A certain number of extrasystoles per day is considered quite normal. In the absence of pathologies, this type of arrhythmia is not dangerous and develops under the influence of irritating factors. The clinical picture becomes noticeable when blood flow is disrupted against the background of an increase in the number of extraordinary (intercalated) contractions. To draw up a treatment plan, you will have to undergo a complete examination. Focusing on the cause of the irregular heartbeat, the doctor will be able to advise effective methods to alleviate the condition.
Diagnosis of pathology
The classic method for recognizing arrhythmias is electrocardiography. Depending on the source of the pathological impulse causing premature contraction of the heart, supraventricular (supraventricular) and ventricular extrasystoles are distinguished. The supraventricular ones include atrial, extrasystoles from the A-V junction, as well as the much rarer sinus. One of the types of ventricular extrasystoles are stem ones.
Variants of extrasystoles from the AV node. a) the P wave has merged with the QRS complex, b) an altered P wave is visible after the QRS complex
All of them have specific ECG signs, which in most cases make it possible to confidently distinguish them from each other. But on a regular resting ECG, recorded within a few seconds, rhythm disturbances are often not detected.
Ventricular extrasystole
Therefore, the main method for diagnosing extrasystole is daily Holter ECG monitoring . Special equipment allows you to record all the electrical activity of the heart during the day, diagnose the type of extrasystoles, their number, distribution over time, connection with exercise, sleep, medication and other important characteristics. Only after this should drugs be prescribed for the treatment of cardiac extrasystole.
Treadmill test or bicycle ergometry
An additional method that helps determine the relationship between arrhythmia and exercise is a treadmill test or bicycle ergometry. This is a type of physical activity (respectively, walking on a moving path or simulating cycling), accompanied by constant ECG monitoring.
If a large number of extrasystoles appear during exercise or at rest, the functional diagnostics doctor reflects this in the conclusion based on the results of the load test.
The method of rhythmocardiography is becoming a thing of the past as it has not found any justified application in the clinic. However, in many medical institutions it is used and also allows you to detect extrasystoles.
Only after receiving a complete description of the extrasystole does the doctor begin treatment.
We recommend reading about atrial extrasystole. You will learn about the causes of its appearance, signs and symptoms in adults and children, diagnosis and basic treatment methods. And here is more information about emergency measures during an attack of atrial fibrillation.
Classification
Gradation of rhythm pathology depending on the location of the source of excitation:
- Ventricular extrasystole. The most commonly diagnosed type of arrhythmia. In this case, impulses distributed only to the ventricles can originate at any segment of the bundle branches or at the point of their branching. The rhythm of atrial contractions is not disturbed.
- Atrioventricular or atrioventricular extrasystole. Less common. Extraordinary impulses originate from the lower, middle or upper part of the Aschoff-Tawar node (atrioventricular node), located at the border of the atria and ventricles. Then they spread upward to the sinus node and atria, as well as down to the ventricles, provoking extrasystoles.
- Atrial or supraventricular extrasystole. The ectopic focus of excitation is localized in the atria, from where impulses spread first to the atria, then to the ventricles. Increased frequency of episodes of such extrasystole can cause the appearance of paroxysmal or atrial fibrillation.
Ventricular extrasystole
Atrial extrasystole
There are also options for their combinations. Parasystole is a cardiac arrhythmia with two simultaneous sources of rhythm - sinus and extrasystolic.
Sinus extrasystole is rarely diagnosed, in which pathological impulses are produced in the physiological pacemaker - the sinoatrial node.
Regarding the causes:
- Functional.
- Toxic.
- Organic.
Regarding the number of pathological pacemakers:
- Monotopic (one focus) extrasystole with monomorphic or polymorphic extrasystoles.
- Polytopic (several ectopic foci).
Regarding the sequence of normal and additional contractions:
- Bigemia is a heart rhythm with the appearance of an “extra” heart contraction after each physiologically correct one.
- Trigeminy is the appearance of extrasystole every two systoles.
- Quadrihymenia is the occurrence of one extraordinary cardiac contraction every third systole.
- Allorhythmia is the regular alternation of one of the above options with a normal rhythm.
Regarding the time of occurrence of the additional impulse:
- Early. The electrical impulse is recorded on the ECG tape no later than 0.5 s. after the end of the previous cycle or simultaneously with z. T.
- Average. The pulse is recorded no later than after 0.5 s. after registration of the T wave.
- Late. It is recorded on the ECG immediately before the P wave.
Gradation of extrasystoles depending on the number of consecutive contractions:
- Paired - extraordinary contractions follow in pairs in a row.
- Group, or salvo - the occurrence of several contractions in a row. In the modern classification, this option is called unstable paroxysmal tachycardia.
Depending on the frequency of occurrence:
- Rare (does not exceed 5 contractions per minute).
- Medium (from 5 to 16 per minute).
- Frequent (more than 15 contractions per minute).
Treatment
Approaches to the treatment of supraventricular and ventricular extrasystoles are somewhat different. This depends on the effectiveness of different groups of antiarrhythmic drugs and the benefits of eliminating precipitating factors for rhythm disturbances.
Lifestyle
For any type of extrasystole, the patient is recommended:
- eliminating emotional stress factors;
- avoiding excessive physical activity;
- refusal of toxic substances - nicotine, stimulants, alcoholic beverages;
- reducing caffeine consumption;
- increasing the content of potassium-rich foods in the diet.
If supraventricular extrasystole
Typically, this type of rhythm disorder occurs with almost no symptoms. Sometimes there is a feeling of palpitations or interruptions in the functioning of the heart. It is not dangerous and has no clinical significance. They do not need to be treated, except in cases where they precede the development of supraventricular tachyarrhythmias or atrial fibrillation. In this case, the choice of drug depends on the arrhythmia being provoked.
For supraventricular extrasystole, drug treatment is prescribed if the rhythm disturbance is poorly tolerated.
Many cardiologists prefer to use long-acting selective beta blockers in this case. These drugs have virtually no effect on carbohydrate metabolism, blood vessels and bronchi. They act throughout the day, allowing you to take them once a day. The most popular drugs are metoprolol, nebivolol or bisoprolol. In addition to them, inexpensive but quite effective Verapamil can be prescribed.
Additionally, if there is a fear of death or poor tolerance to interruptions, valerian, motherwort, Novo-passit, Afobazol, Grandaxin, Paroxetine can be prescribed.
If ventricular extrasystole
A small number of ventricular extrasystoles is not dangerous to health. If they are not accompanied by severe heart disease, drugs for the treatment of ventricular extrasystole are not prescribed. Antiarrhythmics are used for frequent ventricular extrasystole.
