Osteomyelitis
Osteomyelitis refers to an infection of the bone, which can be either acute (recent onset) or chronic (long-standing).
osteomyelitis
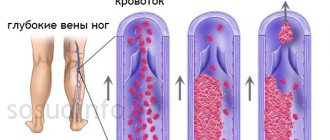
Bacteria are common infectious agents. Two likely methods of access are primary bloodstream infection (including secondary infection through the blood after infection elsewhere in the body) and a wound or wound that allows bacteria to directly reach the bone. In adults, the pelvis and spine are the most vulnerable, and bone infections in children tend to target the long bones of the arms and legs. Without treatment, infection and inflammation block blood vessels. Lack of oxygen and nutrients leads to the death of bone tissue, leading to chronic osteomyelitis. Other possible complications of osteomyelitis include blood poisoning and bone abscesses.
Classification
Clinical classification of osteomyelitis is carried out according to many criteria. The more precise the diagnosis, the clearer the treatment tactics become.
Types of disease depending on the pathogen:
- caused by nonspecific microflora (gram-positive or gram-negative): staphylococcus, pneumococcus, streptococcus, proteus, Escherichia coli and Pseudomonas aeruginosa, less commonly anaerobes:
- caused by one type of microbe (monoculture);
- associated with the association of 2 or 3 different types of microorganisms.
- specific for infectious pathology:
- syphilitic;
- leprous;
- tuberculosis;
- brucellosis;
- other.
- no pathogen was detected.
Bactericidal damage to bone layers.
There are clinical forms of the disease:
- hematogenous:
- after an infection of another organ;
- post-vaccination;
- other.
- post-traumatic:
- after fractures;
- after operation;
- when using spoke devices.
- firearms;
- radiation;
- atypical (primary chronic):
- Brody's abscess;
- Ollier and Garré osteomyelitis;
- tumor-like.
Flow options:
- generalized:
- septicotoxic;
- septicopyemic;
- isolated toxic.
- focal:
- fistulous;
- fistulaless.
Character of the current:
- acute (in particular, lightning);
- subacute;
- primary chronic;
- chronic.
The following stages of the osteomyelitic process are distinguished:
- acute;
- subacute;
- ongoing inflammation;
- remission;
- exacerbation;
- recovery;
- convalescence.
Phases of defeat:
- intramedullary (only the bone marrow is affected);
- extramedullary.
Based on localization, osteomyelitis of tubular and flat bones is distinguished. In long tubular bones, different parts can be affected: epiphysis, diaphysis, metaphysis. Among the flat bones affected are the skull, vertebrae, shoulder blades, sit bones and ribs.
Local complications of osteomyelitis:
- sequestration;
- fracture;
- bone, paraosseous or soft tissue phlegmon;
- pathological dislocation;
- formation of a false joint;
- ankylosis;
- joint contractures;
- violation of bone shape and development;
- bleeding;
- fistulas;
- vascular complications;
- neurological complications;
- muscle and skin disorders;
- gangrene;
- malignancy.
Variants of the disease with common complications:
- amyloid damage to the kidneys and heart;
- severe pneumonia with lung collapse;
- inflammation of the pericardium;
- sepsis;
- other.
The most common variants of the disease are acute hematogenous (in childhood) and chronic post-traumatic (in adult patients).
The disease most often affects certain bones of the human body.
Osteomyelitis of the thigh
Symptoms of femoral osteomyelitis.
It is observed in people of any age, most often of hematogenous origin, but often develops after surgery on the bones. Accompanied by swelling of the thigh, fever and impaired mobility of adjacent joints. A large fistula forms on the skin, through which pus is discharged.
Osteomyelitis of the leg bones
Signs of osteomyelitis of the lower leg bone.
It is observed more often in adolescents and adults, and often complicates the course of tibia fractures. Accompanied by redness and swelling of the lower leg, severe pain, and the formation of fistula tracts with purulent discharge. The tibia is affected first, but then the fibula always becomes inflamed. The patient cannot step on his foot.
Osteomyelitis of the calcaneus
Signs of osteomyelitis of the calcaneus.
Unlike the forms described above, it usually has a long course and often complicates infectious diseases of the foot, for example, diabetes. The main signs are pain and swelling in the heel, redness of the skin, and the formation of an ulcer with the release of purulent contents. The patient may have difficulty walking while resting on the front of the foot.
Osteomyelitis of the shoulder
It often occurs in childhood, has an acute course, accompanied by fever, swelling, and pain in the arm. As the disease progresses, pathological fractures are possible.
Metatarsal osteomyelitis
Signs of osteomyelitis of the metatarsal bone.
It develops when the surgical treatment of a wound resulting from a foot injury is insufficiently thorough. It can also complicate the course of diabetes. Accompanied by pain and swelling of the foot, difficulty walking.
Vertebral osteomyelitis
Develops mainly in adults against the background of immunodeficiency or septic condition. Accompanied by back pain, headache, palpitations, weakness, fever.
Events that can cause osteomyelitis
Bones become infected with blood-supplied microorganisms. In most cases, the microorganism is bacteria such as Staphylococcus aureus, but fungi can also cause osteomyelitis.
Some of the conditions and events that can lead to osteomyelitis include:
Bacteria introduced during bone surgery.
Bacteria are injected when there is a bone injury.
Infection of bone fractures.
Infection of prosthetic implants (such as artificial hip joints).
Infections elsewhere in the body that reach the bones through the bloodstream.
