Left ventricular hypertrophy is a dangerous pathological condition that is often diagnosed in people of all ages, including young people, adolescents and children. It is regarded as a manifestation and harbinger of serious diseases related to the functioning of the heart, so it is important to know how to identify the deviation and what to do next.
What is left ventricular hypertrophy of the heart?
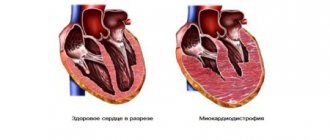
Cardiac hypertrophy, or, in other words, hypertrophic cardiomyopathy, is a thickening of the wall of the left ventricle of the heart, which leads to malfunction of the aortic valve. The problem is common among patients with hypertension, as well as athletes, people leading a sedentary lifestyle, addicted to alcohol and those who have inherited a tendency to pathology.
Myocardial hypertension of the left ventricles of the heart belongs to class 9 on the ICD 10 scale, along with other diseases of the circulatory system. This pathology is mainly a syndrome of other heart diseases, of which it exhibits indirect signs. In order to prevent possible problems in the future, it is necessary to intensively treat the hypertrophied organ in a timely manner, immediately after pathologies are detected.
Degrees of left ventricular hypertrophy
Depending on the signs of LVH and the size of the deformed muscle tissue, several stages of the development of the disease can be distinguished:
- Moderate left ventricular hypertrophy (LVH) occurs as a consequence of hypertension or other heart disease. This seemingly insignificant increase signals an overload of the heart and that the risk of myocardial diseases (heart attack, stroke) for the patient increases. It often occurs without any symptoms and is detected only by ECG analysis. If the left ventricle is enlarged, it is necessary to be treated with the help of specialists, preferably in an inpatient setting.
- Severe LVH is characterized by dystrophic changes in which the mitral valve is located close to the surface of the septum and interferes with blood flow, causing excessive muscle tension and stress on the left ventricle.
Treatment methods
Left ventricular hypertrophy, treatment of which always requires normalization of lifestyle, is often a reversible condition. It is important to give up smoking and other intoxications, lose weight, correct hormonal imbalances and dyslipidemia, and optimize physical activity. There are two directions in the treatment of left ventricular hypertrophy:
- Prevent progression of LVH
- An attempt to remodel the myocardium with a return to the normal size of the cavities and the thickness of the heart muscle.
Next, the main cause that led to hypertrophy is treated (correction of arterial hypertension and treatment of myocardiopathy).
- Beta-blockers can reduce volume and pressure load, reduce myocardial oxygen demand, solve some problems with rhythm disturbances and reduce the risks of cardiac accidents - Atenolol, Metoprolol, Betolok-Zok, Nadolol.
- Calcium channel blockers are becoming the drugs of choice for severe atherosclerosis. Verapamil, Diltiazem.
- ACE inhibitors are drugs that lower blood pressure and significantly inhibit the progression of myocardial hypertrophy. Enalapril, Lisinopril, Diroton are effective for hypertension and heart failure.
- Sartans (Candesartan, Losartan, Valsartan) very actively reduce the load on the heart and remodel the myocardium, reducing the mass of hypertrophied muscle.
- Antiarrhythmic drugs are prescribed in the presence of complications such as heart rhythm disorders. Disapyramide, Quinidine.
- obstruction at the exit of the left ventricle decreases
- The patient's life expectancy increases
- rhythm disturbances, fainting, angina pectoris do not develop
- heart failure does not progress
- quality of life improves.
Thus, left ventricular hypertrophy should be suspected, diagnosed and corrected as early as possible. This will help avoid severe complications with decreased quality of life and sudden death.
Therapy for LVH comes down to three points:
- Eliminate the symptoms of the problem.
- Improved health.
- Prevention of relapse and progression of the disease.
Since in most cases LVH is a consequence of arterial hypertension, then, under the supervision of a doctor, the patient is prescribed the following medications that can normalize his condition:
- ACE inhibitors - tablets "Lisinopril", "Quadripril" and others. These medications improve blood pressure, and if you take them for a long time (at least six months), you can achieve normalization of myocardial wall thickness.
- Beta blockers - drugs Metoprolol, Bisoprolol. These tablets reduce the load on the heart and reduce the heart rate.
- Products based on nitroglycerin. They are able to dilate myocardial vessels, thereby reducing the load on the muscle.
If the cause of wall thickening is a heart defect, then the pathology should be eliminated through surgery. In this case it can take the form:
- Aortic stenting.
- Prosthetics (heart transplant).
- Removing part of the muscle that blocks blood access to the aorta.
Home methods only deal with LVH that was caused by hypertension. You need to resort to non-traditional remedies after receiving doctor's approval.
Among the traditional methods, the following recipes can be distinguished:
- Medicine from St. John's wort - 2 liters of water per 100 g of dry herb. Boil the raw materials and simmer for 10 minutes. Infuse, add honey (200 g). Take 2 tablespoons per day for a month. St. John's wort calms, cleanses blood vessels, prevents arrhythmia.
- Cranberry slurry. Grind fresh berries with honey or sugar. Take 1 tbsp. l. after meal. Cranberry improves blood flow, restores the elasticity of blood vessels, reduces blood pressure, and has a general strengthening effect. It is advisable to make the paste daily to take the medicine fresh.
