Author of the article: Candidate of Medical Sciences O.Yu. Ermolaev
Make an appointment with a gynecologist
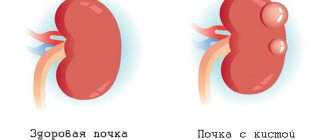
A paraovarian cyst is a round-shaped cavity filled with fluid, located in close proximity to the right and/or left ovary.
The paraovarian cyst is located between the broad ligament of the uterus, between the tube and the ovary.
A paraovarian cyst arises from rudimentary (rudimentary) periovarian tubules (from the epididymis). In other words,
A paraovarian cyst occurs as a result of a disruption in the process of embryonic development, i.e. does not depend on heredity and is not transmitted genetically (to offspring). About abnormal development of the genital organs in detail...
The epididymis reaches its greatest development during puberty, which explains the appearance of paraovarian cysts mainly at the age of 20-40 years.
Cases of detection of paraovarian cysts in girls 7-10 years old have been described.
Paraovarian cyst occurs in 10-12% of all identified tumor-like formations and ovarian tumors.
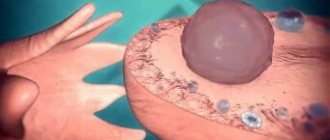
| 3D photo of a paraovarian cyst | |
| 3D photo of a paraovarian cyst of the left ovary. A paraovarian cyst is a round, thin-walled formation adjacent to the ovary. |
See all photos
Pay attention to the excellent quality of the photographs, testifying to the expert class of the equipment of the Women's Health Resort Clinic.
You can find photographs of paraovarian cysts taken by our specialists on many Russian and foreign websites and in textbooks.
A paraovarian cyst never becomes malignant (“does not turn into cancer”), since it is a tumor-like formation. Tumor-like formations grow due to the filling of the cyst and passive stretching of its walls, in contrast to true cysts, the walls of which consist of dividing (multiplying and growing) cells.
Paraovarian cyst never! independently or against the background of conservative (drug) treatment “does not resolve.”
The growth rate and maximum size of a paraovarian cyst are not predictable.
The growth of a paraovarian cyst can be promoted by insolation (sunbathing in natural conditions or in a solarium) and local hyperthermia (taking public baths with a water temperature above 38°C).
| REMOVAL of a paraovarian cyst or OBSERVATION - the gynecologist decides. It is IMPORTANT to start moving in the RIGHT direction! EVERYTHING you need to know about the right direction in the treatment of paraovarian ovarian cysts, see HERE: |
- Symptoms of a paraovarian cyst
- Complications of paraovarian cyst
- Treatment of paraovarian cyst
- Reasonable restrictions in the presence of a paraovarian cyst
- Questions and answers about paraovarian cyst
- Photo gallery paraovarian cyst
Treatment of paraovarian cysts by appointment by multi-line phone number 8 (800) 500-52-74 (toll-free within Russia), or +7 (for international calls).
| ONLINE information about the treatment of paraovarian cysts in Pyatigorsk can be found at REGISTER ONLINE for treatment of paraovarian cyst here. REGISTER online for treatment of paraovarian cyst here. |
Make an appointment with a gynecologist
Reviews about the treatment
Z.R., Nalchik
First of all, thank you very much for the positive experience that every patient receives. The friendliness and professionalism of the staff is already a guaranteed recovery. Oleg Yuryevich - You are a professional with a capital P, a very subtle psychologist, a real doctor. I wish you further expansion and more health, smiling, happy women around you.
Kh.M., Nazran
I am so glad that I found you, you are such a kind, good, bright person. I tell everyone about you. And they also ask me what I found there in this Pyatigorsk. I answer, “I found myself a doctor.” Thank you very much for everything, happiness, health and all the best.
All reviews about treatment in our Clinic
The mechanism of development and causes of paraovarian cysts
The neoplasm develops from the paraophoron. It is a vestigial organ in the ligament between the uterus and ovary. It consists of a duct and small tubules that extend from it. The paraophoron is involved in the formation and development of the reproductive system in girls during the embryonic period, after which it does not perform any functions. The development of a cyst is caused by a violation of tissue differentiation in the embryo’s body. Because of this, during puberty, fluid accumulates in the cavity between the tissues, and the neoplasm increases. Most doctors tend to point to hormonal imbalance as the cause of this phenomenon.
Hormone levels can be disrupted by:
- premature puberty;
- disruptions of the monthly cycle;
- too long periods without medical intervention;
- malfunction of the thyroid gland;
- multiple abortions;
- chronic diseases of the fallopian tubes and ovaries;
- low-grade inflammation and infections of the internal genital organs, provoked by sexually transmitted infections;
- taking incorrectly selected hormonal contraceptives;
- excess weight;
- too strict diets and sudden weight loss;
- excessive passion for natural and artificial tanning;
- improperly performed physiotherapeutic procedures of the pelvic organs;
- excessive physical activity;
- frequent long-term stress.