Primary blood infection (septicemia).
Stages of osteomyelitis
Only specialists can determine the stage of osteomyelitis
Osteomyelitis occurs in two forms: acute and chronic. This classification of osteomyelitis allows us to estimate the duration of the disease and the degree of damage to the bone and adjacent tissues.
Chronic osteomyelitis is more dangerous for human health and life, since the process of destruction occurs constantly and, in addition to bone tissue, the bone marrow is affected. With osteomyelitis, the bone marrow can either scleros (take on a solid form due to the deposition of salts of various elements - Ca, Mg, etc.) or deform (change its structure). In both cases, the function of the bone marrow—the production of blood cells—is disrupted. Against this background, a person suffering from osteomyelitis may experience various blood pathologies. Most often, bone marrow damage occurs if a person has osteomyelitis of the femur.
There are three main types of chronic osteomyelitis.
Secondary purulent osteomyelitis. Develops from untreated acute hematogenous osteomyelitis. Atypical forms of osteomyelitis. Such forms of osteomyelitis are quite difficult to identify: the disease develops asymptomatically. This form can appear in any of the bones. One of its manifestations is Garre's disease. Traumatic osteomyelitis can often occur in a chronic form. Especially if it was caused by a gunshot wound.
Chronic osteomyelitis can worsen: with weakened immunity (colds, injuries, emotional and physical stress), the disease can develop from a chronic condition rms in acute mode.
Acute osteomyelitis often contributes to the development of abscesses - destruction of tissues and the formation of cavities in them that contain pus. This condition is clearly expressed when a person has acute odontogenic osteomyelitis. Acute hematogenous osteomyelitis in children occurs in 30% of children under one year of age. If it is not cured, then it turns into chronic hematogenous osteomyelitis, which can persist in the child throughout his entire life.
Acute osteomyelitis is characterized by the immediate development of inflammatory processes and the high speed and strength of immune defense. Antibiotics for osteomyelitis of this form are mandatory. Otherwise, bone destruction will develop, and the person will experience complications.
The disease can also be classified according to the degree of organ damage:
Local or mild form. The general condition fluctuates between normal and moderate severity, body temperature remains within 38-39˚C, there is mild intoxication of the body.
If the disease is not detected in time, the bone cavity may become empty of pus (pus pours into the internal organs or onto the surface of the skin). Odontogenic osteomyelitis of the jaw is characterized by the release of pus into the oral cavity. If after this the source of the disease is not stopped, osteomyelitis will become chronic.
Septic-pyemic or severe form. With this form of the disease, the body temperature rises sharply, the person constantly feels nauseous, vomiting is observed, and intoxication is pronounced. Changes in tissues appear, pain becomes pronounced and clearly localized, swelling, abscess, pathologies of internal organs and serious disorders in the musculoskeletal system also appear. vigator apparatus.
Toxic or adynamic form. The patient's temperature drops sharply, convulsions appear, the person loses consciousness, he develops cardiovascular insufficiency, and blood pressure decreases. A person can die 2-3 days after the first symptoms appear: the disease develops very quickly. Symptoms need to be identified as soon as possible and treatment started immediately.
Risk factors for osteomyelitis
Some of the risk factors that may increase a person's susceptibility to osteomyelitis include:
Long-term skin infections.
Inadequately controlled diabetes.
Poor circulation (arteriosclerosis).
Risk factors for poor circulation include high blood pressure, cigarette smoking, high blood cholesterol and diabetes.
Immune system deficiency.
Prosthetic joints.
Use of intravenous drugs.
Sickle cell anemia.
Cancer.
Diagnosis of osteomyelitis
In the process of diagnosing acute hematogenous osteomyelitis, first of all, methodical palpation is performed, carried out with caution, with the help of which you can determine the most painful area, which will correspond to the center of development of the inflammatory process.
Using X-ray examination, it is possible to determine the localization and extent of the lesion, as well as determine how severe the changes were from a pathological point of view. However, with the help of x-ray examination, symptoms of the disease can be detected only from 10-14 days of disease development. When examined using X-rays, isolated areas of destruction can be identified. When examining an x-ray, they are visible as holes in the bone. In some cases, it is advisable to use computed tomography to establish an accurate diagnosis. If a specialist suspects that a patient has chronic osteomyelitis, then sometimes the fistulography method is used for diagnosis. This diagnostic method allows you to identify the localization of sequestration in the event that conventional images do not show the necessary data clearly enough. In the process of applying this method, contrast agents (sergosine, iodolipol, diodone) are used. The most accurate results can be obtained by using the radioactive scanning method, which uses radioactive technetium.
Also, in the process of diagnosing osteomyelitis, a complex of laboratory tests is used. Thus, the most informative method is to determine the erythrocyte sedimentation rate ( ESR ), which indicates the presence of an inflammatory process in the body.
In order to definitively clarify the diagnosis, a biopsy method with taking a tissue sample is very often used. Bone puncture is performed under general anesthesia . This technique is also used to conduct bacteriological research.
Acute osteomyelitis
The main categories of acute osteomyelitis include:
Hematogenous osteomyelitis is a primary blood infection or an infection from another location in the body that is carried to the bone through the bloodstream. Children are at increased risk. The bacteria travel to areas with a rich blood supply, so the infection tends to target the growing parts at the ends of long bones.
Direct inoculum osteomyelitis - bacteria are delivered directly to the bone tissue through surgery or trauma.