- Garlic based product. Grind the peeled cloves in a garlic press. Add honey (1:1 ratio). Leave to infuse in a dark place for 5–7 days, periodically shaking the contents of the jar. Take a tablespoon three times a day. Regular intake of garlic cleanses and strengthens blood vessels, helps eliminate arrhythmia, and is useful for hypertension and heart failure.
- Decoction of blueberry shoots. Mix 10 g of raw material with 250 ml of water. Boil for 10 minutes, cool, strain. Take a tablespoon before each meal.
Eccentric, obstructive and concentric left ventricular hypertrophy are difficult to treat. But modern medical technologies make it possible to significantly stabilize the patient’s condition. Treatment tactics are mainly complex.
To restore the natural rhythm of the heart muscle, beta blockers (Propranolol, Anaprilin, Metapropol, Atenolol) are prescribed.
Calcium channel blockers (Verapamil, Procardia) correct the blood supply to the heart and central systems of the body and have a vasodilating effect.
ACE inhibitors - Capoten, Zestril, Enalapril. Reduce blood pressure.
Anticoagulants (Warfarin, Indandione derivatives) prevent the formation of blood clots in the ventricle.
Sartans (Lorista, Valsartan) are first-line drugs for the treatment of hypertension and the prevention of cerebral strokes.
If drug therapy is ineffective, surgical techniques are used. The following surgical interventions are indicated:
- Morrow operation - fragmentary removal of the myocardium in the area of the interventricular septum;
- Mitral valve replacement;
- Aortic valve replacement or transplant;
- Commissurotomy - separation of adhesions at the mouth of the main artery, fused as a result of stenosis (narrowing);
- Stenting of coronary vessels (introduction of an expander implant into the lumen of the artery).
In cases where the treatment of left ventricular hypertrophy does not give the expected results, a cardioverter-defibrillator or pacemaker is sewn in. The devices are designed to restore the correct heart rhythm.
ethnoscience
If the cardiologist approves, you can use the following means:
- Infusions of cornflower, lily of the valley, hawthorn flowers;
- Infusion of St. John's wort with honey;
- A mixture of garlic and honey in equal parts;
- Mixed decoction of wild rosemary, motherwort and cucumber;
- Decoction of parsley stems in red wine.
Long-term consumption of baked milk with strawberry jam, grated cranberries with sugar, dried fruits, raisins, and dried apricots gives a good effect.
Therapy, if concentric hypertrophy of the left ventricular myocardium occurs, consists of eliminating the main cause that caused the development of the disease. It is important to eat right and exclude fatty, fried, spicy and salty foods from your diet. It is necessary to get rid of excess weight, lead an active lifestyle with sufficient, but not excessive physical activity, and also stop taking alcohol and harmful medications. Moderate hypertrophy responds well to treatment if these rules are followed and does not require additional therapy.
Atenolol can be used in the treatment of the underlying disease.
If the disease is caused by arterial hypertension, then it is necessary to take antihypertensive drugs. The choice of drugs depends on the characteristics of the disease in a particular patient. The most commonly used beta blockers are Atenolol and Metoprolol. It is possible to use calcium channel blockers, ACE and renin inhibitors.
Treatment of concentric left ventricular hypertrophy is possible using non-traditional techniques, but they must be combined with traditional medicine. For this purpose, decoctions and infusions of medicinal herbs are used. Physiotherapeutic methods are also possible. Acupuncture, magnetic therapy, mud therapy, medicinal baths and paraffin baths will be useful.
Enlargement of the left ventricle of the heart - causes
The causes of hypertrophy of the left ventricle of the heart can be varied, including both chronic and acquired diseases of different parts of the body:
- hypertension;
- obesity: the development of the disease is very dangerous in young children who are overweight;
- ischemia;
- diabetes;
- arrhythmia, atherosclerosis;
- frequent excessive physical activity;
- alcoholism, smoking;
- high blood pressure;
- lung diseases;
- aortic stenosis;
- disturbances in the functioning of the mitral valve;
- stress, psychological illness, nervous exhaustion.
The development of the body in a child can occur with disruption of the processes of myocardial repolarization and, as a result, an increase in the walls of the ventricle. If such a situation arises, it must be prevented, and then monitored on a regular basis throughout adulthood and prevent progression. Constant exercise can naturally lead to heart enlargement, while work associated with heavy lifting is a potential threat of systolic overload, so you should normalize your physical activity and monitor your health.
Another indirect cause is sleep disturbance, in which a person stops breathing for a short period of time. It can be observed in women during menopause or in older people and entails consequences such as expansion of the diameter of the heart vessels, growth of the septum and walls of the heart, increased blood pressure, and arrhythmia.
Causes
The main causes of left ventricular hypertrophy:
- Hypertonic disease. With high blood pressure, a persistent and prolonged spasm of peripheral vessels is formed. This is why the left ventricle has to make more effort to push blood through than at normal blood pressure . This mechanism is associated with an increase in total peripheral vascular resistance, which leads to overload of the chambers of the heart. Gradually, the walls of the left ventricle thicken, which leads to rapid wear of the myocardium and the formation of heart failure.
