anal fissure is noticeable upon a quick external examination. Outwardly, it resembles a longitudinal line or a small triangle of a bright red hue.
Finger examination
This examination involves palpating the walls of the rectum with a finger inserted into it. This allows you to assess the strength of the sphincter spasm.
Sigmoidoscopy
The most accurate and most popular method of examining the rectum. It is carried out using a sigmoidoscope, a device that allows you to study the mucous membrane at a depth of 30 cm from the anus.
Anoscopy
Involves a thorough examination of the final section of the intestine.
Treatment of chronic fissure
A chronic anal fissure is characterized by the appearance of clear boundaries and the presence of “bumps” along the edges. At this stage, they resort to surgical intervention, which is carried out in the following ways:
- excision of a crack;
- excision with suturing of the wound;
- excision with dissection of the sphincter;
- combined options.
During excision, granulation is removed, “tubercles” are cut off, which leads to the transition of the chronic form back to acute. After this, conservative medicine methods are used to treat the defect, and a strict salt-free diet is prescribed. With proper adherence to preventive and therapeutic measures, complete recovery occurs in 2-4 weeks.
The radiosurgical device “Surgitron” became a new word in excision of cracks. Its difference from the classical surgical method is that the device acts precisely and does not affect healthy tissue, eliminating only damaged ones. The time to heal is reduced, the postoperative period is easier and without complications.
How does cauterization of an anal fissure occur?
Cauterization of an anal fissure is called electrocoagulation, and is performed with an infrared laser. Laser coagulation of cracks is modern and widely used, but it is quite painful and is not indicated in all cases. It is not suitable in the fight against chronic fissures, and is effective only for fresh ruptures of the rectum (for a period of 3, maximum 4 weeks).
It is much more painless and effective to undergo radiofrequency treatment , which, like laser treatment, is called cauterization.
The essence of cauterization is laser or radio wave excision of scar perianal tissue along with a crack. Occurs under local anesthesia.
Ways to treat anal fissure at home
Before doing home treatment, you should definitely consult a doctor to avoid the consequences of incorrect procedures. The main assistants in treatment will be: diet, warm baths, enemas, external ointments and medications injected into the rectal canal, medications.
Diet and nutrition
Nutrition will be the basis of treatment for anal fissure if it is caused by constipation. The doctor’s task is to prescribe a diet for the patient that will help eliminate this problem. You should exclude from your diet:
- spicy dishes;
- salty dishes;
- alcohol;
- refined products;
- fried foods.
To “soften” stool, it is necessary to enrich the diet with plant foods. This will allow the act of defecation to take place painlessly and will contribute to the rapid healing of the crack. The patient should eat more cereals, fresh vegetables and fruits, dried apricots, prunes, figs, and drink plenty of fluids. Boiled beets with sour cream and butter help soften stool.
- Quick treatment of hemorrhoids at home: effective remedies and methods
- How to recognize hemorrhoids at home by signs and symptoms
- How to relieve inflammation of hemorrhoids quickly
Enemas
During treatment, you can use two types of enemas - water and oil. They are used when the patient feels the urge to defecate. Enemas are designed to make defecation easier.
- Water enema. To carry out the procedure, you need to fill the “Esmarch mug” halfway with boiled water, to which a small amount of salt has been added, and raise it as high as possible - this will provide pressure from which the liquid will flow freely into the anus. The addition of anti-inflammatory and disinfectants will enhance the medicinal effect.
- Oil enema. For this procedure, you need to mix 50 ml of oil with 150 ml of water, then cleanse the intestines.
Ointments, suppositories and special creams
After defecation, it is recommended to rinse the anus and the skin around it with cold water - this will reduce pain and make it possible to use special topical products efficiently.
For local anesthesia, healing, relieving itching, inflammation, eliminating irritation, and providing an antiseptic effect, various ointments are used: Vishnevsky ointment, D-panthenol, Bepanten, Levomekol. To soften the skin near the anus, the patient can use baby cream or Vaseline. Creams that have a healing, bactericidal, anti-inflammatory effect will also help.
Anal suppositories will be a good helper in the fight against anal fissure. Suitable options are Relief Ultra, Relief Advance, Proctosan, Natalsid, sea buckthorn suppositories. When purchasing this drug, you should definitely consult your doctor. Separately, it is worth saying that many suppositories are contraindicated for pregnant women and women breastfeeding - for them, the ideal option would be to purchase homeopathy preparations, for example, Natalsid.
Medications
When treating a crack with medications, tablets of different effects are used:
- Vitamins – A, E, promoting tissue regeneration;
- Anti-inflammatory drugs (Salofalk);
- Laxatives to normalize stool (Senade, Normaze).
Treatment methods at home
Treatment for anal fissure depends on the duration of its existence. Fresh injuries quickly heal through conservative therapy: the use of stool normalizers, suppositories and ointments that relieve pain, spasm, inflammation, etc.
If more than 3 weeks have passed since its formation, its edges have become dense, then in most cases it is no longer possible to do without surgical intervention. It is no longer possible to cope with such a problem at home.
Rectal suppositories
Suppositories, the main purpose of which is to eliminate discomfort (itching, pain) and accelerate the healing of the mucous membrane, tend to be quickly absorbed and have a therapeutic effect. Allergic reactions with their use are rare.
- Suppositories with sea buckthorn oil. Herbal suppositories that increase local immunity and accelerate regeneration processes. They have a slight antimicrobial effect. Allowed for children and pregnant women. The course of treatment is 7 days, 1 suppository per day.
- Gepatrombin G. Suppositories and ointment, which have an analgesic and antiallergic effect, relieve itching, burning, and swelling.
- Proctosan. A four-component drug that has an astringent, anti-inflammatory, analgesic and wound-healing effect. The course of treatment is up to 7 days. Suppositories are administered twice a day, one at a time. Contraindicated during pregnancy.