Description of the disease
A paraovarian cyst is a safe ovoid neoplasm that never develops into a malignant tumor. It begins to appear during intrauterine development due to various disorders; it is detected in women aged 20-40 years, and rarely in teenage girls.
The tumor is localized above or in front of the ovary, has thin smooth walls and a cavity filled with fluid.
A paraovarian cyst is localized above or in front of the ovary, has thin smooth walls and a cavity filled with serous fluid. Larger formations are characterized by the presence of a stalk formed by the tissue of the ligaments of the uterus, sometimes by ovarian tissue and the fallopian tube. The cyst is nourished by the mesenteric vessels, fallopian tube and its own capillaries; its development proceeds slowly, sometimes over several years.
The cystic tumor increases due to the accumulation of cavity fluid, stretching the walls of the capsule. When the paraovarian formation reaches a size of 8-10 cm, the first symptoms appear.
Symptoms of the disease
Cysts up to 2.5 cm in diameter do not cause any discomfort to a woman and, as a result, are often not detected for a long time. When the cyst grows over 2.5 cm, the clinical picture is blurry, characteristic of most gynecological diseases. A paraovarian cyst with a diameter of more than 5 cm causes pain and a feeling of fullness in the lower abdomen. The pain radiates to the side and sacrum. The intensity of pain does not depend on menstruation and ovulation. The pain intensifies many times after physical work and sports, increases and goes away spontaneously.
A large cyst compresses the bladder and intestines. This causes a frequent urge to urinate and defecate. Both processes are difficult and painful. With an excessively enlarged cyst, the volume of the abdomen increases.
A sign of a paraovarian cyst is often amenorrhea and infertility. In conditions complicated by torsion of the leg or rupture of the capsule, a clinical picture of an acute abdomen is observed: sharp excruciating pain, tension in the abdominal wall, failure of intestinal motility. This condition requires immediate hospitalization and surgery.
Signs of pathology
Symptoms appear if the cystic formation reaches 3-5 cm in size. Until this moment, it usually does not manifest itself in any way and is discovered by chance during a gynecological examination.
Symptoms are inextricably linked, first of all, with the size of the formation
A cavity with fluid of considerable size often causes pain of a pulling or bursting nature. They are localized on the side of the formation in the lower abdomen, radiating (give) to the hypochondrium, lumbosacral or groin area. The cause of pain is the pressure of the cyst on surrounding organs. The appearance of pain is usually provoked by physical activity, hypothermia or overheating of the body, stress, and straining. A characteristic feature of pain is that it can subside on its own, without taking analgesics.
The following manifestations are also possible:
- Painful and frequent urination.
- Abdominal pain of uncertain localization, accompanied by unstable stools, in which constipation is replaced by diarrhea. Patients often complain of painful bowel movements and flatulence.
- Painful, irregular, scanty or heavy periods, even uterine bleeding. There may be spotting that is not associated with the menstrual cycle, often appearing during pregnancy.
- Unilateral protrusion in the lower abdomen, if the cyst located in this area grows quickly and reaches a large size.
As a rule, the presence of a small cavity does not affect the chances of pregnancy and bearing a healthy child. Pregnancy itself can give rise to the growth of a cystic formation with possible complications.
Diagnosis of paraovarian neoplasm
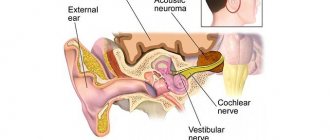
To make a preliminary diagnosis, an examination in a gynecological chair and palpation of the abdomen is sufficient. The cyst can be felt as an elastic roundness, motionless when pressed. To clarify the diagnosis, the woman is sent for a transvaginal ultrasound. On the monitor, a paraovarian cyst appears as a single-chamber neoplasm outside the ovary, which distinguishes this type from other cysts.
If there is doubt about the type of tumor, diagnostic laparoscopy is prescribed. This procedure is performed in a hospital setting under general anesthesia. The abdominal wall is punctured and a tube is inserted into the puncture, through which carbon dioxide is supplied to expand the space. Next, a device in the form of a long thin tube with a camera and an LED is placed under the peritoneum. By turning this camera in the desired direction, the doctor examines the affected area. The image is displayed on the PC monitor in an enlarged format. For small tumors, the paraovarian cyst can be removed immediately. If it is very large, a separate operation is required.
It is important to differentiate a paraovarian cyst from appendicitis, endometritis, cancer, ectopic pregnancy and other types of cysts. Only after final confirmation of the diagnosis is treatment prescribed.
Causes and development factors
It forms after reaching puberty, but according to statistics, there is a small percentage of patients whose cysts form in childhood.
The exact causes of their occurrence have not been identified, but there are a number of predisposing factors.