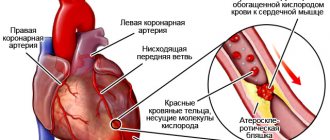
- Cardiac ischemia. During ischemia, the heart muscle lacks oxygen. Cardiomyocytes cannot work efficiently without additional energy substrates, which leads to overload. As a compensatory mechanism, muscle tissue gradually thickens and LV myocardial hypertrophy develops. The cause of age-related cardiac hypertrophy is ischemic changes that develop over time.
- Myocardial dystrophy, cardiosclerosis . Connective tissue grows in the myocardium after inflammatory processes (post-myocardial cardiosclerosis) or after heart attacks (post-infarction cardiosclerosis). Myocardial dystrophy develops with anorexia , anemia, intoxication, infections, etching. After suffering a pathology, some cardiomyocytes lose their contractility, and the remaining cells take on the entire load. In this case, hypertrophy is also a compensatory mechanism.
- Dilated cardiomyopathy. With this pathology, an increase in the size of the heart cavities is observed due to overdistension. The left ventricle must do extra work to push blood out, which leads to the formation of hypertrophy.
- Heart defects. Disruption of the normal anatomy of the heart causes overload of the left ventricle due to increased intracavitary pressure in aortic stenosis , or due to volume overload, which is observed in aortic insufficiency. With other valve defects, hypertrophic cardiomyopathy of the left ventricle also develops over time.
- Congenital LV hypertrophy. Changes begin to form during intrauterine development and appear in the first months after the birth of the child. The reason lies in a genetic predisposition, which leads to disruption of the functioning of myocardial cells.
- Sports heart. In a person who has been involved in sports for a long time and professionally, thickening of the walls of the left ventricle is considered normal. Hypertrophy is due to the fact that the left ventricle takes on the main job of expelling a sufficient volume of blood for the whole body during training. Skeletal muscles require more blood flow during regular exercise, and as muscles grow, the amount of increase in blood flow in muscle tissue becomes constant. That is why the myocardium increases its mass, and the walls of the ventricle become stronger and thicker. For athletes, it is extremely important not to miss the moment when physiological hypertrophy can turn into pathological. This requires regular monitoring by sports medicine doctors.
- Idiopathic LV hypertrophy. If, as a result of a complete examination, it was not possible to identify the cause for the development of hypertrophy, then they speak of idiopathic hypertrophy, which most often implies a genetic predisposition.
Left atrial hypertrophy
From the left atrium, blood enters the ventricle through the mitral valve. With pathology of the valve apparatus, or more precisely with mitral valve stenosis, the atrium has to make more efforts to expel blood. If the valve does not close completely, then part of the blood returns to the atrium with reverse flow, which leads to an increase in the volume of atrial ejection. Similar changes occur in atherosclerosis and rheumatism . If the left ventricle is hypertrophied, then the muscle layer gradually increases in the left atrium.
Right atrial hypertrophy
Main reasons:
- sclerosis of lung tissue;
- obstructive bronchitis;
- bronchial asthma;
- ventricular septal defect;
- changes in the structure of the tricuspid valve;
- right ventricular hypertrophy;
- pulmonary emphysema;
- pathology of the pulmonary valve.
In diseases of the pulmonary system, connective tissue grows, microcirculation is disrupted and pressure in the pulmonary vessels increases. All this leads to forced hypertrophy of the right half of the heart.
Right ventricular hypertrophy, what is it?
The pathology develops after suffering diseases of the pulmonary system of an obstructive nature. Thickening of the muscle layer occurs due to increased pressure in the pulmonary circulation, which makes it difficult for the normal release of blood. Venous congestion caused by progressive heart failure can lead to right ventricular hypertrophy. Thickening of the muscle layer is also observed with congenital heart defects, with narrowing of the pulmonary valve.
Hypertrophy of the interventricular septum
Thickening of the IVS is one of the characteristic signs of hypertrophic cardiomyopathy . In pathology, thickening of the walls of both ventricles is observed with the involvement of the septum between them. This condition is only a derivative of other diseases and is characterized by a specific thickening of the myocardial walls. IVS hypertrophy is considered a fairly common pathology, observed in more than 70% of people, but most often it is completely asymptomatic.
When the interventricular septum thickens, the useful volume of the chambers of both ventricles decreases. All this leads to a decrease in the volume of blood that is released into the vascular bed when the heart contracts. The heart has to work more often to provide organs and tissues with sufficient oxygen and nutrients. Tachycardia wears out the heart muscle and leads to diseases of the cardiovascular system.
Signs of left ventricular hypertrophy
Symptoms of cardiomyopathy are not always obvious, and people are often unaware that there is a problem. If the fetus does not develop properly during pregnancy, there may be a congenital defect and hypertrophy of the left side of the heart. Such cases must be observed from birth and complications should not be allowed. But if there are periodic interruptions in the heart's function and a person feels any of these signs, the walls of the ventricle may be abnormal. The symptoms of this problem are:
- labored breathing;
- weakness, fatigue;
- chest pain;
- low heart rate;
- swelling of the face in the afternoon;
- disturbed sleep: insomnia or excessive sleepiness;
- headache.