- Relief Advance. It has fast pain relief and powerful regenerating effects due to the content of benzocaine and shark liver oil. Relief suppositories and ointment can be used during the rehabilitation period (from 3 to 5 times per day), during pregnancy and immediately before defecation to facilitate the passage of feces. Adverse reactions are rare.
- Natalsid. The suppositories contain sodium alginate, a polysaccharide from algae. They speed up the healing process and have an anti-inflammatory effect. Suppositories are placed twice a day for 1 to 2 weeks.
- Anestezol. Contains zinc and benzocaine. These components relieve pain, dry the wound, and accelerate the regeneration of the mucous membrane. Contraindications: hypersensitivity to the components of suppositories.
- Ultraproct. A combined drug whose components promote rapid wound healing (fluocortolone hormone) and relieve pain (cinchocaine). The course of treatment is no more than 1 month. Contraindicated in the first trimester of pregnancy.
Any suppositories from this list are administered as follows: empty the intestines, while lying on your side (the leg should be bent at the knee), insert a suppository and squeeze the buttocks; You need to lie down for at least 5 minutes.
Ointments
If a person is experiencing severe pain, then the use of suppositories is not possible. Then the proctologist prescribes ointment (or cream) medications. They have a greasy consistency, are easy to apply, relieve pain and inflammation, and also promote the healing of damaged anal tissue.
- Posterisan forte. Contains a suspension of the cell membrane of a strain of Escherichia coli, which activates local immunity, triggers the formation of immunoglobulin A, which forms a thin protective film on the mucous membrane, as well as hydrocortisone, which relieves inflammation. The ointment is administered with a special applicator twice a day (or after each stool) for a maximum of 3 weeks.
- Solcoseryl. A remedy for restoring damaged anal walls. Apply only after the crack has dried. Doesn't relieve pain. Apply a thin layer 2 r. in a day. Aurobin. Ointment with anti-inflammatory and antibacterial effect. Contains prednisolone and
- D-panthenol. Relieves itching and swelling, relieves pain, stimulates tissue regeneration. It may suppress adrenal function, so it is not prescribed in childhood or pregnancy.
- Nitroglycerin ointment. Helps relax the sphincter, which has a beneficial effect on the healing process of the wound. It treats the anorectal area and rectum (using a cotton swab). The course of treatment is up to a month, 3-4 times a day.
- Levomikol. Antibacterial ointment that accelerates skin healing. It is prescribed if the wound is affected by bacteria and becomes inflamed. The ointment is applied for 7-10 days in the morning and evening.
- Ichthyol ointment. Relieves pain and inflammation.
- Warrior. Fights inflammation, accelerates regeneration processes, kills microbes living on the mucous membrane. It is allowed to apply after each bowel movement.
The rules for applying the ointment are as follows: wash the anus with warm water and soap, after drying, apply a thin layer of ointment to the affected area 2-3 times a day (unless otherwise indicated in the instructions).
Folk remedies
Despite the huge number of medications for anal fissure, the desire to try to be cured with folk remedies remains. We list easy-to-make and safe recipes from traditional healers.
- Herbal candles. Dry plantain, chamomile and motherwort taken in equal parts are added to the melted beeswax. 10 suppositories are formed, and after hardening, they are used to relieve swelling and itching.
- Propolis suppositories with the addition of badger fat. Prepare a mixture of 70% alcohol, fat and propolis, taken 40 grams each, leave for 3 days, after which a stick cut from a potato is dipped into it and inserted into the anus. The procedure is repeated until complete recovery every evening.
- Ice candles. Dry raw materials of chamomile, oak bark and calendula (in equal parts) are boiled in a liter of water for 5 minutes. After cooling, the broth is poured into molds (you can use the fingers of medical gloves) and frozen.
- Compress of bile and vegetables. Grated carrots and beets are combined with bile (pork or bovine), taken in a ratio of 3:1. The composition is spread on the tissue and applied to the mucosal tear, held for 15-20 minutes.
- Infusion for sitz baths. Mix 20 grams taken each. calendula, sage, chamomile and St. John's wort. Pour 1.5 liters. boiling water, filter and dilute to an acceptable temperature with warm water. Take a sitz bath for 15-20 minutes.
- Decoctions for microenemas. Brew 1 tbsp in a glass of boiling water. l. chamomile (or yarrow, St. John's wort). When warm, it is introduced into the anus with a microenema of 30-50 ml. After administration, it is recommended to lie on your left side. Duration of use – 1 rub. a day for three weeks in a row.
- Spruce resin ointment. Take 4 tbsp. ate resin, boil it, strain and add 2 tbsp. sheep fat and boil again. Wax is injected. Use chilled 2 r. in a day.
Keep in mind: a chronic fissure cannot be cured using folk remedies. The above means can only speed up the healing process of the operated wound.
Dietary nutrition for illness
Dietary nutrition is aimed at facilitating the process of defecation and reducing pain. It involves minimal heat treatment of vegetables and the inclusion of probiotics and natural yoghurts in the diet. For symptoms of anal fissure and other proctological diseases, it is recommended:
- Include in the diet: whole grain porridge, dried fruits, soups with vegetable broths, vegetable salads (including boiled or baked beets), rosehip decoction.
- Exclude from the diet: seasonings, alcohol (including beer), spicy, salty, fatty protein foods (meat, high-fat dairy products, rich broths, eggs), citrus juices, fresh wheat bread, foods rich in starch.
- Maintain drinking regime. To soften stool, you need to drink 2.5-3 liters per day. water.
- Include bran in your diet, take enzyme preparations Mezim, Gestal, Panzinorm, which facilitate digestion.
- Stick to fractional meals (5-7 times a day).
- To stimulate intestinal contractions, add vegetable oil to salads. Sometimes you can drink Vaseline oil.