Mostly for the treatment of very frequent ventricular extrasystole, surgery is used - catheter ablation (cauterization) of the focus of pathological impulses. However, medications can also be prescribed, primarily class IC and class III:
- etmozin;
- etacizin;
- propafenone;
- allapinin;
- amiodarone;
- sotalol.
Class IC drugs are contraindicated after myocardial infarction, as well as in conditions accompanied by dilation of the left ventricular cavity, thickening of its walls, decreased ejection fraction, or signs of heart failure.
Useful video
For information on what treatment methods for extrasystoles are currently used, watch this video:
The main drugs for the treatment of extrasystole
Bisoprolol (Concor) is most often used to eliminate the supraventricular form of arrhythmia. It is a beta blocker that suppresses sensitivity
corresponding heart receptors.
Beta receptors are also located in blood vessels and bronchi, but bisoprolol is a selective agent that selectively acts only on the myocardium.
If the disease is well controlled, it can be used even in patients with asthma or diabetes.
To achieve the effect, bisoprolol is used once a day. In addition to suppressing arrhythmia, it slows the pulse and prevents angina attacks. It lowers blood pressure well.
The medicine should not be used in patients with edema and shortness of breath at rest (circulatory insufficiency of classes III - IV), with sick sinus syndrome and resting pulse less than 50 - 60. It is contraindicated in atrioventricular block II - III degree, as it can strengthen it expressiveness. You should not take it if the “upper” pressure is less than 100 mmHg. Art. It is also not prescribed to children under 18 years of age.
In more than 10% of patients, especially those with heart failure, the drug causes a heart rate slower than 50 beats per minute. In 1 - 10% of patients, dizziness and headache occur, which disappear with constant use of the medication. In the same percentage of cases, there is a decrease in pressure, increased shortness of breath or swelling, a feeling of cold feet, nausea, vomiting, bowel movements, and fatigue.
Sotalol also blocks beta receptors of the heart and acts on potassium receptors. This necessitates its use for the prevention of severe ventricular arrhythmias. It is used for frequent supraventricular extrasystole, 1 time per day.
Contraindications for sotalol are the same as for bisoprolol, but long QT syndrome and allergic rhinitis are also added.
While taking this drug, 1 - 10% of patients experience the following undesirable effects:
- dizziness, headache, weakness, irritability;
- slowing or increasing heart rate, increased shortness of breath or swelling, decreased blood pressure;
- chest pain;
- nausea, vomiting, diarrhea.
Cordarone is usually prescribed for frequent supraventricular or ventricular extrasystole that cannot be treated with other drugs.
To develop the effect, you must constantly take the drug for at least a week, and then usually take 2-day breaks.
The drug has similar contraindications to bisoprolol, plus:
- iodine intolerance and thyroid disease;
- lack of potassium and magnesium in the blood;
- long QT syndrome;
- pregnancy, breastfeeding, childhood;
- interstitial lung diseases.
More than 10% of patients who use cordarone experience nausea, vomiting, abdominal discomfort, and increased sensitivity to sunlight.
In 1 - 10% of patients, the following unpleasant effects may occur:
- slow heart rate;
- liver damage;
- lung diseases, such as pneumonitis;
- hypothyroidism;
- discoloration of the skin in a grayish or bluish color;
- muscle tremors and sleep disturbances;
- decrease in blood pressure.
Antiarrhythmic drugs for extrasystole
For extrasystole, antiarrhythmic drugs are used depending on the source of extraordinary contractions (according to ECG data):
- supraventricular – Verapamil, Metoprolol;
- ventricular – Lidocaine, Difenin.
When prescribing treatment, the presence of heart and circulatory diseases is taken into account:
- blood stagnation, heart failure - Cordarone, SotaHexal;
- low blood pressure – Lidocaine, Allaforte, Celanide;
- angina pectoris, previous heart attack - Isoptin, Amiodarone, Atenolol;
- hypertension - Anaprilin, Verapamil.
These medications are not needed in all cases of detection of extrasystoles, since in the absence of heart disease they are limited to lifestyle changes (8-hour sleep, quitting smoking, alcohol, caffeine). Indications for taking antiarrhythmic drugs are:
- sensations of the patient in the form of a blow to the heart, interruptions, freezing, strong and rapid heartbeat after a pause;
- general weakness, anxiety, hot flashes, shortness of breath;
- circulatory disorders (more often with bigeminia - one normal beat and extrasystole) - headache, dizziness, attacks of loss of consciousness, disturbances in speech, movements and sensitivity in the limbs;
- suffered severe arrhythmia, performed resuscitation (extrasystoles can provoke fibrillation);
- complex forms of rhythm disturbances (for example, with QT prolongation).
Tablets for cardiac extrasystole
The prescription of tablets for cardiac extrasystole is carried out depending on ECG data and blood tests, since this is not a separate disease, but only a symptom. If the examination does not reveal diseases of the cardiovascular system, then the following medications are recommended:
- calming effect - Valerian, Novo-Passit;
- improving metabolism in the heart muscle - Riboxin, Kratal, Preductal, Actovegin, Mildronate;
- containing potassium and magnesium - Asparkam, Magnicum, Kalipoz prolongatum;
- omega-3 fatty acids – Omacor, Doppelherz Omega 3.
If hypertension, angina pectoris, inflammation (myocarditis, endocarditis) are detected, then all efforts should be directed towards treating the underlying disease. As the condition of the myocardium and blood vessels improves, extrasystoles will also disappear.
Rhythm disturbances can also be caused by:
- cough;
- lack of potassium;
- osteochondrosis;
- damage to the digestive system;
- dysfunction of the thyroid gland, reproductive glands, adrenal glands;
- taking medications;
- smoking, alcoholism.
Therefore, the success of treating this form of arrhythmia depends on identifying and eliminating the main cause.
Watch the video about the causes of arrhythmia:
Extrasystole and other signs of VSD
Considering that extrasystoles cause severe discomfort to dystonics and knock them out of their normal state, they become the cause of the development of other symptoms of VSD. These include:
- increased sweating;
- irritation;
- worry and anxiety;
- weakness and malaise;
- chills and feeling of heat.
Panic attacks that occur during heart dances become the basis for the formation of cardioneurosis. A dystonic person risks developing a phobia against the background of such interruptions in the heart.
Attacks of arrhythmia that occur at night disturb the sleep of the sufferer and provoke insomnia. It can also accompany him as a result of constant worry and anxiety.
Extrasystoles in neurocirculatory dystonia, despite their harmlessness, cause circulatory disorders, including cerebral circulation. As a result, the patient experiences attacks of suffocation, lack of air, and dizziness. Shortness of breath appears.