- Hypertrophic cardiomyopathy - symptoms and diagnosis, treatment
- Diffuse changes in the myocardium: what does it mean?
- How dangerous is hypertension and why: consequences of the disease
Symptoms
Myocardial dysfunction in the form of hypertrophy manifests itself with characteristic symptoms. There is some difference between lesions of the right and left sides of the heart.
Left ventricular hypertrophy is characterized by:
- discomfort in the heart area;
- rhythm disturbances;
- poor tolerance to physical activity;
- shortness of breath when walking;
- fatigue, general weakness.
Right ventricular hypertrophy is characterized by:
- blueness and paleness of the skin;
- swelling;
- heavy breathing accompanied by shortness of breath, unproductive cough;
- the appearance of arrhythmia such as extrasystole , atrial flutter or atrial fibrillation.
In some cases, autonomic symptoms, poor sleep, tinnitus, and headache .
Types of left ventricular hypertrophy
The types of left ventricular hypertrophy vary depending on the structure of changes in the heart muscles. It happens: concentric and eccentric LVH, ventricular dilatation. They are distinguished based on echocardiographic indicators (cardiogram) and the thickness of the organ walls. Each type of LVH is not an independent disease, but occurs as a consequence of other pathologies in the human body.
Eccentric hypertrophy
Eccentric myocardial hypertrophy is characterized by an increase in the heart and the volume of its chambers in parallel with the thickening of the muscles of the left ventricle. It is provoked by a sharp growth of cardiomyocytes, their transverse size does not change. Also, eccentric LVH threatens to slow the pulse and cause breathing complications. Appears with heart defects or after a heart attack.
Concentric hypertrophy of the left ventricular myocardium
Concentric hypertension occurs due to hyperfunction of myocardiocytes due to pressure load. The size of the cavity does not change, sometimes it even becomes smaller. The size of the walls of the left ventricle, the total mass of the myocardium and the heart increase. Concentric hypertrophy occurs with hypertension, arterial hypertension; causes a decrease in coronary reserve.
Left ventricular dilatation
Dilatation is an expansion of the left ventricle of the heart and occurs when the myocardium changes or the healthy ventricle is overloaded. If the arc of the heart is lengthened, this can also be an initial symptom of LVH. Sometimes aortic stenosis leads to dilation, when the narrowed valve cannot perform its pumping function. Past illnesses are often the cause of heart enlargement; in rare cases, it can occur on its own, as a congenital pathology.
Pathogenesis
A healthy, not organically changed heart is characterized by normal thickness of the walls of various cavities:
- left ventricle – 9-11 mm;
- right ventricle – 4-6 mm;
- left and right atrium – 2-3 mm.
Most often, hypertrophy is observed in the left ventricle, the thickness of which can reach up to 3 cm, and the mass of the entire heart can reach several kilograms. Such changes negatively affect the functioning of the entire cardiovascular system and lead to the development of heart failure .
The load on the heart can increase for various reasons, but all of them lead to thickening of the myocardium as a compensatory response to the increasing load. At the first stages, the patient does not notice any changes, but as trophism and nutrition of cardiomyocytes weaken, the vascular bed loses the ability to cover the needs of the increased myocardial area. Due to the lack of oxygen and nutrients, the contractility of the myocardium is weakened.
Just like blood vessels, the conduction system of the heart cannot expand indefinitely following the myocardium, so arrhythmias due to disturbances in impulse conduction. The thickened myocardium gradually begins to be replaced by connective tissue, losing its pumping function. Long-term hypertrophy can lead to diffuse cardiosclerosis .
Thickening of the wall of one chamber of the heart inevitably leads to expansion of other cavities if left untreated. Elimination of the causes and properly selected therapy leads to regression of LVH.
Diagnosis of cardiomyopathy
Diagnosis of left ventricular hypertrophy occurs in several ways: by identifying signs of the disease on an ECG, examining the heart using ultrasound or using a magnetic resonance imaging scanner. If you experience any heart problems or symptoms of illness, you should contact a cardiologist, and if you have already suffered some kind of defect and suspect complications, you need a cardiac surgeon and, possibly, a treatment system.
Left ventricular hypertrophy on ECG
ECG is a common diagnostic method that helps to find out the thickness of the heart muscle and voltage characteristics. However, it can be difficult to identify LVH on an ECG without the participation of other methods: an erroneous diagnosis of hypertrophy may be made, since on the ECG the signs that are characteristic of it can be observed in a healthy person. Therefore, if they are found in you, this may be due to increased body weight or its special constitution. Then it is worth conducting another echocardiographic examination.
LVH on ultrasound
Ultrasound examination helps to more likely judge individual factors and causes of hypertrophy. The advantage of ultrasound is that this method allows not only to diagnose, but also to determine the characteristics of the course of hypertrophy and the general condition of the heart muscle. Indicators of cardiac echocardiography reveal changes in the left ventricle such as:
- ventricular wall thickness;
- ratio of myocardial mass to body mass;
- coefficient of asymmetry of seals;
- direction and speed of blood flow.