Diagnostics
The doctor examines the area around the affected bone to look for swelling, redness, and tenderness of the tissue. A blunt probe is used to examine fistulas.
Blood tests reveal signs of inflammation - an increase in ESR and the number of white blood cells. Blood and fistula discharge are subjected to microbiological examination to recognize the type of microorganism and determine antibacterial agents that effectively destroy it.
The main diagnostic procedures for osteomyelitis are imaging tests.
The area around the affected bone is swollen, red and tender.
X-ray of bones is used to identify necrotic areas of bone - sequestra. Fistulography - the introduction of a radiopaque substance into the fistula tract - is used to study the internal structure of the fistula. In the early stages of the disease, X-ray examination provides little information.
A CT scan is a series of x-rays taken from different positions. When analyzed, a detailed three-dimensional picture of the affected bone is formed.
Magnetic resonance imaging is a safe research method that allows you to recreate in detail the image of not only the bone, but also the soft tissue surrounding it.
A bone biopsy is performed to confirm the diagnosis. It can be performed in the operating room under general anesthesia. In this case, the surgeon cuts the tissue and takes a piece of the inflamed material. A microbiological examination is then carried out to identify the causative agent.
In some cases, a biopsy is taken under local anesthesia using a long, strong needle passed to the site of inflammation under X-ray guidance.
Signs of osteomyelitis:
- fever and chills;
- bone pain;
- swelling of the affected area;
- dysfunction of the affected limb - inability to raise an arm or step on the affected leg;
- the formation of fistulas - holes in the skin through which pus is released;
- poor health, in children – irritability or drowsiness.
Sometimes the disease occurs with almost no external manifestations.
You should seek medical help if you have a combination of fever and pain in one or more bones.
The doctor must conduct a differential diagnosis with the following diseases:
- rheumatoid arthritis;
- infectious arthritis;
- synovitis;
- intermuscular hematoma, including festering;
- bone fracture.
Chronic osteomyelitis of bone
This form most often serves as the outcome of an acute process. A sequestral cavity is formed in the bone substance. It contains loose pieces of dead bone tissue and liquid purulent discharge. The contents of the sequestration box are released through the fistulas onto the surface of the skin.
Fistulas on the surface of the skin.
The development of the disease is wave-like: the closure of the fistula is replaced by a new phase of inflammation and pus discharge. When the exacerbation subsides, the patient's condition improves. Skin temperature normalizes, pain disappears. Blood counts are approaching normal. At this time, new sequesters are gradually formed in the bone substance, which begin to be rejected and cause an exacerbation. The duration of remission can be several years.
Signs of relapse resemble acute osteomyelitis. Inflammation and pain occur in the affected area, a fistula opens, and soft tissue phlegmon may develop. The duration of relapse is determined by many conditions, primarily the effectiveness of treatment.
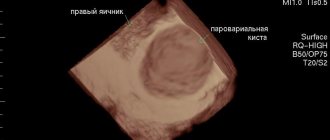
Primary chronic forms occur without signs of an acute stage. Brodie's abscess is a single round cavity in the bone substance, surrounded by a capsule and located in the bones of the leg. The abscess contains pus. There are no pronounced symptoms of the inflammatory process, the disease is sluggish. During exacerbation, pain occurs in the leg, especially at night. Fistulas do not form.
Sclerosing osteomyelitis is accompanied by an increase in bone density and periosteal layers. The bone thickens and takes on a spindle shape. The medullary canal narrows. This form is difficult to treat.
Acute osteomyelitis
The most common variant of this process is hematogenous. It is observed mainly in boys. Phlegmonous inflammation of the bone marrow canal develops.
The toxic variant occurs at lightning speed and can lead to the death of the patient within a few days. The septicopyemic variant is characterized by the presence of ulcers not only in the bone substance, but also in the internal organs.
Most patients have a local form of the disease. The disease begins suddenly. There is a feeling of fullness and intense pain in the limb, often near the knee, shoulder or elbow joints. It intensifies with movement. Body temperature rises.
There is pallor of the skin, rapid breathing and pulse, lethargy and drowsiness. The limb is in a bent position, movements in it are limited. Swelling and redness of the skin occurs above the area of inflammation. There is severe pain when tapping in the affected area or in the direction along the bone axis.
X-ray changes appear only 2 weeks after the onset of the disease.
Complications of osteomyelitis
Some of the complications of osteomyelitis include:
Bone abscess (pocket of pus)
Bone necrosis (bone death)
Spread of infection
Soft tissue inflammation
Hemorrhage (septicemia)
A chronic infection that does not respond well to treatment.
osteomyelitis, diagnosis and treatment
Folk remedies for bone osteomyelitis
After treating osteomyelitis in a hospital and discharging the patient home, you can use some folk recipes to prevent the transition to a chronic form or the development of an exacerbation:
- make a decoction of oat grass (in extreme cases, oat bran will do) and make compresses from it on the sore limb;
- make an alcohol tincture of lilac: fill a full three-liter jar of flowers or buds with vodka and leave in a dark place for a week, use for compresses;
- take 3 kg of walnuts, remove the partitions from them and fill these partitions with vodka, leave in a dark place for 2 weeks; take a tablespoon three times a day for 20 days;
- lubricate the affected area with aloe juice or make a compress from crushed leaves;
- grate a large onion, mix with 100 g of laundry soap; Apply the mixture to the skin near the fistula at night.
Folk remedies.