One of the complications provoked by extraordinary heart contractions during VSD is a panic attack. It begins with an attack of panic and fear, accompanied by a feeling of anxiety and tension. Other symptoms include tachycardia, internal trembling and sweating, nausea, suffocation and dizziness. Characterized by unpleasant sensations in the heart area, tingling and numbness of the arms and legs. The panicker is overcome by fear of death, consciousness is confused, and thinking is impaired.
Thus, arrhythmia, being a sign of VSD, provokes the development of other symptoms of the disease and aggravates its course.
Medicines for supraventricular extrasystole
Supraventricular extrasystole is treated with beta-blockers for:
- rapid heart rate (tachycardia);
- attacks of angina pectoris, previous heart attack;
- rhythm disturbances due to stress, panic attacks, thyrotoxicosis, adrenal diseases.
The following drugs and initial daily doses are recommended:
- Anaprilin 30 mg,
- Atenolol 25-50 mg,
- Betaloc 50 mg,
- Bisoprolol 5 mg,
- Nebil 5 mg.
If necessary, the dosage can be increased by 2 times or a combination of a beta blocker and Sotalol, Amiodarone can be prescribed. If the patient has bronchial asthma or Prinzmetal's angina, then Isoptin or Diacordin are recommended. If extrasystoles occur at rest, Zelenin and Belloid drops are used at night. Teopek has worked well in low doses - 50 mg after lunch and before bed.
If supraventricular arrhythmia appears against the background of myocardial diseases, there is a risk of circulatory disorders, then Propanorm and Etatsizin are used. In most patients without heart damage, significant relief can be achieved with tranquilizers and antidepressants.
Causes
There are many factors that provoke the disease.
Among them:
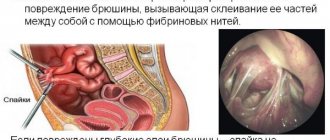
- somatic disorders such as urolithiasis or cholelithiasis, diaphragmatic hernia and even harmless conditions such as stomach fullness, intestinal colic and bloating;
- poisoning with toxic substances, in particular carbon monoxide and benzene;
- negative impact on the functioning of the central nervous system;
- inflammation or chronic pathological processes of the myocardium;
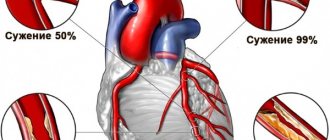
- ischemic disease;
- mechanical disorders of cardiac activity (injuries, surgery, catheterization);
- damage to heart valves;
- intoxication with certain types of drugs, among which adrenaline and digitalis are especially dangerous.
Smoking, both active and passive, can also influence the occurrence of extrasystoles. Dangerous substances that provoke extrasystole include caffeine, which is contained in coffee. Therefore, Cavemans should be more careful and listen to the work of their hearts.
Stress as one of the factors in the occurrence of extrasystole
What to take for ventricular extrasystole
For extrasystoles that occur in the ventricles, take sedatives, antiarrhythmic drugs or a combination of 2 drugs. In asymptomatic cases, no medication is required. For single extrasystoles, diet, lifestyle changes, physical activity, sedatives and beta-blockers are recommended.
Drug of choice
The drug of choice for ventricular extrasystole is often a tranquilizer. It can be of plant origin - extract of valerian, hawthorn, motherwort, Fitosed, Persen, Novo-Passit. For neuroses and vegetative-vascular dystonia with a crisis course, synthetic drugs are also used - Afobazol, Clonazepam or Bellataminal.
How to treat single
For the treatment of single extrasystoles it is recommended:
- a diet rich in foods with potassium - dried apricots, baked potatoes, mushrooms, nuts, legumes, dried fruits, seaweed;
- cessation of smoking, abuse of coffee, diuretics, laxatives, alcohol;
- dosed physical activity - swimming, walking, light running (in the absence of contraindications);
- soothing - peony tincture, Corvalol phyto, Valocordin.
- beta blockers - Atenolol, Anaprilin.
Causes
Each type of extrasystole has its own causes, which lead to conduction disturbances:
Causes of functional extrasystoles:
- Stress.
- Smoking.
- Consumption of alcohol, coffee, strong tea in large quantities.
- Overwork.
- Menses.
- Vegetative-vascular dystonia.
- Infectious and inflammatory diseases that are accompanied by high body temperature.
- Neuroses.
- Osteochondrosis of the cervical and thoracic spine.
Causes of organic extrasystoles:
- Cardiac ischemia.
- Infectious diseases of the cardiovascular system (myocarditis).
- Chronic cardiovascular failure.
- Congenital and acquired heart defects.
- Thyrotoxicosis and other diseases of the thyroid gland.
- Pericarditis.
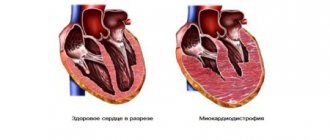
- Cardiomyopathies.
- Pulmonary heart.
- Sarcoidosis.
- Amyloidosis.
- Heart operations.
- Hemochromatosis.
- Pathology of the gastrointestinal tract.
- Oncological diseases.
- Allergic reactions.
- Electrolyte metabolism disorders.
Causes of toxic extrasystoles:
- Chemical poisoning.
- Intoxication in infectious diseases and pathology of the endocrine system.
Frequent extrasystole
For the treatment of frequent ventricular extrasystole, the following is used:
| Treatment | Drug names |
| Antiarrhythmic drugs in tablets | Diphenine, SotaHexal |
| Injections for dangerous forms (heart attack, severe myocarditis, complex arrhythmias) | Lidocaine, Cordarone, less commonly Novocainamide |
| Combinations of 2 drugs to reduce doses of each | Cordarone and Atenolol |
It is possible to reduce the risk of complications during ventricular extrasystole in patients with heart disease with medications that affect:
- blood clotting – Cardiomagnyl, Plavix;
- cholesterol level – Vasilip, Zocor;
- blood pressure – Prestarium, Enalapril;
- metabolic processes in the heart muscle - Preductal, Espa-lipon.
Pathogenesis
As mentioned above, extrasystole is extraordinary and premature contractions of the heart.
Normally, contraction of the heart muscle occurs when a nerve impulse passes from the sinus node, located in the left atrium, through the atrioventricular node, located between the atria and ventricles, along two nerve bundles to both ventricles.
In this case, there should be no deviations along the path of the impulse. This process of passing an impulse is strictly limited in time. This is necessary so that the myocardium has time to rest during the filling period, so that it can then release a portion of blood into the vessels with sufficient force.