MRI of the heart
Magnetic resonance imaging helps to clearly calculate the area and degree of enlargement of the ventricle, atrium or other compartment of the heart, and to understand how strong the degenerative changes are. MRI of the myocardium shows all the anatomical features and configuration of the heart, as if “stratifying” it, which gives the doctor complete visualization of the organ and detailed information about the condition of each department.
- Malignant arterial hypertension - treatment
- Medicines for hypertension without side effects - main groups according to mechanism of action, composition and treatment regimen
- New generation medications for hypertension: list of drugs
General information
Myocardial hypertrophy is understood as a clear increase in myocardial mass, which develops against the background of hypertension , pathology of the heart valve apparatus and other diseases that are accompanied by prolonged overload of a certain part of the heart.
Myocardial hypertrophy is more typical for the left ventricle, but hypertrophy of the right ventricle and atria may occur. As hypertrophy develops, the myocardium of a certain part of the heart thickens, which leads to a change in its shape, volume and size. Today, hypertrophy is considered not so much as a specific damage to the heart in arterial hypertension, but as a risk factor for the development of heart failure and sudden death. An increase in myocardial mass is recorded in 16% of men and 19% of women under the age of 70 years. In the age group over 70 years old, these figures correspond to 33 and 49%.
How to treat left ventricular hypertrophy of the heart
Many people are susceptible to cardiac hypertrophy. If the problem is severe, medical or surgical treatment of left ventricular hypertrophy is performed. In this case, depending on the extent of the damage, treatment can be aimed at preventing the progression of the disease or at returning the myocardium to its normal size. But it happens that this condition is reversible; if the disease cannot be cured completely, then regression can be achieved by correcting such things as:
- Lifestyle;
- food type;
- hormonal balance;
- excess weight;
- amount of physical activity.
Treatment of left ventricular hypertrophy with medication
Medicines for left ventricular hypertrophy of the heart can have an effective result if taken under the supervision of a doctor. It is impossible to completely eliminate the symptoms of hypertension, but taking antihypertensive drugs for this disease and following a diet will help fight the causes and prevent deterioration of health. To treat LVH, the following medications are prescribed:
- Verapamil is an angiarrhythmic drug from the group of calcium channel blockers. Reduces myocardial contractility, reduces heart rate. Can be used by both adults and children, doses are set individually.
- Beta blockers - reduce the pressure and volume load in the heart cavity, help to even out the rhythm and reduce the risk of defects.
- Sartans - effectively reduce the overall load on the heart and remodel the myocardium.
Myocardial hypertension of the left heart belongs to class 9 on the ICD-10 scale, along with other diseases of the circulatory system. Preference should be given exclusively to drugs whose quality has been tested and proven clinically; experimental drugs may not only not have the expected effect, but also negatively affect overall health.
Cardiomyopathy surgical treatment
Surgery for left ventricular hypertrophy may be necessary to remove the hypertrophied portion of the muscle in late and advanced stages of the disease. To do this, a transplant of the entire heart or its individual parts is performed. If the cause of LVMH is damage to a valve or septum, transplantation of these specific organs is first attempted, which is simpler than whole-heart surgery. In the case of such an intervention, the patient will have to be under the supervision of a cardiologist for the rest of his life and take medications to prevent coronary thrombosis.
Traditional treatment of left ventricular hypertrophy
Treatment of hypertrophy of the left ventricle of the heart with folk remedies cannot help in the later stages of lesions, but it can be effective with minor increases, to prevent their development, and reduce the risk of more serious consequences. You will not be able to completely cure the disease, but traditional medicine can relieve discomfort, chest pain, weakness and fainting. The following means are known:
- Herbal infusions as an auxiliary therapy during the main treatment (blueberry, motherwort, blasphemous hawthorn, horsetail, cornflower flowers, adonis)
- Infused milk: boil and pour into a thermos overnight, or put in the oven until it turns brown.
- Lily of the valley in the form of drops of tincture or gruel. For the tincture, pour vodka or alcohol into the lily of the valley, leave in a dark place for 2 weeks, take 10 drops 3 times a day for 2 months. Gruel: pour boiling water over lily of the valley flowers, leave for 10 minutes. Then drain the water, chop the plant and take a tablespoon 2 times a day. Recommended in combination with drops.
- Garlic honey: mix crushed garlic with honey in a 1:1 ratio, leave for a week in a dark place, take 1 tablespoon 3 times a day before meals.
- Dry red wine infused with dried rosemary. Pour wine over the leaves, leave for about a month in a dark place, strain and take before eating.
- Cranberries, mashed with sugar: a teaspoon 4 times a day.
Why is LVH dangerous?
In cases where minor LV hypertrophy is diagnosed in the early stages, and the underlying disease is treatable, complete cure of hypertrophy has every chance of success. However, with severe heart pathology (extensive heart attacks, widespread cardiosclerosis, heart defects), complications may develop. Such patients may experience heart attacks and strokes. Long-term hypertrophy leads to severe CHF, with swelling throughout the body up to anasarca, with complete intolerance to ordinary household stress. Patients with severe CHF cannot move around the house normally due to severe shortness of breath; they cannot tie their shoelaces or prepare food. In the later stages of CHF, the patient is unable to leave the house.