It is worth adhering to a diet in the period after refusing cleansing enemas, as well as after surgery to prevent trauma to the wound surface. During the period of remission, it is allowed to diversify the diet with “harmful” foods in minimal quantities.
How to cure anal fissure with folk remedies
Several ways to treat anal fissure with folk remedies:
- Microenema with calendula and sea buckthorn oil. Pour 0.1 liter of boiling water over dry calendula and leave for several hours. Add 2 teaspoons of oil. Use the resulting solution as an enema before bedtime.
- Sitz bath with herbs (sage, chamomile, calendula, St. John's wort). Take 20 g of each herb, pour boiling water over it, strain. Dilute with water to a temperature of 38 degrees. Take a bath for 20 minutes.
- Aloe. Before going to bed, you need to squeeze out fresh aloe juice, put it in a pipette, and carefully insert it inside. Repeat twice.
What to do if an anal fissure is complicated by a sentinel polyp?
The so-called “sentinel polyp” is a lump formed by rough scar tissue. Polyps with anal fissures indicate a chronic process. The fact that an acute crack, in the absence of treatment, turned into a chronic one. And it will now be more difficult and longer to treat than an acute one.
Treatment of anal fissure and sentinel polyp is most effective by surgical method. And here it is best to resort to a minimally invasive technique of radiofrequency excision of the scar defect.
Reviews
Marina, 28 years old: “A year ago I began to feel severe pain when going to the toilet, and constipation began. It felt like there were shards of glass there. After several weeks of incessant pain, I went to the doctor - he prescribed Relief Advance suppositories, enemas and mild laxatives, and prescribed a diet. Unfortunately, the disease became chronic and had to be excised, but after two weeks I was healthy!”
Natasha, 34 years old: “The most important thing is not to miss the moment! As soon as I diagnosed my fissure, I decided to improve my nutrition. I took laxative pills, applied Bepanten - everything went away.”
Nikolai, 32 years old: “I had an anal fissure, the following set of procedures helped: normalization of stool, Bezornil ointment four times a day and careful hygiene. A month later I was as good as new.”
Inna, 25 years old: “During pregnancy, an anal fissure formed. It was terribly painful, and I became afraid of the toilet. The proctologist prescribed ointments and suppositories, but due to constipation everything continued. Flaxseed oil helped - three times a day half an hour before meals. There were no more problems with the chair!”
Signs of an acute crack
An acute fissure of the rectum has several pronounced symptoms:
- Pain in the anus is severe, but short-lived, and occurs with mechanical irritation, during defecation and within 15 minutes after it. It can be stabbing, pulling, burning, pressing or pinching in nature. The intensity of the sensations directly depends on the depth of the cleft - the deeper, the more painful. Later, as the inflammatory process progresses, the pain can become permanent and appear throughout the day;
- Itching and severe discomfort are caused by synthetic, uncomfortable or too tight underwear. The longer the crack, the larger the itchy area and the greater the discomfort;
- Spasms of the anus (sphincter) - accompanied by severe pain and difficulty during bowel movements;
- Minor discharge of scarlet or dark blood - appears during a trip to the toilet, when dense feces pass through the rectum.
Diagnosis of hemorrhoidal fissures
In the normal state of the sphincter, it is extremely difficult to detect a rectal fissure. The patient is asked to strain slightly, as if having a bowel movement. At this point, the rectal opening begins to descend, exposing the inner lining that covers the anal ring.
In this case, the specialist sees with the naked eye a defect in the mucous membrane of the rectal canal, which extends to the skin of the perianal area. The crack is always located longitudinally, hiding between the leathery folds of the anus.
In acute pathological processes, rectal examination is difficult due to strong spastic reactions and pain. For anesthesia, locally acting ointments are used. Study of the deep parts of the rectum (anoscopy, rectoscopy, colonoscopy) can be prescribed only after acute symptoms have been relieved.
In differential diagnosis, anal fissures are distinguished from perirectal fistulas, syphilitic chancre, ulceration of the rectum, and skin lesions of tuberculous or mycotic origin.
Drugs that stop bleeding
The first-line drugs for the treatment of such complications with anal fissure are hemostatic agents. For this purpose, use:
- candles. For hemorrhoids with cracks and bleeding, suppositories with propolis, adrenaline, methyluracil and homeopathic (with sea buckthorn oil, calendula, Relief-ultra) are used;
- ointments. To stop bleeding, use heparin ointment, Vishnevsky ointment, Fleming ointment, Proctosan, Troxevasin, Relief, Hepatrombin and others;
- creams. Hemorrhoid creams such as Boro-derm, Tianhe, Proctoglivenol, Fitol-5 and others have a hemostatic effect;
- gels. Mastokrel and others.
Treatment of fissures in children
The appearance of anal fissures in children is a big problem, since an immature organism can cause a worsening of the condition. The disease often takes a chronic course. Therefore, if you suspect that a child has symptoms of an anal fissure, you should immediately show him to a proctologist. The doctor decides how to treat pathologies in childhood, individually in each case.
Therapeutic measures in children differ from generally accepted norms, since the use of potent drugs is prohibited. It is important to direct all actions to combat the symptoms of the pathology, as well as alleviate the child’s condition, because children suffer any illness more severely.
Children suffering from constipation should drink plenty of water. In addition, to resolve the problem of defecation in childhood, lactulose-based laxatives are indicated. Such methods make it easier to defecate and reduce pain after the act. It is important to prevent and prevent worms in children.
Children can use glycerin and sea buckthorn-based candles as suppositories. It is necessary to insert suppositories rectally once or twice a day.
Baths with anti-inflammatory herbs - chamomile, string, calendula - also have a good effect in symptomatic therapy. They contain antibacterial effects.
It is important to start treatment as early as possible in order to get rid of the crack before it reaches a severe stage.