These include:
- exposure to unfavorable factors on the fetus (it is believed that cysts of this type are formed from the remains of embryonic tissue due to disorders of intrauterine development);
- early onset of menstruation (at 11-13 years);
- chronic inflammatory focus in the pelvis, including against the background of sexually transmitted infections;
- a history of abortions and miscarriages;
- uncontrolled use of oral contraceptives, which is fraught with sharp fluctuations in hormonal levels;
- endocrine diseases, including diabetes mellitus, thyroid pathology, pituitary adenoma;
- hereditary predisposition to the development of cystic formations;
- chronic physical and nervous stress;
- temperature changes and warming up the lower abdomen (sauna, mud in the treatment of gynecological diseases, lumbosacral osteochondrosis);
- excessive exposure to ultraviolet radiation when visiting a solarium;
- pregnancy, puberty, menopause, since during these periods of a woman’s life there are sharp changes in hormonal levels.
Preparing for surgery
Before the intervention, the woman is sent for examination:
- blood clotting test;
- general analysis of urine and blood;
- test for HIV infection;
- biochemical analysis;
- hepatitis test;
- vaginal smear test for microflora;
- colposcopy;
- Ultrasound of paraovarian cyst;
- fluorography;
- ECG.
The examination is necessary in order to confirm the absence of contraindications and protect the woman from complications.
Classification
Depending on the location of the tumor, such pathology has several forms:
- paraovarian cyst on the right - most often occurs in women of childbearing age, has a pedicle and forms between the ovary and the uterus;
- paraovarian cyst on the left - cases of diagnosis in teenage girls are not uncommon. It can reach large sizes, but otherwise is no different from the previous variety;
- bilateral lesion - the ovaries are affected on both sides. This type of occurrence is extremely rare.
Depending on the volume, paraovarian ovarian cysts are divided into:
- small - characterized by the fact that their size does not exceed two and a half centimeters, and also does not have a leg;
- medium - from 2.5 to 5 centimeters;
- gigantic - are considered such if they exceed 5 centimeters. It is noteworthy that they can have a leg. It is its presence that constitutes the main danger of such a pathology.
Paraovarian cysts
Laparoscopy of paraovarian cyst
The principle of this operation is similar to diagnostic laparoscopy. Hospitalization and general anesthesia are required, which is selected individually. The course of the operation is similar to that of diagnostic laparoscopy. The difference is that during surgical laparoscopy, the doctor makes an additional puncture and inserts an instrument into it. With its help, he carefully cuts off the stem of the cyst and removes its body out. After this, the ovary is additionally examined to exclude the presence of other small neoplasms. Next, the gas is released, the punctures are fixed with suture material or tightening patches.
Very large cysts are punctured and drained using a special device. This is necessary for easier removal - there is no need to cut off the cyst and remove it completely. After the fluid is removed, ethyl alcohol is poured into the cyst, which causes sclerotization of the pathological tissues. The duration of the operation is from 20 minutes to several hours, depending on the volume and complexity of the intervention.
The advantages of the operation are quick recovery. After just five days, a woman can return to normal work and rhythm of life. Scars on the abdomen are almost invisible.
Diagnostics
The difficulty in detecting a paraovarian cyst is that at first it does not have pronounced symptoms. It is often detected during a routine medical examination, ultrasound examination, and sometimes during diagnosis due to infertility.
Symptoms appear in the presence of complications or when the paraovarian formation reaches a significant size. During palpation, it is not difficult for a doctor to detect a formation larger than 3 centimeters. During manual examination, tumors of the ovary are felt, which are usually located on the side of the uterus or above it.
Using vaginal ultrasound, it is determined as a tumor-like, ovoid-shaped formation.
Through vaginal ultrasound, the formation is determined to be a tumor-like, ovoid-shaped formation, through the thin walls of which a homogeneous fluid is visible. Usually, the doctor immediately distinguishes it from other types of tumor, but to accurately determine a paraovarian cyst, it is possible only by the results of histology, which can only be done after surgery.
Paraovarian cyst during pregnancy
It is highly advisable to check for the presence of a cyst when planning a pregnancy.
After the operation, you need to wait 6-12 months and make sure that there are no relapses. If conception occurs with a small tumor, hormonal changes can cause it to grow rapidly. Due to the increasing pressure of the uterus on the cyst, torsion of the tumor's legs, suppuration and even rupture are possible. These conditions require urgent surgical intervention. This can have a negative impact on the fetus and even require termination of pregnancy.
In rare cases, when hormonal changes do not cause the cyst to grow, it cannot affect the health of the woman and the embryo. Then urgent treatment is indicated in the postpartum period.
Childbirth can occur naturally, but strict medical supervision is necessary. During childbirth, there is a high probability of rupture or strangulation of the cyst. The rupture causes profuse blood loss, which can cause shock and even death. To avoid danger, many patients are prescribed a caesarean section.
Reasons for development
There are many factors that lead to the formation of a paraovarian cyst. It is not always possible to establish the root cause of the disease.
Sometimes the formation of a tumor can even be influenced by the bad habits of the mother during pregnancy, which affect the health of her unborn child (smoking, drug and alcohol use, treatment with unauthorized drugs, poor nutrition).