If at any of these stages any obstacles or failures arise, or foci of excitation arise in places other than the typical ones, then in such cases the heart muscle fails to completely relax, the force of contraction weakens, and it almost completely drops out of the blood circulation cycle.
For reference. In order for an extraordinary contraction of the heart to occur, i.e., extrasystole, it is necessary to block the sinus node, the main role in the regulation of which is played by the vagus nerve.
It is through the vagus nerve that signals from the brain come from the brain about a slowdown in the heart rate, and through the sympathetic nerves - signals about the need to increase it. If the vagus nerve predominates in the sinus node, impulse transmission is delayed. The accumulation of energy in other parts of the conduction system tries to generate contractions on its own. This is how extrasystole develops in healthy people.
In addition, extrasystoles can occur reflexively when the diaphragm rises, which entails irritation of the vagus nerve. Such phenomena are observed after a heavy meal, diseases of the digestive tract.
The sympathetic effect on the heart muscle leads to its overexcitation. This manifestation can be caused by smoking, insomnia, stress, and mental overload. According to this mechanism, extrasystole develops in children.
In the case of an existing heart pathology, ectopic (pathological) foci are formed outside the conduction system of the heart with increased automaticity. This is how extrasystoles develop in cardiosclerosis, heart defects, myocarditis, and coronary heart disease.
Very often, when the ratio of potassium, magnesium, sodium and calcium ions in the myocardial cells is disturbed, a negative effect occurs on the conduction system of the heart, which is transformed into the appearance of extrasystoles.
With the development of extrasystoles, extraordinary impulses spread throughout the myocardium. This causes early, premature contractions of the heart in diastole. At the same time, the volume of blood ejection decreases, which entails changes in the minute volume of blood circulation. The earlier the extrasystole is formed, the smaller the blood volume will be during extrasystolic ejection. Thus, coronary blood flow deteriorates in heart pathology.
Important! The most life-threatening are ventricular extrasystoles, which develop against the background of organic pathology of the cardiovascular system.
How to relieve an attack: first aid for extrasystole
To relieve an attack of extrasystole, use the following first aid measures:
- sit the patient in a comfortable position;
- ensure the supply of fresh air;
- give water with 20 drops of a soothing tincture (motherwort, hawthorn, mint, valerian, peony) or Corvalol to drink;
- Place a Validol tablet under your tongue.
If the attack is accompanied by panic, trembling of the hands, strong and rapid heartbeat, then breathing into a paper bag or tightly closed palms helps (there should be no gap between them and the face).
Clinical manifestations
One of the clinical signs that helps distinguish organic extrasystole from functional extrasystole is
the patient’s well-being - with an organic lesion, the patient is better in a horizontal position, and with a functional lesion - vice versa.
Very often, extrasystole is completely invisible to patients and there are no symptoms. But, most patients, on the contrary, characterize their feelings as:
- Stop.
- Freezing of the heart.
- A blow from the inside.
- Failure.
Such sensations of cardiac arrest are due to the fact that these feelings depend on the pause that is generated after an extraordinary contraction. This is followed by a cardiac impulse, which is stronger. This is clinically expressed as a sensation of shock.
The most common symptoms in patients with extrasystole are:
- Pain in the heart area.
- Weakness.
- Dizziness.
- Cough.
- Sweating.
- Feeling of chest fullness.
- Pallor.
- Feeling short of air.
- Anxiety.
- Fear of death.
- Panic.
- Loss of the pulse wave when palpating the pulse, which further increases the fear of patients.
- Paresis.
- Fainting.
- Transient speech disorders.
Important! With the development of extrasystoles, the feeling of fear and panic further enhances the release of adrenaline, which, in turn, aggravates the course of the arrhythmia and its symptoms.
It should be noted that the tolerance of cardiac failures in persons who suffer from vegetative-vascular dystonia is much more severe, which does not correspond to the clinical manifestations. But with patients who have pathology of the cardiovascular system, the opposite is true - they tolerate arrhythmia more easily, since the heart is already “trained” to various types of failures, and such patients are morally more stable.
Treatment of cardiac extrasystole with drugs
Medicines for the treatment of cardiac extrasystole are prescribed for frequent, dangerous forms, poor tolerance of arrhythmia, myocardial diseases, and the most common drugs are Anaprilin, Corvalol, Isoptin.
Anaprilin
Anaprilin during extrasystole helps reduce the effect of adrenaline and other stress hormones on the heart. It is effective for rhythm disturbances that occur during emotional stress and heavy physical exertion.
The negative effect of the drug manifests itself in extrasystoles that appear after meals, at night, and at rest. The dose is selected individually, but it is not recommended to slow the pulse to 50 beats per minute, and for elderly patients the lower limit is 55.
Corvalol
Corvalol during extrasystole acts due to a general calming effect; it does not have a specific antiarrhythmic effect on the heart. The reaction to stress factors decreases, the heart rate normalizes (with initial tachycardia). The drug can only be prescribed to patients without myocardial diseases - with neuroses, vegetative-vascular dystonia. Use is contraindicated in patients with:
- damage to the kidneys, liver;
- low blood pressure;
- severe attacks of angina pectoris;
- myocardial infarction;
- heart failure.
Isoptin
The medication is prescribed for extrasystoles, high blood pressure, and rapid pulse. It is indicated for patients who cannot use beta-blockers (bronchial asthma, fluctuations in blood sugar in diabetes, a tendency to allergic reactions). It can be recommended for patients with angina at rest and exertion (variant) with resistance to nitrates.
Causes of extrasystole
In a healthy person, the presence of up to 200 extrasystoles per day is considered the norm, but, as a rule, there are even more of them. The etiological factors of functional arrhythmias of a neurogenic (psychogenic) nature are:
- alcohol and alcohol-containing drinks;
- drugs;
- smoking;
- stress;
- neuroses and neurosis-like conditions;
- drinking large quantities of coffee and strong tea.
Neurogenic cardiac extrasystole is observed in healthy, trained people involved in sports, and in women during menstruation. Extrasystoles of a functional nature occur against the background of spinal osteochondrosis, vegetative-vascular dystonia, etc.
The causes of chaotic contractions of the heart of an organic nature are any damage to the myocardium:
- heart defects;
- cardiosclerosis;
- heart failure;
- cardiomyopathy;
- inflammation of the membranes of the heart - endocarditis, pericarditis, myocarditis;
- myocardial infarction;
- dystrophy of the heart muscle;
- pulmonary heart;
- mitral valve prolapse;
- coronary artery disease;
- heart damage due to hemochromatosis, sarcoidosis and other diseases;
- damage to organ structures during cardiac surgery.