Clinical picture of the disease
Like varicose hemorrhoids, fissures are a proctological pathology. This condition is characterized by linear or ellipse-like damage to the mucosal surface in the rectum or anal area. The maximum dimensions of the crack are: 3 cm in length, 3 mm in width, the depth depends on the degree of damage, but can also reach the sphincteral muscles. The defect is localized on the posterior wall of the rectum. Ruptures on the anterior wall or on the lateral surface are less common, since the contents of the intestine injure the posterior wall to a greater extent.
The main feature of an anal fissure will be acute pain in the anus at the time of defecation. It can continue after the act (for several hours or days). This pathology is characterized by sphincter spasm and mild rectal bleeding, which can be detected as drops of blood on toilet paper. It is clear that severe pain that accompanies going to the toilet due to great need forces the patient to empty his bowels as rarely as possible. Delaying bowel movements for several days only makes the situation worse.
Sometimes this happens after conservative treatment. During this period, the edges of the crack become coarser, thicken, grow with fibrous tissue, and scars appear. At its base, polypoid thickenings of tissue form (they are called the sentinel tubercle). Such a crack is much more difficult to cure.
Why doesn't the crack heal on its own? A vicious circle arises: a small defect in the mucous membrane causes a strong spasm of the anal sphincter, it maintains the problem and does not give it the opportunity to heal.
An anal fissure is almost always accompanied by anal sphincter tension - sphincterospasm. The sphincter seems to be afraid of pain, preventing the movement of feces through the anal canal.
Overcoming the resistance of the sphincter, feces moves through the narrowed tunnel, causing additional damage. In addition, in response to pain, the sphincter contracts, pressing feces into the fissure, widening it and aggravating the problem. Sphincter spasms are a reflex process, independent of a person’s will, therefore this condition is a significant obstacle to the healing of the fissure.
Another negative consequence of sphincterospasm is a disruption in the nutrition of the fissure. Increased sphincter tone compresses the arteries, reducing its blood supply. This naturally impairs the healing process. A vicious circle develops: pain increases sphincterospasm, which in turn aggravates the damage and interferes with healing, again provoking pain.
General principles of treatment
Acute pathology usually responds well to conservative therapy. It is much more difficult to cure a chronic anal fissure; the result of treatment will depend on the duration of the pathological process, the patient’s complaints, the severity of the clinical picture and the degree of morphological changes in the anal canal. If there is significant growth of scar tissue in the rectum, a surgical solution to the problem is possible using cryodestruction, sphincterotomy or another method. But the priority is the conservative direction in the treatment of anal fissures in accordance with the following principles:
- organization of proper nutrition - alcohol and spicy foods are completely excluded, cereals, plant fiber, fermented milk products are introduced into the diet, fluid intake is increased;
- improving bowel function - taking laxatives (Duphalac, Normaze), counter-oil microenema (introduce 50 ml of vegetable oil and 100 ml of water into the rectum and hold for a couple of minutes before bowel movement) to soften the first hard portion of stool;
- daily hygienic care of the perineum - wash with cool water after each bowel movement;
- changing the usual routine of life - increasing physical activity (hiking, exercise, swimming, jogging, dancing), normalizing night sleep, proper alternation of mental and physical activities.
In some cases, these measures are sufficient to heal an anal fissure in the acute phase. Otherwise, drug treatment is prescribed.
Diagnostic measures
Diagnosis is based on medical history, examination and instrumental examination. As a rule, this is enough to establish the correct diagnosis.
The examination is sometimes carried out on a chair, the patient is in a supine position with his legs apart. For better visualization, he is asked to push, since the crack is covered by folds of skin in the perianal area. Some doctors prefer to examine the patient in the knee-elbow position.
If the pain syndrome is severe, any tension in the abdominal wall muscles will lead to increased pain.
Sometimes the patient accurately indicates the time the anal fissure appeared and what contributed to it. The choice of treatment tactics will depend on these aspects.
It is not always possible to easily insert a finger into the rectum; to reduce pain, local anesthesia with anesthetic solutions can be performed.
Differential diagnostics and instrumental examination methods
Differential diagnosis is carried out with diseases that have similar symptoms, such as:
• hemorrhoids, • paraproctitis, • malignant neoplasm of the rectum, • ulcerative-erosive lesions of the intestine.
Signs that will help in making a diagnosis:
• there is no connection between bowel movement and pain, • upon examination there is no evidence of anal fissure, • atypical localization of pain, • the sphincter is in a relaxed state.
Instrumental diagnostic methods include sigmoidoscopy, colonoscopy and anoscopy
.
During the examination, it is possible to assess the condition of the tissues of the rectum, confirm or refute the presence of tumor formations, determine the boundaries and depth of the crack and decide on the tactics of patient management.
Conservative treatment of hemorrhoids and fissures
For acute fissures, conservative therapy is indicated. Most often, specialists prescribe topical medications, that is, ointment and gel products, as well as rectal suppositories. It is possible to take tablets - laxatives, antispasmodics and venotonics (for the treatment of hemorrhoids).
Rectal suppositories
Suppositories are an easy-to-use pharmaceutical form that allows active ingredients to quickly penetrate damaged tissues. Additionally, many candles contain cocoa butter and other fatty components, which simultaneously moisturize the skin and have a laxative effect.
It is better to treat hemorrhoidal fissures with complex-action drugs that contain anesthetic, anti-inflammatory and antispasmodic components. Suppositories are used twice a day - after waking up and before bedtime.