Prevention of adverse consequences is regular medical monitoring with ultrasound of the heart every six months, as well as constant use of medications.
Diet for left ventricular hypertrophy of the heart
To adjust your diet for cardiomyopathy, follow these tips:
- give up salt;
- eat often, about 6 times a day, but in small portions;
- stop smoking, drink less alcohol;
- choose foods that are lower in fat and cholesterol;
- limit the amount of animal fats;
- Fermented milk, dairy products, fresh vegetables and fruits are healthy;
- eat less flour and sweets;
- if you are overweight, follow a diet to lose weight and reduce the load on your heart.
Prevention
The development of myocardial hypertrophy can be prevented by changing lifestyle and treating the underlying disease that loads the myocardium. Key important recommendations:
- Refusal to drink alcoholic beverages.
- To give up smoking.
- Fighting extra pounds. With a weight loss of even 3-5 kg, it is possible to lower blood pressure and reduce the load on the left ventricle.
- Avoid salt and smoked foods, which slow down metabolism and promote fluid retention.
- Exercise regularly. Loads should be measured, daily. Try to walk more, Nordic walking is encouraged. Yoga and fitness classes have a positive effect on the functioning of the cardiovascular system.
Decoding
Myocardial hypertrophy, regardless of which part of the heart predominates, is always expressed in an increase in the excitation time and amplitude of the segments corresponding to the hypertrophied parts of the heart. For example, hypertrophy of the left atrium on the ECG is expressed by the growth and duration of P, and ventricular hypertrophy - by the QRS complex.
Blockade on the cardiogram - what is it?
In fact, myocardial hypertrophy is the main mechanism that compensates for increasing hemodynamic difficulties and develops when the blood-filled chambers of the heart are overloaded. Thus, the main signs characterizing hypertrophy are:
- an increase in myocardial mass, causing an increase in the electrical impulse, which as a result is expressed by deviations in the form of an increase in the cardiac vector in the direction of the hypertrophied ventricle (on the ECG this looks like an increase in the R wave);
- an increase in the number and length of myocardial muscle fibers, causing an increase in the transit time of the electrical signal along the hypertrophied wall of the ventricle, which on the ECG graph looks like an expansion or deformation of the QRS complex;
- uneven increase in muscle layer fragments disrupts repolarization processes (ST segment and T wave).
Depending on the place where the electrodes are fixed, all the teeth may have different directions. Therefore, when decoding the cardiogram, you should take into account the leads from which the data is read (thoracic region, left or right limb).
Table: Location of electrodes during an ECG study
| № | Lead | Electrode connection point | Electrode polarity |
| 1 | I | right upper limb | — |
| left upper limb | |||
| 2 | II | right upper limb | — |
| left lower limb | |||
| 3 | III | left upper limb | — |
| left lower limb | |||
| 4 | aνR | right upper limb | |
| 5 | aνL | left upper limb | |
| 6 | аνF | left lower limb | |
| 7 | ν1 | 4th intercostal space on the right | |
| 8 | ν2 | 4th intercostal space on the left | |
| 9 | ν3 | between ν1 and ν2 | |
| 10 | ν4 | 5th intercostal space at the level of the center of the clavicle | |
| 11 | ν5 | 5th intercostal space anterior axillary line on the left | |
| 12 | ν6 | 5th intercostal space mid-axillary line on the left |
If left untreated
If you do not pay attention to changes in the heart muscle confirmed by examination, and ignore the doctor’s recommendations, soon one of the diagnoses will appear in the outpatient record:
- Chronic heart failure;
- Arrhythmia;
- Stable or unstable angina.
- Cardiac ischemia.
These pathologies are literally life-threatening. They will not allow you to do without medications and regimen.
Principle of ECG research
An electrocardiogram is a graphical representation of changes in the electrical fields that occur when the heart operates. The contractile activity of the heart is initially regulated by an electrical impulse generated by the sinus node, located at the apex of the right atrium. The impulse quickly spreads through the muscular layer of the atria in the direction from top to bottom and to the left.
Having reached the atrioventricular junction, the impulse significantly reduces the speed and, now, in the opposite direction (from left to right), that is, it first covers the left ventricle, and then the right. All stages of the heart are reflected on the cardiogram in the form of teeth. Normally, an ECG has 5 waves: P, Q, R, S, T.
Table: Correspondence of the designations adopted in the ECG with the duration of the heart phases
| Prong designation | Process | The normal duration is seconds. |
| R | Atrial excitation | 0,16 |
| QRS | Ventricular excitation | 0,08 |
| ST | Complete ventricular excitation | 0,28 |
| straight line | State of rest | 0,23 |
| Total time | 0,75 |
ECG normal
During operation, the heart creates an electric field, registering changes in which, you can obtain information about the processes occurring in it. A complete electrocardiographic examination is carried out by connecting 12 electrodes (leads).
Important! In practice, most often, only 6 leads are used to perform an electrocardiographic study, which often provides insufficient information about the dynamics of changes in heart rhythm.
Danger of disease
The left ventricle in a healthy body is one of the main connecting links in the human circulatory system, allowing blood to move through the arteries to the aorta.