The mechanism of cyst formation itself is known; it occurs as a result of disturbances in the embryonic development of the appendage tubules (paraovaria). They either have poorly formed excretory ducts, or they can be clogged, and sometimes even absent, which is why secreted fluids do not find an outlet and accumulate, forming elastic sacs.
The numbers in the image indicate paraovarian ovarian cysts
Experts note the following reasons for the formation of a paraovarian cyst:
- disruptions in the maturation of ovarian follicles, lack of ovulation;
- deviations in the ratio of hormones caused by various endocrinological diseases or tumor processes;
- onset of first menstruation before age 11, early puberty;
- abortions and pelvic organ surgeries;
- taking anabolic steroids;
- hormonal surges during puberty and at the onset of menopause;
- taking estrogen antagonists in the treatment of breast cancer (Tamoxifen);
- infectious lesions of the genitourinary system and other internal organs;
- poor environmental conditions, polluted air;
- increased emotional stress, stress, depression;
- inflammation of the ovary and uterine appendages (oophoritis, salpingitis, adnexitis);
- improper use of hormonal contraceptives;
- frequent sunbathing under the sun or in a solarium;
- overheating of organs due to taking hot baths, visiting saunas, baths, etc.
Prognosis and complications
If the operation is performed in a timely manner, the ovaries can be saved. Reproductive function is preserved. You can plan a pregnancy 4-5 months after removal of the paraovarian cyst.
If there is no treatment, complications arise.
- Suppuration of the cyst and ovary caused by prolonged inflammation. The condition is characterized by severe pain. Urgent surgical intervention is required.
- Cyst rupture. The causes of rupture can be injuries and too intense physical activity. The fluid pours into the abdominal cavity, which causes acute inflammation of the internal organs. The woman's blood pressure drops and she faints. Treatment is only possible through surgery.
- Torsion of the cyst stalk. The neoplasm rotates around its axis, causing the leg to twist. Tissue compression leads to the fact that the vessels stop supplying blood in the required volume, and tissue necrosis begins. In this condition, pain in the sacrum, lower back and lower abdomen becomes excruciating. Surgery is urgently required to remove the cyst, the affected ovary and surrounding tissue.
- Anomalies of the anatomy of the fallopian tubes. The pipes are deformed under the load from the enlarged tumor. This leads to difficulties with conception, pain and discomfort.
Treatment
A paraovarian cyst will not go away on its own. Taking medications and traditional medicine will also not help cure it completely. If the disease is diagnosed early, surgery is not prescribed if the paraovarian formation does not grow. The doctor prescribes hormonal therapy and regularly monitors the development of pathology.
A - Pathology. B, C - removal of the cyst, D - end of the operation.
Removal surgery is performed if a woman is planning a pregnancy or when the formation continues to grow and poses a risk of complications. A gentle procedure is performed: laparoscopy is an intervention technique in which special devices and a camera are inserted into the abdomen through small incisions; the doctor monitors the progress of the work through a monitor.
The surface of the ovary where the cyst is located is dissected, the edges of the wound are separated, the cyst is moved away from the uterine ligaments for further desquamation. At the same time, the ovary itself and the fallopian tube are preserved, which, due to its properties, is deformed and regains its former shape. Mostly, the operation is performed under local anesthesia, the scars after it are almost invisible, and the woman can leave the hospital the very next day.
Scar after laparotomy when removing a large cyst.
If the cyst is large, another surgical method is used - laparotomy, which involves dissecting the peritoneal cavity; often the cyst is removed along with the ovary. This method is traumatic and leaves a visible scar.
Prevention of paraovarian cyst
The key to preventing cysts is regular visits to the gynecologist and ultrasound examinations. This helps to identify the tumor in the early stages, when the disease is asymptomatic.
Infectious diseases of the genitourinary system should be avoided. To do this, you need to maintain personal hygiene and wear cotton breathable underwear. It is necessary to refuse unprotected sexual contacts with unverified partners.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: Publication date:
Prevention
Medicine does not know the exact reasons for the development of paraovarian cysts. Only the factors that provoke its occurrence and growth are known, which every woman can avoid. Measures to prevent this cystic formation are as follows:
- Treat infectious and inflammatory pathologies of the genitourinary system in a timely manner.
- Strictly monitor your hormonal levels; at the slightest disruption, contact a specialist.
- Avoid casual sex, use reliable barrier contraception measures.
- Do not overuse visits to the solarium, baths/saunas. Avoid prolonged exposure to open sun.
- Visit a woman’s doctor regularly (at least once every six months) for timely detection of diseases dangerous to women’s health.
Cystic ovarian change and pregnancy
Basically, the disease is asymptomatic; their manifestation depends only on the size of the capsule and its type. The following symptoms of the disease (large cysts) are distinguished:
- aching pain in the back, lower abdomen;
- pain in the left side (if the paraovarian cyst is on the left) and pain in the right side (if the paraovarian cyst is on the right);
- the appearance of a feeling of discomfort in the lower abdomen or pain that is not related to the period of menstruation and ovulation;
- sharp pain or its intensification when playing sports or other activities;
- the ability to feel the cyst during examination;
- frequent constipation or diarrhea (due to intestinal compression);
- painful urination;
- increase in abdominal size;
- a sharp decrease or increase in blood discharge during menstruation;
- the presence of foreign discharge during menstruation.