Table. Suppositories used to treat anal fissures.
| Drug name | Therapeutic actions | Contraindications | Price |
| Posterisan | Stimulation of local immunity, relieving inflammation and itching, accelerating healing and regeneration of damaged areas. | Allergy to the components of the drug. | From 380 rubles. |
| Proctosan | Relieving inflammation, pain, promoting rapid healing of cracks, drying the skin, astringent effect. | Infection of the anus, allergy to components, age under 18 years. | From 340 rubles. |
| Ultraproct | Quick relief of inflammation, pain, acceleration of healing and regeneration processes. | Infections in the anal area, intolerance to ingredients, first trimester of pregnancy. | From 620 rubles. |
| Natalsid | Healing of cracks, relieving inflammation, stopping bleeding. | Allergy to the ingredients included in the composition. | From 330 rubles. |
| Methyluracil | Stimulation of regeneration processes in the area of damage to the mucous membrane and skin, increasing local immunity. | Malignant tumors, allergies to the components of the drug. | From 80 rubles. |
| Salofalk | Rapid elimination of inflammatory processes in the intestines. | Liver and kidney failure, allergies to the drug, gastrointestinal ulcers. | From 1000 rubles. |
| Sea buckthorn oil | Stimulation of wound healing processes, increasing local immunity, protecting cells from damage. | Allergy to components, loose stools. | From 80 rubles. |
| Relief | Stopping bleeding, stimulating the immune system, accelerating wound healing and regeneration processes. | Thromboembolism, allergy to ingredients, granulocytopenia. | From 340 rubles. |
Ointments for hemorrhoidal fissures
The best ointments for rectal fissures contain a fatty base that softens the skin, helps relieve inflammation and stimulate regeneration processes. The drugs are administered once or twice a day after defecation and hygiene measures. The ointments presented below are effective in the fight against both cracks and hemorrhoids.
Table. Ointments used to treat rectal fissures.
| Drug name | Therapeutic actions | Contraindications | Price |
| Ultraproct | Quick relief from itching, inflammation, pain, promoting wound healing and tissue regeneration. | Infectious processes in the anus, allergies to components, first trimester of pregnancy. | From 600 rubles. |
| Proctosan | Relieving inflammation, pain, accelerating wound healing, drying the skin. | Anal infection, allergy to ingredients. | From 350 rubles. |
| Methyluracil | Stimulating epithelization in damaged areas, accelerating tissue regeneration, increasing immunity. | Malignant tumors, allergic reactions to the components of the drug. | From 80 rubles. |
| Solcoseryl | Improving metabolic processes, strengthening local protective reactions, accelerating tissue regeneration, strengthening blood vessels. | Allergic reactions to the components of the drug. | From 300 rubles. |
| Levomekol | Relieving inflammation, swelling, destroying pathogenic microorganisms, regenerating damaged tissues. | Ingredient intolerance. | From 100 rubles. |
| Bepanten | Stimulation of regeneration processes in affected tissues, healing of mucous membranes and horse integument, normalization of cellular metabolism. | Intolerance to the components of the drug. | From 400 rubles. |
| Nitroglycerin ointment | Vasodilation and relaxation of the sphincter, improving blood circulation and eliminating spastic reactions in the anal area. | High blood pressure, serious heart disease. | Prepared in pharmacies according to prescription. |
| Aurobin | Relieving inflammation, pain, accelerating wound healing and regeneration processes in damaged areas. | Skin infections in the area of application, allergies to components, first trimester of pregnancy. | from 280 rubles |
The first symptoms of hemorrhoids
You may suspect that you have hemorrhoids based on the following symptoms:
- Blood during bowel movements: This may remain on toilet paper and turn the toilet water red. The bleeding is usually small, but it can be scary.
- Itching and/or pain in the anus (anus).
- There is a bluish bulge near the anus. When pressing on it, pain is felt.
- Leakage of stool or mucus.
If you have such symptoms, you can try to cope with them yourself within a week. To do this, you need to eliminate constipation and have a sufficient amount of fiber in your diet, that is, 20–36 g, and water. A lot of fiber is found in plums, peas, lentils and other beans, peanuts, almonds, etc. There are also special preparations that are sold in pharmacies. But too much fiber is also not good, as it can lead to flatulence (accumulation of gases in the digestive tract). Fiber is needed so that the stool is soft and a) does not injure hemorrhoidal tissue, b) there is no need to push.
If symptoms have not gone away after 7 days, you should consult a doctor. A visit to the doctor should not be put off, especially if you are over 50 years old. The fact is that bleeding is rare, but still a manifestation of colorectal cancer (colon and rectal cancer) or anal cancer. More often, these cancers develop in older people.
We invite you to make an appointment with a coloproctologist at a special price - 500 rubles. The promotion is valid on Friday and Saturday. The appointment is conducted by surgeon, coloproctologist Timur Mavludinovich Magomedkhanov, call: +7 (495) 125-30-32.
When with such symptoms it is impossible to wait even this week? If there are other signs of bleeding in the gastrointestinal tract:
- you notice that some inexplicable changes have occurred during bowel movements;
- the stool is black or maroon, contains blood clots, or the stool is mixed with blood;
- you feel dizzy or faint.
Conservative therapy
If a small amount of blood is released from the anus, then surgical intervention can be avoided. In this case, the person is prescribed certain medications.
This is interesting: Jacob from Twilight actor
First, anticoagulants are prescribed, the active component of which is heparin. This substance helps relieve inflammation, accelerate the restoration of damaged tissue, and improve blood circulation. For rectal fissures, Heparin ointment is usually used.
To eliminate linear ruptures of the rectum, the following are used:
- Combined action candles. A doctor may prescribe suppositories to a person, which contain substances that have a drying effect. What are the best candles to use? The most effective drugs are Natalsid, Gepatrombin G, Ginkor Procto.
- Combined action ointments. Drugs such as Aurobin, Proctosan Neo, Relief can be used. Bioadditives are also widely used. For example, Proctolex cream ointment has a pronounced hemostatic and immunostimulating effect.
- Traditional medicine. They are used along with medications. Castor and sea buckthorn oils have a drying effect. If you have bloody discharge from the anus and severe pain, you can use an ice compress.
But when treating cracks, using only ointments, suppositories and traditional medicine is not enough. In order to reduce the likelihood of increasing the depth of the defect, it is necessary to normalize intestinal motility.