The development of toxic rhythm disturbances is promoted by thyrotoxicosis, fever, intoxication due to poisoning and acute infections, and allergies. They can also occur as a side effect of certain medications (digitalis drugs, diuretics, aminophylline, ephedrine, sympatholytics, antidepressants and others).
The cause of extrasystole may be an imbalance of calcium, magnesium, potassium, and sodium ions in cardiomyocytes.
Functional extraordinary contractions of the heart that appear in healthy people in the absence of visible causes are called idiopathic extrasystole.
Is it possible to cure extrasystole completely?
Since extrasystoles have a reason for their appearance, they can be cured completely if it is detected and eliminated. Drugs for arrhythmia cannot completely eliminate arrhythmia, but only eliminate the manifestations for the period of use.
It is important to take into account that without exception, all medications that normalize the frequency of heart contractions have serious side effects. Therefore, they are used only according to strict indications and in doses prescribed by a cardiologist. During treatment, ECG monitoring is important.
Diagnostics
Extrasystole is diagnosed at an appointment with a doctor when collecting an anamnesis, as well as using methods of auscultation of the heart and palpating the pulse. Cardiologists first note one beat, which occurs ahead of the required time, and then a compensatory pause follows.
If early extrasystoles are observed in the heart, then one of its valve components, namely the second sound, is absent or greatly weakened. The first tone, on the contrary, is reinforced.
The doctor also diagnoses a specific variant of extrasystole, since treatment tactics depend on the nature of the disease. Toxic, functional and organic types of cardiac damage require different therapy.
Diagnosis of the disease
To confirm the diagnosis, it is recommended to conduct an electrocardiographic study (ECG). In some cases, it is necessary to record data over a certain period of time. For this purpose, special sensors are attached to the patient, which record all indicators of cardiac activity both during periods of physical activity and during periods of rest.
How to get rid of extrasystole forever
To get rid of extrasystole forever, patients without heart disease need to:
- make lifestyle changes - sleep at least 8 hours, stop working at night and shift work, and smoking;
- avoid physical, mental and emotional overload;
- stop drinking coffee, energy drinks and alcohol;
- reduce the use of drugs that can disrupt the heart rhythm (vasoconstrictor nasal drops with constant use, tonics, psychotropic drugs, potassium-removing diuretics, laxatives);
- complete a full course of treatment for the disease that caused the extrasystole;
- At least 2 times a year, a complete examination by a cardiologist is necessary, and, if necessary, an examination by a neurologist or endocrinologist.
Extrasystole at rest
Extrasystoles can be organic and functional .
With organic extrasystole, the heart rhythm is restored after the person takes a horizontal position, but the functional pathology in the supine position is more pronounced.
Doctors note a connection between increased tone of the vagus nerve and the development of extrasystole. Extrasystole at rest can occur for the following reasons:
- dysfunction of the kidneys or pancreas;
- obesity;
- hypertension;
- heart failure;
- various heart pathologies.
Important! If the heart rate increases even in a calm state (especially at night or in the evening), it is necessary to consult a specialist as soon as possible and undergo a medical examination.
Diseases that are accompanied by such symptoms must be treated urgently. If during the study, specialists did not reveal serious disturbances in the functioning of the body, in order to bring the heart rhythm back to normal, it is recommended:
- exercise to train your heart muscle and get rid of extra pounds;
- review your daily routine - go to bed on time, take walks in the fresh air;
- give up bad habits - drinking alcoholic beverages and smoking often leads to problems with the heart and blood vessels.
Forecast
Supraventricular extrasystoles are not life-threatening. However, they may be the first symptoms of trouble in the myocardium or other organs. Therefore, if supraventricular extrasystole is detected, consultation with a cardiologist is required, and, if necessary, further examination.
If, according to daily monitoring, the number of ventricular premature contractions is 25% or more of the total number of heartbeats, such a load will ultimately lead to a weakening of the heart muscle. In this case, drug therapy is prescribed to prevent heart failure even in the absence of severe heart disease.
Diagnostic methods
If symptoms characteristic of intercalary contractions are detected, you should contact a cardiologist. He will interview the patient to find out about disturbing signs of failure and the presence of other pathologies. The specialist will then proceed to the examination. The systolic and diastolic pressure threshold will be measured, the pulse will be felt and auscultation will be performed. The last method is the most informative, as it allows you to hear abnormal tones associated with the occurrence of extrasystoles.
The data obtained is not enough to make a diagnosis, but it is enough to suspect arrhythmia and order electrocardiography (ECG):
- Atrial forms of arrhythmia are characterized by a decrease in the distance from the planned P wave to the premature P wave.
- The ventricular and atrioventricular types are characterized by a shortening of the segment from the main QRS complex to the pathological QRS complex.
- A compensatory pause appears after the intercalary ventricular complex and there is no P wave in front of it.
- Pathological changes in the premature QRS complex are observed.
Due to the intermittent nature of the arrhythmia, other ECG monitoring methods may be required:
- Bicycle ergometry is carried out to study the work of the heart at the time of physical overload.
- Daily monitoring using the Holter method is prescribed for a comprehensive assessment of the heartbeat over a 24-hour period.
To differentiate the causative factor, additional diagnostic methods may be recommended:
- Magnetic resonance imaging;
- blood and urine tests;
- echocardiography;
- radiography.
Complications caused by extrasystole
Extrasystole rarely appears out of nowhere, less than 1% of cases; most often, heart rhythm disturbances are a consequence of a serious illness.
The appearance of extrasystole after the age of 40 most often indicates coronary atherosclerosis. Frequent group volley extrasystoles are a sign of myocardial infarction or myacarditis.
The most dangerous types include organic extrasystoles, as they cause complications in the form of myocardial infarction.
Over time, group extrasystoles can develop into more complex forms of heart rhythm disturbances: atrial flutter, paroxysmal tachycardia or atrial fibrillation. Ventricular extrasystole is dangerous due to the development of ventricular fibrillation and sudden death, that is, cardiac arrest.
Frequent extrasystoles lead to consequences such as heart failure and changes in the structure of the ventricles and their fibrillation, that is, irregular operation, which eventually leads to death.
Classification of extrasystole
In medicine, there are several categories into which extrasystoles are divided: by reasons of occurrence, by localization and by the frequency of occurrence of extrasystoles (rhythm disturbances).
According to localization, extrasystole occurs:
• Supraventricular
or
superaventicular
- extraordinary excitation of the atria with discharge of the sinus node.