Treatment of osteomyelitis
Treatment for osteomyelitis depends on the severity, but may include:
Hospitalization and intravenous antibiotics.
Long-term (four to six weeks or more) course of antibiotics, either oral or intravenous.
Painkillers.
Lifestyle changes such as quitting cigarettes to improve circulation.
Treating underlying causes such as diabetes.
Replacement of the infected prosthetic part, if necessary.
Surgery to clean and wash the infected bone.
Skin grafts if necessary.
Amputation, in severe cases.
Symptoms of acute hematogenous osteomyelitis
The initial symptoms of this disease, which appear in the very first days, are general weakness and malaise, a feeling of aching limbs, muscle pain, and headache . A little later, the patient feels severe chills, while the body temperature rises to 39 degrees. The initial symptoms may include vomiting and a feeling of weakness. The patient feels very bad, blackouts, delirium appear, the meninges are irritated, and sometimes convulsions occur. The patient has no appetite and a dry tongue. In addition, the symptoms of acute hematogenous osteomyelitis are paleness of the face, dry skin, which also acquires a yellowish tint, cyanotic color, of the mucous membranes. blood pressure is reduced, muffled heart sounds are heard, the pulse quickens, breathing becomes rapid and shallow. During palpation, the doctor often detects an enlarged liver and spleen. The kidney area is sometimes painful.
One or two days after the onset of the disease, pain begins to appear, which is strictly localized in the affected limb. In this case, the pain has a tearing character, which is why children often, after the slightest movements of the limb, scream loudly from increased pain. In some cases, due to severe pain, the child is forced to hold the limb in a state of complete immobility. This condition is called pseudoparalysis . Also, in the first days, swelling of the soft tissues begins to appear, which is accompanied by distinct pain. The skin in the affected area is red and swollen, and its temperature rises. The swelling of the diseased limb constantly increases, after some time dilated veins become visible, regional lymph nodes enlarge. Sepsis often develops with this condition.
Depending on how severe the disease is, locally focal , toxic ( fulminant ) and septicopyemic forms of the acute type of the disease are distinguished. The locally focal form of osteomyelitis is characterized by the most stable course. The disease begins in a completely healthy child who complains of pain in a specific place. The temperature rises to 39-40 degrees C, over time there is a restriction of movement. Gradually there appears: restriction of movements in the joints, redness of the skin, severe constant pain.
With the septicopyemic form, the patient quickly develops many purulent foci, and this process occurs in parallel in the internal organs or bones.
In the toxic form, a person may suddenly lose consciousness and become delirious. These signs are called signs of “septic intoxication.” They progress unusually quickly and lead to death in the first hours or days of the disease. In this case, clinical signs of bones and soft tissues do not have time to form.
In adult patients, as a result of hematogenous osteomyelitis, the hip or spine is usually affected. Accordingly, pain occurs in this area. However, due to the presence of many causes for pain in these areas, diagnosing osteomyelitis in adults is sometimes more difficult than in children.
The course of acute hematogenous osteomyelitis directly depends on how timely treatment of the disease was started, which primarily includes taking antibiotics.
As a rule, acute osteomyelitis becomes chronic due to ongoing necrosis of the infected area of the spongy or compact layer of bone. In patients who suffer from chronic osteomyelitis, clinical symptoms are usually mild. Their intensification is observed only in case of exacerbation of inflammation. The clinical manifestations of symptoms are aggravated if the overall resistance of the body decreases due to the presence of infection in the bone. This phenomenon can be caused by cold, injury, serious illness and other phenomena.
Hematogenous form
Stages of development of hematogenous osteomyelitis
Acute hematogenous osteomyelitis occurs as a result of the introduction of bacteria that cause inflammation into the blood vessels of the bone. Acute hematogenous osteomyelitis often occurs in children. Usually this inflammation affects long bones, but the duration and nature of the course varies.
Thus, acute hematogenous osteomyelitis can last only two to three months, during which all the body’s defenses are activated and the inflammation goes away on its own.
This is an abrupt form of the disease.
Also, hematogenous osteomyelitis can last about six months. Recovery also comes naturally, but it is a longer process.
In addition, acute hematogenous osteomyelitis can be fulminant. It is provoked by staphylococci. In this case, many decay products of endogenous bacteria are immediately released into the blood, and the pressure instantly drops. In this case, acute hematogenous osteomyelitis can result in death.
It can also last more than eight months and become chronic. Complications may include protein metabolism disorders and muscle atrophy.
Consequences
An infection in the femur often leads to a fracture of the limb. After this, the patient faces a long recovery.
The presence of infection causes intoxication. The site of inflammation contains many phagocytes and leukocytes. They produce substances that destroy bacteria. But along the way, these enzymes destroy bone tissue.
The decay provokes the development of arthritis. The likelihood of infection entering the blood also increases, which often leads to death.
Complications
We also recommend reading:
Hip fracture
As a result of the constant presence of infection, poisoning occurs with metabolic products of microorganisms. This often causes degeneration of the liver and kidneys, disruption of the heart and endocrine system. The inflammatory process attracts a large number of leukocytes and phagocytes to the site of infection. They produce enzymes to kill bacteria. But this also leads to bone destruction. Sequesters consisting of dead pieces of bone tissue and purulent fistulas are formed.
The affected bone is severely deformed, movement in nearby joints is impaired, and a false joint or muscle contractures may form. The purulent process leads to the development of infectious arthritis, and the likelihood of sepsis is also high. Due to bone destruction in chronic osteomyelitis, pathological fractures often occur. In some cases, there is even a need to amputate a limb.