Patients with this diagnosis require special attention. Doctors regularly monitor the patient's condition. If the disease was diagnosed before the artificial insemination procedure, it is imperative to remove the paraovarian cyst.
Quite often, a cyst is diagnosed after pregnancy. Cysts up to 5 cm will not affect the course of pregnancy in any way, but there is a possibility that due to changes in hormonal levels the size of the tumor will increase.
Cavity formation can be completely asymptomatic and detected by a gynecologist during routine preventive examinations or an ultrasound examination of the pelvic organs for another reason.
- leg torsion;
- capsule rupture;
- suppuration.
We suggest you read: How cysts formed in the vessels of the brain resolve after a stroke
In this case, complaints signaling a catastrophe in the abdominal cavity come to the fore. These include:
- cramping abdominal pain;
- weakness;
- nausea and vomiting;
- dizziness;
- feeling of fear;
- chills;
- drop in blood pressure;
- decreased intestinal motility;
- hyperthermia.
When the formation of the periovarian appendage reaches a significant size, and in some cases its diameter can reach 20 centimeters, symptoms of compression of neighboring organs come to the fore.
Cavity formation of the periovarian appendage does not respond to fluctuations in the level of sex hormones; its characteristic feature is the absence of dependence of the intensity of pain on the phase of the menstrual cycle.
If there is a cystic formation of the paraophoron, it is necessary to decide what to do with it, and only then plan a pregnancy. If the cyst is 1-2 cm in size, surgery may not be performed; if larger, laparotomy is indicated. It is better to plan conception no earlier than 3 months after surgery.
The discovery of a paraophoron cyst in a pregnant woman is not a contraindication to pregnancy. It is necessary to regularly visit an antenatal clinic and follow the recommendations of an obstetrician-gynecologist.
The small diameter and lack of growth of the cavity formation allow us to limit ourselves to ultrasound monitoring during pregnancy and with the exception of:
- excessive physical activity;
- sexual intercourse in the presence of discomfort, pain during or after intimacy;
- thermal procedures (sauna, hot bath, etc.).
It is necessary to observe a work-rest schedule and wear a bandage in late stages of gestation.
The rapid growth of the cyst and the development of complications are not compatible with conservative tactics. Modern technologies make it possible to perform operations without disrupting the course of pregnancy.
A paraovarian ovarian cyst forms in the space limited by the ligaments of the uterus, ovary and fallopian tube. It affects not only the gonads, but also the uterine appendages. The cyst itself is a thin-walled formation of an oval, less often round shape, with a tight consistency.
Inside, the cyst is a smooth-walled, homogeneous structure filled with aqueous fluid. It contains a large amount of protein and some mucin. The formation is characterized by low mobility and slow growth.
The increase in size occurs as a result of the accumulation of cyst contents and stretching of its walls. A paraovarian cyst can reach 10–15 cm in diameter. Such formations are not predisposed to malignancy (degeneration into cancer).
Women who have this pathology often wonder whether a paraovarian cyst affects conception. Doctors say that this formation is not an obstacle to conception. This is confirmed by cases of pregnancy in which a paraovarian cyst is detected during the next ultrasound.
If the cyst is larger than 5 cm in diameter and continues to grow, a surgical response may be considered. At the same time, doctors try to combine this event with childbirth. If delivery is still far away, and the cyst is large and interferes with the normal development of the fetus, laparoscopy is performed - a low-traumatic operation in which access is carried out through three punctures on the abdominal wall.
Small cystic formations do not cause symptoms. A woman can walk with a cyst for a long time without knowing about its existence. Pathology can be detected during a routine examination or an ultrasound scan when diagnosing another disease.
The first signs and clinical manifestations of the pathology are noted when the cyst reaches a diameter of 5 cm. The growth of the cyst is accompanied by the periodic appearance of aching and bursting pain in the side on the affected side.
Increased pain occurs with increased physical activity and stress. A characteristic feature is a sharp, spontaneous cessation of pain. There are other clinical signs of the disease. When a paraovarian cyst develops, symptoms may include the following:
- compression of the bladder, intestines - manifested by urination disorder, constipation or frequent urge to go to the toilet;
- increase in abdominal volume - occurs with rapid growth of the cyst;
- menstrual irregularities (not always observed).
Initially, doctors conduct numerous examinations to find out whether hydrosalpinx or paraovarian cyst is observed in a particular case. With hydrosalpinx, fluid accumulates in the lumen of the tube, which also causes a change in its volume. Doctors say that treating paraovarian cysts without surgery is not possible.