This type of extrasystole combines atrial and sinus extrasystoles from the atrioventricular junction. Atrial – premature contraction of the heart from impulses from the atria; Nodal (sinus)—premature impulses of sinus rhythm; • Ventricular
– occurs due to premature excitations from the conduction system of the ventricles.
Extrasystole may be rare
and
frequent
, more than 4 per 40 heartbeats,
single
or
group
, 2-5 in a row, as well as
volley
, 5-7 extrasystoles and in the form of allorhythmia, that is, alternating a complex of normal heartbeat with a complex of several extrasystoles in a row.
There are three types of allorhythms: bigeminy
- extrasystole following each normal contraction, after two normal ones -
trigeminy
, after three -
quadrigeminy
.
According to the number of sources of occurrence, extrasystole as a disease is divided into such types as polytropic
, that is,
multiple
and
monotropic
or
single
.
According to the number of extrasystoles that occurred within an hour, ventricular extrasystole, as the most severe, is divided into 6 groups according to the classification of scientists Laun and Wolf.
1. up to 30 extrasystoles per hour of monitoring; 2. more than 30 extrasystoles per hour; 3. polymorphic extrasystole; 4. a. steam extrasystole; b. group extrasystoles leading to ventricular tachycardia; 5. early ventricular extrasystoles of type R on T (according to electrocardiogram data).
Categories 4a, 4b, 5 by medical standards are high-grade extrasystoles, that is, they can be life-threatening due to the triggering of pathologies such as ventricular tachycardia or ventricular fibrillation, and then to cardiac arrest
According to etiology, extrasystole is divided into the following types:
— organic
– the most complex and serious type of heart rhythm disturbances caused by trophic changes in the myocardium, coronary disease or heart defects, coronary insufficiency and cardiosclerosis;
- toxic
- associated with pathological changes in tissues and metabolic disorders in the heart muscle due to the effects of alcohol, coffee, medications and other toxic and narcotic drugs;
- functional
or
vegetative
form - occurs in connection with neurogenic disorders, vegetative-vascular dysfunction, neuroses and strong psycho-emotional stress, in addition they are provoked by gastrointestinal pathologies, heartbeat disturbances are possible with osteochondrosis and hormonal imbalances;
- idiopathic
- extrasystole in a healthy person, without specific reasons for this, occurs in the ventricular part of the heart.
All categories of extrasystoles can be diagnosed using echocardiography, but not all of them are noticeable, and some do not even require significant treatment. A cardiologist will help you understand the causes and prescribe effective treatment.
Reasons for the development of extrasystoles
There can be many reasons for heart rhythm disturbances. It is important to understand the cause and nature of the disease. Extrasystoles are divided into several groups.
Functional extrasystole
This type of extrasystole generally does not require drug treatment. The main method of preventing heart rhythm disturbances is to eliminate the factor that causes extrasystoles. In this case, the development of extrasystole is provoked by the following reasons:
- psychogenic – the presence of stress, psycho-emotional fatigue;
- physical – carrying heavy objects, overwork, running;
- hormonal – menstruation, pregnancy, abortion, menopause.
You should avoid overeating, especially at night. The cause of extrasystole in this case is dysfunction of the vagus nerve.
Organic extrasystole
Frequent extrasystole occurs against the background of various diseases of the cardiovascular system, which is why it is called organic. In this case, an electrical heterogeneity occurs in the heart muscle, which affects the myocardium. Why is this happening:
Not only heart disease can lead to extrasystole. Often, provocateurs can be malignant and benign tumors, allergies of various types, hepatitis, HIV and even banal osteochondrosis of the thoracic region.
Toxic extrasystole
This is the most rare cause of extrasystoles. It develops in cases where there was drug poisoning, which resulted in an overdose or side effects:
- tricyclic antidepressants;
- glucocorticoids;
- aminophylline;
- caffeine
Extrasystole in the heart can also appear during a feverish state.
Symptoms of extrasystole
Often, patients with extrasystole do not feel its symptoms. The signs of this pathology are more pronounced in people suffering from vegetative-vascular dystonia.
With some organic lesions of the heart, extrasystoles can be tolerated even more easily than in the absence of concomitant diseases.
With extrasystole, patients note peculiar tremors, “turnings” of the heart, in other words, sudden interruptions and fading. With functional disorders, general discomfort, weakness, hot flashes, sweating, and lack of air may be observed.
People with atherosclerosis may experience coronary circulatory disorders, dizziness, paresis, and fainting.
Sedatives
Sedatives for extrasystole are prescribed when arrhythmia is caused by neurotic disorders. This group unites a large number of drugs from many pharmacological classes with different mechanisms of action and effectiveness. Here are just a few representatives.
Herbal sedatives are well known and available to everyone. Valerian, motherwort, mint, lemon balm, as well as their combinations - Persen, Sedavit.
Drugs with an anxiolytic effect eliminate anxiety and excessive emotionality by influencing the neurotransmitter system. Popular remedies are Afobazol, Adaptol.
The article discusses the main methods and medicinal substances for the treatment of premature cardiac contraction. However, this is not an instruction for independent action for the patient. Consultation with a specialist is always necessary.
The causes of arrhythmia and its types are different, and therefore the approaches to treatment are different.
In some cases, it is enough to carry out sedative (Sedavit) or metabolic (Mexidol) therapy. And in others, arrhythmia may be unfavorable and the prescription of antiarrhythmics cannot be avoided.
Extrasystole in children
In children, disruptions can occur at any age, even while still in the womb. The reasons for the development of this pathology in childhood are the same factors as in adults.
A special type includes genetic processes for which ventricular extrasystole and tachycardia are the main manifestations. This anomaly lies in the fact that, against the background of arrhythmogenic dysplasia of the right ventricle, the myocardium develops incorrectly. The danger of this pathology is that sudden death often develops.
This type of heart rhythm disorder often does not manifest itself clinically and is determined by chance in 70% of cases.
As the child grows up, he has the same complaints as adults, which may intensify during puberty.
Important! If a child, in addition to complaints of failure, shock, or cardiac arrest, indicates symptoms such as general severe weakness and dizziness, this indicates the development of severe damage to the cardiovascular system and a disorder of hemodynamic processes.
Since extrasystoles of vegetative origin are more typical for children, such extrasystoles are divided into several types:
- Vago-dependence is more common in older children in the form of group, allorhythmic manifestations.
- Combined-dependent – typical for younger children and schoolchildren.
- Sympathetic dependence - most often occurs during puberty. A distinctive feature of such extrasystoles is their intensification in a vertical position, predominance in the daytime and decrease during sleep.