What is osteomyelitis of the jaw
Osteomyelitis in dentistry is an inflammation of the jaw bone tissue of an infectious and purulent nature. The causative agents of the disease include:
- staphylococci;
- coli;
- tuberculosis bacillus;
- rickettsia;
- streptococci;
- Pseudomonas aeruginosa;
- Klebsiella;
- gram-negative bacteria;
- viruses.
The most common are streptococcal and staphylococcal infections of the jaw tissue. Often the disease leads to generalization of the infection, which causes infection of the entire human skeletal system and nearby tissues.
Osteomyelitis is a multifactorial disease, the likelihood of its development is influenced by:
- infection by pathogenic microorganisms;
- state of the immune system;
- disturbance of local blood circulation.
Prevention of bone inflammation
The most common type is hematogenous or post-traumatic osteomyelitis. Damage to bone tissue does not occur immediately; it is usually preceded by other infectious diseases or injuries. Therefore, if you take preventive measures, inflammation can be avoided. It is very important to immediately consult a doctor if symptoms of infection appear, to treat chronic diseases in a timely manner and to prevent the presence of foci of infection in the body, for example, caries.
To prevent traumatic osteomyelitis, you need to provide proper first aid immediately after the injury. If soft tissue is damaged or there is an open bone fracture, it is necessary to treat the wound with Chlorhexidine solution, lubricate its edges with brilliant green or iodine and apply a sterile napkin. The affected limb should be immobilized and ice may be applied to prevent swelling and relieve pain.
Infectious lesions of bone tissue are often not taken seriously by patients. But if treated incorrectly, osteomyelitis can lead to disability and even death. Therefore, you need to be more attentive to your health and consult a doctor at the first symptoms of inflammation.
Causes of inflammation
The pathogen can penetrate internally (endogenously) through blood vessels. This is a hematogenous type of transmission of infection, more often it occurs in children and adolescents. In the exogenous route, the introduction of microorganisms occurs from the external environment, for example, during an open fracture. The contact type develops as a result of infection of the bone from inflamed soft tissue. The aseptic course of spinal osteomyelitis is observed during closed fractures and surgical operations. The main causative agent of the purulent process is Staphylococcus aureus, sometimes Escherichia coli, Pseudomonas aeruginosa or Streptococcus. The causes of inflammatory disease of the bones of the spine may be the following:
- the presence of infectious foci in the body - boils, sore throat, adenoids;
- open fractures, wounds, ulcers, penetrating wounds;
- the body's tendency to allergic reactions;
- decreased general immunity;
- lack of nutrition, physical exhaustion;
- renal and heart failure, diabetes mellitus;
- uncontrolled use of steroids or psychotropic drugs.
There are other reasons, for example, the use of untreated injection needles; medical catheters can also serve as a conduit for infection. The risk group includes older people, as well as people with chronic diseases.
Diagnosis of the disease
Diagnosis of osteomyelitis includes several research methods: 1. Laboratory. 2. Bacteriological. 3. Morphological. 4. Radiation.
Laboratory tests include urine and blood tests. The blood is checked for the presence of glucose (to exclude or confirm diabetes), and the level of white blood cells, ESR and C-reactive protein is also determined. Of course, this will not give a clear picture and will not indicate the presence of osteomyelitis, but it will reveal inflammation.
If there is a fistula or purulent wound on the patient’s body, a culture is taken to determine the type of pathogenic microflora and its sensitivity to antibiotics. However, cultures of purulent compartments do not allow us to accurately determine which bacteria are attacking the bone. Often, in the chronic form of the disease, when the study is carried out in a hospital setting, the culture contains a hospital infection that is not related to the real pathogen. Biopsy data are more accurate.
X-rays can show the presence of a disease, but this data is not enough to create a complete picture. Tomography is needed to examine large bones and joints, the spinal column and the pelvic area. And if there are fistulas - fistulography.
An important role in the diagnosis of osteomyelitis is played by its main symptom – osteonecrosis and sequestration. In addition, it is necessary to take into account the periosteal reaction. Its power depends on the age of inflammation. Layered periostitis indicates that exacerbation of osteomyelitis has occurred again.
A clear sign of chronic osteomyelitis is thickening of the bone, in which cavities are formed, due to which the medullary canal narrows and is not visualized on an x-ray. It is most difficult to make a diagnosis when the bones are changed due to osteonecrosis and hyperostosis. In such cases, it is necessary to carry out computer diagnostics.
Computed tomography allows us to study the layered structure of bone. This method quite often helps to see hidden areas of tissue destruction and sequestration. MRI has higher sensitivity than CT. Using this method, you can not only detect pathology, but also distinguish between the microflora that has attacked bone and soft tissue. In addition, MRI allows you to determine the extent of tissue affected by necrosis and the location of vital organs adjacent to the lesion in order to avoid injuries and complications during surgical operations.
Radionuclide diagnostics is aimed at identifying the disease in the early stages. It has a fairly high sensitivity, but the specifics of its application and price do not make it possible to use it in relatively small or ordinary public medical institutions.
In cases of acute gunshot osteomyelitis, complex treatment with mandatory surgical intervention is used
Using ultrasound, you can detect pus, swelling, changes in the surface of bones, peristalsis, cortical and bone sequestration, and the presence of fluid in the joints. It also allows you to assess the quality of blood supply to the limb. Separately, no single method will give a 100% guarantee of the presence or absence of osteomyelitis, so in practice several examination methods are used simultaneously.