If the formation is small, a wait-and-see approach can be adopted: doctors attempt hormonal therapy, with the help of which it is rarely possible to achieve positive results. Due to the fact that paraovarian cysts occur more often in women of reproductive age and can become complicated, doctors prefer to adhere to surgical treatment. Planned removal of the cyst is mandatory when planning a pregnancy using IVF.
When a paraovarian cyst is discovered, treatment with hormones is rarely performed. According to clinical studies, the use of hormonal agents for this type of cyst is ineffective.
However, they can be used as part of complex therapy for cysts. These drugs are prescribed for symptomatic treatment, normalization of the menstrual cycle, which is sometimes disrupted with a paraovarian cyst. In such cases, drugs based on estrogen and progesterone are used:
- Yarina,
- Janine,
- Proginova,
- Premarin.
For a disease such as paraovarian ovarian cyst, treatment with folk remedies can be considered as an auxiliary method. With their help, it is possible to reduce pain and remove some symptoms.
Basically, all the symptoms of a paraovarian cyst are inextricably linked with its size. Small cysts, as a rule, may not manifest themselves for a long time. The main symptom is pain. It appears only when the cyst greatly increases in size.
Typically, paraovarian cysts do not grow larger than 8 or 10 centimeters. But even a cyst of 5 centimeters can cause pain. Such a cyst can put pressure on the intestines or bladder. The pressure can lead to pain when urinating. It may also cause constipation or stomach upset.
One of the symptoms of a paraovarian cyst is pain in the lower abdomen or in the back, in the sacral area. Sometimes, such a cyst can manifest itself through disruptions in the menstrual cycle.
A paraovarian ovarian cyst differs from other types of cysts in its composition, size and type of membrane. Typically, such cysts contain clear fluid inside.
In addition, the membrane of a paraovarian cyst is thin, which distinguishes it from true cysts. Such a cyst is always single-chamber. A paraovarian ovarian cyst can be pedunculated or non-pedunculated. Usually, while the cyst is small, it grows directly on the ovary without a stalk. But as it grows, the cyst can form a stalk.
Another distinctive property of such a cyst is that it does not degenerate into a cancerous tumor. But at the same time, complications may arise. For example, twisting of the cyst stalk, which can be accompanied by severe pain.
Very often, a paraovarian cyst grows on the right ovary. Women of childbearing age are mainly susceptible to this disease. But such cysts can also appear in girls during adolescence.
A paraovarian cyst on the right can grow between the uterus and ovary. Small cysts are without a stalk, but large ones can form a stalk. This stalk may consist of a fallopian tube or an ovarian ligament.
Who's at risk
It is difficult to identify any groups of people prone to the disease. Among all ovarian neoplasms, the described disease occupies approximately 10-15%.
The most reliable prognostic dependence is age-related:
- In childhood (up to 11 years) and during puberty (12-17 years), such neoplasms are almost never registered. - They are either absent or they are extremely small in size (less than 1 cm). - To the point that they are not identified on ultrasound.
- Similarly, paraovarian neoplasm is a rare diagnosis in menopause (45-55 years) and in old age (after 60 years).
- In 90% of all cases, pathology is observed during puberty, especially during childbearing age (18-45 years).
Women during pregnancy
Pregnancy with a paraovarian cyst always proceeds normally (unless, of course, there are any other concomitant pathologies).
In the early stages, the neoplasm cannot affect the development of the embryo at all.
Occasionally during pregnancy, especially in the later stages (third trimester), an already existing cyst increases slightly in size.
- Some doctors attribute this to the influence of specific hormonal levels during pregnancy.
- Others have suggested that fetal growth changes the regional anatomy of the peritoneum. Accordingly, this also affects the paraovarian pathological structure.
The issue of in vitro fertilization is discussed separately.
Here everything is decided by 3 factors:
- structure size;
- presence of a leg;
- internal contents.
Usually, the gynecologist gives the go-ahead for IVF if the tumor is small (less than 3 cm) and does not have a leg. In other cases, the doctor does not recommend, or gives a direct contraindication to the IVF protocol.
The main reason is that the cyst will interfere with the puncture, and in the future it may twist, become inflamed, or rupture.
Conservative treatment methods
This disease cannot be treated conservatively without surgery. It is only possible to slow down the growth of education by prescribing medications. For this purpose, combined oral contraceptives are used.
These include:
- Regulon;
- Novinet;
- Duphaston;
- Diana is 35.
Characteristic features of the tumor
Since this cyst is formed from healthy tissue of the appendage,
it is not prone to malignancy, but can reach large sizes and compress nearby internal organs. At the initial stages of development, symptoms of the disease do not appear, so it is difficult to diagnose the tumor without additional instrumental methods. Paraovarian cyst of the right ovary is much more common than the left one, this is explained by the anatomy of the organ (the right ovary is more active and bears significant loads during periods of changes in a woman’s hormonal levels).
Conservative methods of therapy, that is, treatment without surgery for this type of benign formation are considered ineffective and are not used in gynecological practice.
The paraovarian cyst located near the ovary is removed, for this purpose laparoscopy is used (the operation is performed through a small incision in the peritoneum) or the abdominal method (for large cysts).