What drugs should I use for this? If a person has constipation, then laxatives with osmotic or irritant effects are prescribed. Cleansing enemas or glycerin suppositories can also be used.
If diarrhea is present, medications that slow intestinal motility, such as Loperamide Hydrochloride, are most often prescribed. But probiotics and enterosorbents are also very effective against diarrhea.
If bleeding is accompanied by severe pain, then tableted antispasmodic or painkillers are used. In severe cases, a technique such as anal fissure blockade is used. It involves the use of Novocaine or Lidocaine.
Using medications is not enough. When treating rectal fissures it is also necessary:
- Change your diet. It should contain foods that are rich in dietary fiber and protein. The menu should be dominated by vegetable soups, fresh vegetables, cereals and fruits. You should refrain from fatty, hot, spicy and sweet foods. Alcohol is strictly prohibited.
- Follow the rules of intimate hygiene. If there are cracks, you need to take sitz baths and wash the anorectal area after each bowel movement. But using toilet paper is highly discouraged.
- Refrain from anal sex.
You also need to lead an active lifestyle. Daily walking and swimming will be helpful. In the postoperative period, the patient may be prescribed physical therapy (at the discretion of the attending physician).
Questions about anal fissure: does not heal, does not hurt, bleeds, fissure with papilloma.
Question: Why does an anal fissure not heal, and how to treat it?
When an anal fissure heals poorly, it inevitably leads to only one thing: chronicity of the process. And at this stage, treatment is much more difficult.
A crack may not heal for only two reasons:
- in case of inadequately selected treatment;
- if irritating factors continue to be present in the patient’s daily life (hard and dry feces, constipation, diarrhea, poor quality nutrition).
We often hear from people that their fissure does not heal after hemorrhoid removal. Nowadays, combined surgical practice has been successfully used for a long time, when both the fissure and hemorrhoids are removed simultaneously, during one operation . If this does not happen, you will have to excise the anal fissure additionally. But you need to get rid of it, and this is only surgical treatment.
Fortunately, now the non-healing fissure of the anus is quickly, painlessly and efficiently removed using the Surgitron radioknife. This technique is preferred by medical coloproctologists.
Question: What should I do if my anal fissure bleeds?
If there is chronic bleeding from a posterior fissure, and the volume of blood released is quite large, it is worth thinking about the likelihood of a combined proctological problem. This is often observed with a combination of anal fissure and hemorrhoids. After all, the fissure usually bleeds slightly. There can be a lot of blood only with hemorrhoids. This combination occurs in 70% of cases. Very often, a crack occurs against the background of existing hemorrhoids. Anal fissure and blood - in addition to spasm, pain and itching, this is the most unpleasant thing that complicates hemorrhoids.
In modern coloproctology, there is a tendency to simultaneously surgically solve these two problems. When an anal fissure and prolapsed hemorrhoids are removed in one operation. This tactic allows you to reduce the burden on the patient’s body and not split his treatment into two surgical interventions. Only a doctor must have experience in performing such combined operations.
Question: I got condylomas from a fissure in the anus. What to do?
Papillomatosis and condylomatosis are viral diseases. In half of the cases, the virus is transmitted sexually. But it is always activated in the body only in the case of a strong decrease in immune status. Of course, if the anal fissure is not dealt with in any way, it becomes fertile ground for the development and proliferation of condylomas in the perianal area , since local immunity is also reduced. Therefore, proctologists often have to deal with cases where a patient has a papilloma in the anus at the site of the fissure.
Most often, the anal area is dominated by a specific species - genital warts. It is a soft tumor-like formation on a thin stalk. If left untreated, it can also invade the genital area, affecting almost the entire perineum. There are single formations, but they are able to quickly form group ones. Such a group tubercle of papillomas on the fissure of the rectum is called papillomatosis.
If fissures and papillomas of the anus are combined, a parallel course of conservative and surgical treatment is required. It is necessary to increase general and local immunity. Anal fissures and condylomas are effectively eliminated by radiofrequency evaporation using the Surgitron apparatus, which leaves virtually no trace of them.
Question: If a chronic anal fissure does not bother you, is it worth doing something about it?
If a chronic fissure doesn’t bother you, well, that’s just great. Unfortunately, this does not happen often. For, like any chronic disease, anal fissure can experience periods of remission (relative calm, when it does not make itself felt) and exacerbation (when all the unpleasant clinical manifestations - bleeding, pain, spasm - are pronounced).
Can a chronic anal fissure hurt without an exacerbation? Of course it can. In chronic cases, pain occurs not during the act of defecation, but after it, and is often spasmodic in nature. It can last from a few minutes to 6-8 hours.
Prevention
In order to prevent the formation of anal fissures, you must follow simple recommendations:
- Empty your bowels regularly and avoid developing constipation or diarrhea.
- Engage in light physical activity (mainly walking or swimming) - this primarily applies to pregnant women and older people.
- Drink at least 1.5-2 liters of water per day.
- Maintain personal intimate hygiene.
- Consult a doctor promptly if you suspect diseases of the digestive tract.
- Do not self-medicate.
Medicines need to help
It is necessary to carefully control your diet; this is a prerequisite for successful treatment. The diet should be dominated by fermented milk products, as well as dishes of plant origin. Avoid spicy, salty, bitter dishes, seasonings that irritate the intestines, and alcohol.
It is important to monitor bowel function: stool should be once a day, its consistency should be soft.
If the first lump is strong enough, do a counter oil enema of 100-150 g of vegetable oil and the same amount of water. The procedure is recommended to be carried out before defecation. The stool is held for 2-3 minutes, then everything passes painlessly and without injury.
After defecation, hygienic procedures are required, warm sitz baths with chamomile, sage, marigold, St. John's wort or potassium permanganate are prescribed, at the final stage you need to put a candle - Relief Advance, Natalsid, Proctoglivenol. The list of medications can be continued, but the main criterion should be their composition: wound healing agents plus painkillers. It would be a good idea to remember the rules for administering suppositories.