Pathogenesis (disease development)
1. Spread of infection from hidden or obvious foci of infection. With the blood flow, the infection penetrates into the area of the expanded section of the long tubular bones (metaphysis). In these areas, the bone tissue has a cellular appearance (spongy substance). The speed of blood flow here is significantly slowed down. Fixation of microbes occurs in the sinuses of the spongy substance. The infection then spreads under the bone. The resulting pus peels off the periosteum, forming an abscess. The pressure inside the bone canal increases significantly, causing unbearable pain. After the purulent masses break through the periosteum, the process moves to soft tissues, forming phlegmon. The pain subsides somewhat during this period.
Next, the inflammatory process breaks out, forming multiple channels communicating with each other and fistula tracts. With good immunity and adequate antimicrobial therapy, the infection dies. Otherwise, the process takes a long time. Sometimes it becomes chronic.
Rice. 11. Gunshot wound of the thigh after suppuration: 1 - sequestration; 2 – purulent cavity; 3 - leaks of pus; 4 — bone fragment (free); 5 – wound channel; 6 – bone tissue (regenerating).
2. In open fractures and gunshot injuries, inflammation develops as a result of infection of the wound surface, which quickly spreads to the bone marrow. With a favorable outcome of the disease, the resulting granulation tissues prevent the spread of infection. But, if the repair processes are disrupted, then the process takes on a long course. Bone fragments become necrotic, and cavities filled with purulent masses form. Molten purulent masses, spreading, form multiple channels. When the skin breaks through, fistula tracts are formed.
3. In the chronic course of osteomyelitis, a cavity begins to form in the bone structures, which contains purulent molten masses and sequesters. Over time, the wall of the cavity is replaced from the inside by bone substance. From purulent cavities, forming numerous channels, pus spreads into nearby tissues. Fistula tracts formed when the skin is destroyed do not allow the development of callus. If the fistulas function well, the periosteum begins to thicken (sclerosis). In a chronic course, during periods of remission, granulation tissues become scarred. Over time, calcium salts are deposited there, and pathological ossification of muscle tissue develops (myositis ossificans). An exacerbation of the process occurs due to a violation of the outflow of purulent contents from the cavities.
Causes
Most often, chronic osteomyelitis develops after the acute stage. The reasons for this are simple: the patient’s weakened immunity and improper treatment of the disease. It usually occurs 3-6 weeks after the onset of the inflammatory process. The patient's condition improves, but the infection in the bone remains. This happens for the following reasons:
- late treatment;
- incorrectly chosen antibiotics;
- failure by the patient to comply with all doctor’s instructions;
- errors during the operation;
- insufficient cleaning of the purulent focus.
Most often, osteomyelitis becomes chronic in children, elderly patients, and people weakened by other diseases. This is approximately 20-30% of patients. In other cases, even with the formation of sequestration and bone necrosis, the damaged areas are gradually replaced by healthy tissue.
Even with external improvement of the condition, the purulent process in the bone continues
Diagnosis of chronic odontogenic osteomyelitis
Diagnosis of chronic odontogenic osteomyelitis consists of collecting a history of the disease, examining the patient and performing radiography.
From the anamnesis we learn that the patient either suffered from acute osteomyelitis and did not seek help, or assistance was provided to him, but the acute form of the process became chronic. In both cases, further examination of the patient is carried out.
The clinical picture is very diverse, so it is difficult to accurately characterize all the signs of the disease.
Externally, the face may be asymmetrical due to soft tissue swelling or bone deformation. In the productive form, asymmetry can be caused by an increase in the volume of bone tissue.
The opening of the mouth is either normal or not fully, which is caused by inflammatory contracture of the masticatory muscles.
Lymph nodes are normal or may be slightly enlarged and painful on palpation.
When examining the oral cavity, an inflammatory infiltrate, hyperemic mucosa, the causative tooth or the socket of an extracted tooth are determined. Fistulas are found on the mucous membrane of the oral cavity or on the skin, through which formed sequestra are probed. Teeth that are mobile in acute osteomyelitis are less mobile in the chronic form of the disease.
Next, an X-ray diagnosis is carried out, preferably an orthopantomogram or radiography in two projections (direct and lateral). In the acute form of odontogenic osteomyelitis, only the source of infection is observed - thinning of the bone tissue in the area of the apex of the root of the causative tooth. If the disease has become chronic, sequestration is visible on the image. But the first manifestations of the disease in the picture appear only at the end of the 2nd, and sometimes 3rd, week. The situation with the destructive form of osteomyelitis is described above.
If we talk about the productive form, then bone sequestration is not observed. But the amount of mineralized tissue increases due to the reaction of the periosteum. The patient's face becomes asymmetrical, the bone increases in volume.
Chronic odontogenic osteomyelitis of the lower jaw
Chronic odontogenic osteomyelitis of the lower jaw often affects only the alveolar part of the bone, less often the body or branch of the jaw. Due to the structural features, the disease is severe with the formation of small and large sequesters. Often, the destruction of bone tissue leads to a pathological fracture (the bone breaks with a weak “blow” to the jaw).
Chronic odontogenic osteomyelitis of the upper jaw
Chronic odontogenic osteomyelitis of the upper jaw develops faster and is easier than in the lower jaw. Sequestra are formed in 3-4 weeks, while in the lower jaw - in 6-8 weeks. With the diffuse nature of the disease, destruction of the anterior wall of the maxillary sinus or even the lower edge of the orbit is possible.