Treatment provided
Unlike follicular tumors, treatment of paraovarian cysts with folk remedies or medications is not used due to the fact that cases of its resorption or reduction have not been recorded in medicine. The only effective method is laparoscopy or abdominal surgery. By removing the tumor in a timely manner, doctors preserve women’s health, the integrity and function of the ovaries. A successful operation allows you to plan a pregnancy in the future, carry and give birth to a child. The choice of surgical methods depends on the location and volume of the tumors.
After laparoscopy, women are discharged home on days 2-3, after abdominal surgery on days 7-10. To fully restore sexual and reproductive abilities, a gentle motor regimen is recommended in the first months after surgery and strengthening therapy (full rest, moderate physical activity, good nutrition, taking vitamins and microelements) for 3-6 months.
It is important to know! Only a doctor can prescribe the treatment necessary for the affected ovary. Self-medication can only worsen your health condition. The sooner you see a doctor, the greater the likelihood of a speedy recovery.
If a paraovarian formation is detected in time and treated (surgery is performed), all adverse consequences and complications for the female body can be avoided. To prevent the disease, you need to undergo routine gynecological examinations and follow all medical recommendations and prescriptions.
Symptoms
Symptoms of a paraovarian cyst vary in severity.
Small pathologies without legs will be asymptomatic.
Common manifestations include:
- mild or moderate pain syndrome - pain in the lower abdomen, in the side;
- a feeling of spasm and discomfort in the lower abdomen outside of menstruation;
- irregularities during menstruation;
- changes in the menstrual flow itself, both in volume and quality;
- with careful palpation there is a chance to feel an oval or round compaction;
- the frequency of urination increases, pain may occur during urination;
- Possible bowel dysfunction, constipation;
- There may be a slight increase in the abdominal area, as if bloated during gas pollution.
In the event of complications (rupture of the cyst, torsion of the leg, compression of the fallopian tube), the symptoms change dramatically.
It becomes many times more pronounced:
- First of all, the pain syndrome increases significantly, and a condition of acute abdomen occurs.
- The general condition resembles shock. The temperature rises sharply (or, conversely, drops sharply), nausea and vomiting occur.
- There is tachycardia, decreased blood pressure and cold sweat.
- The skin on the abdomen becomes very pale.
If such a symptomatic picture occurs, urgent medical attention is required.
Diagnostic methods
Most often, the disease is diagnosed during a routine examination by a gynecologist or during an ultrasound scan. The gynecologist palpates the abdomen. On the side above the uterus, the presence of a slow-moving, dense, tumor-like neoplasm is noted; when pressing on it, the woman may experience severe pain.
An ultrasound of the abdomen may be performed, but a transvaginal examination is considered more informative. During the procedure, a neoplasm with thin walls and homogeneous internal contents is discovered.
Less commonly, it is detected during a diagnostic laparoscopic examination to determine the causes of infertility. During laparoscopy, a small hole is made in the peritoneum and the laparoscope is inserted through it. During this procedure, a paraovarian ovarian cyst is discovered.
The disease must be differentiated from ectopic pregnancy, ovarian cancer and other types of cysts. All of these diseases can be accompanied by similar symptoms.
Ultrasound of the ovaries
Other types of neoplasms
In addition to paraovarian cysts, the following types :
- functional. Formed during menstruation. The reason for the formation is an imbalance of hormones in a woman’s body. Develops before the age of 40. Characterized by increased pain during physical activity and fast walking;
- follicular. A risk factor is long-term persistent hormonal imbalances. With these cysts, prolonged and acute pain in the lower segment of the abdomen, a rise in body temperature, a feeling of fullness in the lumbar region, disruption of the menstrual cycle (duration, volume of discharge), spotting discharge in any phase of the cycle are noted;
- Corpus luteum cysts. Belongs to the functional type. The reason for its formation is still unknown. One of the assumptions is that it is a consequence of impaired blood flow and lymph circulation within the ovary itself. Another theory says that the reason lies in hormonal imbalance. Formed after the absence of long-term reduction of the corpus luteum. The size can reach 8 cm. It is characterized by a rise in basal temperature, a pain reaction in the projection of the appendages, a delay in menstruation for more than 2 weeks, a feeling of fullness in the abdomen;
- dermoid. It is a consequence of impaired embryogenesis. It can be detected in women of absolutely any age. It has a round shape, inside there are particles of hair, teeth, and fragments of bone tissue. For a long time it does not attract attention until a hormonal imbalance occurs. Very often it can be diagnosed in the postmenopausal period, during pregnancy, lactation, and puberty;
- serous. Also referred to as cytoadenoma. It is a cavity formation filled with transparent contents, with rigid walls. It develops directly in the body of the ovary, due to which the latter increases in size. With this cyst, women most often complain of painful sexual intercourse and menstrual irregularities. It is extremely rarely complicated by rupture.
Dangerous complications
Complications of such a disease can have very sad consequences if no measures are taken: from problems with childbirth to a threat to life.