Next, the blood penetrates into organs and tissues through blood vessels. However, with hypertrophy, the muscle tissue of the interventricular septum grows, which greatly narrows the lumen of the left ventricle. As a result, not only blood circulation is disrupted, but also other metabolic processes of the body. This occurs due to the fact that little oxygen and microelements reach the organs and tissues.
Kinds
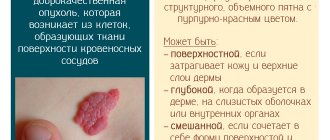
In modern medicine, there are several varieties of this pathology, depending on the reasons for its development:
- Fat. The disease is provoked by impaired fat metabolism, pathologies of the cardiovascular system, alcohol poisoning, hypoxia, etc.
- Ischemic, occurring during a coronary crisis. This condition can cause heart failure.
- Dishormonal. It is observed when there are hormonal imbalances. Very often occurs in women during menopause.
- Diffuse. Occurs in the presence of an extensive inflammatory process.
- Grainy. The cause of the pathology is protein metabolism disorders.
Left ventricular atrophy often occurs in professional athletes. One of the main factors leading to the development of this disease is regular physical activity. The second reason is an unbalanced diet.
Statistical data
- LVH of the heart is often recorded in patients aged 20-40 years.
- Women suffer from LVH less often than men.
- Thickening of the left ventricle over time and if left untreated leads to enlargement of the right atrium.
- Death from this disease occurs in 2–8% of cases.
- At the initial stage of hypertrophy, the patient has a favorable prognosis for recovery.
- It is important for patients to rest at least 7 hours a day, avoid foods that lead to intoxication and toxins, constantly monitor blood pressure, and reduce physical activity.
LVH of the heart is a dangerous pathology, because at first it may not manifest itself in any way and only on ECG, ultrasound and MRI will the cardiologist see changes in the functioning of the heart muscle. If the doctor discovers LVH, he will definitely begin to treat the patient: with medication or surgery. Depending on the cause of the pathology and its severity. If you consult a cardiologist in a timely manner, the prognosis is favorable.
conclusions
Of all the parts of the heart, the left ventricle plays the greatest role in ensuring adequate blood circulation. The large chamber volume, thick muscular wall and opening into the aorta are key characteristics that determine the importance of the structure. Damage to the left ventricle by ischemic, traumatic, inflammatory processes is accompanied by severe hemodynamic defects with symptoms of heart failure. Shortness of breath, swelling, chest pain, a feeling of interruptions in the functioning of the organ are signs of serious disorders that require comprehensive diagnosis and adequate therapy.
Difficulties in treating patients with concomitant pathologies
Drugs are prescribed if left ventricular hypertrophy manifests itself clinically. The prescribed medications should have an effect on the increased pressure in the left ventricular outflow tract, take into account the degree of LVH, and correct the symptoms of chronic heart failure.
The main drugs used to treat myocardial hypertrophy are beta-blockers and calcium channel blockers. If a rhythm disturbance is established, then amiodarone and disopyramide are used for LVH.
Beta-blockers help achieve success in 30-60% of cases, both in the case of obstructive and non-obstructive forms. Drugs in this group: atenolol, propranolol, nadolol, sotalol. They all reduce the need for oxygen in the heart muscle, and during psychoemotional and physical stress they reduce the impact of the sympathoadrenal system.
The result of treatment with drugs of this group is an improvement in the patient’s quality of life, relief of symptoms: a painful attack of angina is stopped or its occurrence is prevented, and shortness of breath and palpitations are reduced. Beta-adrenergic locators can prevent an increase in the pressure gradient in the LV outflow tract in labile or latent forms of obstruction, causing myocardial remodeling. The disadvantage of these drugs is that they do not affect the survival of patients with left ventricular hypertrophy.
Preference is given to beta-blockers that do not have internal sympathomimetic activity. For example, propranolol. Initial dosages are from 20 mg, frequency of administration 3-4 times a day. The dose should be gradually increased, while constant monitoring of heart rate and blood pressure levels is carried out.
The dose is increased to the maximum effective, from 120 to 240 mg. If the use of high doses leads to undesirable reactions, it is recommended to replace the drug with a cardioselective beta-receptor blocker. A separate approach is used for patients who have developed chronic heart failure. This should be taken into account when prescribing metoprolol, carvedilol, bisoprolol.
Calcium channel blockers have a different mechanism of action. Their prescription is justified according to the pathogenesis of LV hypertrophy. They reduce the concentration of calcium ions inside cardiomyocytes, thereby normalizing contractile function and suppressing the process of hypertrophy. Their main actions are a decrease in the contractile force of the heart, a positive inotropic effect, as well as a positive chronotropic effect.
Accordingly, the subjective manifestations of the disease decrease. An example is verapamil. It, like beta receptor blockers, reduces the need of myocardial cells for oxygen and reduces its consumption by heart tissue. This significantly reduces the manifestations characteristic of myocardial ischemia, improves its diastolic function, patients are more resistant to physical stress, and the subaortic pressure gradient is reduced.
When prescribing the drug, some features should be taken into account:
- it reduces total peripheral vascular resistance;
- reduces afterload.