Clinical picture and symptoms of atypical forms of osteomyelitis
Chronic sclerosing osteomyelitis Garre (Garre) is a type of staphylococcal infection. Most often, the tibia or femur is affected in the middle third of the diaphysis, less often - closer to the metaphysis. A piece of bone up to 12 cm long is affected. Swelling in soft tissues without redness, very dense to the touch, never resolves, and suppuration and fistulas never form. The muscles become immobile.
The pain is very severe, especially at night. The bone thickens in a spindle-shaped manner. External contours are clear. There is a sharp thickening of the outer layer. Sclerotic masses gradually fill the entire canal. There are no foci of destruction. The course of the disease is torpid, without significant symptoms. Young men aged 20–30 years are most often affected.
Rice. 13. Garre's osteomyelitis. Fusiform thickening of the bone.
Rice. 14. Garre's osteomyelitis. Sclerotic masses gradually fill the entire canal.
Ollier's albuminous osteomyelitis is a type of staphylococcal infection whose virulence is significantly reduced. The inflammation occurs without suppuration. The process begins with the cortex of the femur. The peeling of the periosteum has a significant extent. The course of the disease is without significant symptoms. The disease mainly affects children.
Brodie's abscess is caused by Staphylococcus aureus. The disease is rare. Young men get sick. The area of inflammation is limited. The process is localized in the femur in the area next to the joint. Over time, an abscess forms here. The course is sluggish, perennial, asymptomatic. The pathogen is often absent from the contents of the abscess. The virulence of staphylococci is significantly weakened.
Rice. 15. Brodie's abscess. Abscess in the spongy substance of the tibia.
X-ray technique
If osteomyelitis is suspected, it is necessary to select the optimal dose of X-ray radiation. The higher the hardness of the rays, the more contrast the image and the better the inflammatory areas are visible.
The chronic course of the pathology requires mandatory research. This is necessary to clarify the degree of damage and control the dynamics of the development of the process, since the study expands the field of view and helps the doctor fully imagine the volume of the lesion.
When sequestration and fistulas appear, the method of direct magnification of radiographs or fistulography is used - a study with intravenous contrast.
Diagnostics helps to accurately determine the extent of destructive damage to bone and soft tissue, and allows the traumatologist to select the optimal method of surgical intervention.
In the chronic course of hematogenous osteomyelitis, the technique is not very informative, since dense foci of sclerosis make visualization difficult. In this case, a fistula tomographic examination is required.
Symptoms
Chronic osteomyelitis, like acute osteomyelitis, can occur both generalized and local, so the symptoms may differ.
Osteomyelitis
The local form is characterized by:
- Bursting pain and aches.
- Temperature up to 38.5 (if osteomyelitis is chronic, then there may not be a high temperature).
- Elevations and swelling in the area that is damaged.
- Movement is painful and limited.
- The skin on the damaged area turns red and warms up.
- Pus is released through the skin.
- Abscesses occur.
In the generalized form, other symptoms occur:
- The pain becomes constant and intensifies.
- Body temperature is 39–40 degrees.
- Urination becomes painful and frequent.
- Possible damage to the nervous system (fainting, convulsions, less often delirium).
- General health worsens due to intoxication of the body.
- The skin turns pale.
- Thermoregulation disorders – chills, sweating.
If the disease is not noticed, then the acute form quickly turns into chronic, so diagnosis is important here more than anywhere else.
The diagnosis is established based on the results of a microbiological examination (bone biopsy, blood culture, fistula opening, joint fluid), x-ray (although in the early stages it is impossible to detect the disease with its help), computed tomography (helps to find gas in the bone marrow, as well as areas of dead tissue ), fistulography, MRI, radionuclide diagnostics (suitable for the earliest diagnosis) and ultrasound.
Treatment of spinal infection
As a rule, in the main cases osteomyelitis is treated conservatively. Therapy is carried out with intravenous antibiotics.
Since the disease is primarily caused by the Staphyloccocus bacterium, which is highly sensitive to antibiotics, the intravenous treatment process takes about a month, and then a control two-week course begins, which is administered orally. During the entire period, the patient is prescribed bed rest.
Antibiotics for osteomyelitis
Important! If the infection is of tuberculosis etiology, the patient may take antibiotics for up to a year.
In addition to therapy, the spine is fixed for six to twelve weeks using a rigid corset, until x-rays show positive dynamics of therapy.
At the same time, detoxification procedures may be prescribed, painkillers and immunomodulators may be prescribed.
Treatment of osteomyelitis with folk remedies
Surgical method
Surgical intervention is performed in exceptional cases of the need for decompression of nerve structures, as well as if complete sanitation of the damaged bone with removal of necrotic areas is necessary.
Surgery is performed if the patient is resistant to antibiotic therapy
In the presence of a large number of bone destruction, accompanied by pain and deformation of the vertebrae, surgical reconstruction of the damaged elements with grafts is performed.
Possible complications
Being, of course, a dangerous and serious disease, osteomyelitis can cause a number of complications.
- Bone necrosis resulting from tissue death.
- Septic arthritis, in which infection spreads to nearby joints.
External signs of infection of the knee joint
- Stunted bone growth, common in children.
- Squamous cell skin cancer, which is caused by the formation of an open wound that produces purulent discharge.