If a child is diagnosed with ventricular extrasystole, it is necessary to monitor him, since in many cases treatment is not required, and the extrasystole itself goes away by the time puberty is completed. But if the number of extrasystoles per day is 15,000 or more, treatment must be started immediately.
Diagnosis and treatment in children are completely identical to those in adults.
Disease prevention
An effective means of combating the disease is timely prevention of the disease. Preventive measures for ventricular extrasystole include:
- a balanced regimen of physical activity and rest;
- long, full sleep;
- proper balanced nutrition;
- rejection of bad habits;
- exclusion of psycho-emotional shocks;
- periodic examinations;
- timely treatment of diseases;
- compliance with the instructions of the attending physician.
You can learn about the characteristics of symptoms and treatment of ventricular extrasystole from the following video:
Metabolic
The modern pharmaceutical industry has a wide range of metabolic agents to choose from. Their main goal is to launch recovery processes, which makes it possible to improve cardiac activity. You can pay attention to the following medications.
Trimetazidine, which has an anti-ischemic, cardioprotective effect. Due to the normalization of energy exchange processes in the myocardium, it reduces the volume of its damage. Restoring coronary blood flow reduces the likelihood of activation of heterotopic foci of excitation, and as a consequence the appearance of arrhythmia.
DETAILS: Bronchitis in adults - treatment and symptoms. How to treat obstructive (chronic and acute) bronchitis in an adult patient? Antibiotics, massage and other medications
Actovegin is extracted from the blood of calves using the ultrafiltration method. It has a positive effect on metabolic processes at the cellular level. Stimulates the regenerative properties of tissues, the ability of cardiomyocytes to fully absorb substances necessary for life.
Mexidol is characterized by antihypoxic, antioxidant, hypolipidemic effects. Reduces blood viscosity and cholesterol levels, which restores microcirculation in the myocardium. Thanks to these properties, the electrical activity of the heart is normalized.
Symptoms
So, quite a few varieties have such a disease as extrasystole. Symptoms of the disease depend on its type. For example, a single atrial extrasystole may not cause patient complaints and manifest itself as rare individual beats of the heart. With frequent or group extrasystoles, the signs are:
increased heart rate; regular shortness of breath; angina pectoris; fatigue, muscle weakness.
Why is extrasystole dangerous? Symptoms of some forms of the disease can progress to heart failure. Timely diagnosis and adequate treatment of extrasystole (and each type of this disorder) is of great importance, since the disease is insidious with its complications. This is especially true for some types of extrasystole, which are caused by heart pathologies. The most undesirable complication in this case is fibrillation - ineffective contractions of the heart that occur chaotically and lead to death. Ventricular extrasystole is manifested by fading of the heart, a feeling of interruptions in its work and rare dizziness. The last symptom is due to the fact that blood is ejected from the ventricle with insufficient force when it contracts prematurely.
ethnoscience
To treat heart contraction disorders, better known as arrhythmia, the folk method of using various infusions and decoctions of plants and herbs is often used. The following remedies, prepared at home, are most effective in the treatment of arrhythmia and tachycardia, as manifestations of extrasystole:
• infusion of black radish with honey helps improve blood circulation; • lemon balm decoction is also effective for arrhythmia; • hawthorn in the form of a decoction or alcohol infusion helps with tachycardia and arrhythmia of all localizations; • a mixture of lemons, honey and apricots should be taken one tablespoon per day; • an infusion of lubstock root or mountain celery relieves heart pain; • to normalize the heartbeat in case of atrial fibrillation and tachycardia, a decoction of Adonis herb is used; • cleaning vessels from a mixture of garlic and lemon; • a mixture of onions and apples in between meals is very effective.
Treatment with folk remedies has excellent analgesic and sedative effects; it makes sense to take them for minor symptoms. But in cases where the cause of extrasystole is heart disease or the condition is accompanied by pain, you need to contact a cardiologist.
Localization of the disease
Extrasystole as a disease is divided into several types of localization, which have already been listed earlier.
Ventricular extrasystole occurs due to the appearance in the cardiac ventricles of an independent focus of contraction impulses, which interferes with the normal functioning of the heart muscle.
This disorder is most often observed in men, especially in old age. This disorder of the heart muscle has virtually no symptoms. As with other arrhythmic disorders, patients experience increased heart rate.
It is not a threat to the patient’s life, however, with high rates of rhythm disturbance, it requires in-depth examination and subsequent therapy. It should be said that the symptoms and medical indications are the same for any location.
Supraventricular appears due to arrhythmia caused by independent foci of impulses of the heart muscle, which occurs in the supraventricular region, the atrioventricular septum. Atrial is caused by the appearance of foci of electrical impulses of the heart in the atria. Atrioventricular occurs due to the occurrence of a lesion in the area of the ventricular-atrial septum.
Find out more about what to do in case of cardiac extrasystole and what it is in general from the video:
Treatment methods
Sometimes such an illness requires only psychological treatment . It happens that you just need to get a person out of an anxious or depressive state for this illness to go away. To do this, you can contact psychiatrists and psychologists.
be treated with medication. What kind of medicine should I take for extrasystole of the heart for unpleasant symptoms? In this case, the following drugs are used:
Allapinin, etatsizin, which are used for arrhythmia Metoprolol, Sotalol, which are adrenaline blockers Verapamil - a calcium antagonist drug
Some do not want to turn to drug treatment methods, preferring folk remedies for cardiac arrhythmia in the form of extrasystole. Here are some recipes for treating cardiac extrasystole:
Hawthorn tincture 10 drops 3 times a day. To prepare it, pour vodka over the hawthorn and leave for 10 days. A mixture of valerian in the same mode. To make it, pour a few teaspoons of this plant into 100 ml of boiling water and cook for 15 minutes. Next, the mixture must be filtered.
When the above remedies are ineffective, you should turn to surgery.
Most often, a special catheter is used , which is “delivered” through the arteries to the desired part of the heart and from it, using radio frequencies, the impulses necessary for the correct heart rhythm are sent.
Possible consequences and complications
If you do not fight the problem in any way, then this “cosmetic” disease can develop into tachycardia , which is much more serious.
In addition, the likelihood of myocardial infarction may be increased , so it is necessary to deal with this disease if it has already occurred and the doctor talks about it. Otherwise, the consequences can be much more detrimental to the main muscle that disperses the blood. Extrasystole can be regarded as the first “bell” that can signal problems.
If you start therapy (if it is needed) promptly, then there can be no consequences or complications.