Torsion of pedunculated cyst
The cord connecting the cyst cavity to the ovary, uterus or fallopian tube is capable of twisting.
This can happen spontaneously or due to mechanical trauma. But an acute symptomatic picture always occurs.
First of all, it is characterized by a pronounced pain syndrome. If nothing is done, the twisted cord quickly becomes inflamed.
Then symptoms of general intoxication arise:
- high temperature up to 39 degrees;
- nausea;
- vomit;
- dizziness;
- weakness.
Cyst torsion is an indication for urgent surgery.
Capsule rupture
Rupture of a paraovarian cyst occurs much less frequently than twisting of the pedicle.
The tumor may burst:
- for particularly large sizes;
- mechanical injury (fall, blow);
- in case the cystic structure is unsuccessfully deployed and experiences strong pressure from surrounding tissues and organs.
If severe pain comes first during torsion, then the rupture may not be accompanied by severe pain.
But due to the leakage of cystic contents into the pelvic area, symptoms of intoxication quickly develop.
Suppuration
Suppuration is a sign of a chronic course. This occurs when, in addition to the cyst, there is a chronic genitourinary infection.
The attachment of a bacterial pathogen is symptomatically more blurred. Usually, this fact begins to be indicated by an evening low-grade fever, joined by dull, nagging pain in the lower abdomen, as well as cloudy, foul-smelling vaginal discharge.
At first, the purulent process does not produce such acute conditions as other complications. But if the cyst is not removed in time and treated with antibiotics, then there is a high probability of developing an abscess - a large source of infection, essentially a purulent bubble inside the tissue.
An abscess poses a serious threat to a woman’s reproductive system, and even to life itself, because threatens the onset of general sepsis.
Disease prevention
Preventive measures for paraovarian cysts are as follows:
- correction of diseases of the endocrine system;
- restoration of normal hormonal levels;
- maintaining proper and balanced nutrition;
- timely diagnosis and treatment of infectious and inflammatory processes;
- avoid exacerbations of chronic pathologies;
- normalization of body weight;
- adherence to sleep and wakefulness;
- maintaining an active lifestyle;
- use of hormonal drugs only as prescribed by a doctor.
Location Features
The blood supply to the right ovary is more intense than to the left. Therefore, most often you can find a paraovarian cyst near the appendages located on the right side .
In this case, the cyst also has a good blood supply, due to this there is a sufficient supply of nutrients for it. The result is an achievement of significant size.
A formation may appear on the left, next to the left ovary. But this is much less common, and such a cyst has a more flattened base.
Symptoms of pathology
Any woman who knows about the symptoms of a paraovarian tumor can suspect its development in her body. The presence of pathology is indicated by the following characteristic signs:
- Pain that is nagging in nature. They are felt in the abdominal area. The pain often extends to the lower back.
- Discomfort in the anus. It is also possible that a feeling of numbness in the rectum may occur.
- Constant urge to go to the toilet. This phenomenon is due to the fact that the tumor puts pressure on the bladder. Urination itself may be accompanied by mild pain.
- False need to defecate, prolonged constipation. This is because the cyst compresses the rectum.
- An increase in the volume of the abdomen due to a tumor growing inside it. Asymmetry caused by the development of a cyst in only one ovary cannot be excluded.
- Problems conceiving a child and disruption of the menstrual cycle.
Symptoms of the disease manifest themselves only if the tumor begins to grow significantly. Until it reaches 3 cm, a woman will not even know about its existence, unless she visits a gynecologist for a routine examination. The main signs of pathology reveal themselves when the cyst grows to 6 cm.
The pain caused by the cyst is periodic. This means that they arise on their own and also disappear. Their intensity especially increases when a woman experiences physical activity or has sex.
It is worth noting that a paraovarian cyst rarely affects the menstrual cycle.
Surgical intervention
All small cysts that do not cause discomfort and do not have any clinical symptoms are subject to dynamic observation.
If the size of the cyst reaches 5 cm or more, and also changes the functioning of nearby organs (compression), then surgical intervention is indicated to treat these formations.
Surgical treatment
of paraovarian cysts is carried out through:
- laparoscopy;
- laparotomy.
Laparoscopy is the most acceptable, as it is less traumatic and also has a better cosmetic effect. The operation can be performed under general anesthesia or spinal anesthesia. 3 punctures are made in the anterior abdominal wall, through which special equipment is inserted into the abdominal cavity.
The laparotomy method involves incision of the anterior abdominal wall. Used less frequently, it is used most often for complicated cysts.
If the pathology is uncomplicated, then during surgery the anterior layer of the broad ligament of the uterus is dissected with further enucleation of the paraovarian cyst from the interligamentary space. The ovary and fallopian tubes must be preserved.
After enucleation of the cyst, the uterine tube returns to its normal shape and correct location.
It is extremely rare to resort to puncture of the cyst cavity with further drainage of the contents, after which alcohol is introduced to promote its sclerosis.