Squamous cell keratinizing carcinoma
Reconstructive procedures may be required after both surgical and conservative treatment. As soon as the infection is neutralized and a complete cure has occurred, the rehabilitation stage begins, including health-improving exercises and physiotherapy.
As a result, normal mobility returns to the spine, residual discomfort disappears, inflammation completely disappears, and the affected areas return to normal.
Video – Osteomyelitis
Surgery
It is mandatory to wash the wound and fistula cavities with an antibiotic solution. The muscle phlegmon is opened and drained. During the operation, which is carried out during the period of remission, the doctor must remove all necrotic parts of bones and tissues, and the fistula canals are excised. According to indications, transplants are used, the Ilizarov apparatus is used.
Surgical treatment of chronic osteomyelitis is a long and multi-stage process; complete restoration of the limb is almost impossible. Refusal to undergo surgery can lead to sepsis, limb amputation, pulmonary embolism, and death.
Causes
It’s worth saying right away that the classification of osteomyelitis is not an easy matter, because each inflammation, alas, is individual. And yet, both acute and chronic osteomyelitis and hematogenous osteomyelitis occur due to bacteria. The most well-known causative agents of chronic osteomyelitis are bacteria such as Staphylococcus aureus (and other staphylococci, by the way), and Pseudomonas aeruginosa. It is also possible for anaerobic bacteria (for example, in diabetes and foot ulcers), gram-negative bacilli, entire groups of bacteria, tuberculosis bacilli, histoplasmosis, brucellosis, etc. to enter the bone marrow.
It is worth noting that acute osteomyelitis often occurs as a result of hidden infections, allergies, lack of nutrients, with weak immunity and general asthenia.
All kinds of injuries, frostbite and burns, colds, severe stress on the body and stressful situations can also “trigger” the disease.
Clinic
There are general and local symptoms of osteomyelitis. General manifestations are nonspecific, they are caused by bacteremia. These are chills, increased body temperature, tachycardia, weakness, fatigue, decreased performance, and drowsiness.
After a few days, local signs of osteomyelitis appear in the affected area: redness of the skin, swelling, local rise in temperature, limitation of movements, pain, a feeling of bursting inside the bone in the affected area. The pain syndrome increases with movements and tapping on the bone.
Later, fistulas with purulent discharge appear. After the fistula breaks through, pain and other signs of inflammation decrease. In chronic osteomyelitis, the presence of old fistula tracts can be seen.
Atypical forms differ in their characteristics. Brody's abscess is characterized by a poor clinical picture. This form of osteomyelitis develops with good immunity. Localization of the pathogen is formed by encapsulating an intraosseous abscess. Pain is detected when the bone is tapped. The X-ray picture is specific - periostitis is weakly expressed, a cavity is found in the bone.
In albuminous osteomyelitis, the soft tissue around the bone becomes saturated with fibrin. Radiologically, the picture of periostitis is not clearly expressed; fibrinous deposits are detected.
Antibiotic osteomyelitis occurs when antibiotics are taken irrationally. The concentration of the drug is insufficient to destroy the microbe. It is encapsulated. The clinic is sluggish, asymptomatic.
With sclerosing osteomyelitis, a subacute onset is noted, with an increase in temperature to subfebrile levels. Periods of remission are followed by exacerbation. Sclerosis of the bone marrow canal occurs, which is confirmed by x-ray.
Prevention
Preventive measures are not only the key to preventing the development of osteomyelitis, but also a factor that reduces the risk of complications and shortens the recovery period if the disease cannot be avoided:
- Timely treatment of caries, even if it has no clinical manifestations.
- Maintaining normal immune status through regular physical activity, rational and nutritious nutrition.
- Sanitation of all chronic foci of infection in the body.
- In case of injury, in the postoperative period or after tooth extraction, compliance with all preventive medical prescriptions.
In conclusion, it should be noted that, despite all the achievements of modern medicine, osteomyelitis of the jaw in adults and children does not lose its relevance. Timely detection of its signs and adequate treatment increase the patient’s chances of a full recovery and maintaining a high quality of life.
Clinical picture and symptoms of acute osteomyelitis after gunshot wounds
The clinical picture is influenced by many factors: how large the volume of the lesion is, what is the degree of bone destruction, how much periosteum has been exfoliated, what is the degree of muscle damage, the condition of the nerves and blood vessels. When injured, the wound always becomes dirty. Many microbes penetrate into damaged areas, which quickly multiply and spread. Further development of the disease depends on the body’s resistance and mental status.
As soon as the infection has spread to the bone structures, symptoms of intoxication appear: body temperature rises, weakness appears, the amount of hemoglobin in the blood decreases, and the number of leukocytes increases. If the process is not stopped, the infection spreads through the bone marrow canal into the periosteum and further into the soft tissue, forming multiple canals and fistula tracts. The process becomes chronic.
Features of the disease in childhood
Chronic osteomyelitis in children occurs differently, depending on their age. This fact makes it difficult to diagnose the pathology.
Due to the structural features of the skeleton, in newborn babies the epiphyseal part of the bone is often involved in the pathological process. Cartilage tissue in the joint area is also affected.
Older children are most often susceptible to the hematogenous type of disease. The situation is aggravated by the difficulty in diagnosis. The pathological process progresses while the child is being treated for another disease.
Odontogenic osteomyelitis is often diagnosed in childhood during the period of replacement of the primary teeth with permanent molars. Untimely treated dental diseases lead to damage to the jaw bone.