Prevention
For prevention, you should adhere to certain rules that will help not only avoid recurrence of the disease, but also strengthen the body in general:
Try to adhere to a healthy lifestyle: do not eat fatty foods, exercise within reason, give up bad habits. Get enough sleep Take all kinds of vitamins Spend a lot of time outdoors Reduce emotional stress Avoid caffeine and energy drinks
Follow these rules so that extrasystole does not threaten you in the future.
After all, heart health should be a priority for every person!
Cardiac extrasystole is a premature excitation and contraction of the heart caused by the occurrence of an extraordinary electrical impulse from various parts of the conduction system of the heart. The following types of cardiac extrasystoles are distinguished: atrial extrasystoles, extrasystoles emanating from the atrioventricular junction and ventricular extrasystoles.
Cardiac extrasystole is an untimely contraction of the entire heart or its individual parts
Ventricular extrasystole
The source of ventricular extrasystole are, for the most part, foci located in the conduction system of the ventricles. The impulse first causes excitation of the ventricle in which it originated, and then, with a great delay, excitation of the other ventricle occurs. On the electrocardiogram this is manifested by the following signs.
An increase in the total duration of the ventricular QRS complex by more than 0.12 s and its deformation. Displacement of the ST segment above or below the isoline and the formation of an asymmetric T wave, which is directed in the opposite direction to the main wave of the QRS complex of the extrasystole. An additional electrocardiographic sign of ventricular extrasystole is a complete compensatory pause, but it may be absent in case of ventricular extrasystole against the background of atrial fibrillation.
Ventricular extrasystole in patients with organic heart disease has an unfavorable prognosis, as it significantly increases the risk of sudden death.
Supraventricular extrasystole
With supraventricular extrasystole, the focus of premature excitation is in the atria or atrioventricular junction. There are two types of such extrasystole - atrial extrasystole and extrasystole from the atrioventricular junction.
Atrial extrasystole
Atrial extrasystole is characterized by the appearance of a focus of excitation in the atrium, which is transmitted to the sinus node (up from the focus of excitation) and to the ventricles (down). This is a rare type of extrasystole, which is mainly associated with organic damage to the heart. If the number of contractions increases, complications such as atrial fibrillation or paroxysmal tachycardia are possible. Atrial extrasystole is very often observed when the patient is in a horizontal position. Electrocardiographic signs of atrial extrasystole
Extraordinary appearance of a P wave followed by a normal QRS complex. The location of the P-wave in the extrasystole depends on the location of the impulse: the P-wave is normal if the source of excitation is located near the sinus node; The P-wave is reduced or biphasic if the focus of excitation is located in the middle parts of the atria; The P wave is negative if the impulse is generated in the lower parts of the atria. Incomplete compensatory pause. There are no changes in the ventricular complex.
Extrasystole from the atrioventricular junction
There are three types of this type of extrasystole -
With atrial excitation preceding ventricular excitation. This type does not differ in its characteristics from atrial extrasystole. With simultaneous excitation of the atria and ventricles. With ventricular excitation preceding atrial excitation.
Electrocardiographic signs of extrasystole from the atrioventricular junction.
The P wave is negative and is located after the QRS complex, or merges with the ventricular complex and is not visible on the ECG. The QRS complex is not deformed or widened. Incomplete compensatory pause.
Is it worth fighting extrasystoles?
Since such an abnormal heart rhythm is a common occurrence for a large number of people who do not have organic heart damage, the question remains open: do extraordinary myocardial contractions require medical intervention?
Basic principles of treatment and prevention of complications
The decision about whether to treat extrasystole depends on the concomitant heart pathology and the frequency of occurrence of uncomfortable symptoms. Risk factors, conditions and triggers that increase the likelihood of premature contractions are eliminated or compensated for:
- caffeine, tobacco and alcohol;
- high blood pressure (hypertension);
- chronic stress;
- organic diseases of the heart muscle, including congenital heart defects, coronary artery disease, heart failure.
If, after examination, the doctor concluded that the extrasystoles are caused by problems in other organ systems (not cardiovascular), then the patient treats the provoking causes of the rhythm disturbance. The pathological significance of ventricular extrasystoles increases with their number. The more incorrect contractions, the more likely the development of serious consequences of arrhythmia.
The clinical significance of extrasystoles depends on the context in which they occur:
- in young patients without structural heart disease, extraordinary contractions are not usually associated with an increased risk of sudden cardiac death;
- in older patients, especially with coronary artery disease, the risk of instantaneous asystole (cardiac arrest) with prolonged ventricular arrhythmia is extremely high;
- people after myocardial infarction avoid atrioventricular extrasystole due to the high probability of malignant fibrillation, which blocks the impulse coming from the sinoatrial node.
How often to visit a cardiologist in case of extraordinary heart contractions
A person with a normal number of extrasystoles is advised to see a doctor with regular examinations twice a year in order to promptly identify structural changes or deterioration in the functional state of the heart. If a patient is registered with a cardiologist with chronic myocardial pathology, which is associated with ischemia, hypertension, he is prescribed a consultation at the slightest negative change in condition. If the course of the arrhythmia is favorable, such a patient visits the doctor once every three months.
conclusions
Extrasystoles are often detected during ECG recording. When isolated, extraordinary contractions are of little clinical importance and are found in healthy individuals. Frequent extrasystoles are associated with an increased risk of dangerous cardiac events and complications in patients.
Self-help strategies to help prevent extrasystoles:
- Monitor your triggers . This will identify substances or activities that trigger premature contractions.
- Change your lifestyle . Caffeine, alcohol, tobacco and other recreational drugs are provocateurs of premature ventricular contractions.
- Manage stress . Anxiety causes abnormal heartbeats. If you think your anxiety is making your condition worse, talk to your doctor about prescribing sedatives.
Treatment of ventricular extrasystoles
The main goal of therapy for ventricular extrasystole is to relieve symptoms of the disease and prevent life-threatening arrhythmias. The treatment method primarily depends on the severity of extrasystoles of the ventricular tissue.
For paroxysmal unstable extrasystole, drug treatment is not provided. Patients are advised to exclude factors that provoke arrhythmias - alcohol, smoking, strong coffee and tea, and are prescribed dietary nutrition.
Therapy for persistent symptomatic ventricular extrasystole involves taking medications. For the conservative treatment of VES (ventricular extrasystole), the following groups of drugs are prescribed:
- sedatives – relanium, valerian extract, diazepam;
- beta-blockers – carvedilol, cordinorm, anaprilin;
- antiarrhythmic - novocainamide, mexiletine, quinidine, disopyramide, flecainide;
- antihypertensives – captopril, enaprilin, ramipril.
If drug therapy is ineffective and there is a threat to the patient’s life, they resort to surgical treatment methods - radiofrequency ablation or installation of a pacemaker.