Due to the risk of developing life-threatening complications in patients with severe cardiac asthma, the presence of severe obstruction of the ventricular outflow tract, and high levels of pressure in the pulmonary artery trunk, drugs are prescribed with caution. Possible complications: pulmonary edema, sudden cardiac death syndrome, cardiogenic shock as a result of a sharp increase in the pressure gradient in the cavity of the left ventricle.
The dosage of verapamil is from 20 to 40 mg. three times a day. Preference is given to slowly releasing forms. If the patient tolerates the treatment well, then gradually increase the average daily dose, bringing it to 160-240 mg, not forgetting to control the heart rate.
Additional drugs.
- First of all, these are antiarrhythmic. For example, Disopyramide. It belongs to class 1A and has a pronounced inotropic effect. The use of this medicine for myocardial hypertrophy helps to reduce obstruction, the volume of reverse blood flow (mitral regurgitation) also decreases, and the diastolic function of the heart improves. The dose ranges from 300 to 600 mg. A side effect is considered to be a negative effect on hemodynamics by accelerating the conduction of an electrical impulse through the atrioventricular node, resulting in an increased heart rate.
- Anticoagulants. Prescribed to patients at risk of developing thromboembolism.
- Magnesium and potassium preparations.
- If left ventricular myocardial hypertrophy is caused by or accompanied by arterial hypertension, then treatment is supplemented with antihypertensive drugs.
Therapy effectiveness criteria:
- the degree of obstruction in the outflow tract of the left ventricle is reduced;
- increased life expectancy;
- there is no danger of developing life-threatening complications (arrhythmias, syncope, angina attacks);
- the progression of chronic heart failure is stopped or prevented;
- improving the patient’s quality of life (tolerates acceptable physical activity, easily performs daily housework).
Significant difficulties arise in situations where the patient's hypertrophy is accompanied by chronic heart failure. Drugs such as diuretics, vasodilators from the nitrate group, angiotensin-converting enzyme inhibitors, and glycosides affect the level of pressure in the outflow tract of the left ventricle.
Correct therapy for any disease should be based on the cause of its occurrence. Therefore, it is very important not only to relieve the symptoms, but also to eliminate the immediate cause of the disease. The attending physician should be responsible for drawing up the course of treatment.
It is worth noting that it is not recommended to use medications on your own. This is very dangerous, since each organism has personal characteristics, which manifests itself in drug intolerance. Therefore, taking certain medications without consulting a doctor can only worsen the nature of the disease.
- Treatment with medicinal herbs
Due to the beneficial medicinal properties of some plants, drug treatment can be supplemented with traditional medicine.
Many folk remedies for the treatment of left ventricular hypertrophy are based on medicinal herbs. This allows you to normalize the functions of the heart and restore damaged structures. In addition, herbs significantly improve metabolic processes in the body.
Today, many herbs with medicinal value are used that can be used to treat left ventricular hypertrophy: tinctures of motherwort, St. John's wort and hawthorn, blueberry shoots, wild rosemary, cudweed, cranberry berries and leaves, adonis, lily of the valley flowers, garlic.
When treating with traditional methods, it should be borne in mind that some remedies for hypertrophy contain many different medicinal herbs; you must strictly observe the dosage of each ingredient for preparing a tincture or suspension. This will avoid the risk of complications or worsening the nature of the disease.
Risk group
The incidence of hypertrophic disorders in the left ventricle (LV) depends on gender, age, body weight, and concomitant heart diseases. This pathology is often found in significantly overweight men suffering from hypertension.
Hypertension causes LVH in 70% of cases. The danger of LV hypertrophy is an increased risk of heart failure, ischemia by 3 times, arrhythmia by 5 times, myocardial infarction by 7 times.
An important factor contributing to the formation of myocardial pathology is obesity. One of the clearest indicators of obesity is waist size. This value reflects the amount of internal visceral fat. Women's waist size should not exceed 88 cm, men's - 102 cm.
Signs of LVH of the heart
The problem with hypertrophy is that it has no symptoms. Doctors may suspect the disease based on the following symptoms:
- feeling of suffocation;
- fainting;
- dizziness;
- insomnia;
- fluttering heart syndrome;
- pain in the left side of the chest - pinching, squeezing, squeezing, etc.;
- severe fatigue with previous active physical activity;
- pressure changes;
- migraine;
- accumulation of fluid in the lower extremities (edema);
- dyspnea.
Indirect signs of LVH of the heart are those indicators that are visible using instrumental research methods with an ECG. These include: disturbance of intraventricular conduction, repolarization phases, decrease in the amplitude of the T wave.
Left ventricular hypertrophy
Characterized by thickening of the ventricular wall.
The causes of this condition may be:
- Constant long-term training (professional sports).
- Physical inactivity.
- Smoking tobacco.
- Alcoholism.
- Farby's disease.
- Muscular dystrophy.
- Stress.
- Pathologies of peripheral vessels.
- Obesity.
- Atherosclerosis.
- Diabetes.
- Ischemia.
- Hypertension.
At first, the disease is asymptomatic, but as the process progresses, cardialgia, fainting, dizziness, and fatigue occur. Then comes heart failure, characterized by shortness of breath (including at rest).