Before the procedure, they need to be warmed a little in your hands so that the tip becomes a little softer, then the candle is dipped in oil and inserted into the anus. It is not advisable to push the cone further at once: it must be held at the entrance for several minutes so that the medicine works in the anal canal and not in the ampulla of the rectum.
The best remedy for hemorrhoids and fissures is prevention. No matter how you get rid of an anal fissure, no one can guarantee its recurrence if you do not follow basic preventive measures:
- Monitor your diet and stool quality;
- Maintain personal hygiene standards;
- Don't forget about adequate physical activity;
- Treat dysbiosis, intestinal infections, and defecation rhythm disturbances in a timely manner.
If pain, bleeding, or other disorders occur, do not delay a visit to the proctologist to prevent the disease from becoming chronic. First of all, this applies to those patients who have already been diagnosed with hemorrhoids. Patients who have lived with a fissure for several years continue to wonder after surgery: why did they endure such discomfort?
How will the reception take place?
First, your doctor will ask you about your symptoms. Try to prepare yourself and remember how long ago you had problems and how often you go to the toilet.
The doctor will also likely perform a rectal examination. To do this, he will put on gloves, apply lubricant to his finger and insert it into the anus. Anoscopy may also be required - an examination using a small device with a diameter of a finger, which is inserted into the anus. This way the doctor can see the condition of the anal canal. This is usually the extent of the diagnosis; no laboratory tests are required.
However, the doctor can do without this and refer you for a sigmoidoscopy (examination of the rectum and sigmoid colon by inserting a thin tube with a camera at the end) or colonoscopy (examination of the colon in a similar way). These studies can be carried out under sedation, that is, superficial medicated sleep. Your doctor will refer you for a colonoscopy or sigmoidoscopy if:
- the doctor suspects a disease other than hemorrhoids (for example, polyps, solitary rectal ulcer syndrome, rectal prolapse, anal cancer, or proctitis);
- you are over 50 years old and have not recently had a colonoscopy;
- you have risk factors for colorectal cancer.
Why do anal fissures occur?
Currently, the exact causes of anal fissures are not completely known.
Changing ideas about the causes of anal fissures in adults
Until recently, most proctologists considered constipation to be the main cause of the development of anal fissures. The crack development mechanism was explained as follows:
During the passage of dense and voluminous feces, the walls of the lower part of the rectum are greatly stretched and can “crack” on the surface. In cases where constipation occurs rarely and does not last long (for example, constipation occurred only once), rectal fissures heal quickly without any treatment. On the contrary, if constipation occurs frequently, the cracks can persist for several weeks, months or even longer, since each time dense stool passes, the healed tissues are torn again. Although this theory explains well the appearance of anal fissures in children (discussed in detail below), it cannot explain the appearance of most cases of this disease in adults.
As clinical observations show, in more than 75% of adults with anal fissures (especially chronic ones), there is either no constipation at all, or it occurs rarely and has little effect on the development of the disease. Also, some studies have shown that eliminating constipation does not always lead to healing of chronic fissures.
Obvious contradictions between theoretical ideas about the causes of the disease and practical data have led to a number of additional studies.
In particular, a detailed study of the processes occurring in the tissues in the anus in people with chronic fissures showed that one of the possible reasons for the development of this disease may be an increase in the tone (tension) of the muscle that ensures tight closure of the anus (syn. anal sphincter) .
It was found that relaxation of the anal sphincter depends on the production of a number of biologically active substances, including nitrogen monoxide (NO), the relaxing effect of which on the smooth muscles of internal organs and blood vessels has long been known and used in cardiology.
Thanks to these discoveries, new and very effective treatments for chronic anal fissures have been proposed, which are described in detail below.
Drugs
The basis of conservative treatment of anal fissures is local remedies - rectal suppositories. The range of suppositories is huge; they are of natural and synthetic origin, often have a multi-component composition and are used to eliminate all the main symptoms of the disease.
The best suppositories for the treatment of anal fissures should have analgesic, hemostatic and wound-healing effects.
What drugs are used most often:
- Ultraproct is a combination of glucocorticoid hormone and anesthetic;
- Relief Ultra - contains shark liver oil (accelerates tissue regeneration), phenylephrine (vasoconstrictor and hemostatic effect) and hydrocortisone (anti-inflammatory effect);
- Relief Advance – provides pain relief and wound healing;
- Posterizan - have an immunostimulating effect, promote the restoration of injured mucosa and the healing of cracks;
- Natalsid is a herbal preparation made from brown seaweed, prevents bleeding and heals defects in the mucous membrane, is effective and safe for pregnant women and nursing mothers;
- propolis-based suppositories - have analgesic, hemostatic and regenerating effects;
- suppositories with sea buckthorn - relieve inflammation, have an antibacterial and regenerating effect, this remedy is suitable for children, the elderly and pregnant women.
This is interesting: Cancer horoscope sign characteristics
Very important in treatment is the correct use of suppositories according to the instructions and recommendations of the doctor. Before administration, the suppository should be slightly warmed in your hand to soften it. After insertion, you cannot immediately push the suppository deep into the rectum; you must hold it for several minutes in the anal canal - the main point of application.
In many cases, it is not possible to quickly recover due to severe spasm of the sphincter. What to do in this case? Nifedipine and Nitroglycerin ointment is used topically in a concentration of 0.2-0.4% for application to the affected area in the morning and evening. Old proven methods that are still used by proctologists are blockades - the injection of a small amount of lidocaine under the crack, followed by the use of Solcoseryl. The procedures are repeated according to individual schemes, for example, once a week. A contraindication is the combination of an anal fissure with hemorrhoids.
Surgery
If there is bleeding and pain in the anus becomes unbearable, the person may be prescribed surgical treatment. The specific type of surgical intervention is selected by the attending proctologist.
Conventionally, all methods of surgical treatment are divided into radical and minimally invasive. Radical methods are those that require hospitalization of the patient and a long period of rehabilitation. Minimally invasive – surgical methods that are performed on an outpatient basis and do not require long-term rehabilitation.
To eliminate rectal fissures, the following can be used:
- Cryodestruction. This technique is widely used in the treatment of hemorrhoids. What is the essence of cryodestruction? This method involves the use of liquid nitrogen. That is, the defect, roughly speaking, is frozen. But the operation has a significant disadvantage - often the intervention damages neighboring healthy tissues. Therefore, cryodestruction is used quite rarely.
- Laser coagulation. This method is also widely used in the treatment of hemorrhoids. The essence of this manipulation is to excise the defect using a special device called a coagulator. Laser coagulation is performed on an outpatient basis and takes no more than 1 hour. This technique has a characteristic advantage - during laser coagulation, capillaries and blood vessels are cauterized, so that rectal bleeding does not develop after the operation.
- Excision of anal fissure. This technique is radical and requires special training and a rehabilitation course. The essence of the operation is that the surgeon excises the affected area and leaves the wounds open. Moreover, if the cracks are accompanied by a spasm of the sphincter, then the physician dissects the inner surface of the obturator muscle. In this case, the depth of the cut is approximately 4-5 mm.
After surgical procedures, the disease enters a stage of stable remission. However, there is still a small chance of relapse.
How to recognize the disease
Anatomically, the problem seems to be small, but it manifests itself quite severely. The pain can be of varying intensity and cannot always be tolerated.
If the patient's stool is soft enough, the disease may be asymptomatic.
Many people walk for years with such a crack, and this is not such a harmless phenomenon, since cracks can cause complications of varying severity - from sphincteritis, when the bottom of the ulcer is affected, to the degeneration of the crack into a malignant neoplasm of the rectum.
What should you pay attention to if you have discomfort in the rectum?
- Soreness. It can be pronounced (in the acute stage) or muted (in the chronic form), the condition leads to psychogenic constipation and deterioration in sleep quality.
- Sphincter spasms. When defecating, pain can be accompanied by muscle spasms of varying duration - from several minutes to several hours.
- Burning and itching. This is a characteristic sign of a hemorrhoidal fissure, since when the nodes become inflamed, a caustic exudate is released. Discomfort increases with diarrhea, in the chronic stage, with constant wearing of synthetic underwear.
- Bleeding. The discharge of blood is not intense: a barely noticeable stripe on the stool or a drop on paper. The color is scarlet, without impurities, since only the capillaries burst. If hemorrhoidal bleeding occurs (the color of venous blood is dark), it may be more intense. This condition is dangerous due to anemia.
With an acute symptom, the pain will be strong, continuous, but relatively short-lived: during defecation and 20 minutes after the act.
Anal fissure can be acute or chronic. In the first case, this is a fresh tear, the edges and bottom of the wound are fresh, elastic, there is no pronounced sphincterospasm, and with treatment it has a good chance of healing. A chronic crack appeared a long time ago (it takes at least a month to establish such a diagnosis). The wound is rough, loses elasticity, when injured by stool, it separates into fibers, tears, cracks, like a rough old wound. The prognosis of such a disease, even with high-quality conservative treatment, is very doubtful, so surgical treatment is mainly used.
Diagnosis of hemorrhoids and fissures cannot be based only on these symptoms, because similar complaints are recorded in other pathologies in the rectum (for example, paroproctitis), requiring specific treatment. A specialist will make an accurate diagnosis. Drug treatment of cracks does not always lead to the desired result, as it requires the patient to take a responsible attitude to the problem.
How to treat hemorrhoids with rectal fissure?
To treat hemorrhoids and fissures, several techniques are used, which can be divided into three main categories:
- conservative therapy (use of medications);
- surgical interventions;
- use of folk recipes.
The choice of the leading therapeutic method depends on the severity of the hemorrhoidal process, the size of the rectal fissure, the presence of concomitant diseases and the individual characteristics of the patient’s body.
In addition, an integrated approach to the treatment of hemorrhoids and anal fissures is important. If you focus solely on the use of medications, then you may not expect a special effect. It is necessary to strictly follow a special diet and carry out hygiene procedures.
In general, the complex of therapeutic measures consists of the following important measures.
- Diet food. To improve intestinal motility and soften stool, cereals and fruits that are rich in digestive fiber are introduced into the diet. You should not consume alcoholic beverages, fried, salty or spicy foods.
- Hygiene. After each visit to the restroom, it is recommended to wash the anus with antiseptics or decoctions of medicinal plants (chamomile, marigold, sage, etc.).
- Medicines. Suppositories, ointments, laxatives and antispasmodics help relieve most negative symptoms: pain, spasms, inflammation, bleeding, constipation, etc.
- Enemas. They are not always prescribed, but only in cases where dietary nutrition has not helped improve bowel movements. In addition, enemas with a healing solution can heal rectal fissures and hemorrhoids.
- Sitz baths. Such procedures are carried out both to heal damaged tissues and to relieve spasms of the anus. In the latter case, baths are indicated before visiting the restroom to facilitate bowel movements.
The question of how to treat hemorrhoids and fissures is decided by a proctologist. If he recommends surgical methods after conservative therapy has not yielded positive results, you must agree. It is not always possible to cope with the problem solely with the help of medications.
What causes prolonged or heavy bleeding with anal fissure?
Constant small blood loss, existing for a long time, ultimately contributes to the development of chronic iron deficiency anemia. The patient develops:
- general weakness independent of job performance;
- headaches and dizziness;
- staggering when walking;
- heartbeat;
- loss of appetite;
- pale skin;
- blueness of lips.
In addition to problems with the rectum, one has to constantly be treated with iron supplements and vitamins.